Mental Health Integration Diagram Interactive version DRAFT 00731
- Slides: 16
Mental Health Integration Diagram *Interactive version (DRAFT 007/31. 09. 10: DT/QIS) For further information please contact: David Thomson NHS Quality Improvement Scotland. Mental Health Projects Manager, Directorate of Implementation, Improvement and Support & National ICP Coordinator, Patient Safety and Performance Assessment Unit dthomson 2@nhs. net
Mental Health Integration Diagram *Interactive version The following presentation is a Power. Point based version of an interactive diagram which helps focus on where key drivers and work streams in mental health align, crossover and run parallel. The diagrams are generated from the developments and successful role out to mental health of ‘Releasing Time to Care’. These diagrams will evolve as services develop and progress towards excellence. This capacity for change reflects and promotes the principles of quality improvement and the necessity for on-going cycles of improvement as key. If you would like additional information to be added to the diagrams, please contact David Thomson - dthomson 2@nhs. net
Quality Infrastructure A key requirement to realise our Quality Ambitions is for our systems and actions to be integrated and aligned across the whole NHS system. We need to identify and remove any hurdles and barriers presented by the current approaches to policy development and delivery across Scottish Government and NHSScotland. (The Healthcare Quality Strategy for NHSScotland, The Scottish Government, May 2010 ) By developing diagrammatic representations of key initiatives in mental health, it is intended that promoting better comprehension of integration contributes to removing obstacles to progress and further more, encourage increased confidence from individuals and organisations from all aspects of health care to participate and contribute to service improvement.
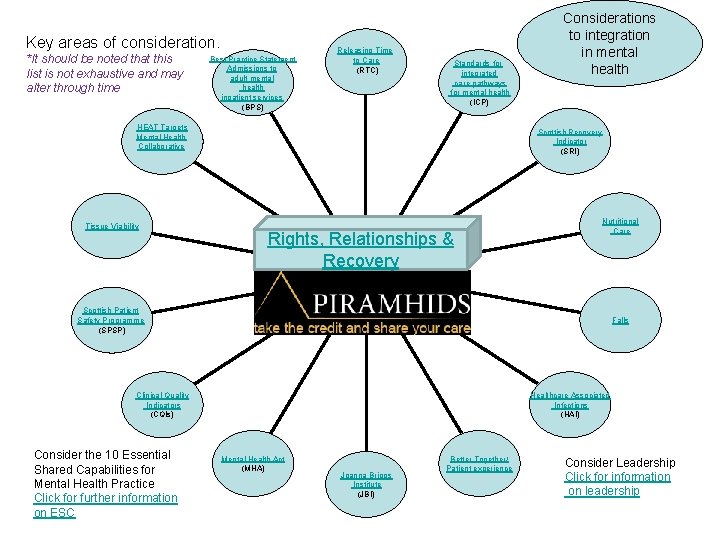
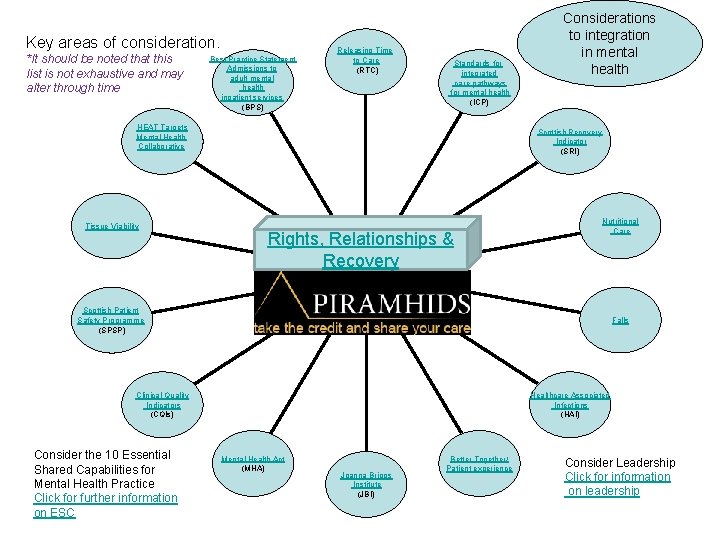
Key areas of consideration. *It should be noted that this list is not exhaustive and may alter through time Best Practice Statement Admissions to adult mental health inpatient services (BPS) Releasing Time to Care (RTC) Standards for integrated care pathways for mental health (ICP) HEAT Targets Mental Health Collaborative Tissue Viability Considerations to integration in mental health Scottish Recovery Indicator (SRI) Rights, Relationships & Recovery Nutritional Care Scottish Patient Safety Programme (SPSP) Falls Clinical Quality Indicators (CQIs) Consider the 10 Essential Shared Capabilities for Mental Health Practice Click for further information on ESC Healthcare Associated Infections (HAI) Mental Health Act (MHA) Joanna Briggs Institute (JBI) Better Together/ Patient experience Consider Leadership Click for information on leadership
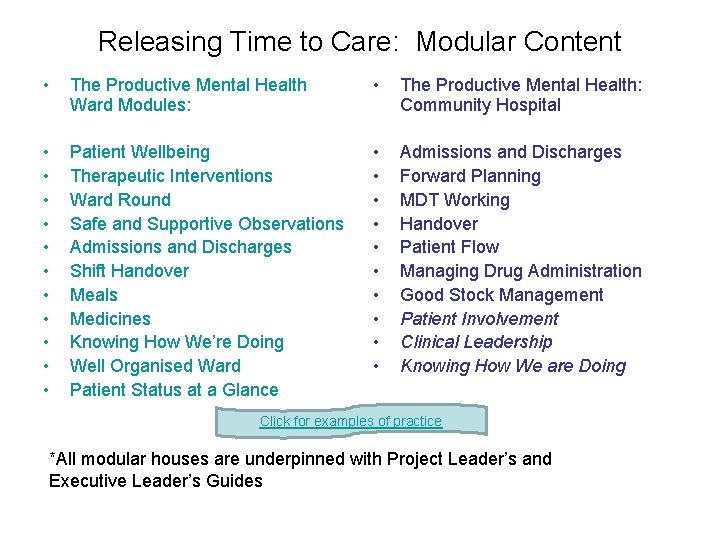
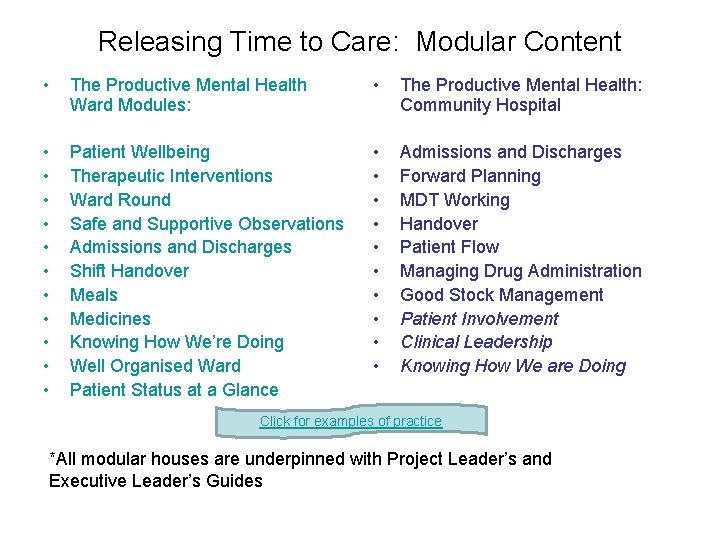
Releasing Time to Care: Modular Content • The Productive Mental Health Ward Modules: • The Productive Mental Health: Community Hospital • • • Patient Wellbeing Therapeutic Interventions Ward Round Safe and Supportive Observations Admissions and Discharges Shift Handover Meals Medicines Knowing How We’re Doing Well Organised Ward Patient Status at a Glance • • • Admissions and Discharges Forward Planning MDT Working Handover Patient Flow Managing Drug Administration Good Stock Management Patient Involvement Clinical Leadership Knowing How We are Doing Click for examples of practice *All modular houses are underpinned with Project Leader’s and Executive Leader’s Guides
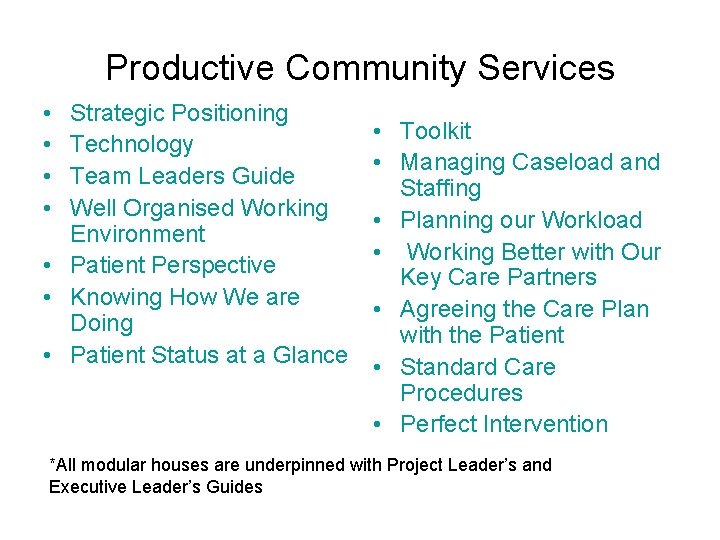
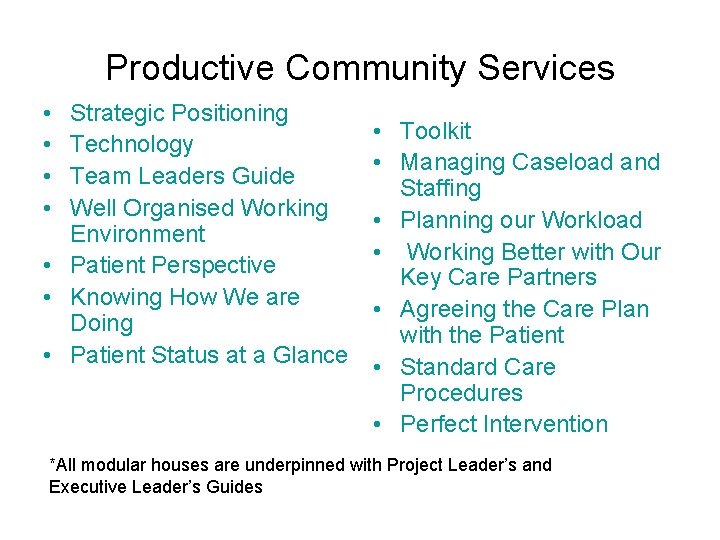
Productive Community Services • • Strategic Positioning Technology Team Leaders Guide Well Organised Working Environment • Patient Perspective • Knowing How We are Doing • Patient Status at a Glance • Toolkit • Managing Caseload and Staffing • Planning our Workload • Working Better with Our Key Care Partners • Agreeing the Care Plan with the Patient • Standard Care Procedures • Perfect Intervention *All modular houses are underpinned with Project Leader’s and Executive Leader’s Guides
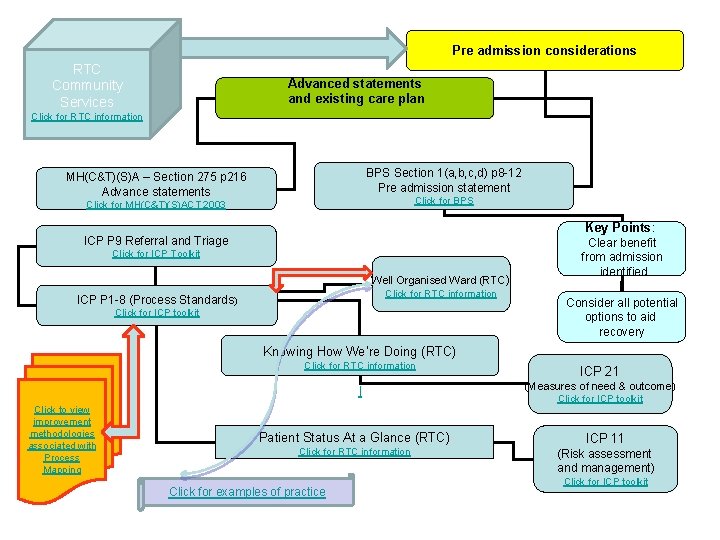
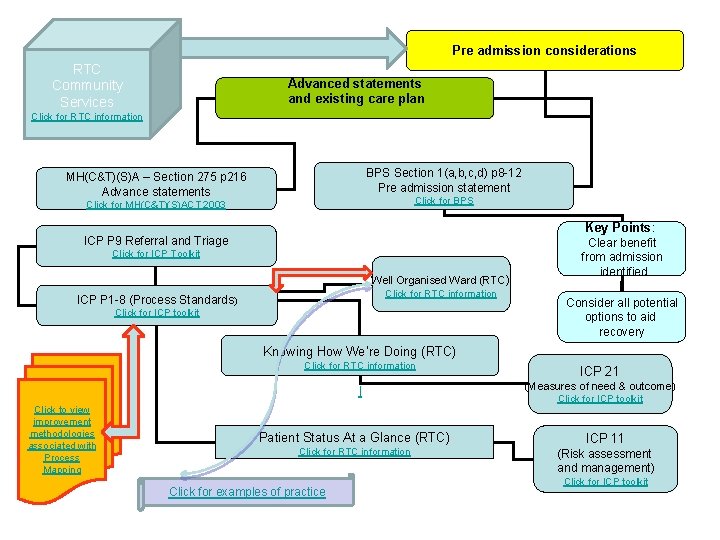
Pre admission considerations RTC Community Services Advanced statements and existing care plan Click for RTC information BPS Section 1(a, b, c, d) p 8 -12 Pre admission statement MH(C&T)(S)A – Section 275 p 216 Advance statements Click for BPS Click for MH(C&T)(S)ACT 2003 Key Points: ICP P 9 Referral and Triage Click for ICP Toolkit Well Organised Ward (RTC) Click for RTC information ICP P 1 -8 (Process Standards) Click for ICP toolkit Clear benefit from admission identified Consider all potential options to aid recovery Knowing How We’re Doing (RTC) Click to view improvement methodologies associated with Process Mapping Click for RTC information ICP 21 l (Measures of need & outcome) Patient Status At a Glance (RTC) Click for RTC information Click for examples of practice Click for ICP toolkit ICP 11 (Risk assessment and management) Click for ICP toolkit
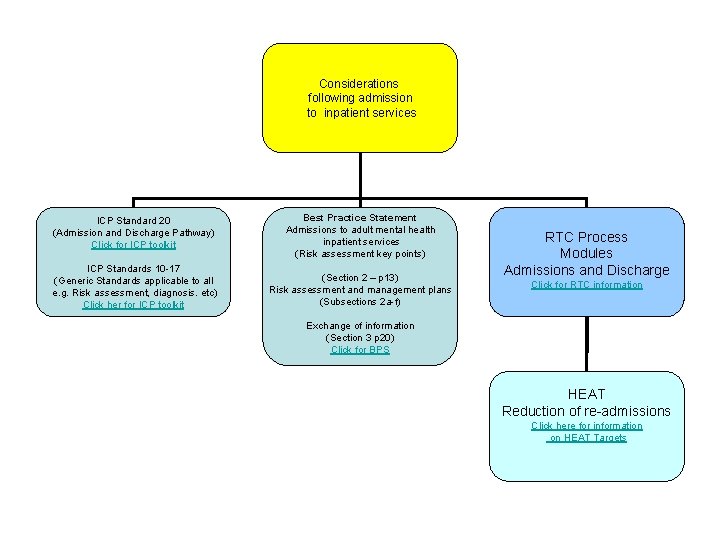
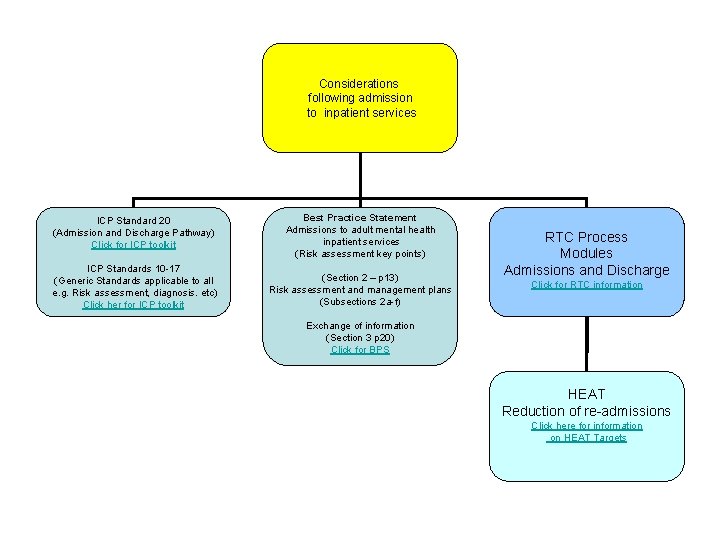
Considerations following admission to inpatient services ICP Standard 20 (Admission and Discharge Pathway) Click for ICP toolkit Best Practice Statement Admissions to adult mental health inpatient services (Risk assessment key points) ICP Standards 10 -17 (Generic Standards applicable to all e. g. Risk assessment, diagnosis. etc) Click her for ICP toolkit (Section 2 – p 13) Risk assessment and management plans (Subsections 2 a-f) RTC Process Modules Admissions and Discharge Click for RTC information Exchange of information (Section 3 p 20) Click for BPS HEAT Reduction of re-admissions Click here for information on HEAT Targets
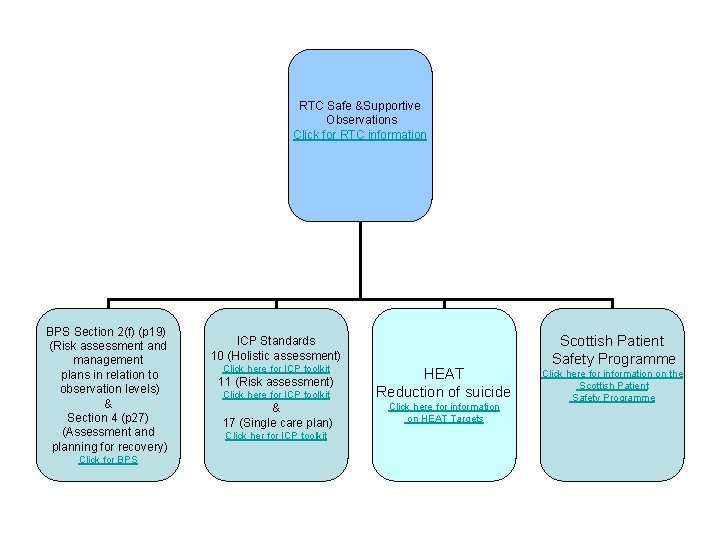
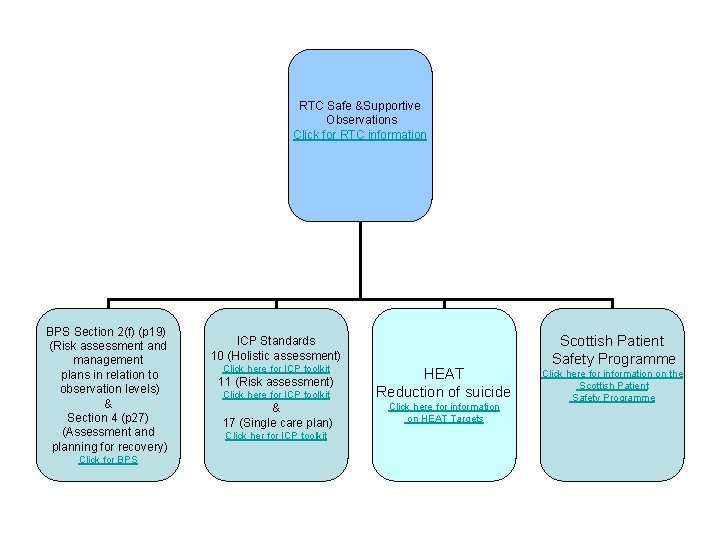
RTC Safe &Supportive Observations Click for RTC information BPS Section 2(f) (p 19) (Risk assessment and management plans in relation to observation levels) & Section 4 (p 27) (Assessment and planning for recovery) Click for BPS ICP Standards 10 (Holistic assessment) Click here for ICP toolkit HEAT Reduction of suicide & 17 (Single care plan) Click here for information on HEAT Targets 11 (Risk assessment) Click her for ICP toolkit Scottish Patient Safety Programme Click here for information on the Scottish Patient Safety Programme
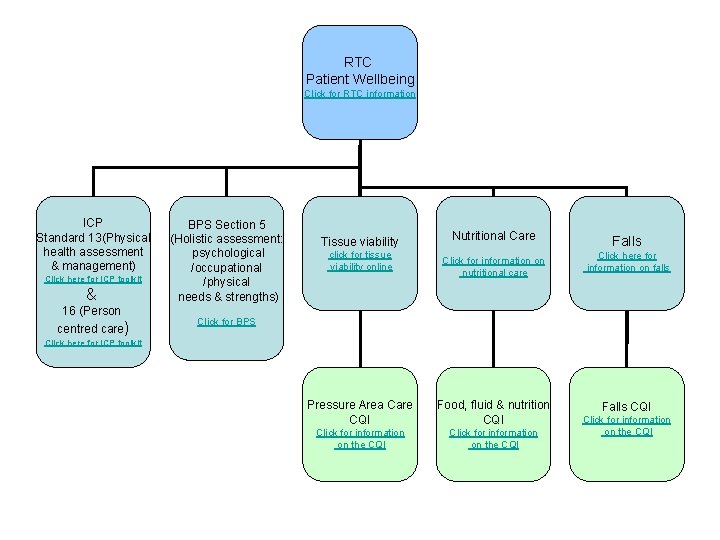
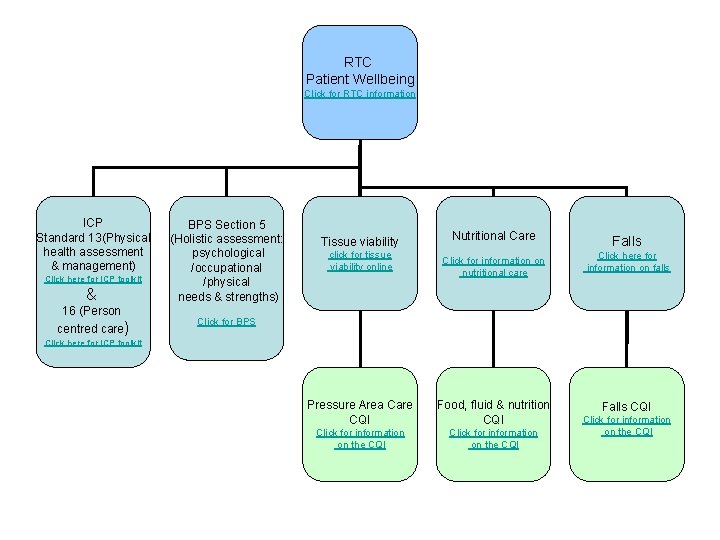
RTC Patient Wellbeing Click for RTC information ICP Standard 13(Physical health assessment & management) Click here for ICP toolkit & 16 (Person centred care) BPS Section 5 (Holistic assessment: psychological /occupational /physical needs & strengths) Tissue viability click for tissue viability online Nutritional Care Falls Click for information on nutritional care Click here for information on falls Click for BPS Click here for ICP toolkit Pressure Area Care CQI Food, fluid & nutrition CQI Click for information on the CQI Falls CQI Click for information on the CQI
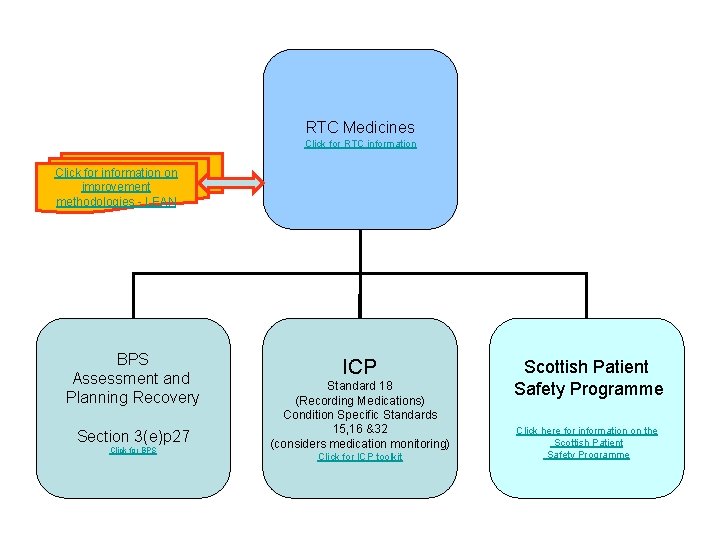
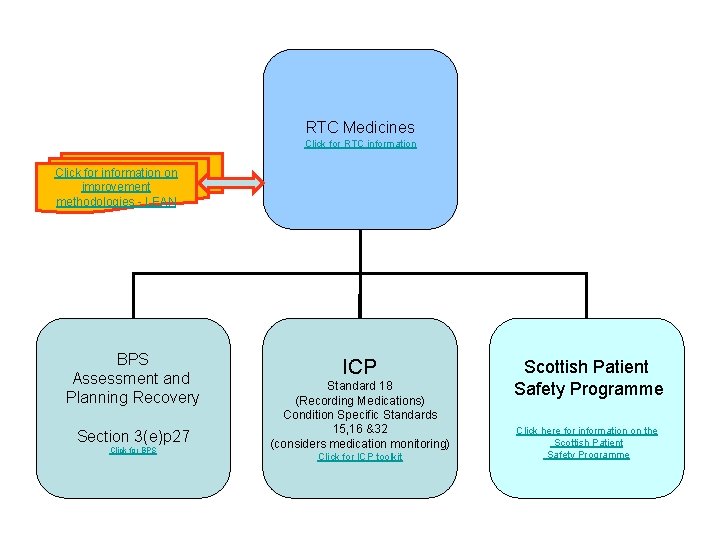
RTC Medicines Click for RTC information Click for information on improvement methodologies - LEAN BPS Assessment and Planning Recovery Section 3(e)p 27 Click for BPS ICP Standard 18 (Recording Medications) Condition Specific Standards 15, 16 &32 (considers medication monitoring) Click for ICP toolkit Scottish Patient Safety Programme Click here for information on the Scottish Patient Safety Programme
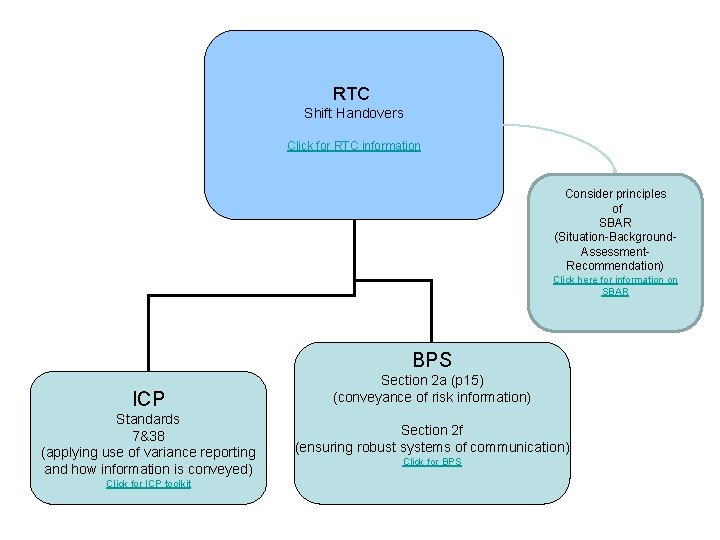
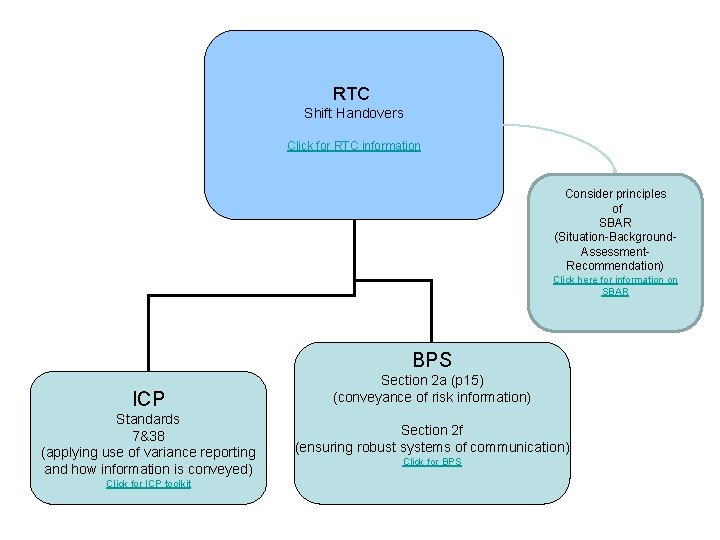
RTC Shift Handovers Click for RTC information Consider principles of SBAR (Situation-Background. Assessment. Recommendation) Click here for information on SBAR BPS ICP Standards 7&38 (applying use of variance reporting and how information is conveyed) Click for ICP toolkit Section 2 a (p 15) (conveyance of risk information) Section 2 f (ensuring robust systems of communication) Click for BPS
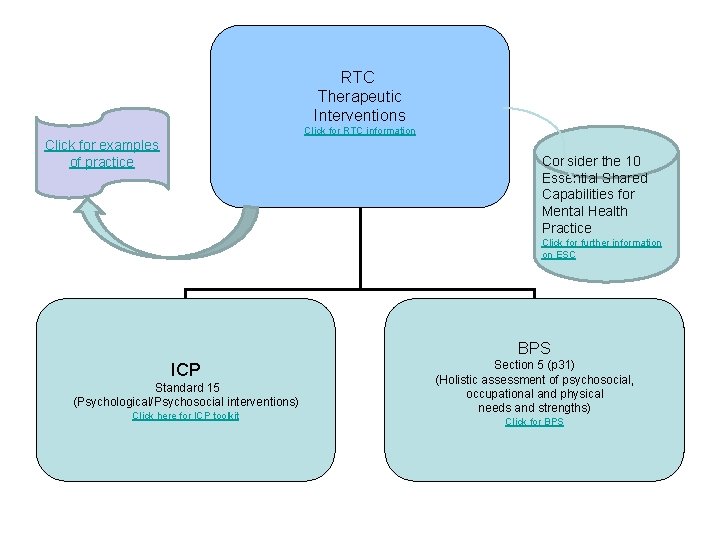
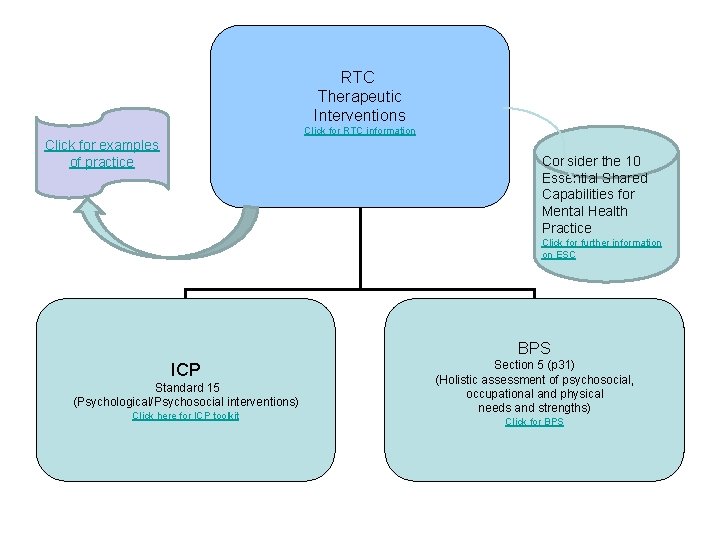
RTC Therapeutic Interventions Click for RTC information Click for examples of practice Consider the 10 Essential Shared Capabilities for Mental Health Practice Click for further information on ESC BPS ICP Standard 15 (Psychological/Psychosocial interventions) Click here for ICP toolkit Section 5 (p 31) (Holistic assessment of psychosocial, occupational and physical needs and strengths) Click for BPS
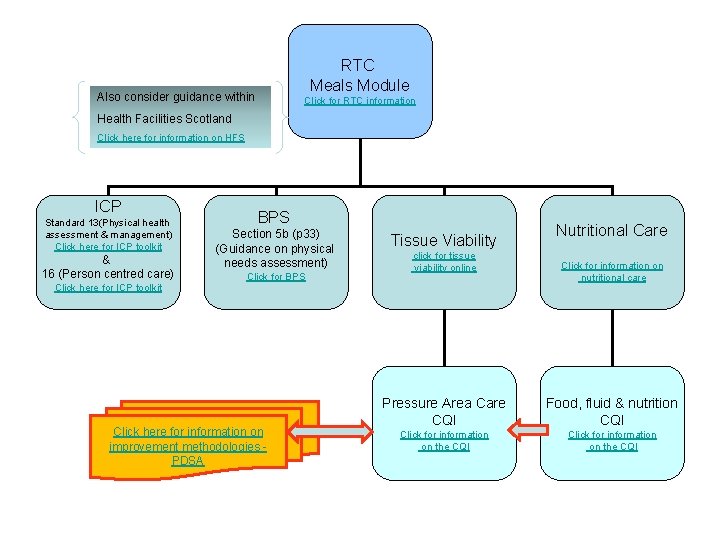
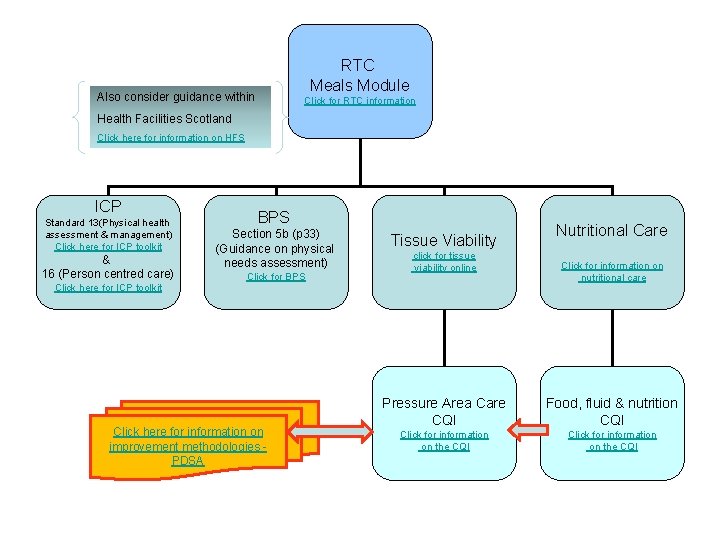
RTC Meals Module Also consider guidance within Click for RTC information Health Facilities Scotland Click here for information on HFS ICP Standard 13(Physical health assessment & management) Click here for ICP toolkit & 16 (Person centred care) Click here for ICP toolkit BPS Section 5 b (p 33) (Guidance on physical needs assessment) Click for BPS Click here for information on improvement methodologies PDSA Tissue Viability click for tissue viability online Nutritional Care Click for information on nutritional care Pressure Area Care CQI Food, fluid & nutrition CQI Click for information on the CQI
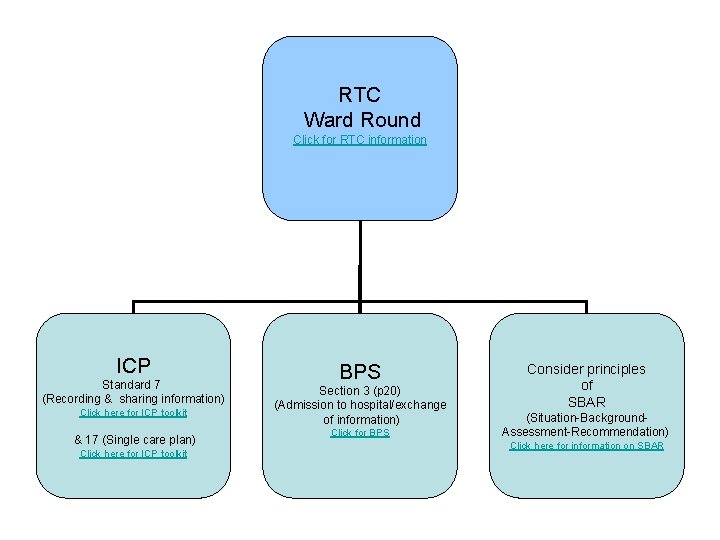
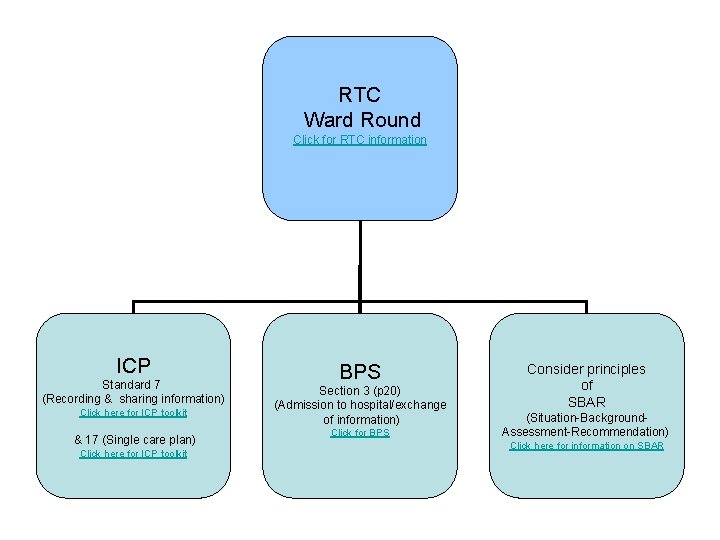
RTC Ward Round Click for RTC information ICP Standard 7 (Recording & sharing information) Click here for ICP toolkit & 17 (Single care plan) Click here for ICP toolkit BPS Section 3 (p 20) (Admission to hospital/exchange of information) Click for BPS Consider principles of SBAR (Situation-Background. Assessment-Recommendation) Click here for information on SBAR
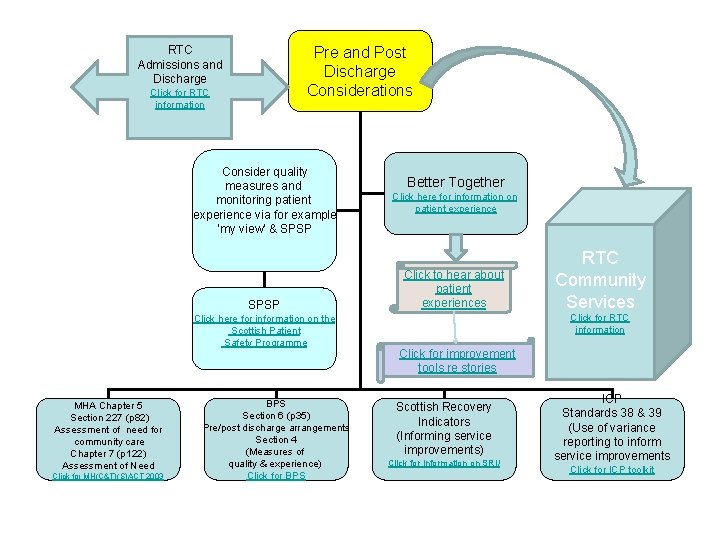
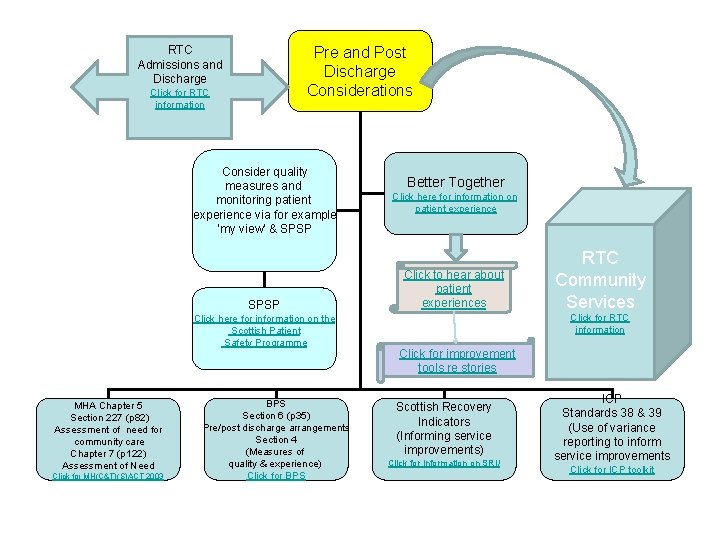
Pre and Post Discharge Considerations RTC Admissions and Discharge Click for RTC information Consider quality measures and monitoring patient experience via for example ‘my view’ & SPSP Click here for information on the Scottish Patient Safety Programme MHA Chapter 5 Section 227 (p 82) Assessment of need for community care Chapter 7 (p 122) Assessment of Need Click for MH(C&T)(S)ACT 2003 BPS Section 6 (p 35) Pre/post discharge arrangements Section 4 (Measures of quality & experience) Click for BPS Better Together Click here for information on patient experience Click to hear about patient experiences RTC Community Services Click for RTC information Click for improvement tools re stories Scottish Recovery Indicators (Informing service improvements) Click for information on SRI/ ICP Standards 38 & 39 (Use of variance reporting to inform service improvements Click for ICP toolkit