MENINGITIS NITMED TUTORIALS Definition Meningitis is the inflammation





- Slides: 15
MENINGITIS © NITMED TUTORIALS
Definition �Meningitis is the inflammation of the meninges �Inflammation of the brain cortex is called encephalitis �Meningismus refers to meningeal irritation not due to CNS infection

AETIOLOGY � Neonatal period �< 5 years Group B streptococcus Haemophilus influenzae Type B E. Coli Streptococcus pneumoniae Listeria Monocytogen Neisseria Meningitidis >5 years Neisseria Meningitidis Haemophilus influenzae Type B Streptococcus pneumoniae

Risk factors � GROM CAP Genetic susceptibility Race (black race) Overcrowding Male gender Congenital defects Young Age Poverty
Route of infection Haematogenous spread � Direct contiguous spread Acquired defect-trauma with basal skull fracture Congenital defects: meningomyelocele Lumbaosacral dural sinus cribriform plate (roof of the nose) stapedial foot plate(Middle ear) inner ear-oval window, internal auditory canal, cochler aqueduct �
Pathogenesis � Immune system activation with subsequent cytokine production 1. Increased BBB permeability 2. Altered cerebral blood flow 3. Increased reactive oxygen species 4. Leucocytes adherence to capillary endothelium
Pathogenesis CT…. � The final 4 pathological processes will lead to 1. Neuronal death 2. Increased ICP 3. Cerebral oedema
Q &A Concerning meningitis Symptoms and signs are specific during the neonatal period Children with anatomic defect or functional asplenia have infection rate higher than healthy children N. Meningitidis has 5 major serogroups A, B, C, Y and W 135, epidermics in Africa is assted with serogroup A and C Preceding history of upper respiratory tract infection is sacrosanct Inflammation of the spinal nerves and roots produces meningeal signs Streptococcal meningitis has the highest mortality rate while, H. influenzae has the lowest mortality rate
Q &A The seizure is caused by cerebritis, infarction and electrolyte disturbance Hypoglycorrhachia is attributable to decreased glucose transport by the cerebral tissue Raised CSF protein is as a result of increased vascular permeability of BBB and the loss of albumin-rich fluid from the capillaries and vein traversing the subdural space Blood culture should performed in all patient with suspected meningitis-positive in 80 -90% of cases. The classical CSF finding in Bacterial meningitis is increased WBC, increased protein and reduced CSF glucose
� pleocytosis, hypoglycorrhachia and elevated protein is the usual CSF findings in bacteria meningitis. � Duration of treatment for bacteria meningitis Strep pneumonia is 10 -14 days H. influenzae is 7 -10 days N. meningitis is 5 -7 days gram negatives bacillary meningitis is treated for 3 weeks

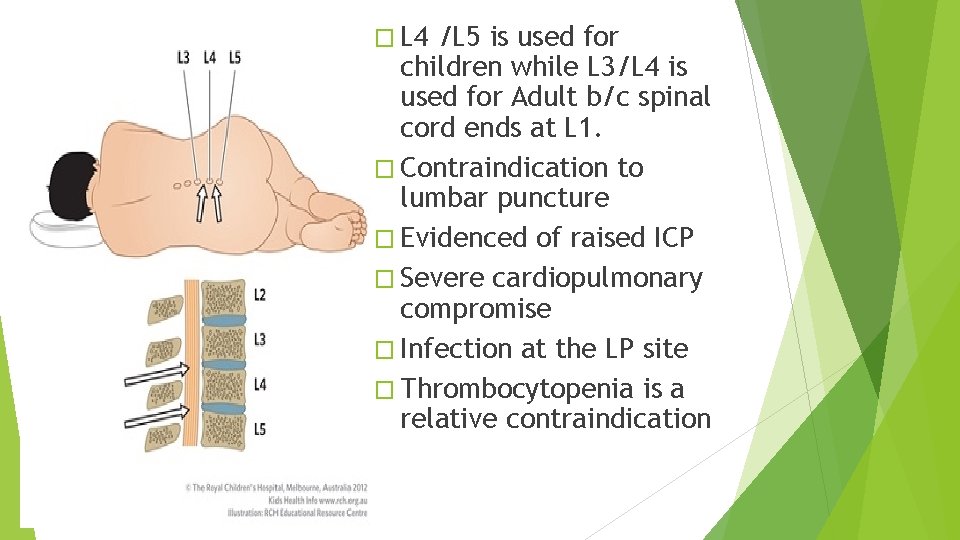
What is the instrument ?
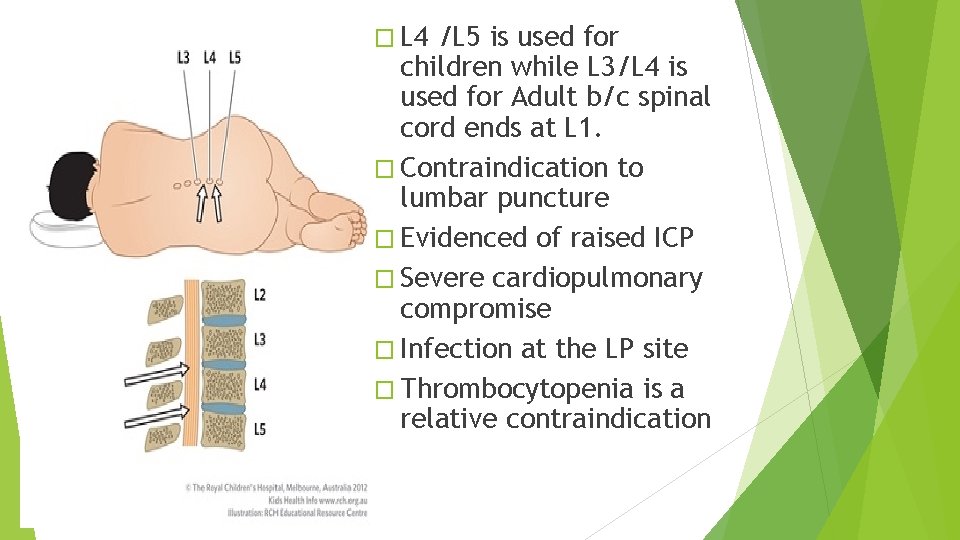
� L 4 /L 5 is used for children while L 3/L 4 is used for Adult b/c spinal cord ends at L 1. � Contraindication to lumbar puncture � Evidenced of raised ICP � Severe cardiopulmonary compromise � Infection at the LP site � Thrombocytopenia is a relative contraindication
� The CSF should be sterile within 24 -48 hr of initiation of appropriate antibiotic therapy. � what are the causes of CSF xanthochromia � Traumatic lumber puncture � Subarachnoid haemorrhage � Hyperbilirubinaemia � Markedly elevated CSF protein

� Evidenced of raised ICP and severe cardiopulmonary compromise are contraindications for LP � Site for LP is L 3/L 4 or L 4/L 5 � Xanthochromia is pathognomonic for subarachnoid haemorrhage � Viral meningitis is usually less severe than bacteria meningitis � All patient with bacterial meningitis shd be assessed for hearing or visual deficit before discharge.

Thank you