MENTAL HEALTH UNIT III CHILDHOOD MENTAL HEALTH PROBLEMS

MENTAL HEALTH UNIT III
CHILDHOOD MENTAL HEALTH PROBLEMS • Attention deficit hyperactivity – Needs structured environment with consistent limits • Family education • Special education in school • Drug therapy – Ritalin – Concerta – Adderall
CHILDHOOD MENTAL HEALTH PROBLEMS • Behavioral or conduct disorders: persistent pattern of unacceptable behaviors – Defiant of authority – Aggressive – Refuse to follow society’s rules or norms • Focus on stable environment & consistent enforced limitations
CHILDHOOD MENTAL HEALTH PROBLEMS • Oppositional defiant disorder: recurring pattern of disobedient, hostile behavior toward authority figures – Lose tempers with adults – Argue with adults – Deliberately annoy adults – Refuse to compromise – Blame others & test limits • Family therapy with limit setting & consistency
NORMAL MENTAL CHANGES IN OLDER ADULTS • See page 180, Table 16 -1
LATE ADULTHOOD PROBLEMS RELATED TO MENTAL HEALTH • Vulnerability, abuse, memory loss, dementia, & Alzheimer’s Disease (AD) • Physical or biochemical disorders • Loneliness & social isolation
ELDER ABUSE Any action that takes advantage of an older person, their emotional well-being, or property • Domestic • Institutional • Self-abuse
DEPRESSION • Common mental health disorder of late adulthood • Retirement, lifestyle changes, losses per death • Mask dementia • Medications • Effective therapies – Individual & group therapy – Reminiscing – Antidepressants (SSRI’s)
DEMENTIA Loss of multiple abilities: short –term / longterm memory, language, ability to think & understand • Memory loss: inability to recall a certain detail or event • Delirium: change of consciousness that occurs over short period of time
• Sundown syndrome: group of behaviors characterized by confusion, agitation & disruptive actions • Unknown cause • Visual cues & social interactions decrease with the onset of nighttime = confused, irritable, agitated
ALZHEIMER’S DISEASE • Progressive, degenerative disorder affecting brain cells = impaired memory, thinking, & behavior • Diagnosis; rule out all other possibilities • Incidence increases with age • Can progresses slowly • Cognitive abilities lose • Can’t recall recent events or process new information
ALZHEIMER’S DISEASE • Increasingly forgetful; personality changes – Aphasia: loss of language – Apraxia: loss of the ability to perform everyday activities – Visual agnosia: loss of recognition of previously known or familiar people & objects
ALZHEIMER’S DISEASE • Affective losses: loss of their personality • Stress & anger ↑ fatigue levels • Minor anxieties become full catastrophic reactions = ↑ confusion, agitation, & fear • Wander, Noisy, act compulsively or behave violently
ALZHEIMER’S DISEASE • • Low stimuli environment Eliminate stress provoking situations Physical & emotional support Medications to slow the disease (pg 197 Table 17 -3) (pg 199, common cholinesterase inhibitors)
ALZHEIMER’S DISEASE • Goals to therapeutic care – Provide safety & well-being – Manage behaviors therapeutically – Provide support for family, relatives, & caregivers • Tables 17 -1, 17 -2 • Boxes 17 - 4, 5, 6, 7 • Table 17 -4, 17 -5
PSYCHOTHERAPEUTIC MEDICATION EFFECT • Interrupts chemical messenger pathways in the brain • Act in/around the synapse - alters flow of neurotransmitters
ANXIETY • Uneasiness, uncertainty, & helplessness • State of tension sometimes associated with feeling of dread or doom • Normal emotional response to a threat or stressor • Part of survival & growth
ANXIETY PURPOSES • Warning • Increase learning – help with concentration & focus • Motivate
ANXIETY DISORDERS • Anxiety expressed ineffectively, coping mechanisms do not relieve the stress • 6 categories per DSM-IV-TR
GENERALIZED ANXIETY • Broad, long-lasting, excessive • Disturbance in emotional area of functioning eventually affects every aspect • Worried, anxious more times than not • Fret about numerous things • Difficult to control worries • Cannot complete simple tasks & responses way off base in relationship to actual situation
PANIC DISORDER • Brief period of intense fear or discomfort • Usually last 1 – 15 minutes with peak after 10 minutes • 2 types – Those associated with agoraphobia: anxiety about possible situations in which a panic attack may occur (public situations) – Those not associated with agoraphobia
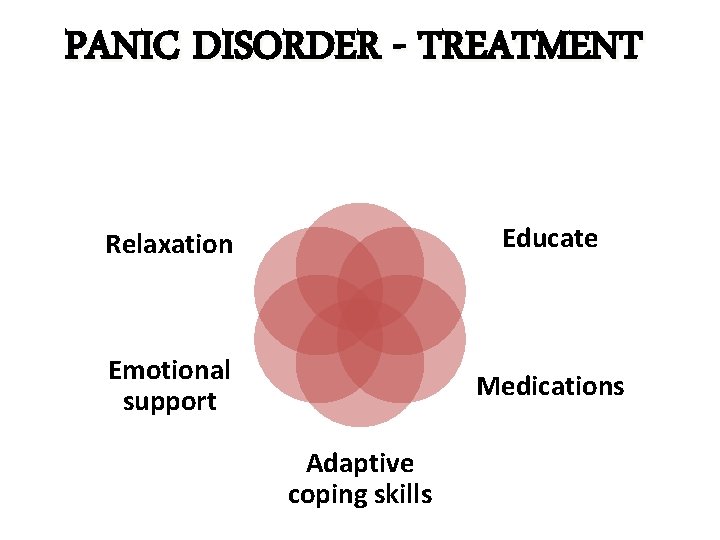
PANIC DISORDER - TREATMENT Relaxation Educate Emotional support Medications Adaptive coping skills
PHOBIC DISORDER • Unnatural, obsessive fear • Dwell on object of fear almost to point of fascination • Immobilizes
OBSESSIVE-COMPULSIVE DISORDER (OCD) • OBSESSION: Distressing, persistent, recurring, inappropriate thought • COMPULSION: specific behaviors that must be performed to reduce anxiety
OBSESSIVE – COMPULSIVE DISORDER • Cleanliness, dirt & germs; aggression & sexual impulses; health concerns; safety concerns, order & symmetry • Thoughts, doubts, fears, images or impulses • Defense mechanism of repression • Focus anxieties into compulsive actions & engage in undoing behaviors to relieve stress • Know behaviors are maladaptive but cannot stop • Treated with behavioral therapy & antidepressants
BEHAVIORAL ADDICTIONS • Obsessive-compulsive activities taking on certain forms of addictive behaviors • Gambling, shopping, working, excessive sexual activity • Destruct personal & professional lives
POSTTRAUMATIC STRESS DISORDER (PTSD) • Reliving of traumatic event or situation • Traumatic experience resulted in intense fear, horror, or helplessness • Flashbacks • Assure safety & reorientation • Meds, psychological therapy & emotional support
ANXIETY INTERVENTIONS Prevent Detect & treat early Antianxiety agents Systematic desensitization – learn to cope with 1 anxiety situation at a time • Flooding – rapidly or repeatedly exposing client to the feared object or situation; phobias • Rational-emotive therapy – learn how their illogical thinking leads to maladaptive behaviors • Relaxation – deep breathing • •
ANTIANXIETY MEDS Reduce psychic tension of stress • Benzodiazepines (drug of choice) - Decrease anxiety but also can provide sedation, induce sleep, prevent seizures, prepare clients for general anesthesia - Act by ↑ GABA neurotransmitter level - Onset 1 hr. & duration of 4 – 6 hrs. - Side effects are fatigue, sedation, dizziness & orthostatic hypotension; may experience diarrhea during withdrawal - Dependence can result = limited use; prn basis See page 214 Table 18 -3 for nursing actions • Nonbenzodiazepines - Antihistamines - Barbiturates
MOOD DISORDER Disturbance in emotional dimension of human functioning Maladaptive when interferes with effective living Mania to depression
DEPRESSION • Whole body illness • Last few days or several years; several levels • MILD: short lived, triggered by life events or situations; usually self limiting • MODERATE: persists over time; interfere with ADL’s – – Fatigue, eating & sleeping difficulties Anhedonia: inability to enjoy life Impaired judgment & decision making Higher risk of suicide
DEPRESSION • MAJOR DEPRESSIVE EPISODE: severe depression lasting ≥ 2 weeks (familial) - Feelings of worthlessness, guilt, despair - Suicidal thoughts begin - When episodes routinely repeat itself for ≥ 2 yrs. = MAJOR DEPRESSIVE DISORDER • DYSTHYMIC DISORDER: daily moderate depression lasting ≥ 2 yrs - Chronically sad, self critical - See self as incapable & uninteresting - See world from a negative point of view - Can carry out ADL’s but unable to enjoy them
BIPOLAR DISORDERS • • Sudden, dramatic shift in emotional responses Time intervals vary Behaviors build in intensity during mania If untreated, manic stage can lasts 3 months when depressive stage steps in
BIPOLAR DISORDERS • BIPOLAR I – Episodes of depression alternating with mania episodes – More severe & incapacitating – Delusions & hallucinations occur during mania • BIPOLAR II – 1 -2 weeks of severe lethargy, withdrawal followed by days of elevated/irritable mood, constant activity & risky decision making – May not be as severe as Bipolar I but still devastating
Bipolar Disorder • Cyclothymic disorder: repeated mood swings alternating between hypomania & depression • No periods of “normal” functioning • Usually leads into full blown bipolar disorders
MOOD DISORDERS TREATMENT – Acute: 6 -12 wks • Reduce symptoms & inappropriate behaviors • Inpatient hospitalization may be required • Medications – Continuation: 4 -9 months • Outpatient basis • Medication management • Psychotherapy – Maintenance • Preventing recurrences • Maintenance meds & psychotherapy • Current standard treatments…
MEDICATION CLASSES & CATEGORIES • ANTIDEPRESSANTS – Seritonin Specific Reuptake Inhibitors (SSRI) – Tricyclic Antidepressants (TCA) – Monoamine Oxidase Inhibitors (MAOI’s) • ANTIMANICS – Antimanics – Anticonvulsants • ANTIPSYCHOTICS – Phenothiazines – Nonphenothiazines
ANTIDEPRESSANTS • • ↑ certain neurotransmitter activities 1 -2 weeks before symptom relief Side effects may be noticed soon after starting Monitor closely for ↑ energy when suicidal
ANTIMANICS • Lithium – natural occurring salt • • • Drug of choice for treatment bipolar disorder Pre lithium workup Educate Monitor side effects & toxic reactions Minimal difference therapeutic & toxic levels – too low = mania returns – too high (≥ 1. 5 m. Eq/L) = uncomfortable & life threatening side effects may occur Positive effects may take 3 weeks
ANTIPSYCHOTICS • Referred to as major tranquilizers or neuroleptics • Most treat symptoms of major mental disorders • Numerous & troublesome side effects & adverse reactions
EXTRAPYRAMIDAL SIDE EFFECTS • CNS side effects of abnormal movements produced by imbalance of neurotransmitters in brain • PNS side effects: dry mouth, blurred vision, & photophobia • 1 st few weeks orthostatic hypotension possible
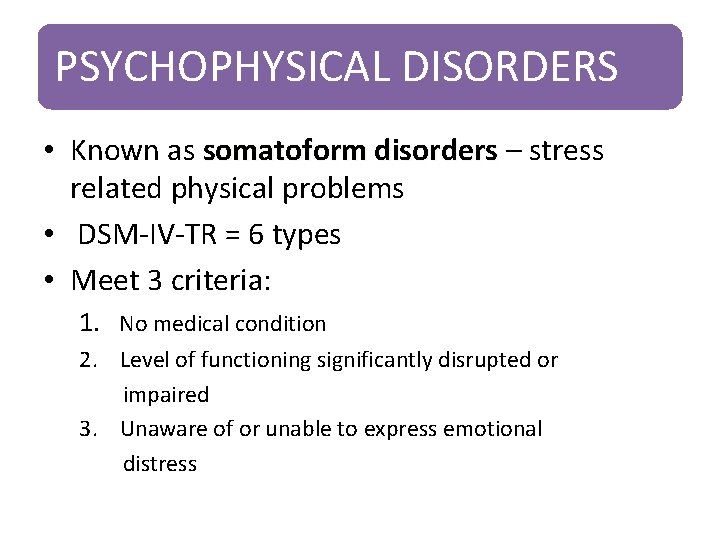
PSYCHOPHYSICAL DISORDERS • Known as somatoform disorders – stress related physical problems • DSM-IV-TR = 6 types • Meet 3 criteria: 1. No medical condition 2. Level of functioning significantly disrupted or impaired 3. Unaware of or unable to express emotional distress
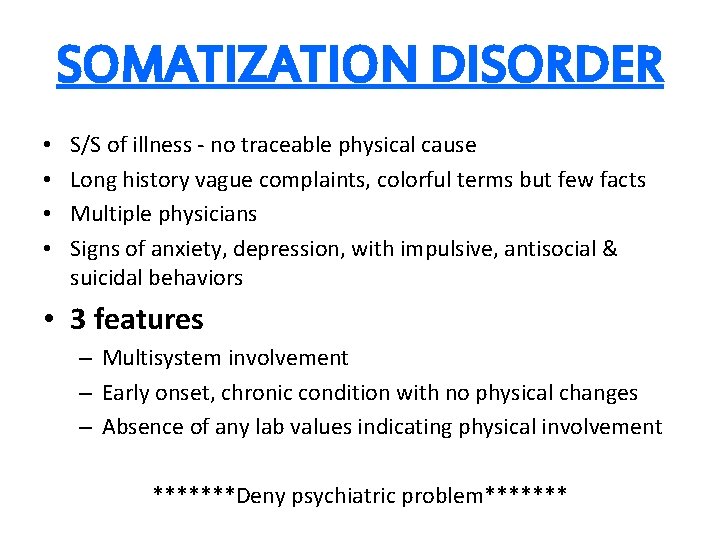
SOMATIZATION DISORDER • • S/S of illness - no traceable physical cause Long history vague complaints, colorful terms but few facts Multiple physicians Signs of anxiety, depression, with impulsive, antisocial & suicidal behaviors • 3 features – Multisystem involvement – Early onset, chronic condition with no physical changes – Absence of any lab values indicating physical involvement *******Deny psychiatric problem*******
CONVERSION DISORDER Sensory or Motor functions Result from emotional conflict ? Treatment: • Eliminate any physical causes • Identify conflicts responsible for S/S
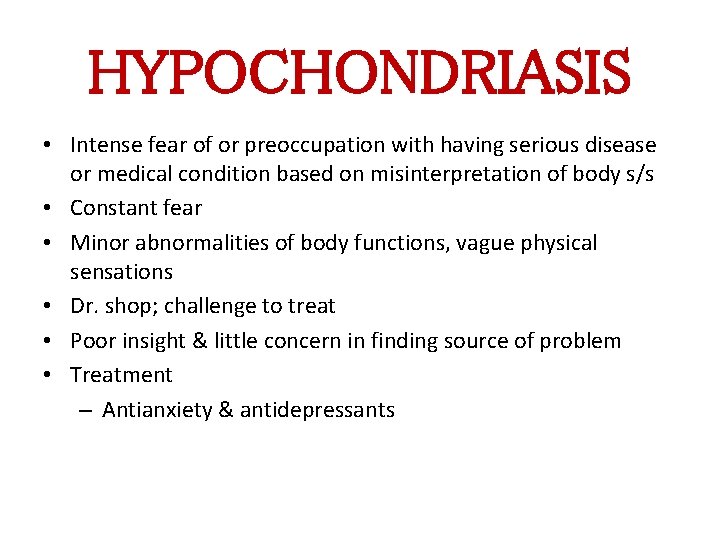
HYPOCHONDRIASIS • Intense fear of or preoccupation with having serious disease or medical condition based on misinterpretation of body s/s • Constant fear • Minor abnormalities of body functions, vague physical sensations • Dr. shop; challenge to treat • Poor insight & little concern in finding source of problem • Treatment – Antianxiety & antidepressants
SOMATOFORM PAIN DISORDER • Pain / discomfort major focus of distress • No other cause of pain identified • Treatment: Pain clinic
BODY DYSMORPHIC DISORDER • Preoccupation with perceived physical difference or defect in one’s body • Describe distress as tormenting, devastating, or intensely painful • Describe self as ugly, unacceptable & often avoid work, social or public gathering
FACTITIOUS & MALINGERING • Symptoms intentionally produced – Factitious = to assume the sick role – Malingering = to meet a goal – Factitious disorder by proxy = deliberate production of s/s in another person; usually mother to child (Munchausen's syndrome) • Rarely diagnosed, move Dr. to Dr. • Identify & treat underlying cause
DISSOCIATIVE DISORDERS Dissociation: interruption of fundamental aspect of waking consciousness – Normal common experience (daydreaming) – Coping mechanism to protect from trauma – Children dissociate more easily than adults & if used as defense mechanism can grow into dissociative disorder • Disturbance in the normally interacting functions of consciousness – Identity, Memory, Perception • Most anxiety producing aspect of self walled off from rest of personality in attempt to cope • DSM-IV-TR = 4 types
DEPERSONALIZATION • Feeling detached or unconnected to self • Response to severe anxiety associated with blocking of awareness & a fading of reality • Defense mechanism but not relieve the cause of stress = maladaptive behavior = attempt to escape distress & anxiety; lose identity
DISSOCIATIVE AMNESIA • Inability to remember personal information • Cant be explained by ordinary forgetfulness • Attempt to avoid extreme stress by blocking memories from consciousness • Gaps in ability to recall certain events • Sights, sounds, odors, images may trigger emotional distress • Actual memories too painful so stay submerged but still inflict pain • Need high level of support • Primary concern = safety d/t suicide attempts
DISSOCIATIVE FUGUE • Sudden, unexpected travel with an inability to recall the past; response to overwhelming stressful or traumatic event • Extreme expression of fight or flight • New identity, occupation, significant others • Return to prefugue state, – Experience aggressive impulses, conflict, depression, guilt, suicidal wishes • Recovery – Psychosocial care – Emotional support
DISSOCIATIVE IDENTITY DISORDER • 2 or more personalities, take control of behavior • Defense mechanism against trauma • Time losses, unexplained possessions or changes in relationships, out of body experiences • Each personality unique • All serve a protective purpose
DISSOCIATIVE IDENTITY DISORDER • • Primary personality = HOST All other personalities = ALTERS Transition usually sudden & r/t stress Sometimes cooperate but more often will struggle
DISSOCIATIVE IDENTITY DISORDER • Main treatment goal – Integrate personalities into 1 functional individual, cope with stresses in a healthy manner • Stages of treatment – Assessment – Stabilization – Reworking past traumas • Based on symptoms • Short term use of antianxiety, antidepressants, antipsychotics; encourage coping skills to develop
- Slides: 55