Merseyside Cheshire Pathology QIPP Network Progress and Challenges
- Slides: 10
Merseyside & Cheshire Pathology QIPP Network “Progress and Challenges” Ken Barr Network Director
MCPN Pathology Network l 9 Trusts on 14 sites l 3 x Acute FT, 4 x Specialist FT, 2 x Acute l Population served ~1. 7 m l 5. 7 m requests per annum with 25. 8 m tests l 1, 030 staff l £ 64 m direct budget spend 2009/10 l ~12, 400 sq m lab space currently in use l QIPP savings target = £ 14 m
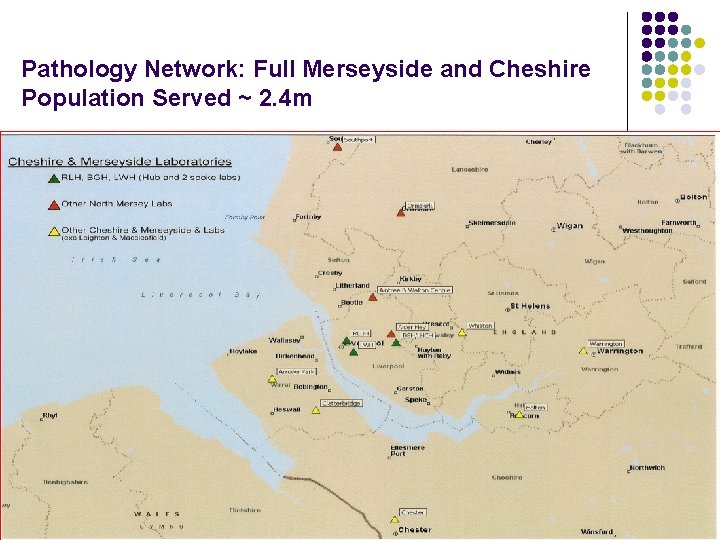
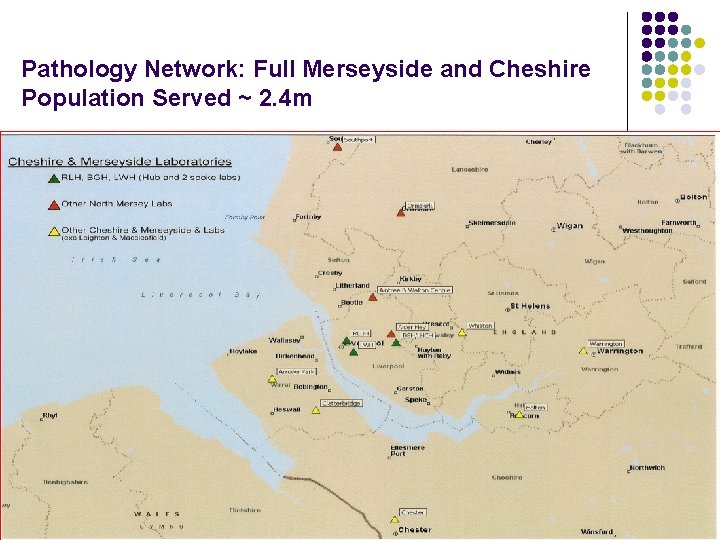
Pathology Network: Full Merseyside and Cheshire Population Served ~ 2. 4 m
Network Progress Vision: “To provide an efficient and effective Pathology service that is patient focused and clinically led, delivering measurable quality and performance that is continually improving” l Establish a singly managed Pathology organisation l Consolidate and re-design services using a hub & spoke model, supporting community and primary services to keep patients as close to home as possible l Through clinical leadership reduce inappropriate variation in tests and results via standardisation of operating processes and protocols, using evidence-based best practice l Invest in IT connectivity to improve access to information to support patients/NHS staff with the right services at the right time in the right place l Establish a single Pathology Integrated Board to manage and deliver pathology services in the most efficient and effective manner to save £ 14 m by 2014/15
Outline Business Case l Single managed network with single identity/employer l l ‘Carter consolidated model’ – hub and spoke concept l l Cost benefit analysis to include access to peer support, R&D, training, MDTs etc. Clinically led integrated services l l Improve standardisation, quality, efficiency based on agreed TAT Centralise specialist and sub-specialist services l l NHS host, social enterprise, JV Centralise multi-discipline, automated, non-urgent testing l l Flexibility to reuse/rent space as available and affordable Explore options for single business structure l l Remove historic organisational barriers and deliver services to population/GPs Respond to population/patient needs - improve access & patient experience Increased efficiency l Reduce direct spend from £ 64 m to £ 50 m over four years (>20%)
Challenges: Pathology Information Systems l 7 different types of LIMS in MCPN - some integrated to PAS systems l Cost issues – need migration plan funded via overall efficiencies l Keep track of referred test and samples within and outside the network l Procure same analytical equipment – avoid risk of poor standardisation l Many interfaces required, order comms/reporting, GP messaging, cytology recall, GUM, cancer registry, infection control etc. l Operational – report printing, management, finance, audit, R&D l Many supporting IT systems – document management, supplies, asset register, risk register, QC information l POCT connectivity, order and result comms to community/primary sectors
Transport • Key to making the network viable – Pathology specific • May require temperature regulated vehicles on longer routes • May utilise motorcycles couriers on shorter routes • Needs to be flexible, based on “zones” + ad-hoc collections • IT tracking, specimen numbers, collection times, management • Specialist companies are already in use – need scaling up ensure VFM via formal specification and tender
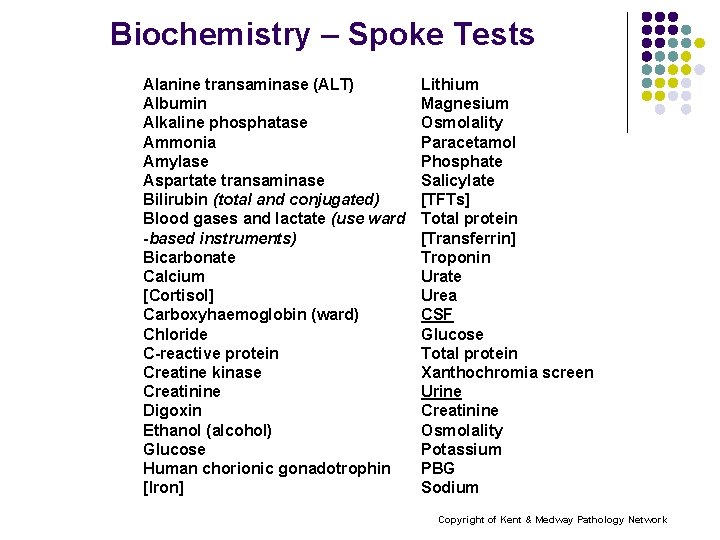
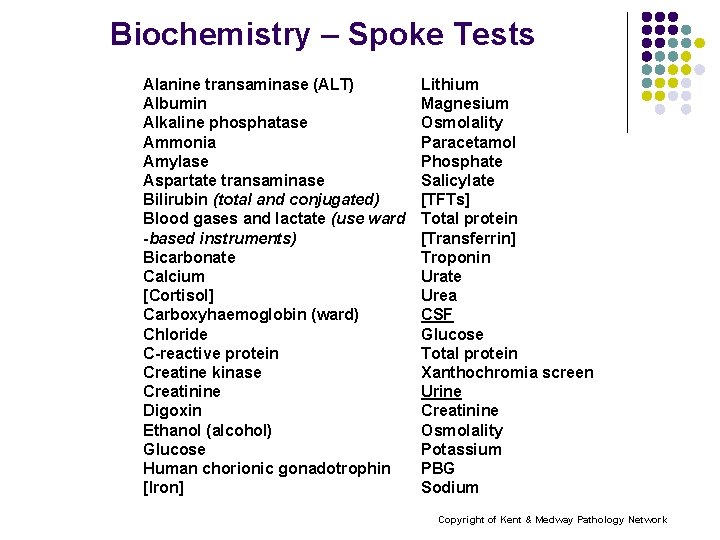
Biochemistry – Spoke Tests Alanine transaminase (ALT) Albumin Alkaline phosphatase Ammonia Amylase Aspartate transaminase Bilirubin (total and conjugated) Blood gases and lactate (use ward -based instruments) Bicarbonate Calcium [Cortisol] Carboxyhaemoglobin (ward) Chloride C-reactive protein Creatine kinase Creatinine Digoxin Ethanol (alcohol) Glucose Human chorionic gonadotrophin [Iron] Lithium Magnesium Osmolality Paracetamol Phosphate Salicylate [TFTs] Total protein [Transferrin] Troponin Urate Urea CSF Glucose Total protein Xanthochromia screen Urine Creatinine Osmolality Potassium PBG Sodium Copyright of Kent & Medway Pathology Network
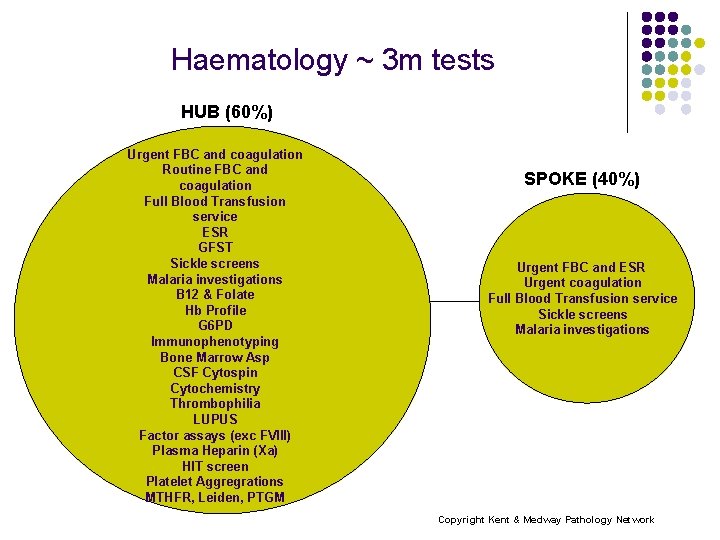
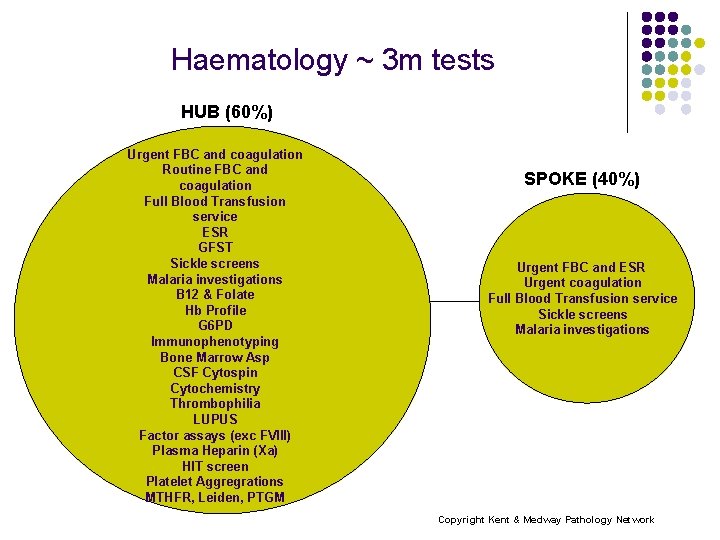
Haematology ~ 3 m tests HUB (60%) Urgent FBC and coagulation Routine FBC and coagulation Full Blood Transfusion service ESR GFST Sickle screens Malaria investigations B 12 & Folate Hb Profile G 6 PD Immunophenotyping Bone Marrow Asp CSF Cytospin Cytochemistry Thrombophilia LUPUS Factor assays (exc FVIII) Plasma Heparin (Xa) HIT screen Platelet Aggregrations MTHFR, Leiden, PTGM SPOKE (40%) Urgent FBC and ESR Urgent coagulation Full Blood Transfusion service Sickle screens Malaria investigations Copyright Kent & Medway Pathology Network
Next Steps l Develop OBC/Service Spec with external management support l l CEO decision on business model/delivery method l l Commence consolidation during 2011/12 Meaningful consultation/communication with staff and stakeholders l l by April 2011 Estate ‘hub’ option appraisal l l by March 2011 To commence November now CEOs have approved OBC work Project team to develop and deliver implementation plan 2011 -2015 l April 2011