Mental Status Examination Chapter 8 Uzm Psk zlem
- Slides: 31
Mental Status Examination Chapter 8 Uzm. Psk. Özlem Ataoğlu
What is Mental Status Examination (MSE)? ¡With MSE, we try to organize and evaluate the patient’s mental status and our clinical observation under the existent circumstances ¡Our primary goal is to evaluate cognitive processes ¡We generally use MSE in medical settings whose psychiatric conditions are severe ¡You have to know how to report MSE – it is very common (everyday procedure) in mental hospitals
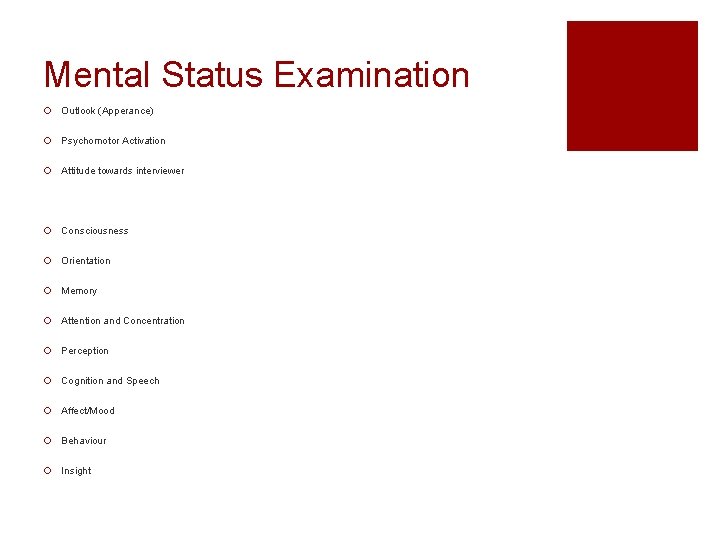
Mental Status Examination ¡ Outlook (Apperance) ¡ Psychomotor Activation ¡ Attitude towards interviewer ¡ Consciousness ¡ Orientation ¡ Memory ¡ Attention and Concentration ¡ Perception ¡ Cognition and Speech ¡ Affect/Mood ¡ Behaviour ¡ Insight
Outlook (Appearance) ¡ You should take notes about the appearance of the patient ¡ Sometimes you can include demographical information as well, if it is related ¡ What is included? ¡ Physical characteristics ¡ Self – care ¡ Clothes ¡ Make – up ¡ Piercing / Tattoo ¡ Height / Weight ¡ Facial expressions ¡ Sweat, trimmer, cold, etc.
¡ You should be careful about these before you start to your interview ¡ Physical appearance can be sign of psychiatric diagnose. Example? ¡ “Ece Taşkın, 24 yaşında, Eskişehir’den görüşmeye geliyor. Yaşından daha yaşlı gözükmektedir. Özbakımı yerindedir. Abartılı bir makyaj yaptığı gözlemlenmiştir. Kıyafetleri görüşmeye uygun, temiz ve düzgündür. Boyu ve kilosu orantısızdır, aşırı kilosundan dolayı diyetine dikkat etmediği düşünülmüştür (fiziksel hastalık – ruled out). Göz kontağı çok kurmamıştır. Ellerinin titrediği gözlemlenmiştir. ”
Psychomotor Activation ¡This is about physical behaviours. You should be careful about them during the interview. ¡Even if your patient denies his/her experiences, you can collect the signs from these activations ¡What can be included? ¡ Eye contact ¡ Repetitive behaviours ¡ Physical behaviours ¡ Scanning ¡ Psychomotor retardation, etc.
¡ Psychomotor activation can be a sign of a psychiatric diagnosis. Example? ¡ Retarded activation depression, schizophrenia, substance use; increased activation anxiety, bipolar disorder, substance use; scanning paranoid behaviour, etc. ¡ “Didem Hanım’ın görüşme esnasında sıklıkla dikkatinin dağıldığı, saatini, gömleğinin yakalarını, saçlarını düzelttiği, küpeleriyle oynadığı gözlemlenmiştir. Ayrıca görüşme odasına ve görüşmeciye ara inceleyerek (ayrıntılara dikkat ederek) göz atması dikkat çekmiştir”
Attitude towards interviewer ¡ The reactions the patients give to the interviewer or the interpersonal behaviours ¡ Differences can be due to cultural variances or individual differences ¡ You should ask whether this behaviour is rare, give any harm to the patient or others, compatible, due to circumstances ¡ What can be included? ¡ Answers given by the patient ¡ How they are given (direct, delayed, indirect, etc. ) ¡ Tone of voice ¡ Eye contact ¡ Posture
¡ Some of the adjectives that can be used to define these attitudes angry, cooperative, hostile, inpatient, uninterested, manipulative, open, passive, seductive, skeptical, pessimistic, etc. ¡ “Efe Bey’in görüşme esnasında göz kontağı kurmadığı, sorulan soruları direkt cevap vermek yerine orada bulunmasının onun istemediği bir durum olduğunu “Zaten buraya gelmem de ablamın isteğiyle oldu. ” cümlesiyle belirtmiştir. Bu, görüşme esnasında pasif olduğuna işaret etmektedir. Koltuğa yayılarak oturmuş olması görüşmeyle ilgisiz olduğunu göstermektedir. Zaman zaman bacağını sallaması, birkaç defa “Bitti mi? ” diye sorması sabırsız olduğunu göstermektedir. ”
Consciousness ¡ If your patient is under vegetative state, this means s/he is unconscious ¡ Consciousness has its levels to being unconscious ¡ Clouding of (cloudy) consciousness: Lack of full consciousness. Sensorial stimulus cannot create an exact perception. Orientation, attention and perception is damaged. There is psychomotor retardation, reactions are slowed down, cognition is confused. It is common in organic brain syndromes/disorders ¡ Delirium: Fear and hallucinations are basic factors. The patient is confused, anxious, restless, agitated; orientation is damaged. The patient can fee that s/he lives in a dream. Delusions can be observed. The table is wavy, can change within hours/days. The most common reasons substance, drug intoxication; metabolic disorders (diabetes); organic brain syndrome; secondary development due to sudden quit of alcohol
¡ Stupor: Being almost unconscious. The patient cannot react or develop any awareness. The patient is mutated, akinetic but still conscious, reflexes are normal; eyes are open, can follow the visual stimulus; if it is closed, shows resistance to open them; can remember the memories from stupor state ¡ Coma: The most severe state of stupor. The patient is unconscious, cannot show any voluntary actions. The most common reasons diabetic coma, head trauma, uremic coma, acute alcoholism, opiates, etc.
Orientation ¡ It is aimed to evaluate whether the patient has an awareness about their state. ¡ We try to evaluate basic cognitive functioning ¡ Our basic questions to measure orientation are who, where, when. ¡ If the patient shows resistance to answer, changes to topic and if the other clinical observations support, this means that the patient has disorientation ¡ You can vary the questions according to the patient’s level of intelligence, education, cultural background ¡ If the patient starts to show disorientation signs, s/he will first lose time, then place and then person awareness ¡ Before you start asking these orientation questions, use a swing question at the beginning
¡ “Adınız nedir? ” ¡ “Şu anda neredeyiz? ” ¡ “Bugün günlerden ne? ” ¡ “Eviniz hangi ilçede? ” ¡ “Şu anki cumhurbaşkanımızın adı nedir? ” ¡ “Doktorunuzun adı nedir? ” ¡ “Odanız hangi katta? Kaç numaralı oda? ” ¡ “Bugün öğlen yemeğini kaçta yediniz? ” ¡ “Refakatçinizin adı nedir? ” ¡ “Şu an kaçıncı kattayız? ” ¡ “Hangi mevsimdeyiz? ” ¡ “Buraya geleli kaç gün oldu? ”
¡You can use these words while reporting consciousness and orientation conscious, confused, blurry, unconscious, coma ¡“Melisa Hanım uyanık (concsious); kişi, zaman, yer yönelimi yerinde. ” ¡“Alp Bey’in bilinci karışık; kişi ve yer yönelimi yerinde (Ox 2). Zamanı tanımlayamamıştır. ”
Memory ¡ It has 3 components working memory, short term memory, long term memory ¡ How do we measure memory? ¡ “Size birazdan 3 kelime söyleyeceğim. Dikkatlice dinleyin. Ben bitirdikten sonra tekrarlamanızı isteyeceğim. Tabak. . Elma. . Okul. . ” working memory ¡ “ 100’den geriye doğru 7şer çıkartarak sayın, ben dur deyince durabilirsiniz. ” attention (can be number sequence), “Bana torunlarınızın ismini sayabilir misiniz? ” orientation, drawing a clock any possible brain damage. ¡ All of these are also destructions, lasts 3 – 5 minutes ¡ “Az önce size 3 kelime söylemiştim, hatırlıyor musunuz? Bana tekrar edebilir misiniz? ” short term memory ¡ “Bana ilkokulda yaşamış olduğunuz bir anınızı anlatabilir misiniz? ”, “Evlilik tarihinizi hatırlıyor musunuz? ”, “Üniversiteye hangi yıl girdiniz? ”, “Doğduğunuz tarihte başbakan kimdi? ” long term memory
¡“İlhami Bey söylenen 3 kelimenin tamamını tekrarlayabilmiştir. Bu anlık belleğinin çalıştığını göstermektedir. Sayıları geriye doğru sayarken yalnızca iki işlem yapabilmiş ve ‘Zaten matematikte hiç iyi olmadım ki…’ diyerek bu alandaki yetersizliğini kabul etmiştir. Bu performansı İlhami Bey’in dikkatinin bozuk olduğunu göstermektedir. Kelimelerden tabak ve okulu hatırlamış olan İlhami Bey, kısa süreli bellek testinde de yeterli performans gösterememiştir. Uzun süreli bellek testinde verdiği cevapların doğruluğu eşi tarafından onaylanmıştır. ”
¡ Confabulation: Making up or distorting stories. It can happen during calling the memories back from long term memory. Memories should be verified by a relative/parent/partner. ¡ It can happen if the patient feels under pressure to remember the certain details try not to force your patient for answers, s/he may try to give the answers you would like to hear ¡ If you are suspicious about confabulation, ask more objective questions that you can test its objectivity ¡ Mostly the patients with organic brain syndrome, head trauma, depression can show memory deficiency and confabulation
¡Amnesia: Loss of memory – remembering past experiences partially or not remembering at all ¡Fugue: It is mainly dissociation. Forgetting about the past and suddenly leaving home/office. Personal identity is confused or a new identity is adopted. After becoming conscious, s/he does not remember the things happened during the fugue stage.
Attention and Concentration ¡ Focusing on some of the parts of a story, maintaining the focus, the effort spent to focus on a part of a story ¡ You can ask your patient “Bana d harfi ile başlayan 5 kelime söyleyebilir misiniz? ”, “ 100’den geriye 3 er sayar mısınız? ”, “Kitap kelimesinin harflerini sondan başa söyleyebilir misiniz? ” ¡ Distractability: The patient is not able to focus on a task, a little stimulus/distractor may cause loss of concentration ¡ Hypervigilance: Focusing on all of the inner and outer stimulus at the same time ¡ Selective inattention: Ignoring the stimulus that may create anxiety
¡“Melis Hanım’dan görüşme esnasında 100’den geriye 3 er sayması istenmiştir. 5 işlem yaptıktan sonra aniden duran ve çok acıktığını, koridorda bir çocuğun ağladığını söyleyen Melis Hanım’a devam etmesi söylendiğinde verilen görevi unutmuş ve tekrarlanmasını istemiştir. Bu, Melis Hanım’da distraktibilite ve hipervijilans olduğuna işaret etmektedir. ”
Perception ¡Perception includes two factors hallucinations and illusions ¡Hallucinations are false sensory experiences, it can appear in all of our 5 sensory organs. Most common one is auditory hallucinations. ¡Hallucinations mostly appear in patients with schizophrenia, chemical intoxication and acute traumatic stress ¡You should be very skeptical while questioning these areas
¡ “Size bazı sorular soracağım. Bunlar belki alışılmamış, tuhaf durumlar olabilir sizin için. Aynı zamanda yaşadığınız durumlarla çok da benzerlik gösterebilir. Zaman zaman televizyondan, sosyal medyadan size yönelik konuşuluyor ya da sizi hedef alarak paylaşımlar yapılıyor gibi düşünceleriniz oldu mu? ” ¡ “Peki bu size mesaj veren ses/TV programcısı ne demeye çalışıyordu size? ”, “Bu konuşan bir kadın mı? ”, “Siz bu konuşan kişiyi tanıyor musunuz? ”, “Her zaman aynı ses mi yoksa sesler değişiklik gösteriyor mu? ”, “Ne kadar zamandır size konuşuyor? ” ¡ “Hepimizin başına zaman gelmiştir, belli bir şarkıya, kokuya, yemeğe takılıp sürekli onu deneyimlemek isteriz. Merak ediyorum, sizin de oldu mu böyle takıldıklarınız? ”, “Ne süreyle bunu tekrarlayan biçimde yaptınız? ”
¡ Depersonalization: The patient watches him/herself from an outer world. It is common in depression, dissociation, schizophrenia, schizoid personality disorder ¡ Derealization: The outer world seems too weird, unreal. It is common in schizophrenia ¡ “Onur Bey algıyla ilgili sorular sorulduğuda görsel ve işitsel hallüsinasyonlardan bahsetmiştir. İşitsel hallüsinasyonlarının yaklaşık 5 yıldır olduğunu, görsel hallüsinasyonlarınsa yakın bir zamanda oluştuğunu söylemiştir. Hallüsinasyonları ile ilgili içgörüsü olan Onur Bey, onlardan kurtulmak için duşa 3 kez girip çıktığını ve duşta şarkı söylediğini, böylece hallüsinasyonları kovmaya çalıştığını söylemiştir. ”
Cognition and Speech ¡ While interviewing, you should observe your patient’s cognitive processes and content of the cognitions. ¡ Speech: You should define in terms of pace, tone of voice and the amount. The definition should be based on non – directed speech. You can define speech as spontaneous, speech deprivation, delayed. ¡ “Demet Hanım, konuşması hızlı, ses tonu yüksek ve konuşma miktarı fazladır. ” ¡ “Murat Bey konuşma azlığı yaşamaktadır, sesinin duyulması zor ve konuşması yavaştır. ” ¡ Cognitive Process: It is related to HOW the patient expresses him/herself. Is it logical and structured? Can they answer the questions? ¡ Circumstantiality (Ayrıntıcılık): The patient cannot answer the questions directly. S/he gives too detailed information about the questions that is not able to get to the main point. You can understand this if you need to interrupt your patient too much during the session.
¡ Compressed speech (Basınçlı konuşma): The patient talks too much and too fast with a loud tone of voice. Even if nobody listens to and you try to interrupt, s/he continues his/her speech. You need to be careful about the tone, the amount and the appropriateness of the speech. It is peculiar to manic episode. ¡ Blocs: While the patient is talking, suddenly s/he cuts the speech, blocs and cannot remember what s/he is talking about. It is common in schizophrenia. ¡ Distractible speech: While the patient is talking, suddenly s/he stops, some other object/voice/etc. distracts and talks about it.
¡ Perseveration: The patient is obsessed with a special word and repeats it over again even if you asked another question. It is common in schizophrenia and dementia. ¡ Incoherence (Enkoherans): It is also said “word salad”. The patient says meaningless words sequentially that no one understands. It is peculiar to schizophrenia. ¡ Cognition fuzziness (Fikir uçuşması): One cognition triggers another cognition which is generally not related/a little related to the previous one. Patients generally report this as “Düşüncelerim konuşmama yetişmiyor. ” It is peculiar to acute manic episode.
¡ Cognitive Content: It points to the special meanings of the speech/cognition. ¡ You should be aware of the hallucinations, delusions, phobias, obsessions, suicide and homicide thoughts, etc. ¡ Delusions (Hezeyan): Distorted cognitions, they are disengaged cognitions from the reality, cannot be based on objective evidence. If it is a delusion, then you cannot explain it by cultural, religious, educational background. ¡ Phobias: A special thing, situation or event that creates excessive amount of fear that leads to quitting/avoiding behaviours ¡ Hypochondriasis: Without having an organic pathology, the patient processes some sensory perceptions as harmful/life-threatening/abnormal. S/he thinks that there is a serious medical conditions. ¡ Obsessions: They are repetitive, disturbing cognitions and images that comes up to the mind. The patients generally report this as meaningless but they cannot resist that cognition/image which leads them to engage in compulsive or avoiding behaviours.
Affect / Mood ¡ Affect (duygulanım) is the emotions that are experienced during the interview which can be observed by the interviewer. Happiness, upset, unhappiness, joy, fear, anger are the common affects. ¡ You should be careful about these while evaluating the affect: ¡ The range of the affect (olağan, kısıtlı) ¡ The intensity of the affect (yoğun, donuk/tekdüze, künt) ¡ The stability of the affect (tutarlı, değişken) ¡ The coherence of the affect (duruma ve içeriğe uygunluğu)
¡ Mood (duygudurum) is about how the patient perceives the world generally. Most common moods are depression, anxiety, anger. ¡ To differentiate affect from mood: If the affect is the weather of the day, mood is the season ¡ Alexithymia: The patient is not aware of the mood, has difficulty to define them or cannot define them at all ¡ Anhedonia: The patient has no interest in the activities that are used to give pleasure. Even if s/he engages in activities, there is no enjoyment. It is common in depression and schizophrenia ¡ Dysphoria: The patient defines his/her mood in terms of unhappiness, anxiety, irritability, hopelessness, tense ¡ Euphoria: Exaggerated, incompatibly cheerful mood. The mood is not compatible with the objective circumstances. It is common in manic episodes. It can also be seen in the usage of toxic substances ¡ Eutimic: Usual mood – not dysphoric, not euphoric
Behaviour ¡ Agiatation: Increased motor activation due to inner tension. The activation is repetitive and is not directed to a special goal. Walking around, restlessness are the common factors. ¡ Impulsive behaviours: Without thinking and foreseeing the probable outcomes, only getting into the action ¡ Acting – out behaviours: Unconscious wills are told by actions but the patient is not aware of these acting – out behaviours ¡ Compulsions: The reactions to the obsessions that the patient should follow the rules very strictly. It aims to decrease the anxiety that the obsessions create
Insight ¡ Very generally and basically it means whether the patient understands him/herself and the openness to understanding ¡ It is expected them to understand the underlying reasons of the problems ¡ If the patient is lack of insight, they say that they have no problems that lead them to an inpatient hospital or to a therapist ¡ Partial insight: The patient is aware of the every day problems and how it affects his/her life but their motivation change according to their everyday mood. You need to lead them to the “real goals”