Meeting the ACGME Milestones through Group Prenatal Care
- Slides: 1
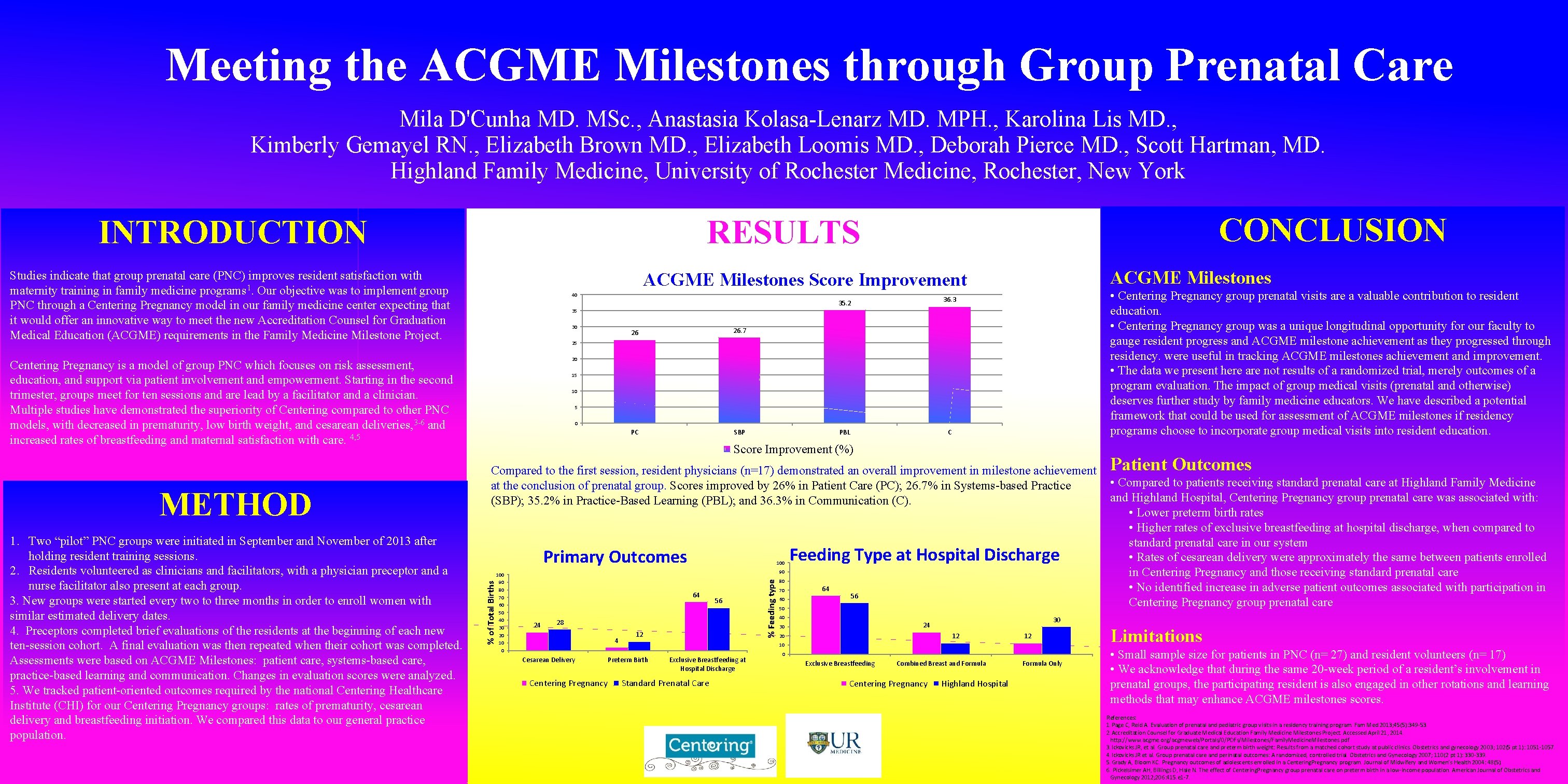
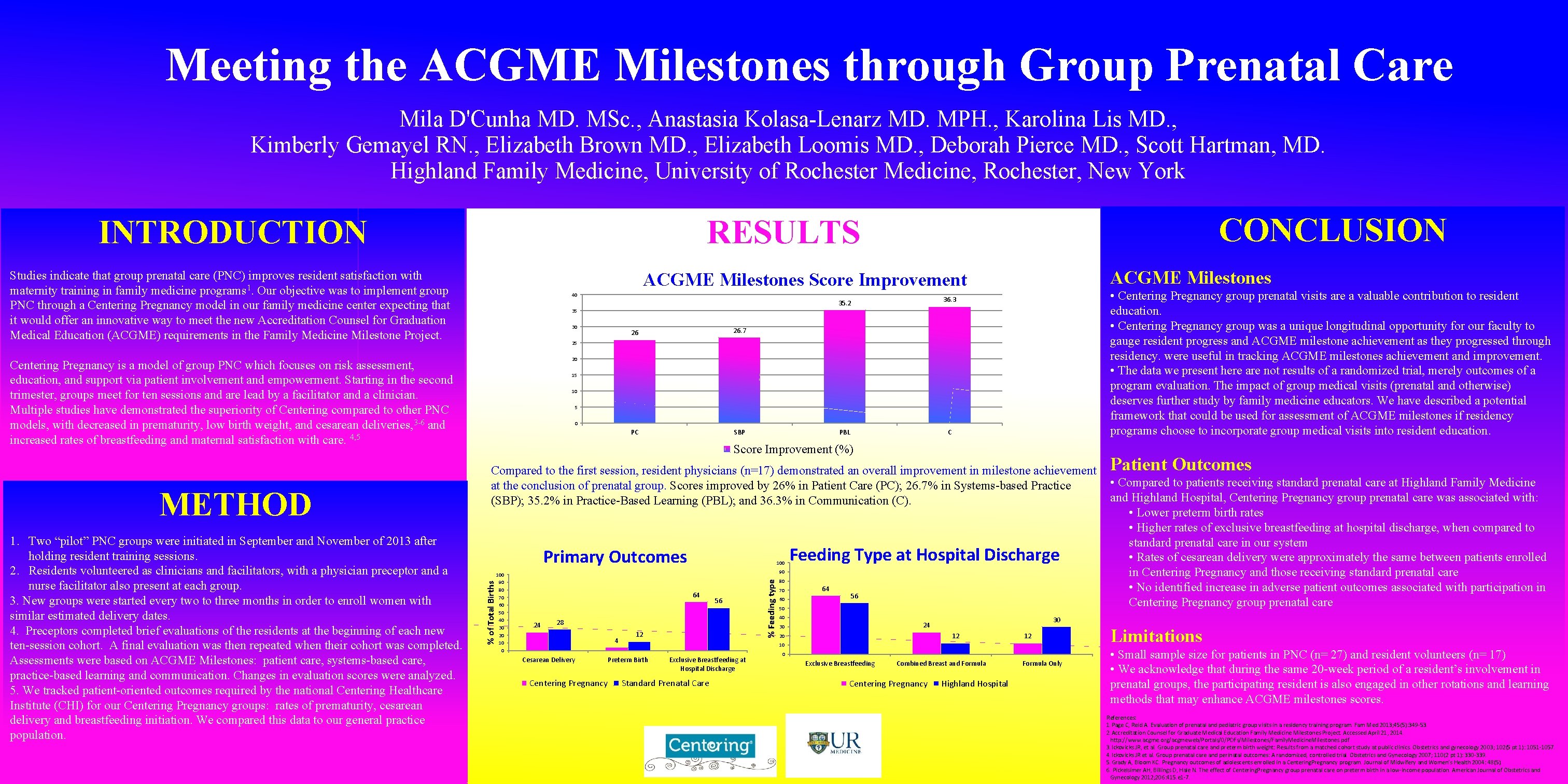
Meeting the ACGME Milestones through Group Prenatal Care Mila D'Cunha MD. MSc. , Anastasia Kolasa-Lenarz MD. MPH. , Karolina Lis MD. , Kimberly Gemayel RN. , Elizabeth Brown MD. , Elizabeth Loomis MD. , Deborah Pierce MD. , Scott Hartman, MD. Highland Family Medicine, University of Rochester Medicine, Rochester, New York INTRODUCTION Studies indicate that group prenatal care (PNC) improves resident satisfaction with maternity training in family medicine programs 1. Our objective was to implement group PNC through a Centering Pregnancy model in our family medicine center expecting that it would offer an innovative way to meet the new Accreditation Counsel for Graduation Medical Education (ACGME) requirements in the Family Medicine Milestone Project. 40 35. 2 36. 3 PBL C • Centering Pregnancy group prenatal visits are a valuable contribution to resident education. • Centering Pregnancy group was a unique longitudinal opportunity for our faculty to gauge resident progress and ACGME milestone achievement as they progressed through residency. were useful in tracking ACGME milestones achievement and improvement. • The data we present here are not results of a randomized trial, merely outcomes of a program evaluation. The impact of group medical visits (prenatal and otherwise) deserves further study by family medicine educators. We have described a potential framework that could be used for assessment of ACGME milestones if residency programs choose to incorporate group medical visits into resident education. 35 30 26 26. 7 PC SBP 25 20 15 10 5 0 Score Improvement (%) Compared to the first session, resident physicians (n=17) demonstrated an overall improvement in milestone achievement at the conclusion of prenatal group. Scores improved by 26% in Patient Care (PC); 26. 7% in Systems-based Practice (SBP); 35. 2% in Practice-Based Learning (PBL); and 36. 3% in Communication (C). Primary Outcomes 100 90 80 70 60 50 40 30 20 100 Feeding Type at Hospital Discharge 90 64 24 56 28 4 Cesarean Delivery Centering Pregnancy 12 % Feeding type % of Total Births 1. Two “pilot” PNC groups were initiated in September and November of 2013 after holding resident training sessions. 2. Residents volunteered as clinicians and facilitators, with a physician preceptor and a nurse facilitator also present at each group. 3. New groups were started every two to three months in order to enroll women with similar estimated delivery dates. 4. Preceptors completed brief evaluations of the residents at the beginning of each new ten-session cohort. A final evaluation was then repeated when their cohort was completed. Assessments were based on ACGME Milestones: patient care, systems-based care, practice-based learning and communication. Changes in evaluation scores were analyzed. 5. We tracked patient-oriented outcomes required by the national Centering Healthcare Institute (CHI) for our Centering Pregnancy groups: rates of prematurity, cesarean delivery and breastfeeding initiation. We compared this data to our general practice population. ACGME Milestones Score Improvement Centering Pregnancy is a model of group PNC which focuses on risk assessment, education, and support via patient involvement and empowerment. Starting in the second trimester, groups meet for ten sessions and are lead by a facilitator and a clinician. Multiple studies have demonstrated the superiority of Centering compared to other PNC models, with decreased in prematurity, low birth weight, and cesarean deliveries, 3 -6 and increased rates of breastfeeding and maternal satisfaction with care. 4, 5 METHOD CONCLUSION RESULTS 80 70 60 64 56 50 40 12 20 12 10 Preterm Birth Exclusive Breastfeeding at Hospital Discharge Standard Prenatal Care 0 Exclusive Breastfeeding Combined Breast and Formula Centering Pregnancy • Compared to patients receiving standard prenatal care at Highland Family Medicine and Highland Hospital, Centering Pregnancy group prenatal care was associated with: • Lower preterm birth rates • Higher rates of exclusive breastfeeding at hospital discharge, when compared to standard prenatal care in our system • Rates of cesarean delivery were approximately the same between patients enrolled in Centering Pregnancy and those receiving standard prenatal care • No identified increase in adverse patient outcomes associated with participation in Centering Pregnancy group prenatal care 30 24 30 Patient Outcomes Highland Hospital Formula Only Limitations • Small sample size for patients in PNC (n= 27) and resident volunteers (n= 17) • We acknowledge that during the same 20 -week period of a resident’s involvement in prenatal groups, the participating resident is also engaged in other rotations and learning methods that may enhance ACGME milestones scores. References: 1. Page C, Reid A. Evaluation of prenatal and pediatric group visits in a residency training program. Fam Med 2013; 45(5): 349 -53. 2. Accreditation Counsel for Graduate Medical Education Family Medicine Milestones Project. Accessed April 21, 2014. http: //www. acgme. org/acgmeweb/Portals/0/PDFs/Milestones/Family. Medicine. Milestones. pdf 3. Ickovicks JR, et al. Group prenatal care and preterm birth weight: Results from a matched cohort study at public clinics. Obstetrics and gynecology 2003; 102(5 pt 1): 1051 -1057. 4. Ickovicks JR et al. Group prenatal care and perinatal outcomes: A randomized, controlled trial. Obstetrics and Gynecology 2007; 110(2 pt 1): 330 -339. 5. Grady A, Bloom KC. Pregnancy outcomes of adolescents enrolled in a Centering. Pregnancy program. Journal of Midwifery and Women’s Health 2004: 48(5). 6. Pickelsimer AH, Billings D, Hale N. The effect of Centering. Pregnancy group prenatal care on preterm birth in a low-income population. American Journal of Obstetrics and Gynecology 2012; 206: 415. e 1 -7.