Meeting the 2025 salt reduction target and responding

- Slides: 59
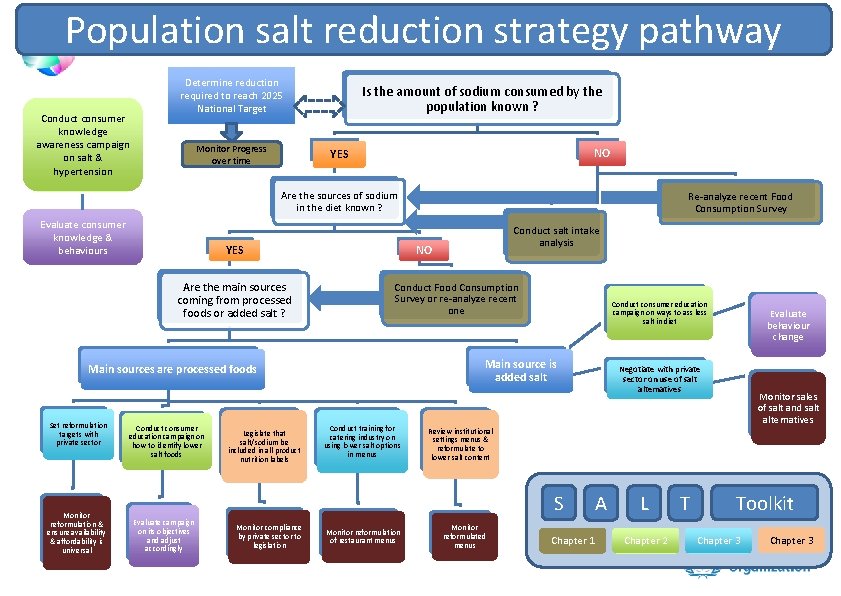
Meeting the 2025 salt reduction target and responding to the GMF dietary risk factors on fruit and vegetable consumption and policies to limit saturated and trans fats 7 th WHO-IUMSP International Seminar on the Public Health Aspects of Noncommunicable Dieases. Lausanne & Geneva, 3 -8 June 2013 Jason Montez Technical Officer Department of Nutrition for Health and Development Leo Nederveen Technical Officer Department of Prevention of Noncommunicable Diseases
Presentation overview • Promoting a healthy diet and WHO dietary recommendations • Reducing saturated and trans fats • Nutrient profiling and labelling • Salt reduction strategies
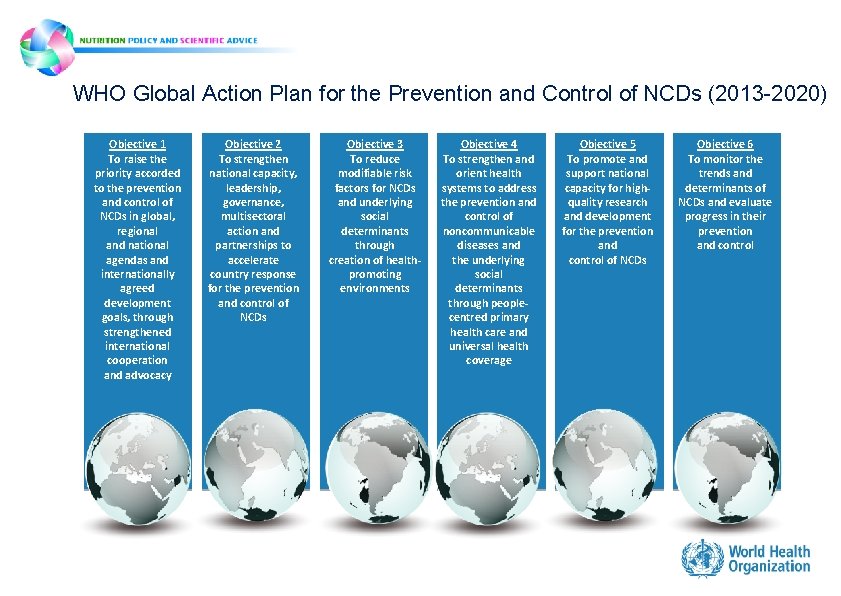
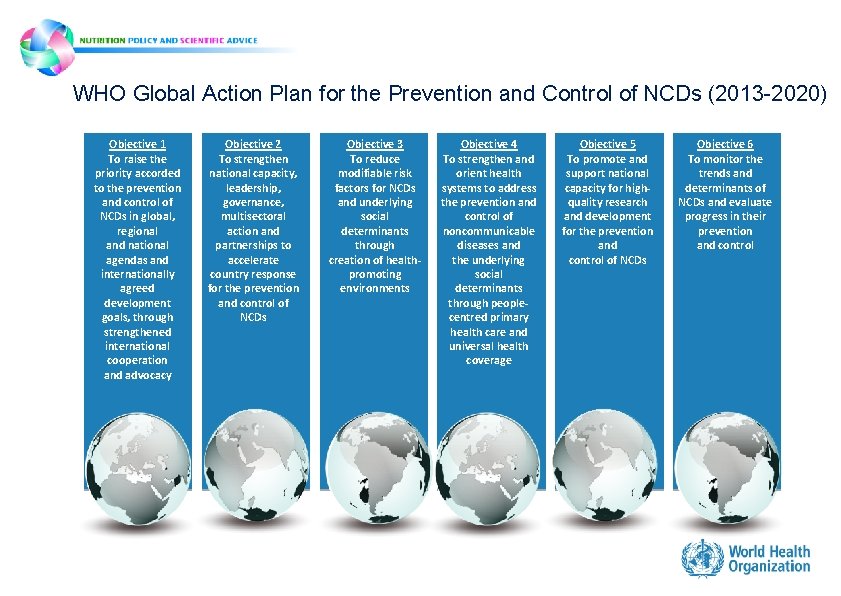
WHO Global Action Plan for the Prevention and Control of NCDs (2013 -2020) Objective 1 To raise the priority accorded to the prevention and control of NCDs in global, regional and national agendas and internationally agreed development goals, through strengthened international cooperation and advocacy Objective 2 To strengthen national capacity, leadership, governance, multisectoral action and partnerships to accelerate country response for the prevention and control of NCDs Objective 3 To reduce modifiable risk factors for NCDs and underlying social determinants through creation of healthpromoting environments Objective 4 To strengthen and orient health systems to address the prevention and control of noncommunicable diseases and the underlying social determinants through peoplecentred primary health care and universal health coverage Objective 5 To promote and support national capacity for highquality research and development for the prevention and control of NCDs Objective 6 To monitor the trends and determinants of NCDs and evaluate progress in their prevention and control
WHO Global Action Plan for the Prevention and Control of NCDs (2013 -2020) Objective 1 To raise the priority accorded to the prevention and control of NCDs in global, regional and national agendas and internationally agreed development goals, through strengthened international cooperation and advocacy Objective 2 To strengthen national capacity, leadership, governance, multisectoral action and partnerships to accelerate country response for the prevention and control of NCDs Objective 3 To reduce modifiable risk factors for NCDs and underlying social determinants through creation of healthpromoting environments Objective 4 To strengthen and orient health systems to address the prevention and control of noncommunicable diseases and the underlying social determinants through peoplecentred primary health care and universal health coverage Objective 5 To promote and support national capacity for highquality research and development for the prevention and control of NCDs Objective 6 To monitor the trends and determinants of NCDs and evaluate progress in their prevention and control
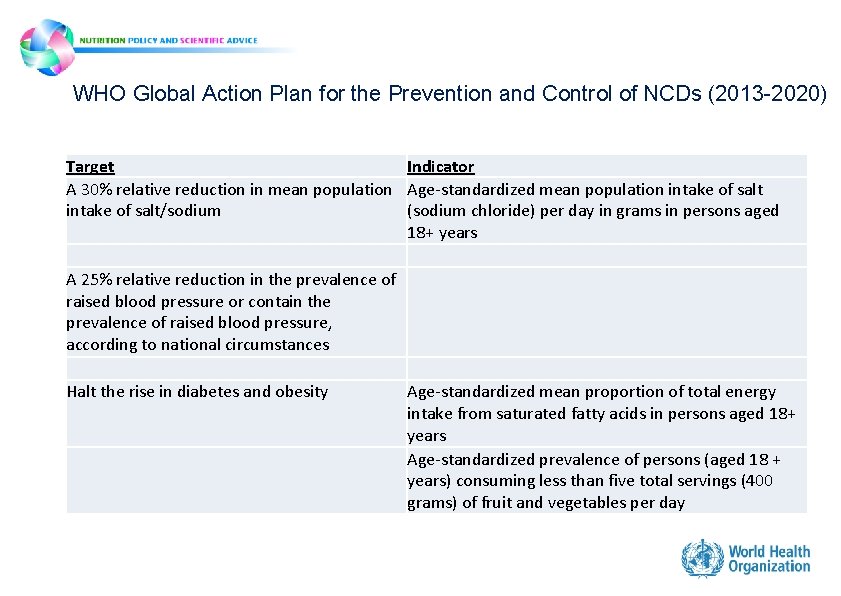
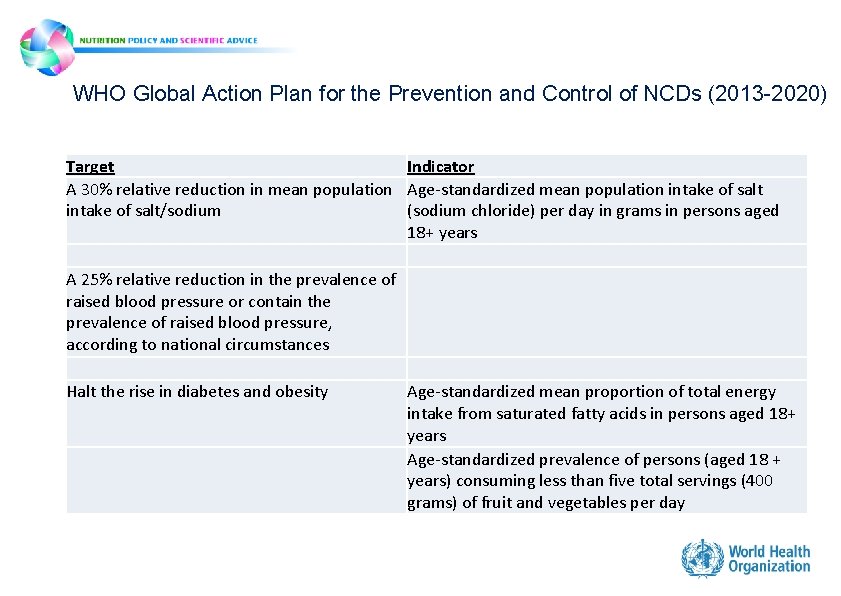
WHO Global Action Plan for the Prevention and Control of NCDs (2013 -2020) Target Indicator A 30% relative reduction in mean population Age-standardized mean population intake of salt/sodium (sodium chloride) per day in grams in persons aged 18+ years A 25% relative reduction in the prevalence of raised blood pressure or contain the prevalence of raised blood pressure, according to national circumstances Halt the rise in diabetes and obesity Age-standardized mean proportion of total energy intake from saturated fatty acids in persons aged 18+ years Age-standardized prevalence of persons (aged 18 + years) consuming less than five total servings (400 grams) of fruit and vegetables per day
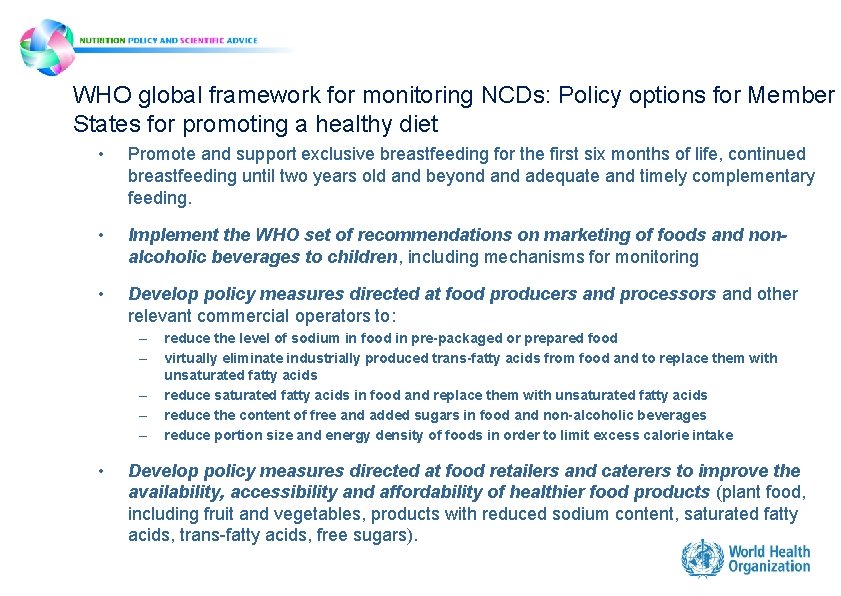
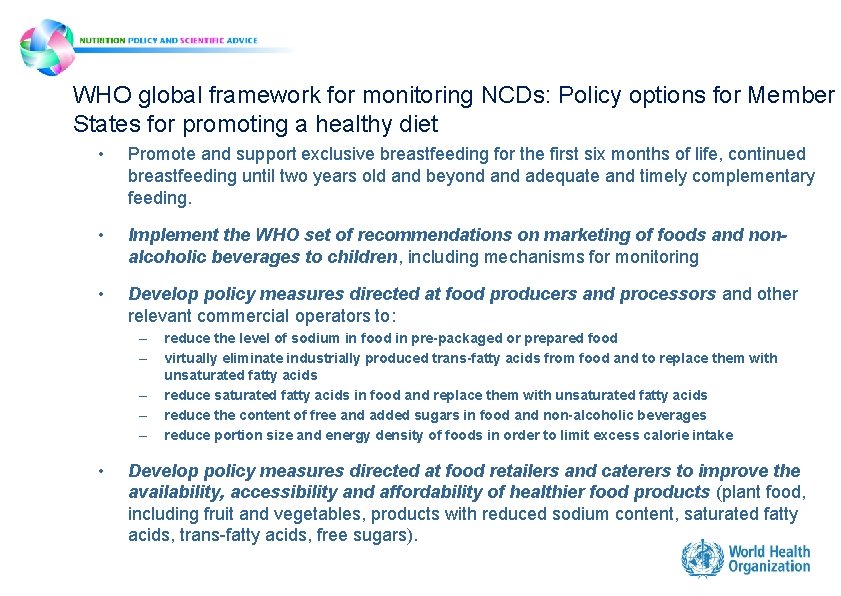
WHO global framework for monitoring NCDs: Policy options for Member States for promoting a healthy diet • Promote and support exclusive breastfeeding for the first six months of life, continued breastfeeding until two years old and beyond adequate and timely complementary feeding. • Implement the WHO set of recommendations on marketing of foods and nonalcoholic beverages to children, including mechanisms for monitoring • Develop policy measures directed at food producers and processors and other relevant commercial operators to: – – – • reduce the level of sodium in food in pre-packaged or prepared food virtually eliminate industrially produced trans-fatty acids from food and to replace them with unsaturated fatty acids reduce saturated fatty acids in food and replace them with unsaturated fatty acids reduce the content of free and added sugars in food and non-alcoholic beverages reduce portion size and energy density of foods in order to limit excess calorie intake Develop policy measures directed at food retailers and caterers to improve the availability, accessibility and affordability of healthier food products (plant food, including fruit and vegetables, products with reduced sodium content, saturated fatty acids, trans-fatty acids, free sugars).
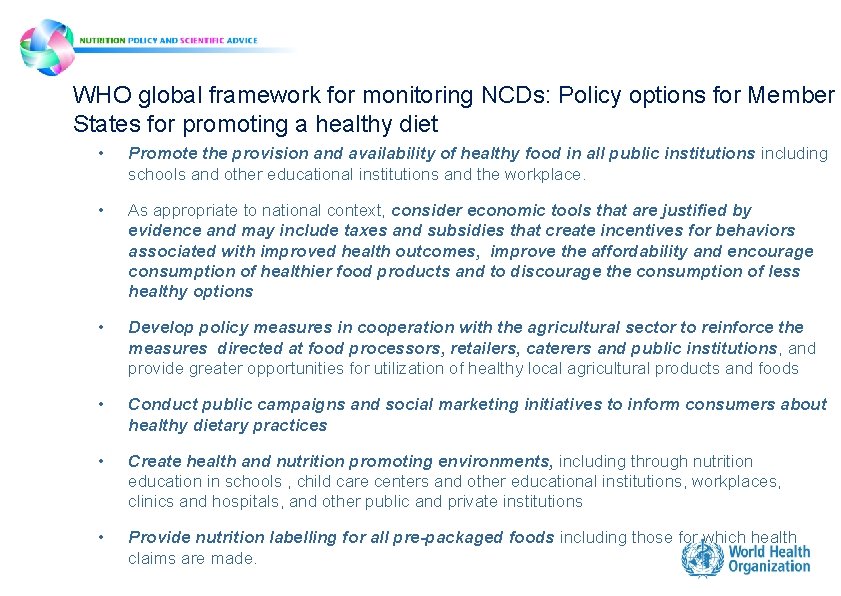
WHO global framework for monitoring NCDs: Policy options for Member States for promoting a healthy diet • Promote the provision and availability of healthy food in all public institutions including schools and other educational institutions and the workplace. • As appropriate to national context, consider economic tools that are justified by evidence and may include taxes and subsidies that create incentives for behaviors associated with improved health outcomes, improve the affordability and encourage consumption of healthier food products and to discourage the consumption of less healthy options • Develop policy measures in cooperation with the agricultural sector to reinforce the measures directed at food processors, retailers, caterers and public institutions, and provide greater opportunities for utilization of healthy local agricultural products and foods • Conduct public campaigns and social marketing initiatives to inform consumers about healthy dietary practices • Create health and nutrition promoting environments, including through nutrition education in schools , child care centers and other educational institutions, workplaces, clinics and hospitals, and other public and private institutions • Provide nutrition labelling for all pre-packaged foods including those for which health claims are made.
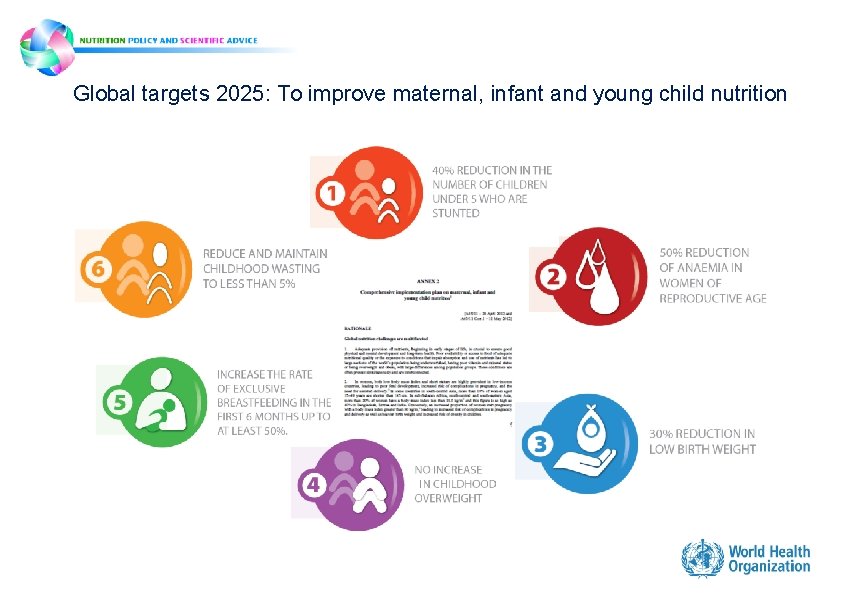
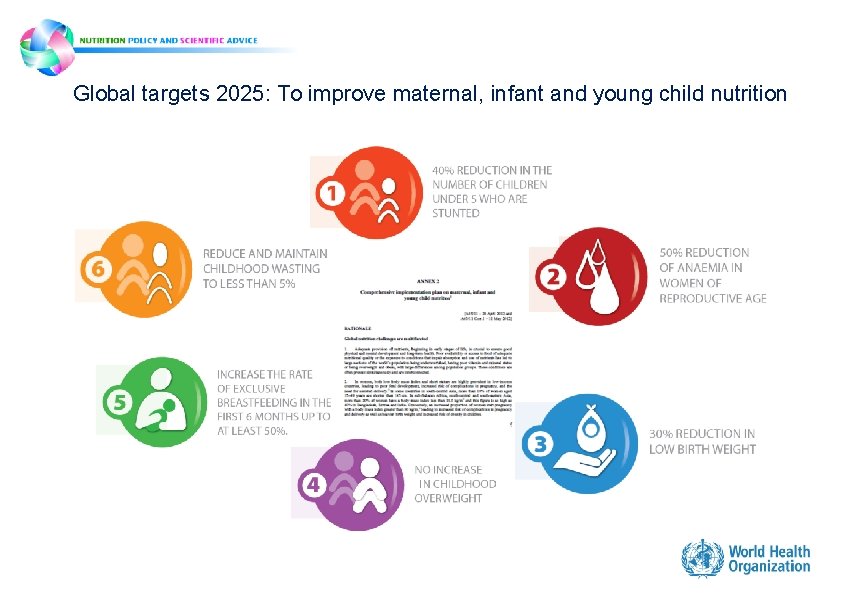
Global targets 2025: To improve maternal, infant and young child nutrition I
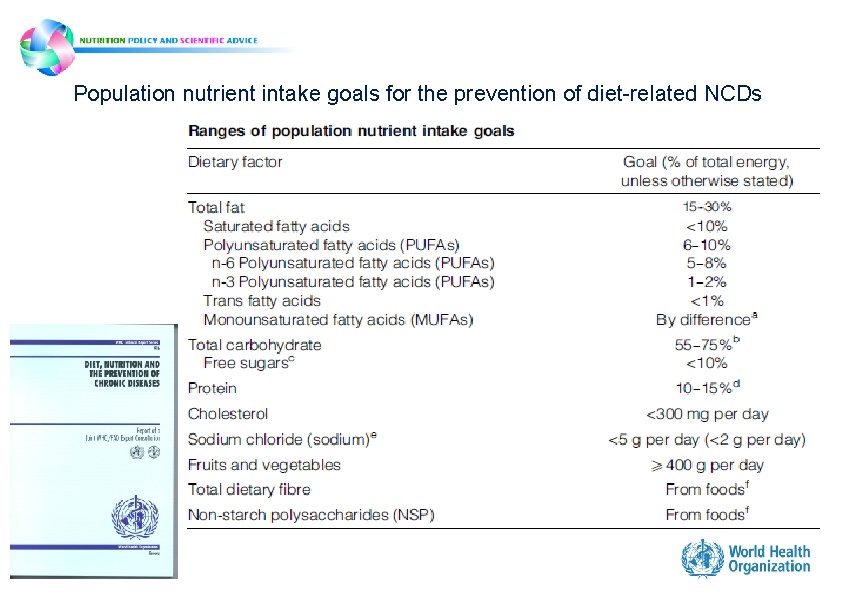
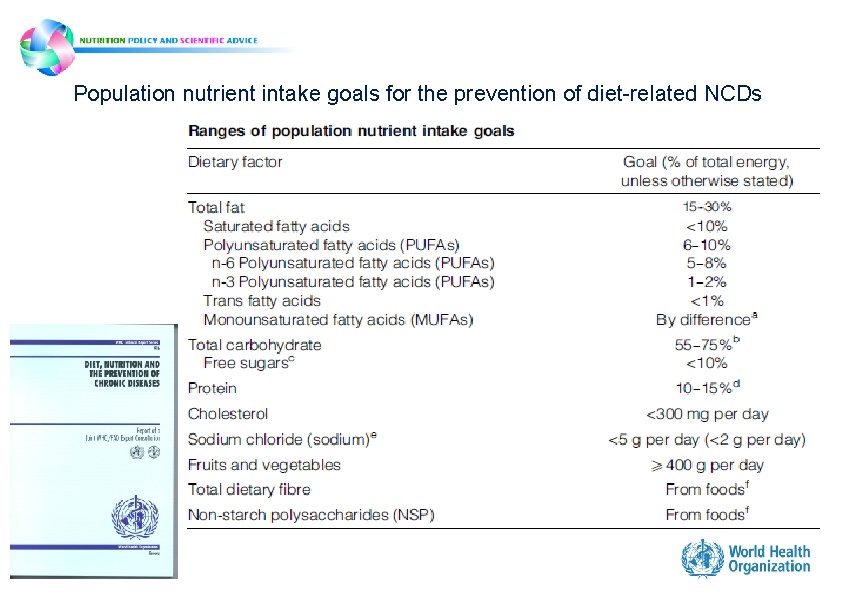
Population nutrient intake goals for the prevention of diet-related NCDs
NCD-related nutrition guidelines • Sodium intake for adults and children – Published 2012 • Potassium intake for adults and children – Published 2012 • Total fat intake for adults and children – Expected late 2013 • Free sugars intake for adults and children – Expected late 2013 • Saturated fat intake for adults and children – Expected early 2014 • Trans fat intake for adults and children – Expected early 2014
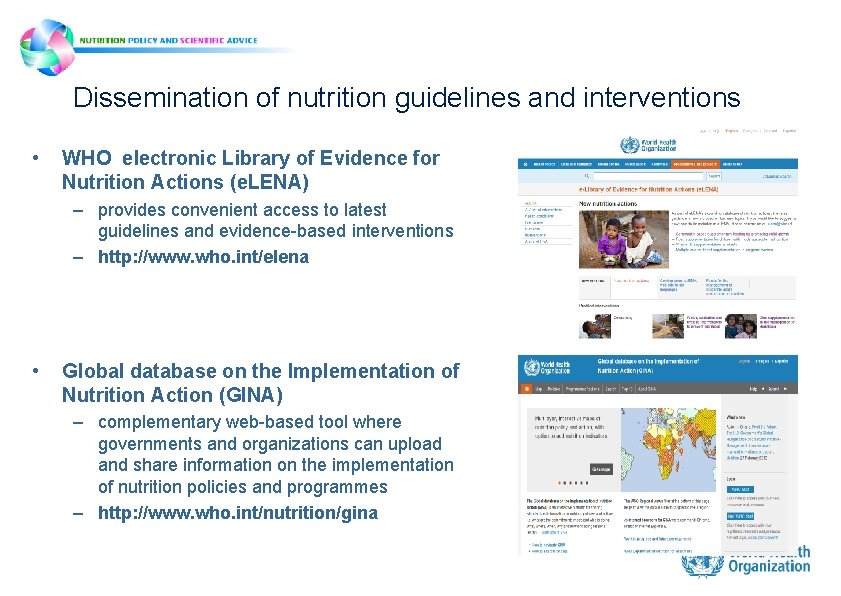
Dissemination of nutrition guidelines and interventions • WHO electronic Library of Evidence for Nutrition Actions (e. LENA) – provides convenient access to latest guidelines and evidence-based interventions – http: //www. who. int/elena • Global database on the Implementation of Nutrition Action (GINA) – complementary web-based tool where governments and organizations can upload and share information on the implementation of nutrition policies and programmes – http: //www. who. int/nutrition/gina
Reducing saturated and trans fat intake 7 th WHO-IUMSP International Seminar on the Public Health Aspects of Noncommunicable Dieases. Lausanne & Geneva, 3 -8 June 2013
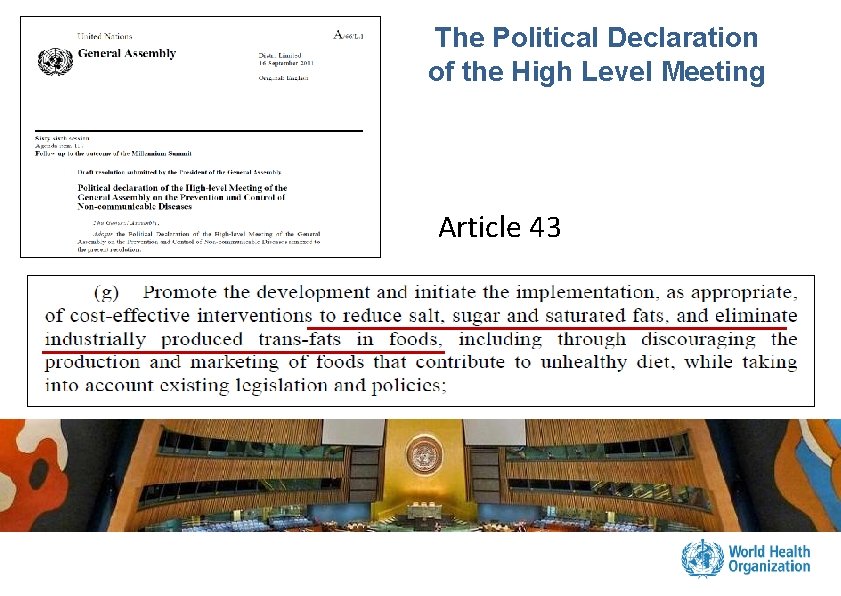
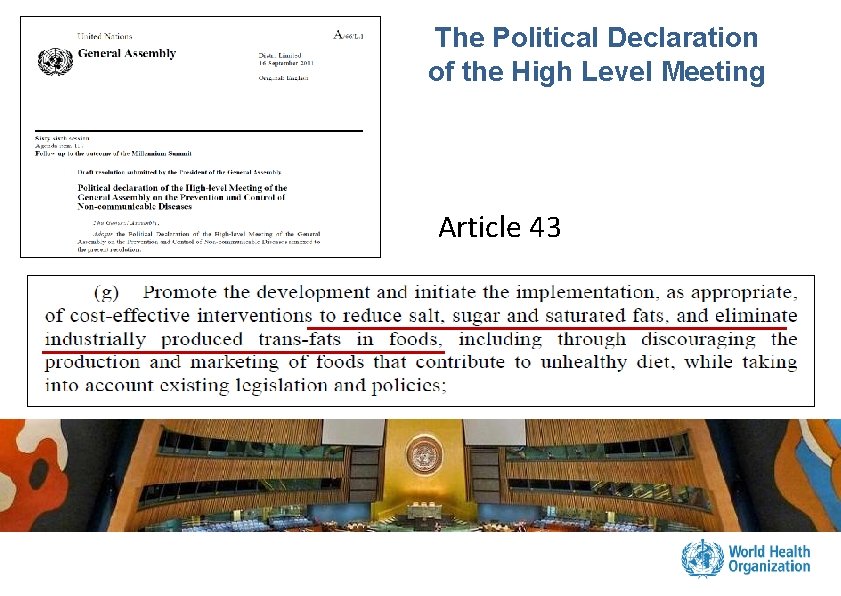
The Political Declaration of the High Level Meeting Article 43
SFA and TFA in the Diet and Physical Activity Strategy (WHA 57. 17) 1. Recommendations for populations and individuals should include : – limit energy intake from total fats and shift fat consumption away from saturated fats to unsaturated fats and towards the elimination of trans-fatty acids 2. Governments are encouraged to adopt policies that support healthy diets at school and limit the availability of products high in salt, sugar and fats 3. Recommendations to the food industry – limit the levels of saturated fats, trans-fatty acids, free sugars and salt in existing products – practice responsible marketing that supports the strategy, particularly with regard to the promotion and marketing of foods high in saturated fats, trans-fatty acids, free sugars, or salt, especially to children SFA and TFA are well known risk factors for cardiovascular diseases
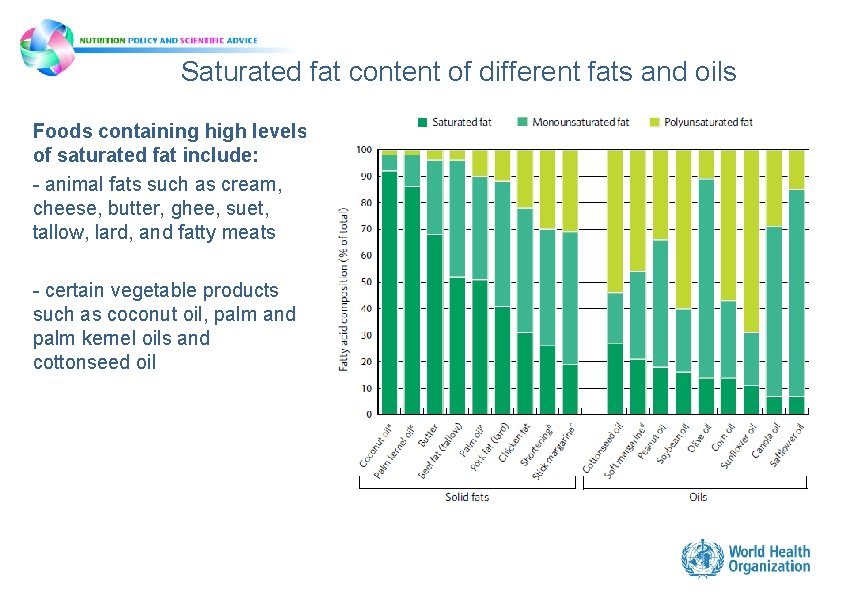
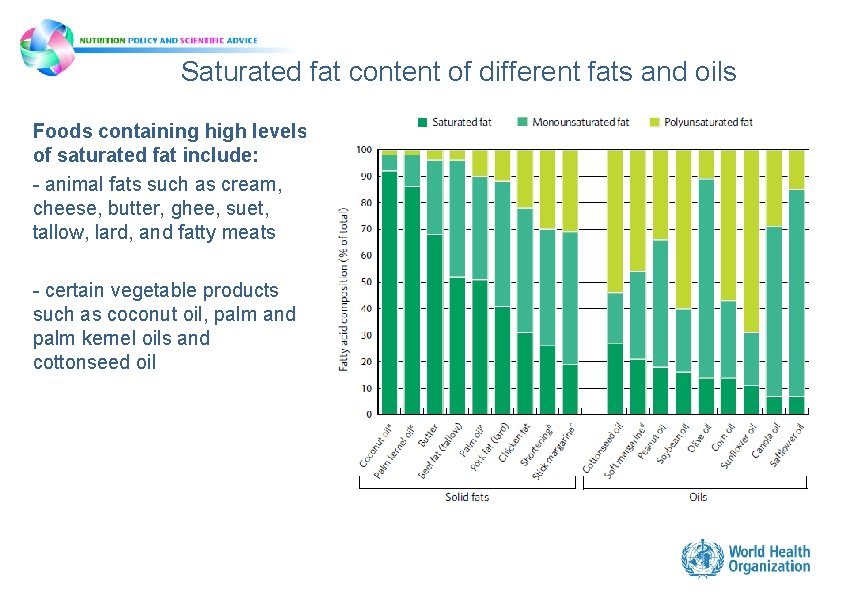
Saturated fat content of different fats and oils Foods containing high levels of saturated fat include: - animal fats such as cream, cheese, butter, ghee, suet, tallow, lard, and fatty meats - certain vegetable products such as coconut oil, palm and palm kernel oils and cottonseed oil
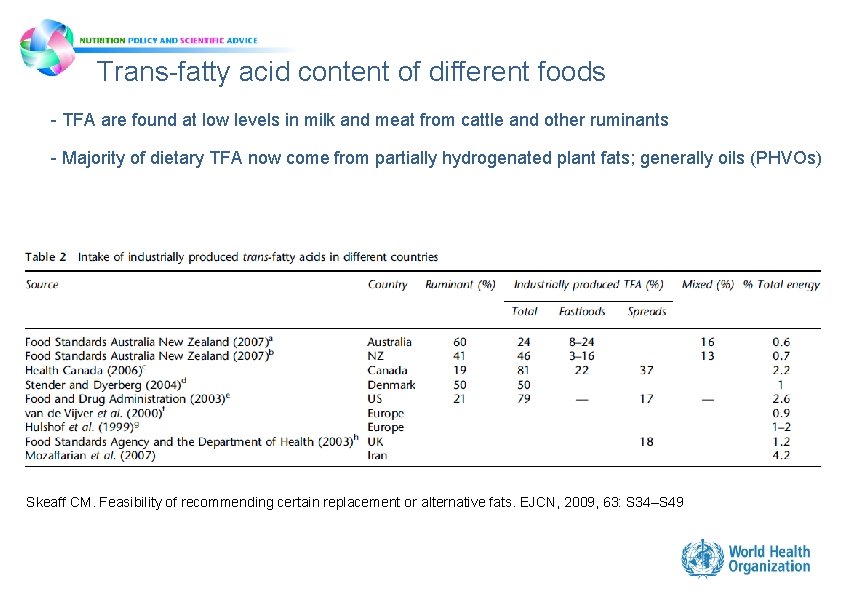
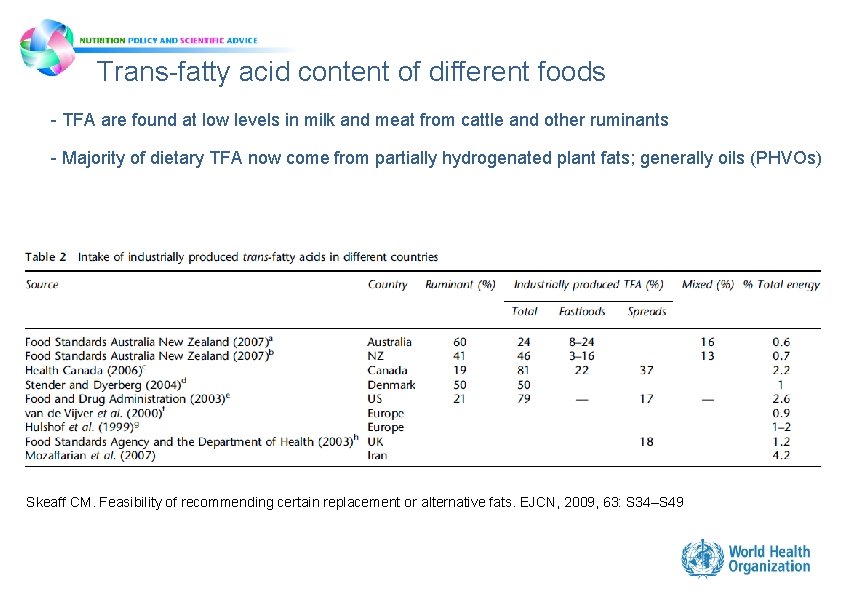
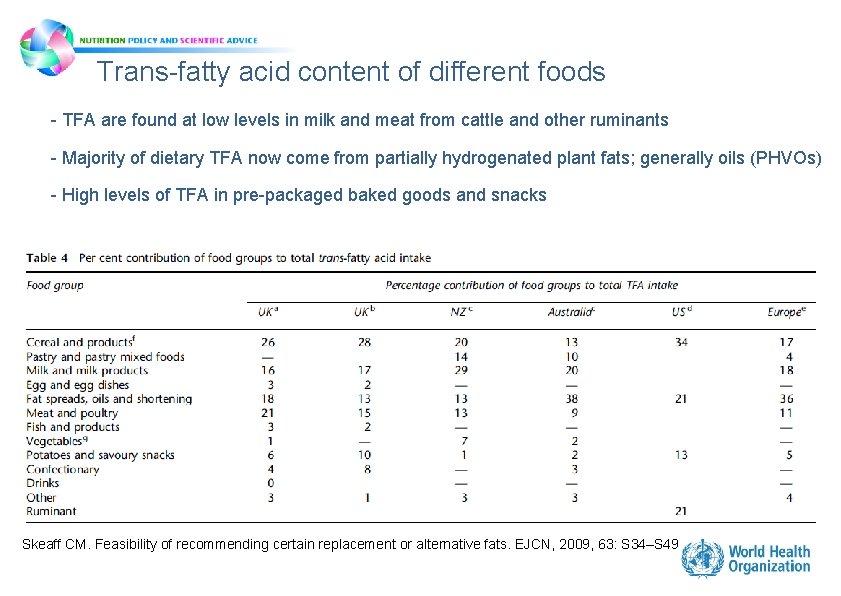
Trans-fatty acid content of different foods - TFA are found at low levels in milk and meat from cattle and other ruminants - Majority of dietary TFA now come from partially hydrogenated plant fats; generally oils (PHVOs) Skeaff CM. Feasibility of recommending certain replacement or alternative fats. EJCN, 2009, 63: S 34–S 49
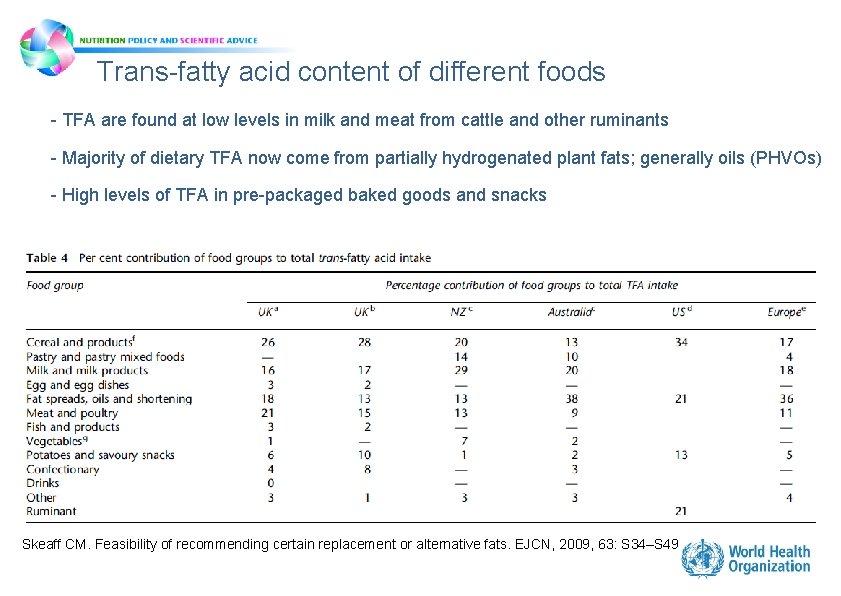
Trans-fatty acid content of different foods - TFA are found at low levels in milk and meat from cattle and other ruminants - Majority of dietary TFA now come from partially hydrogenated plant fats; generally oils (PHVOs) - High levels of TFA in pre-packaged baked goods and snacks Skeaff CM. Feasibility of recommending certain replacement or alternative fats. EJCN, 2009, 63: S 34–S 49
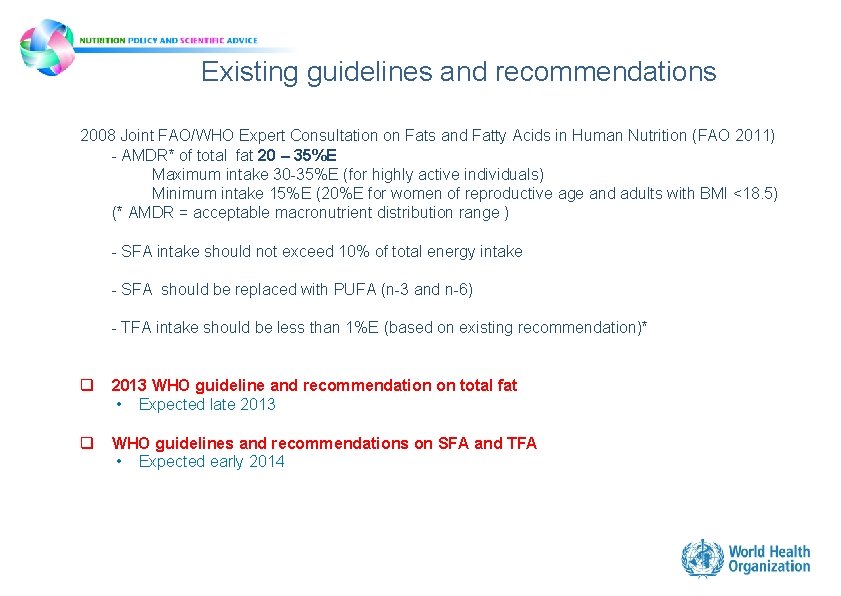
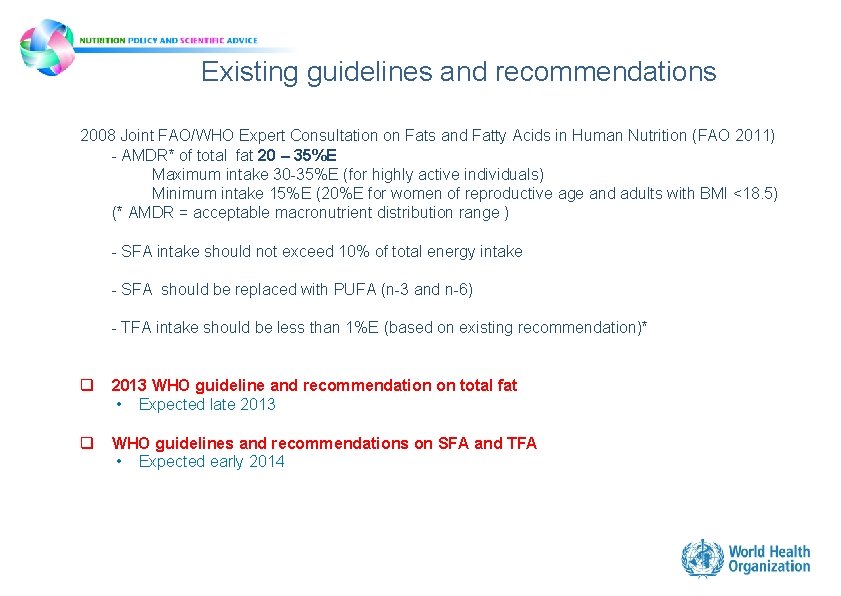
Existing guidelines and recommendations 2008 Joint FAO/WHO Expert Consultation on Fats and Fatty Acids in Human Nutrition (FAO 2011) - AMDR* of total fat 20 – 35%E Maximum intake 30 -35%E (for highly active individuals) Minimum intake 15%E (20%E for women of reproductive age and adults with BMI <18. 5) (* AMDR = acceptable macronutrient distribution range ) - SFA intake should not exceed 10% of total energy intake - SFA should be replaced with PUFA (n-3 and n-6) - TFA intake should be less than 1%E (based on existing recommendation)* q 2013 WHO guideline and recommendation on total fat • Expected late 2013 q WHO guidelines and recommendations on SFA and TFA • Expected early 2014
Interventions to reduce intake of SFA and TFA • • Reformulation – Replacement of TFA with unsaturated FA , esp. PUFA (bans) – Reduction of SFA and replacement with unsaturated FA, esp. PUFA – Monitoring product composition Labelling – Mandatory labelling of SFA and TFA – Science-based consumer friendly labelling schemes (nutrient profiling) Pricing policies – Differential taxation of products with reduced TFA and SFA content Marketing restrictions – Advertisements to children Menu changes in public institutions Public awareness and education campaigns – National Food-Based Dietary Guidelines – Mass media – School education Evidence generation – Measurement of intake of SFA and TFA
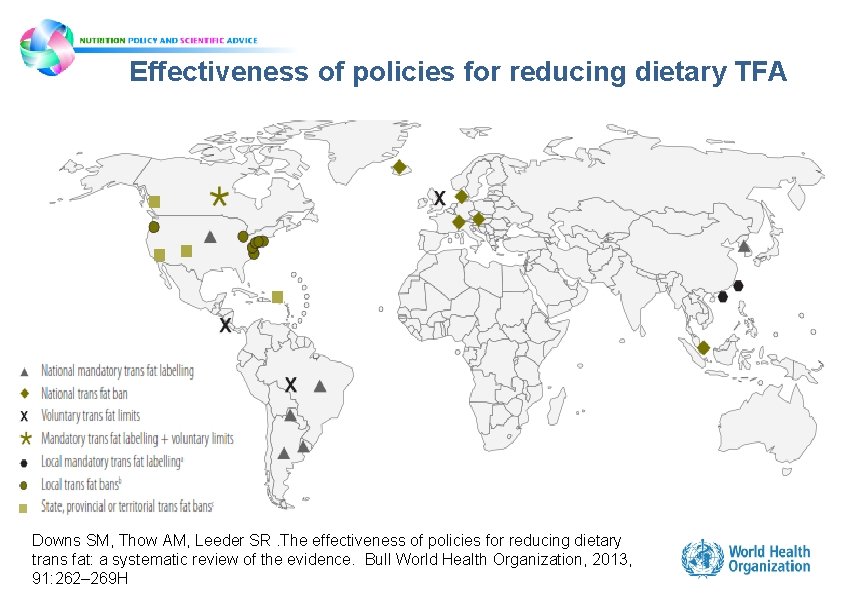
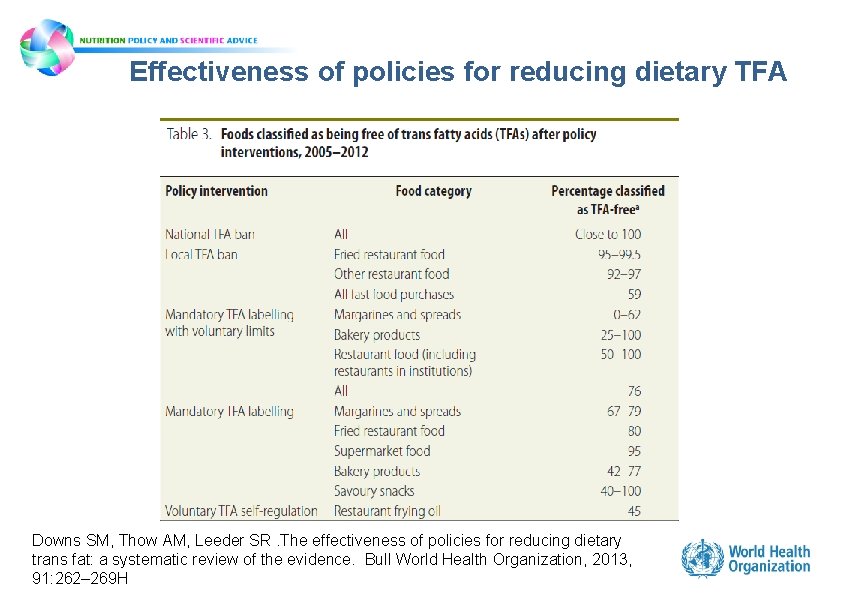
Effectiveness of policies for reducing dietary TFA • Systematic review – Voluntary self-regulation – Labelling alone – Labelling and voluntary limits – Local bans – National bans • TFA content of food decreased with all types of intervention • SFA levels increased or stayed the same depending on product type • Total fat remained stable • National and local bans were most effective at eliminating TFA from food supply
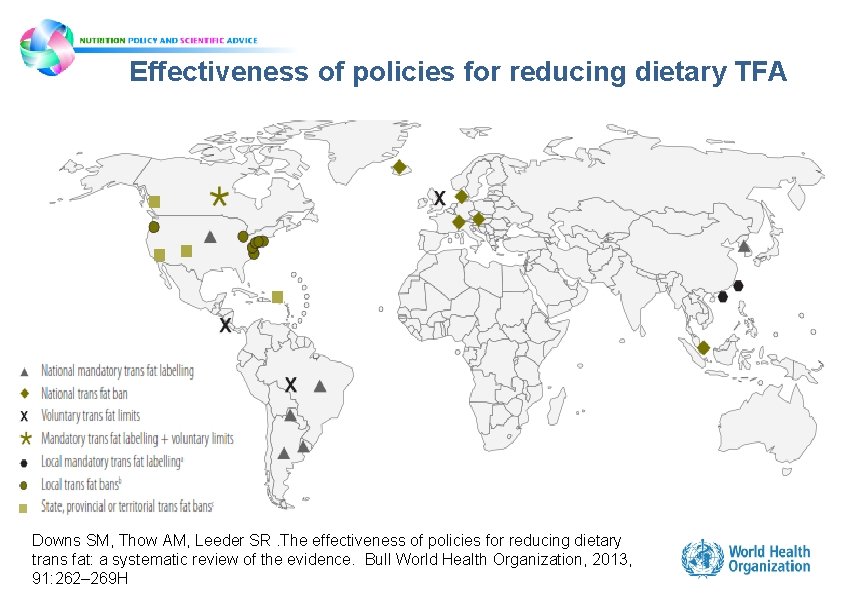
Effectiveness of policies for reducing dietary TFA Downs SM, Thow AM, Leeder SR. The effectiveness of policies for reducing dietary trans fat: a systematic review of the evidence. Bull World Health Organization, 2013, 91: 262– 269 H
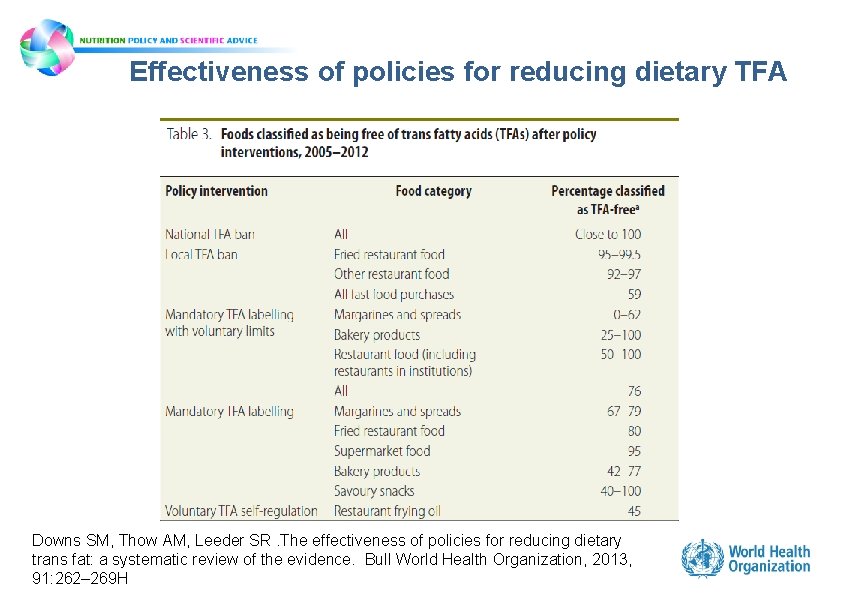
Effectiveness of policies for reducing dietary TFA Downs SM, Thow AM, Leeder SR. The effectiveness of policies for reducing dietary trans fat: a systematic review of the evidence. Bull World Health Organization, 2013, 91: 262– 269 H
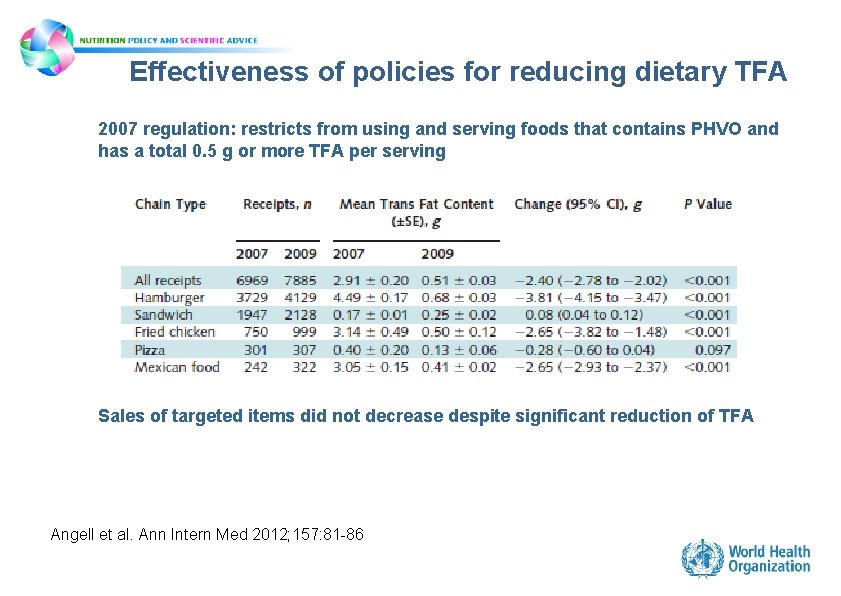
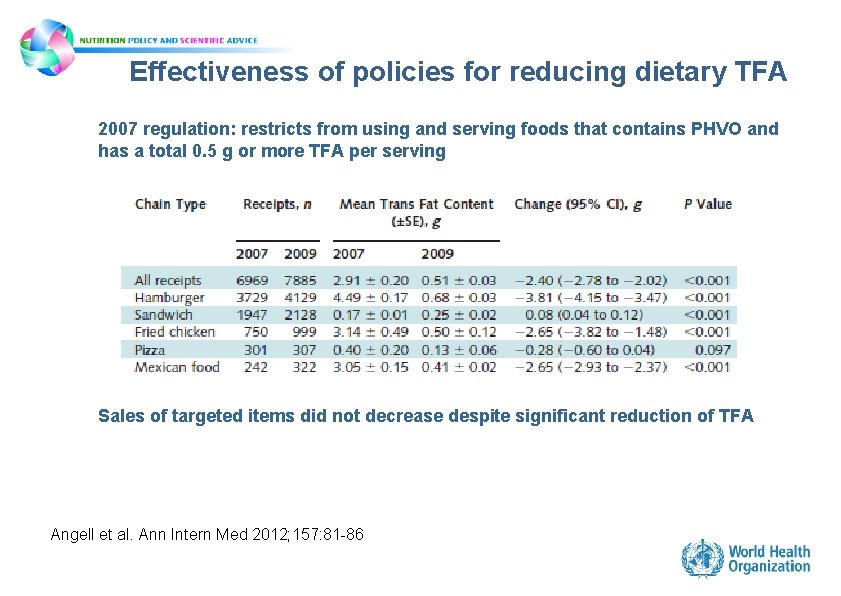
Effectiveness of policies for reducing dietary TFA 2007 regulation: restricts from using and serving foods that contains PHVO and has a total 0. 5 g or more TFA per serving Sales of targeted items did not decrease despite significant reduction of TFA Angell et al. Ann Intern Med 2012; 157: 81 -86
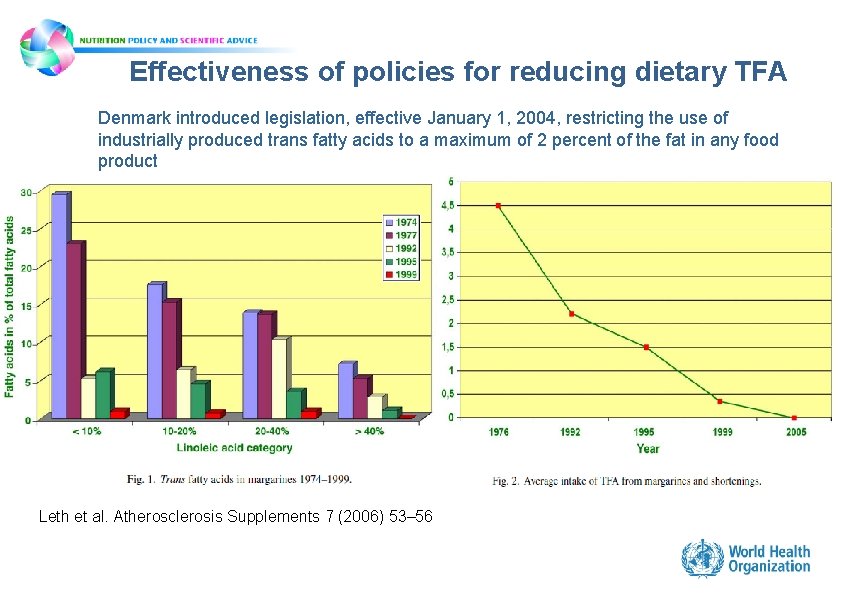
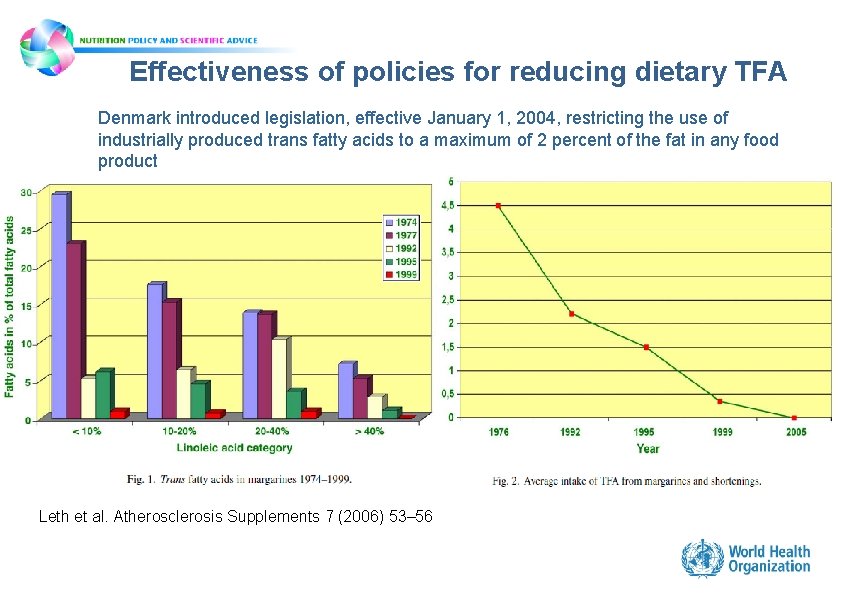
Effectiveness of policies for reducing dietary TFA Denmark introduced legislation, effective January 1, 2004, restricting the use of industrially produced trans fatty acids to a maximum of 2 percent of the fat in any food product Leth et al. Atherosclerosis Supplements 7 (2006) 53– 56
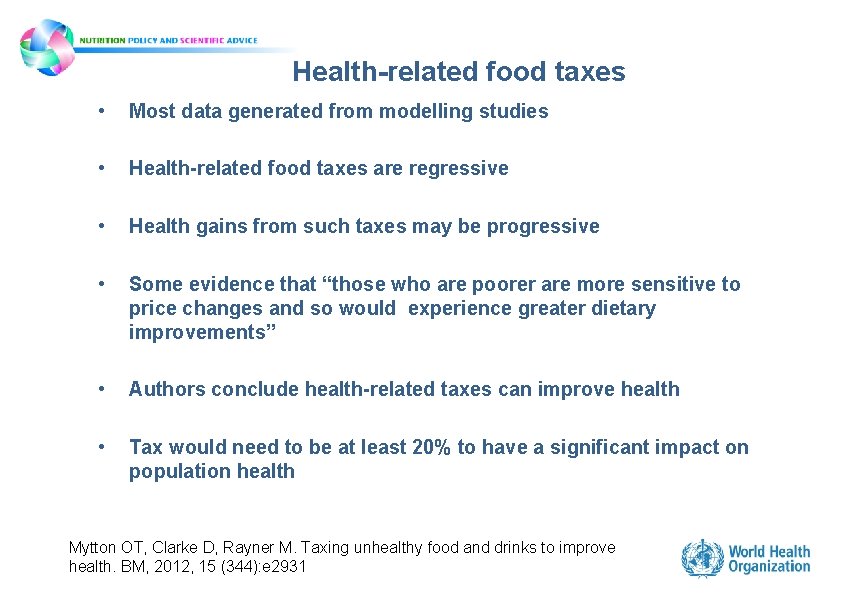
Health-related food taxes • Most data generated from modelling studies • Health-related food taxes are regressive • Health gains from such taxes may be progressive • Some evidence that “those who are poorer are more sensitive to price changes and so would experience greater dietary improvements” • Authors conclude health-related taxes can improve health • Tax would need to be at least 20% to have a significant impact on population health Mytton OT, Clarke D, Rayner M. Taxing unhealthy food and drinks to improve health. BM, 2012, 15 (344): e 2931
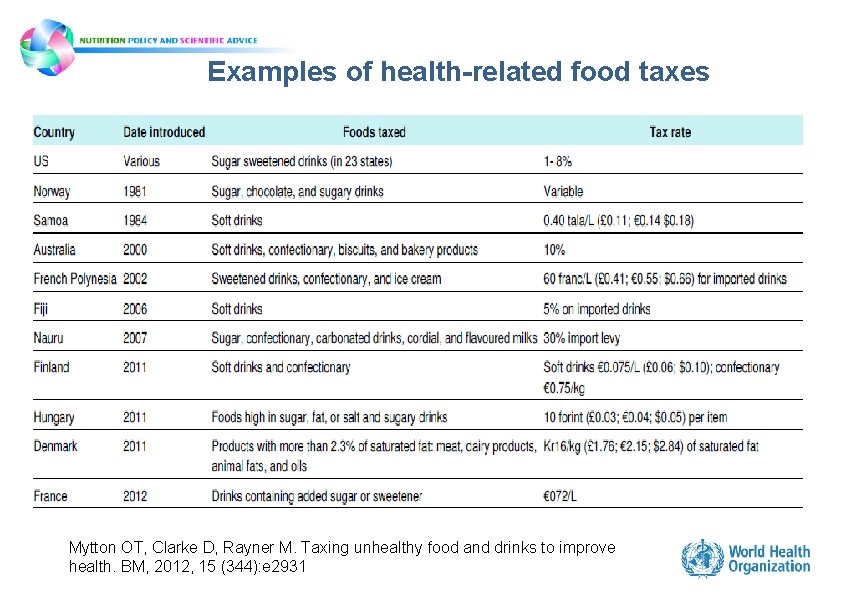
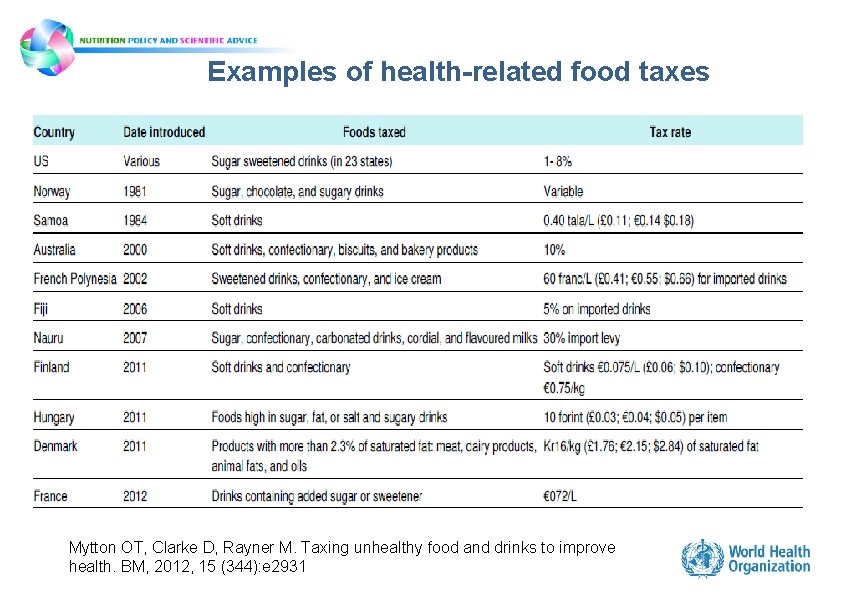
Examples of health-related food taxes Mytton OT, Clarke D, Rayner M. Taxing unhealthy food and drinks to improve health. BM, 2012, 15 (344): e 2931
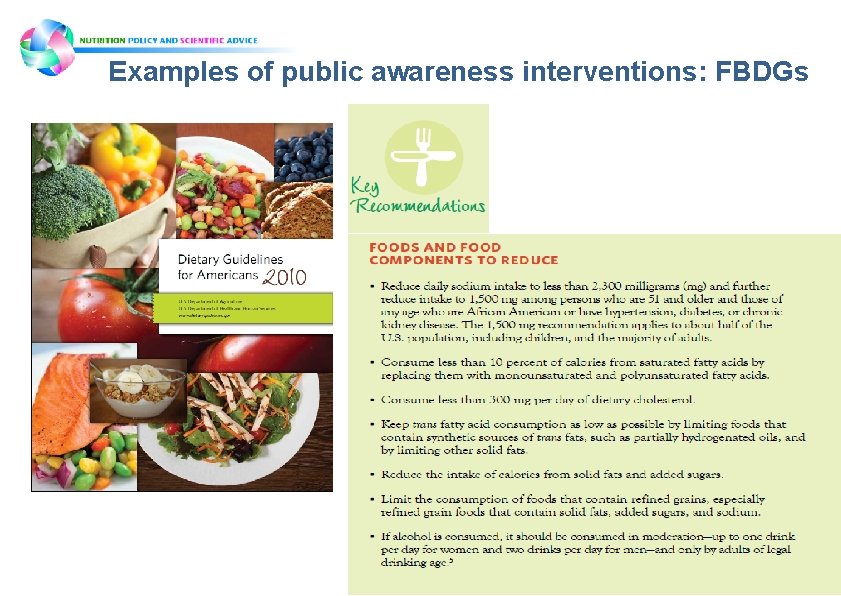
Examples of public awareness interventions: FBDGs
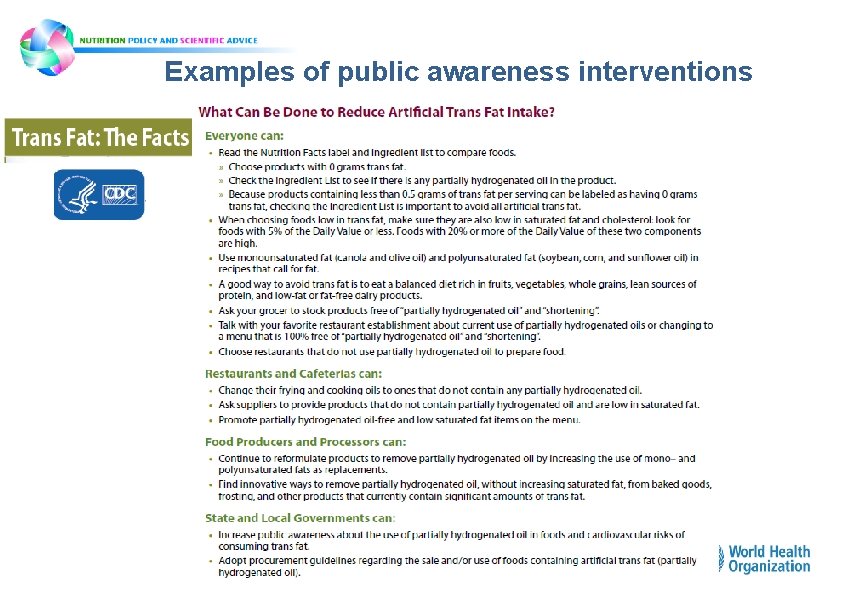
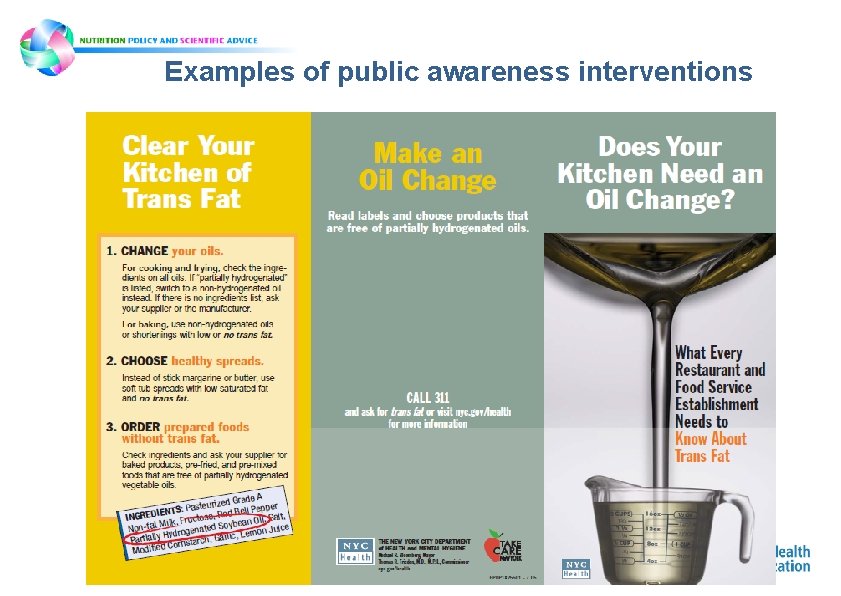
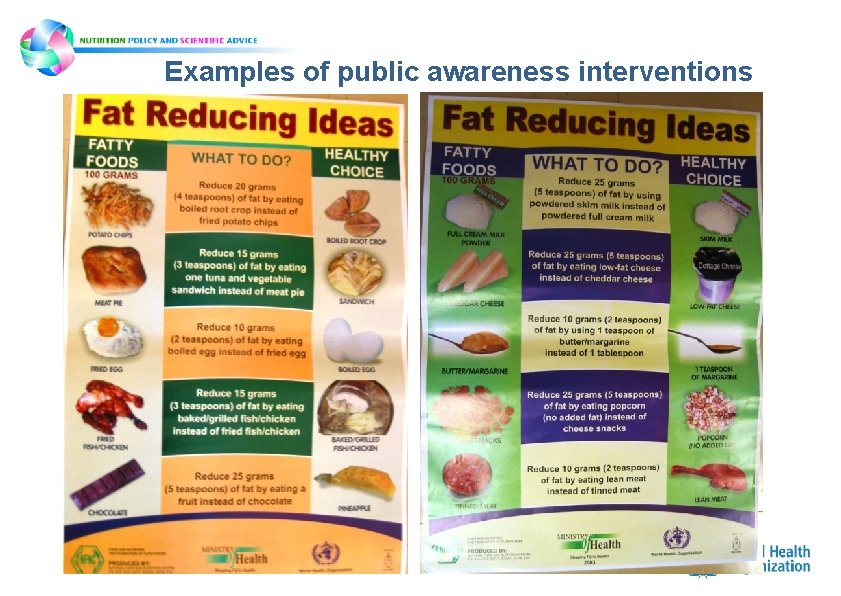
Examples of public awareness interventions
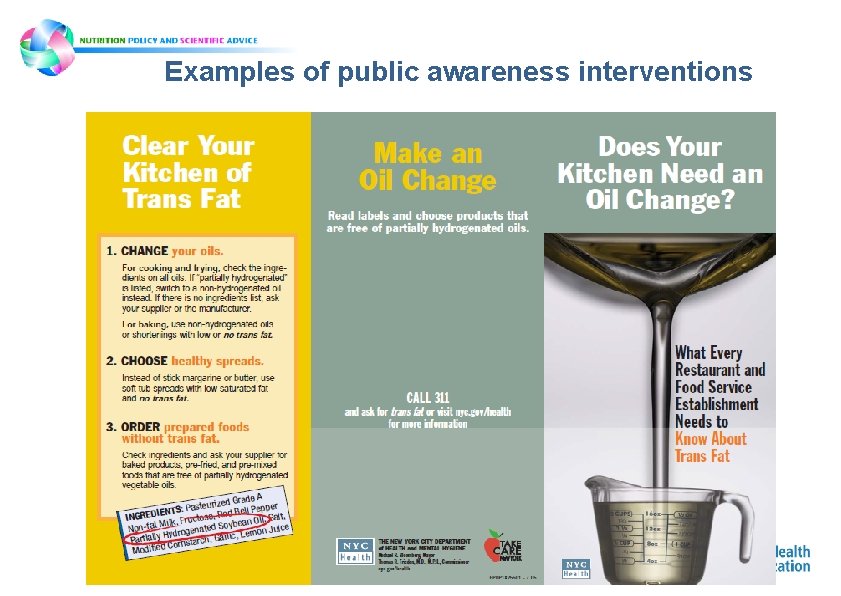
Examples of public awareness interventions
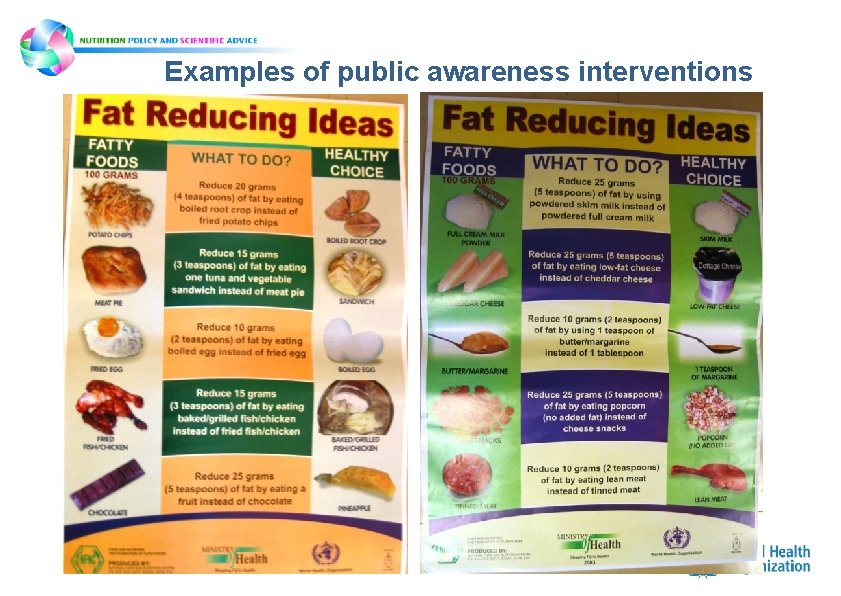
Examples of public awareness interventions

Nutrient Profiling and Labelling 7 th WHO-IUMSP International Seminar on the Public Health Aspects of Noncommunicable Dieases. Lausanne & Geneva, 3 -8 June 2013
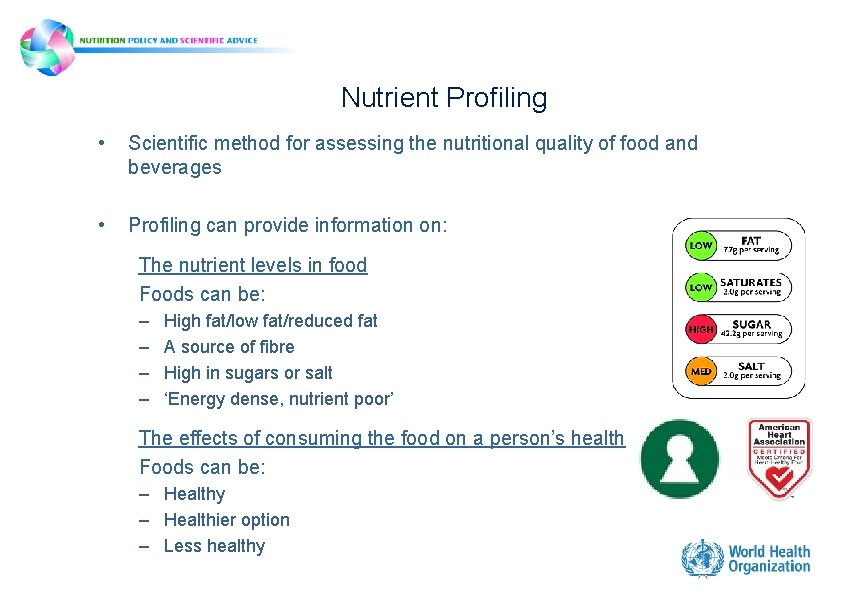
Nutrient Profiling • Scientific method for assessing the nutritional quality of food and beverages • Profiling can provide information on: The nutrient levels in food Foods can be: – – High fat/low fat/reduced fat A source of fibre High in sugars or salt ‘Energy dense, nutrient poor’ The effects of consuming the food on a person’s health Foods can be: – Healthy – Healthier option – Less healthy
Nutrient Profiling • Profiling is a tool that can be used to assist with: – Public health interventions aimed at improving diets – Influencing the wider environmental determinants of diets (e. g. the ways in which foods are marketed) • Public health interventions which benefit from nutrient profiling include those targeting: – – Marketing of food to children Product labelling (esp. ‘front-of- package’ labelling) Procurement of foods for public institutions (e. g. schools) Health claims • Nutrient profiling is compatible with food-based dietary guidelines (FBDGs) • Profiling can be used by national authorities in achieving dietary recommendations by complementing and supporting FBDGs in the regions and countries in which they are applied
Nutrient Profile models • Nutrient profile models: – Algorithms for classifying / ranking foods • Ad hoc development of models and their applications resulted in: – Inconsistencies – Confusion for target audience and consumers • Need for systematic evaluation and comparison of different models – WHO developing coordinated approach for developing (or adapting) nutrient profile models for use in applications (interventions) that may be integrated in a coherent public health strategy
WHO guiding principles and framework manual • Part 1. Background and guiding principles • Part 2. Framework manual for the development and adaptation of a nutrient profile model - Module 1: Planning the development or adaptation of a nutrient profile model - Module 2: Step by step procedures for developing or adapting a nutrient profile model - Module 3: Validating a nutrient profile model - Module 4: Implementation, monitoring and evaluation of applications involving nutrient profile models
Module 1: Planning the development or adaptation of a nutrient profile model • Identify nutrition-related public health problems and how they relate to existing dietary patterns • From all possible interventions, select those that require nutrient profiling
Module 2: Step by step procedures for developing or adapting a nutrient profile model • Define the purpose of the model (classification of single/multiple nutrients, target population, etc. ) • Decide which nutrients are to be addressed • Decide whether to use/adapt an existing model or develop a new one – Reflect on the purpose of the model and desired characteristics – Identify and consider whethere are other relevant issues (e. g. cultural considerations) – Review all possible models and develop a short list of potentially compatible ones
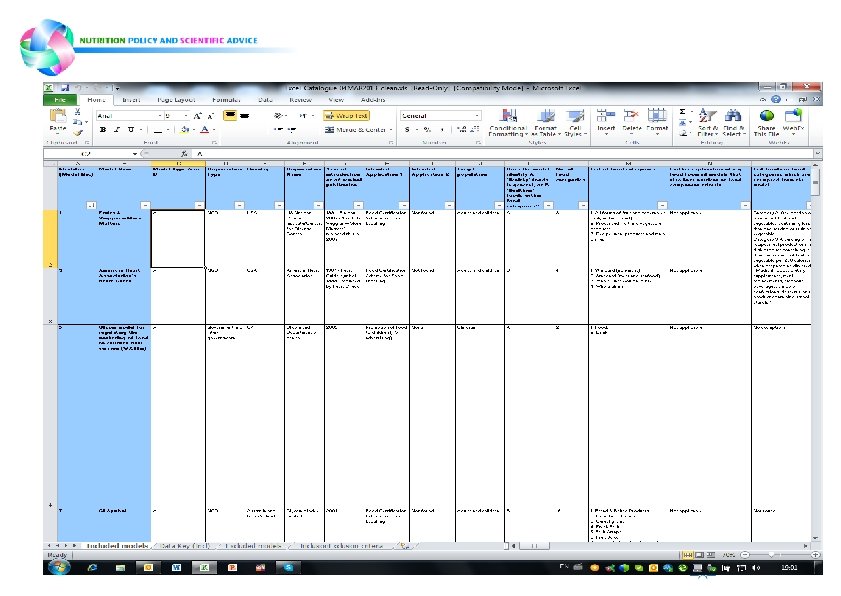
Module 2: Step by step procedures for developing or adapting a nutrient profile model Development of tools for reviewing and adapting nutrition profile models • • • 118 models identified 63 met the inclusion criteria Only one third of included models have been validated in any way
Module 3: Validating a nutrient profile model • Lack of a “gold standard” in terms of defining a healthy food • Comparing classifications produced with the nutrition profile model in question with those from another model that has been designed for similar purposes and has already been validated • Identify a small number of “indicator” foods that have already been identified as healthy/unhealthy, etc. and assess whether classification by the model agrees with what has been established • Other more complicated methods
Module 4: Implementation, monitoring and evaluation of applications involving nutrient profile models • Evaluation might include – Assessing impact on targeted activity itself (e. g. success of an application/intervention aimed at identifying healthy foods with front of package labelling might be determined by increased purchase and/or consumption of the labelled foods) – Assessing impact of the application/intervention on dietary quality or dietrelated health outcomes (e. g. rates of obesity, raised cholesterol, etc. )
Field-testing of WHO nutrient profiling manual
Salt reduction strategies
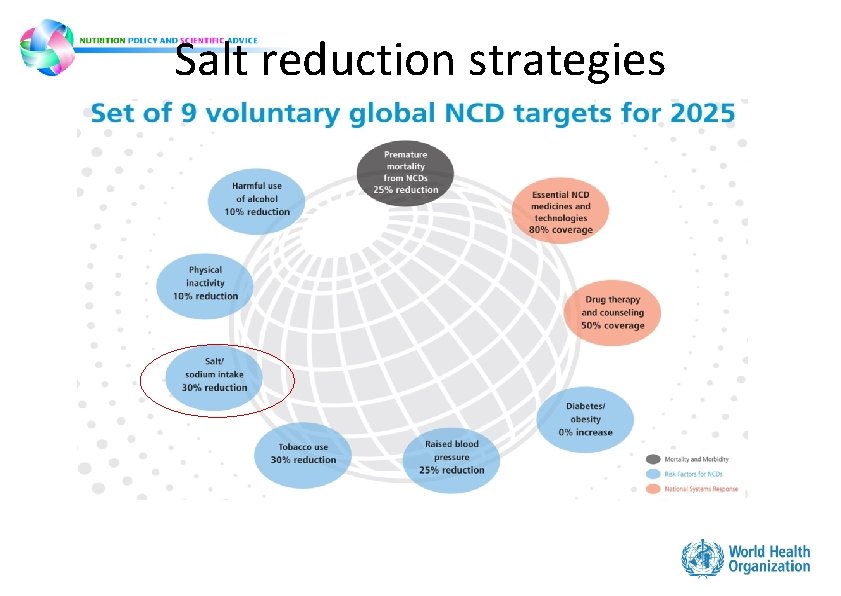
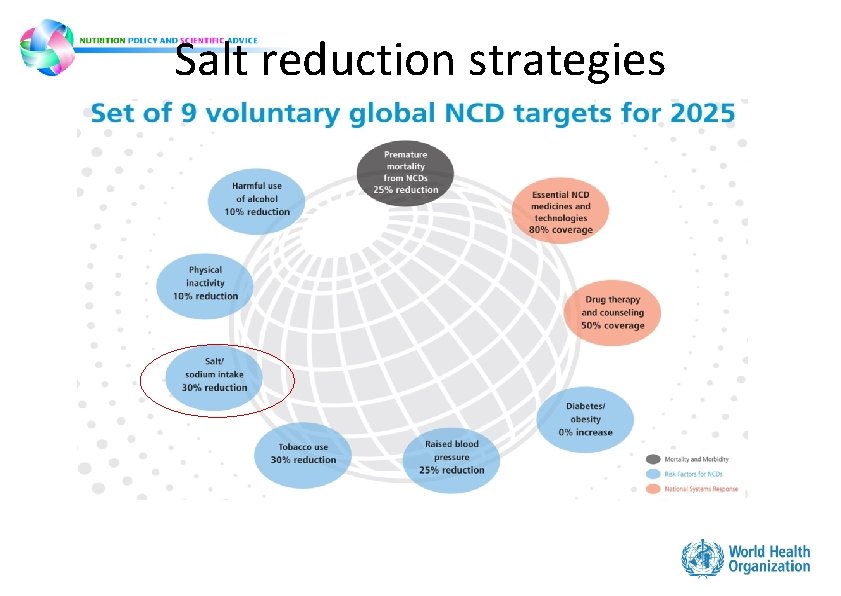
Salt reduction strategies
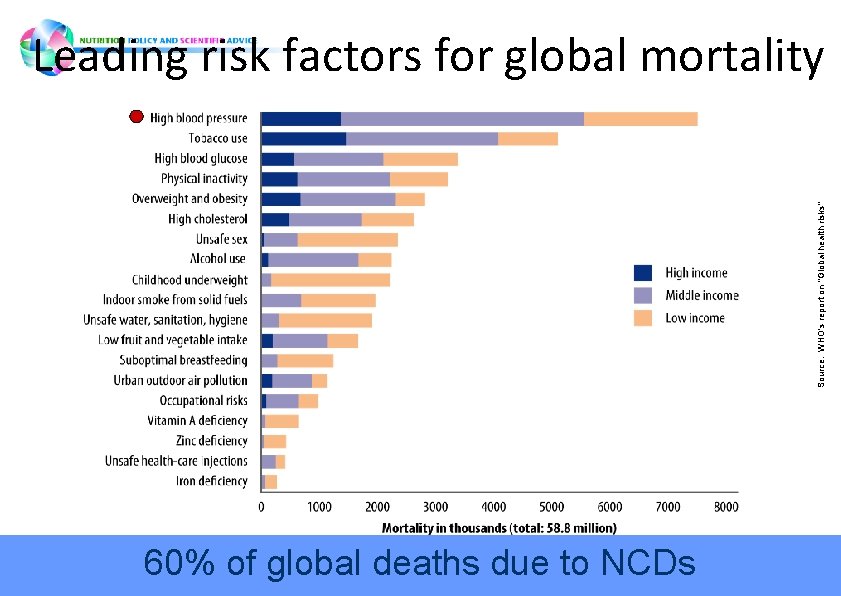
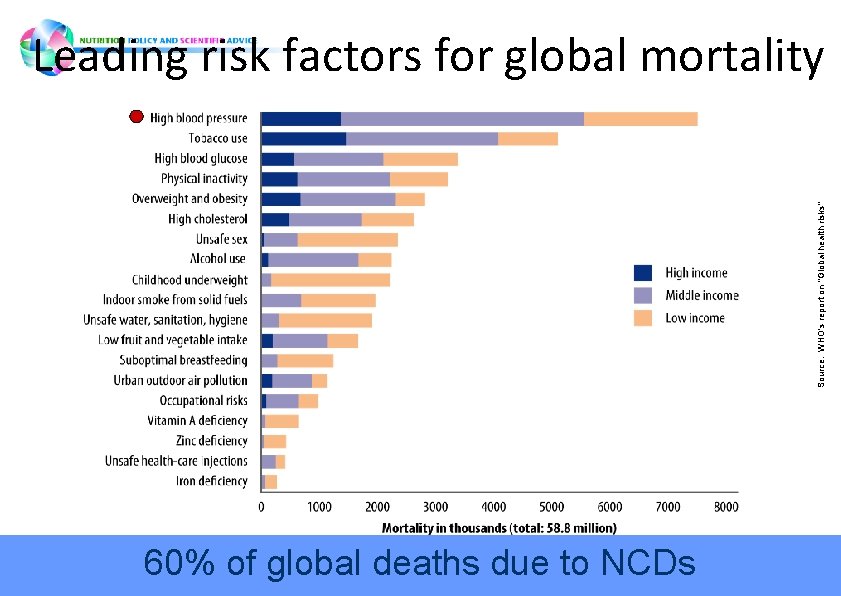
Source: WHO's report on "Global health risks" Leading risk factors for global mortality 60% of global deaths due to NCDs
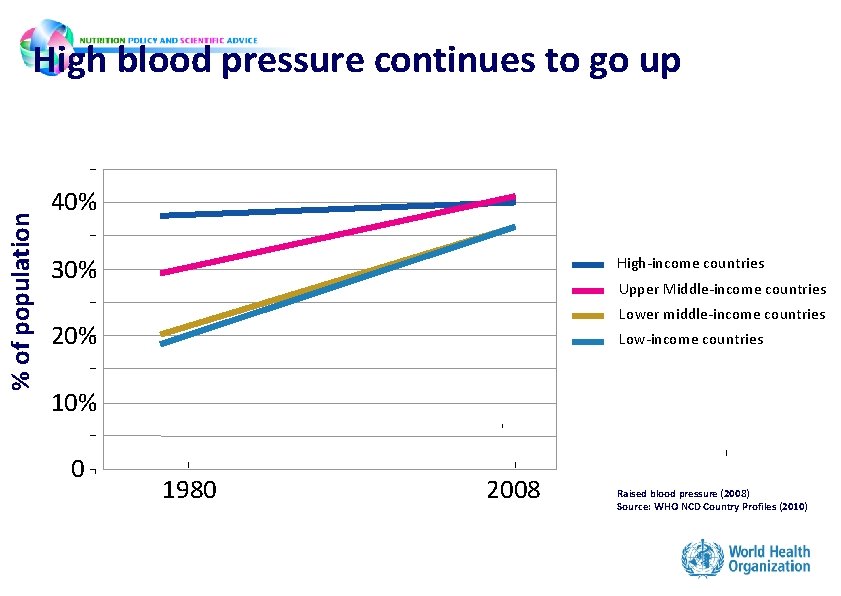
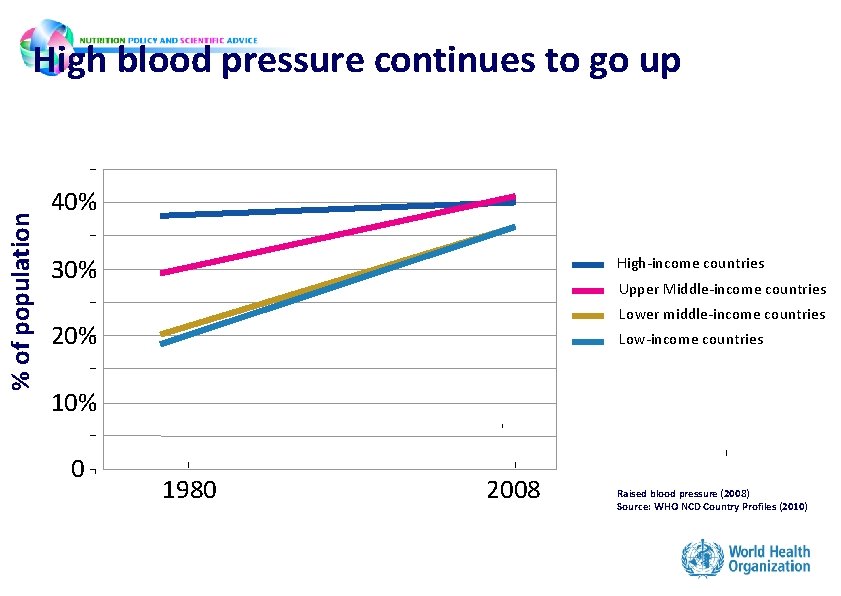
% of population High blood pressure continues to go up 40% 30% High-income countries Upper Middle-income countries Lower middle-income countries 20% Low-income countries 10% 0 1980 2008 Raised blood pressure (2008) Source: WHO NCD Country Profiles (2010)
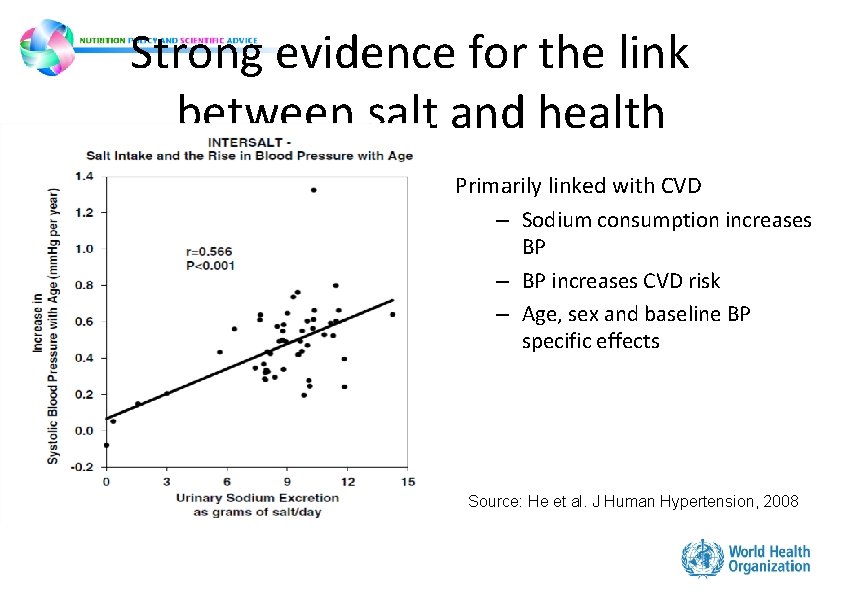
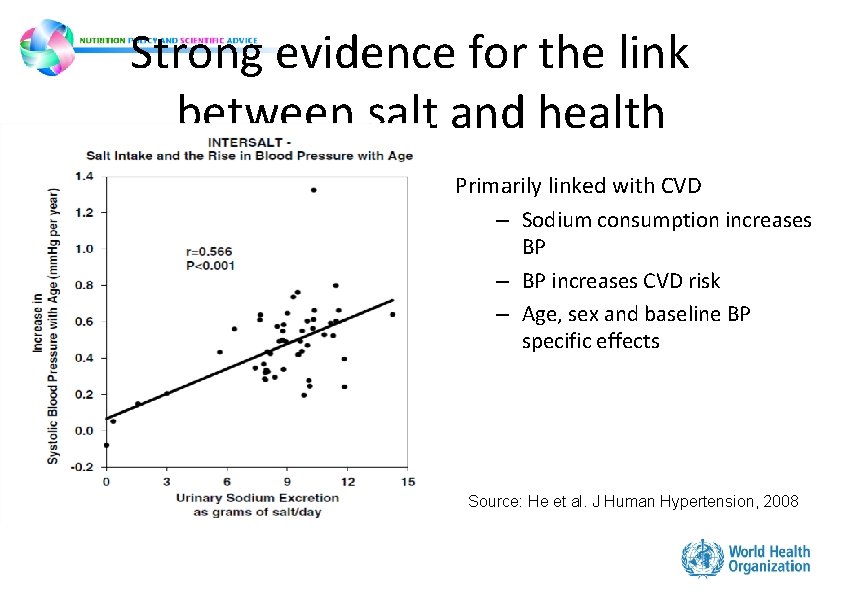
Strong evidence for the link between salt and health Primarily linked with CVD – Sodium consumption increases BP – BP increases CVD risk – Age, sex and baseline BP specific effects Source: He et al. J Human Hypertension, 2008
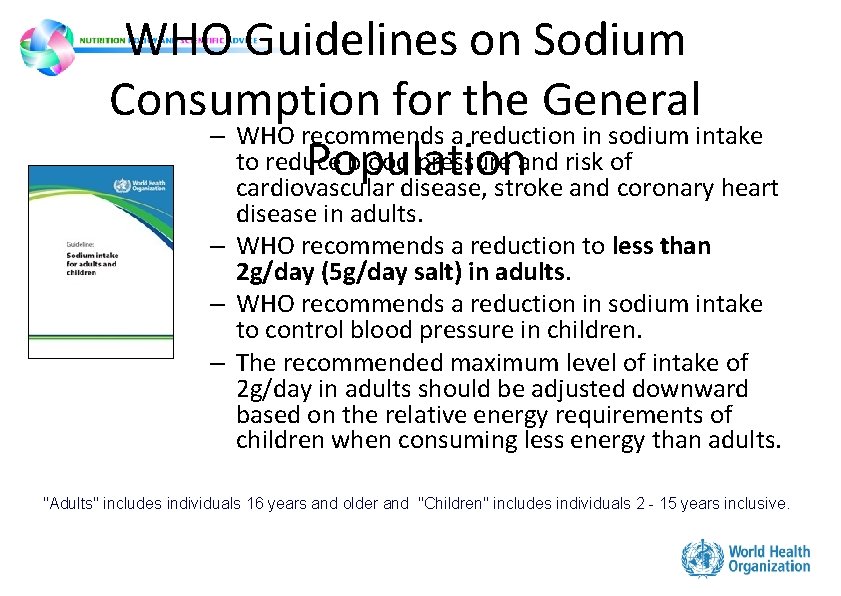
WHO Guidelines on Sodium Consumption for the General – WHO recommends a reduction in sodium intake to reduce blood pressure and risk of Population cardiovascular disease, stroke and coronary heart disease in adults. – WHO recommends a reduction to less than 2 g/day (5 g/day salt) in adults. – WHO recommends a reduction in sodium intake to control blood pressure in children. – The recommended maximum level of intake of 2 g/day in adults should be adjusted downward based on the relative energy requirements of children when consuming less energy than adults. "Adults" includes individuals 16 years and older and "Children" includes individuals 2 - 15 years inclusive.
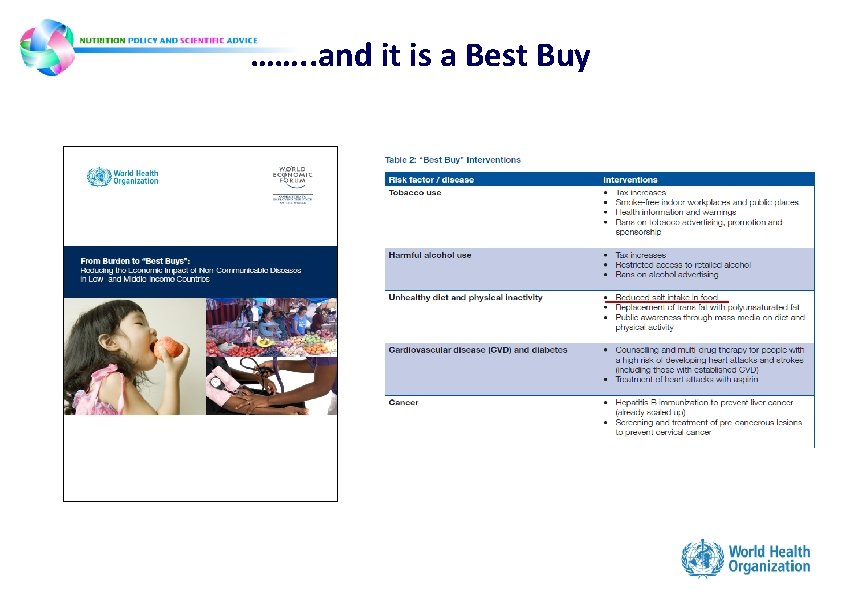
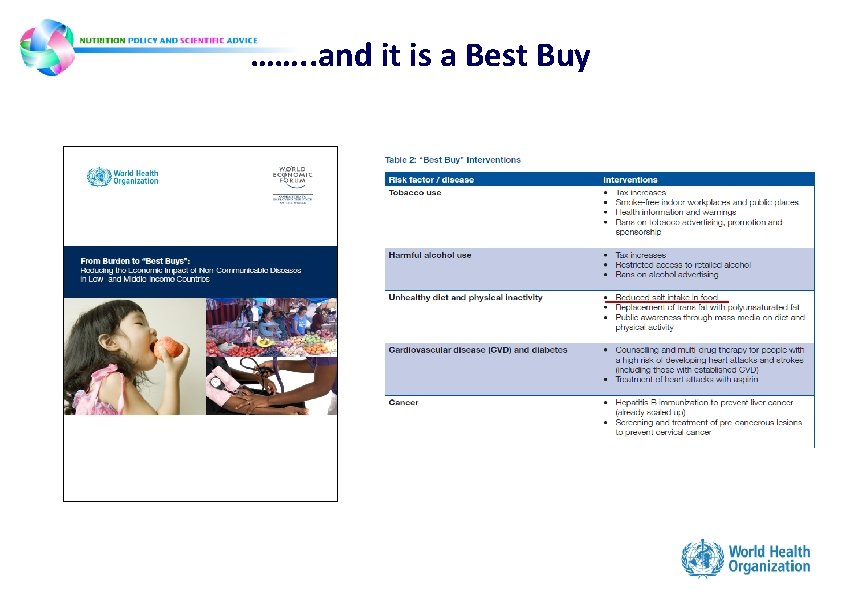
……. . and it is a Best Buy
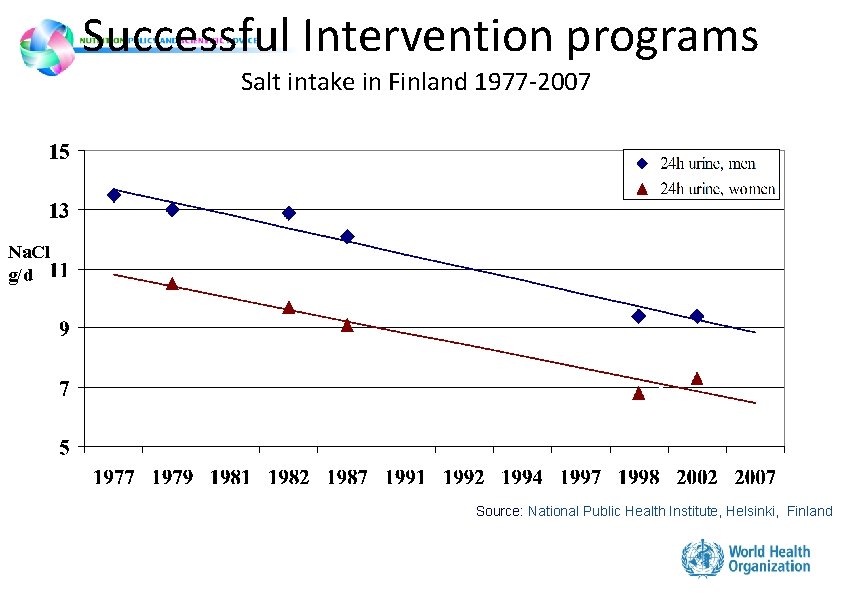
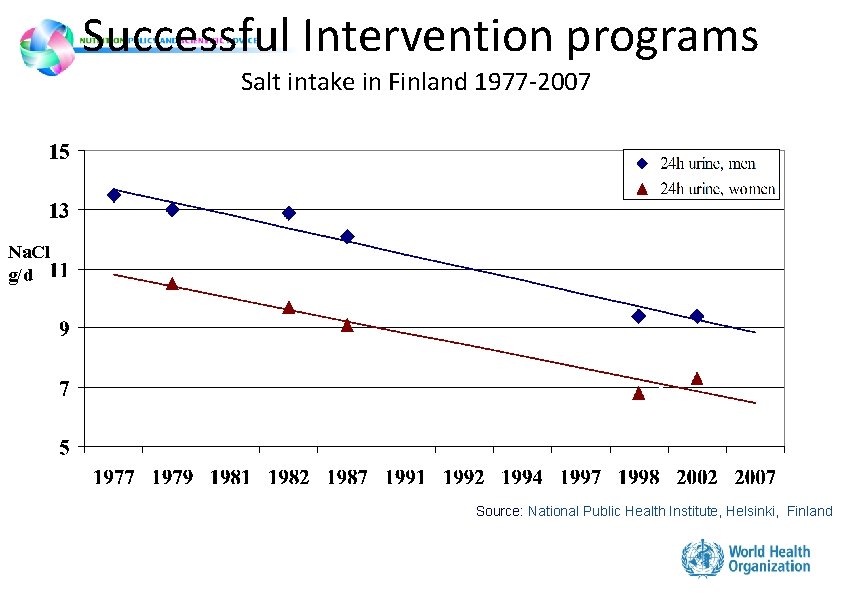
Successful Intervention programs Salt intake in Finland 1977 -2007 Na. Cl g/d Source: National Public Health Institute, Helsinki, Finland
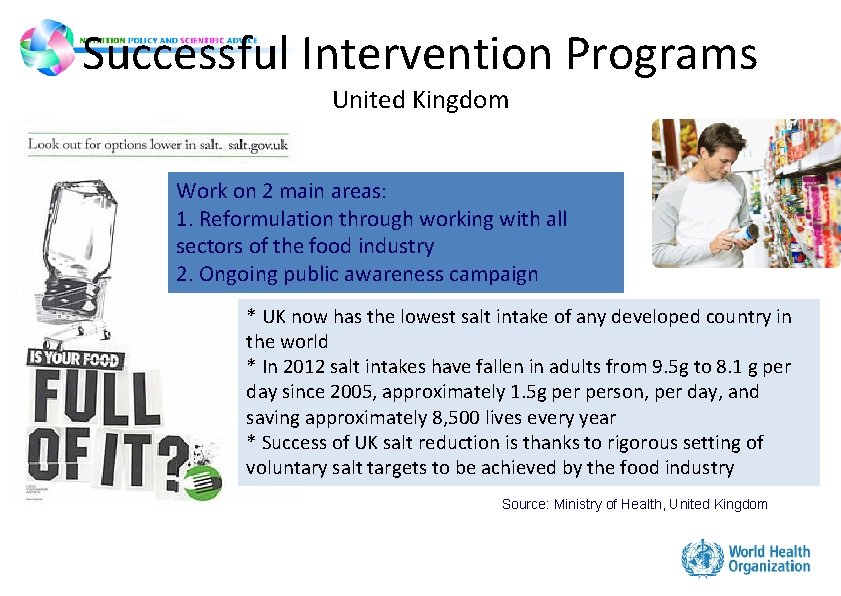
Successful Intervention Programs United Kingdom Work on 2 main areas: 1. Reformulation through working with all sectors of the food industry 2. Ongoing public awareness campaign * UK now has the lowest salt intake of any developed country in the world * In 2012 salt intakes have fallen in adults from 9. 5 g to 8. 1 g per day since 2005, approximately 1. 5 g person, per day, and saving approximately 8, 500 lives every year * Success of UK salt reduction is thanks to rigorous setting of voluntary salt targets to be achieved by the food industry Source: Ministry of Health, United Kingdom
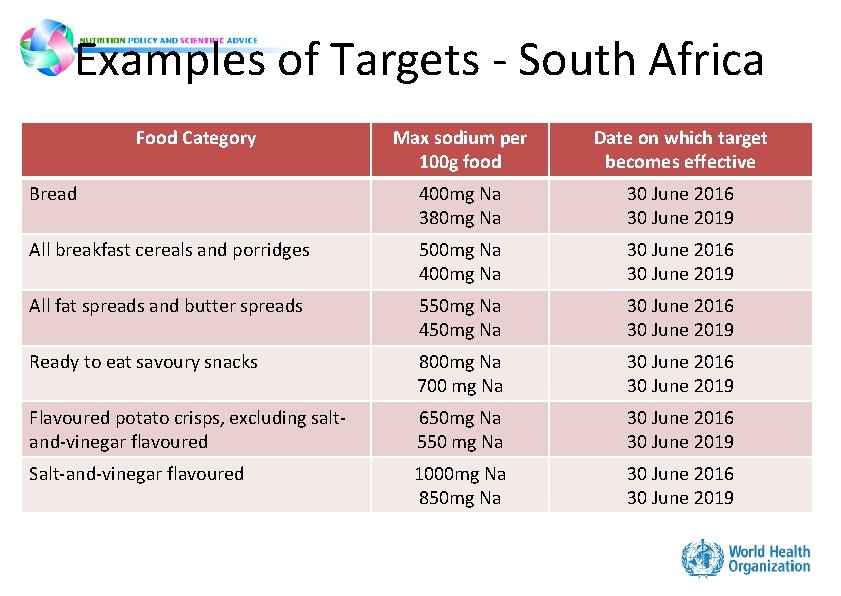
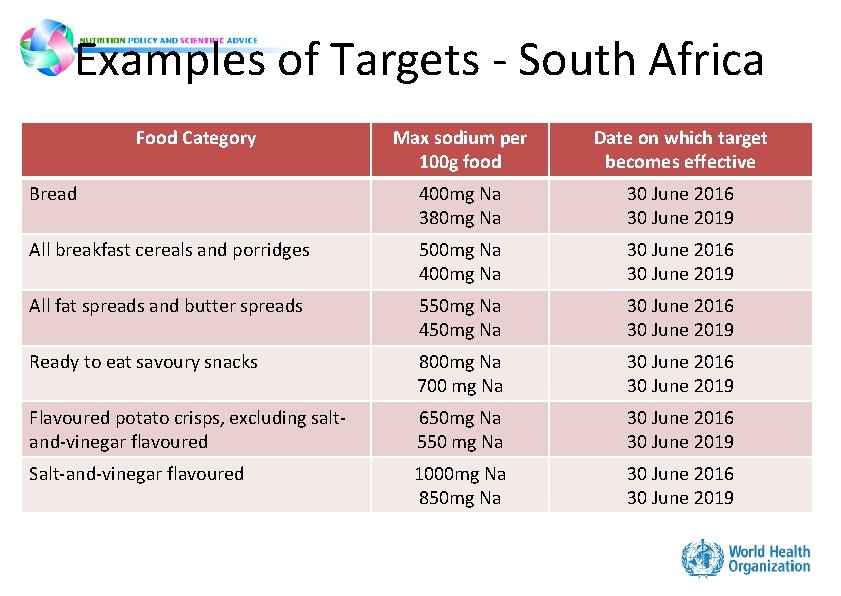
Examples of Targets - South Africa Food Category Max sodium per 100 g food Date on which target becomes effective Bread 400 mg Na 380 mg Na 30 June 2016 30 June 2019 All breakfast cereals and porridges 500 mg Na 400 mg Na 30 June 2016 30 June 2019 All fat spreads and butter spreads 550 mg Na 450 mg Na 30 June 2016 30 June 2019 Ready to eat savoury snacks 800 mg Na 700 mg Na 30 June 2016 30 June 2019 Flavoured potato crisps, excluding saltand-vinegar flavoured 650 mg Na 550 mg Na 30 June 2016 30 June 2019 Salt-and-vinegar flavoured 1000 mg Na 850 mg Na 30 June 2016 30 June 2019
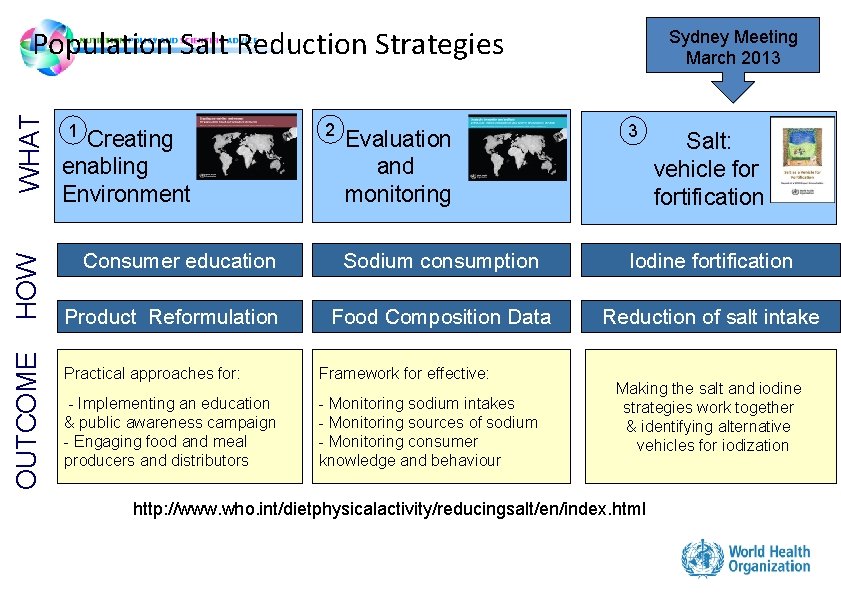
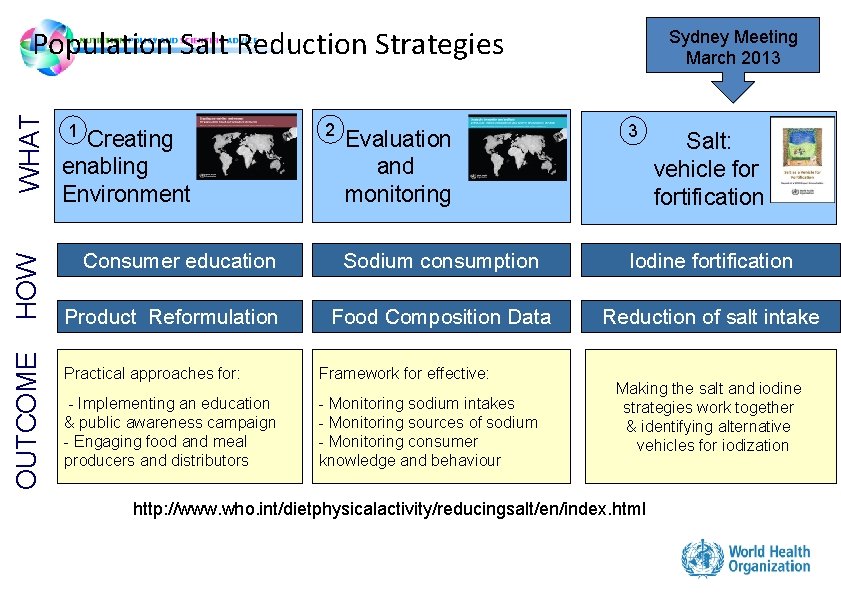
OUTCOME HOW WHAT Population Salt Reduction Strategies 1 Creating enabling Environment Consumer education Product Reformulation 2 Sydney Meeting March 2013 Evaluation and monitoring 3 Sodium consumption Iodine fortification Food Composition Data Reduction of salt intake Practical approaches for: Framework for effective: - Implementing an education & public awareness campaign - Engaging food and meal producers and distributors - Monitoring sodium intakes - Monitoring sources of sodium - Monitoring consumer knowledge and behaviour Salt: vehicle fortification Making the salt and iodine strategies work together & identifying alternative vehicles for iodization http: //www. who. int/dietphysicalactivity/reducingsalt/en/index. html
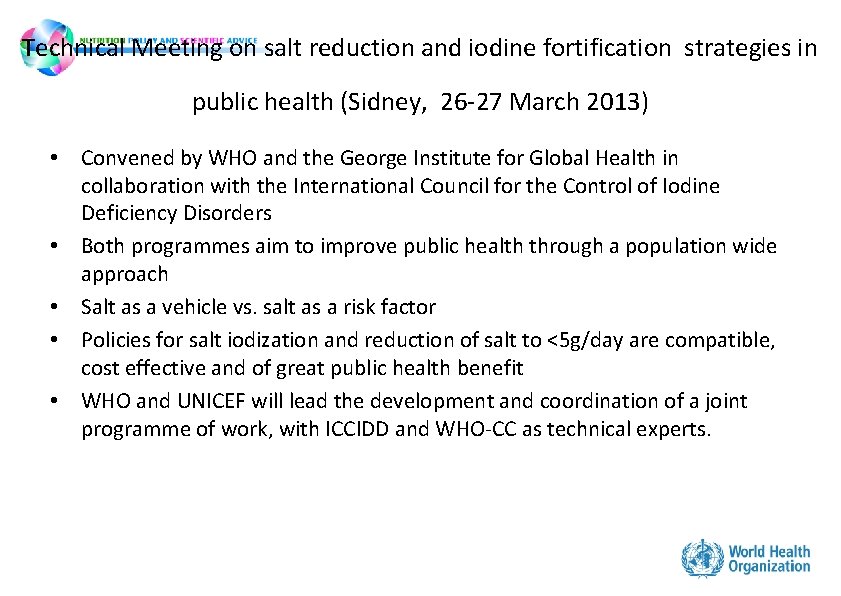
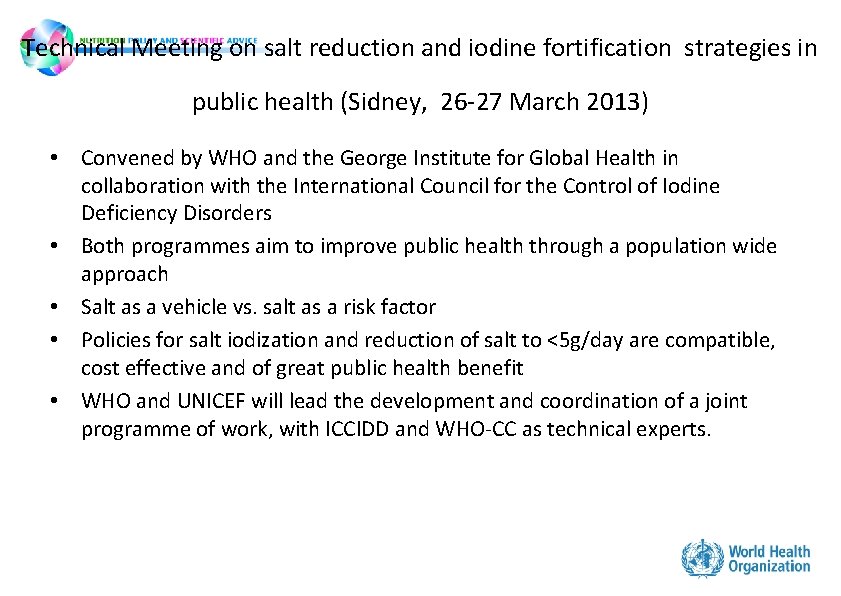
Technical Meeting on salt reduction and iodine fortification strategies in public health (Sidney, 26 -27 March 2013) • Convened by WHO and the George Institute for Global Health in collaboration with the International Council for the Control of Iodine Deficiency Disorders • Both programmes aim to improve public health through a population wide approach • Salt as a vehicle vs. salt as a risk factor • Policies for salt iodization and reduction of salt to <5 g/day are compatible, cost effective and of great public health benefit • WHO and UNICEF will lead the development and coordination of a joint programme of work, with ICCIDD and WHO-CC as technical experts.
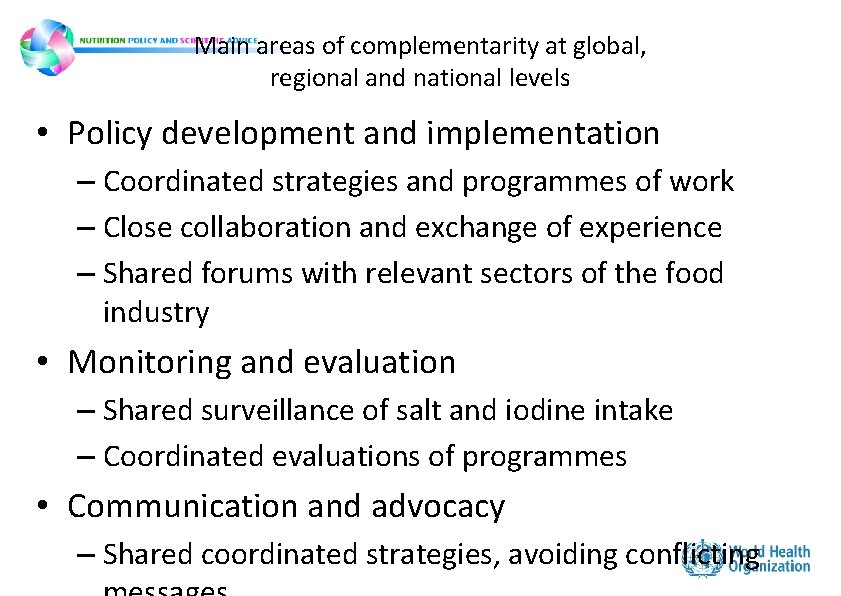
Main areas of complementarity at global, regional and national levels • Policy development and implementation – Coordinated strategies and programmes of work – Close collaboration and exchange of experience – Shared forums with relevant sectors of the food industry • Monitoring and evaluation – Shared surveillance of salt and iodine intake – Coordinated evaluations of programmes • Communication and advocacy – Shared coordinated strategies, avoiding conflicting
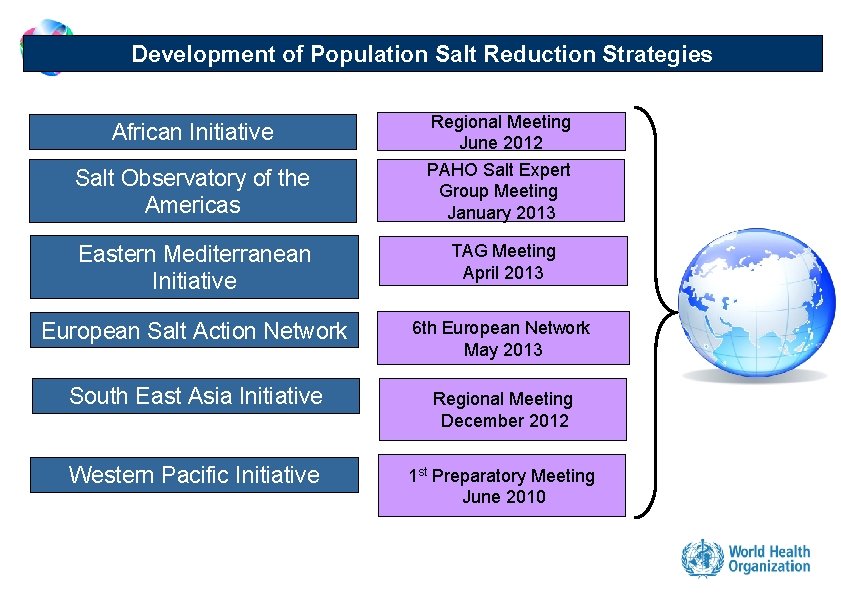
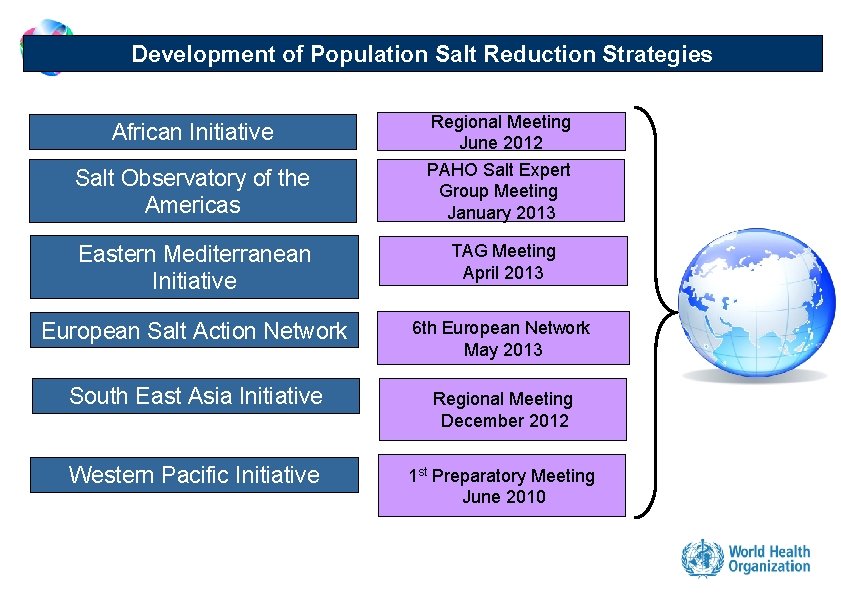
Development of Population Salt Reduction Strategies African Initiative Salt Observatory of the Americas Regional Meeting June 2012 PAHO Salt Expert Group Meeting January 2013 Eastern Mediterranean Initiative TAG Meeting April 2013 European Salt Action Network 6 th European Network May 2013 South East Asia Initiative Regional Meeting December 2012 Western Pacific Initiative 1 st Preparatory Meeting June 2010
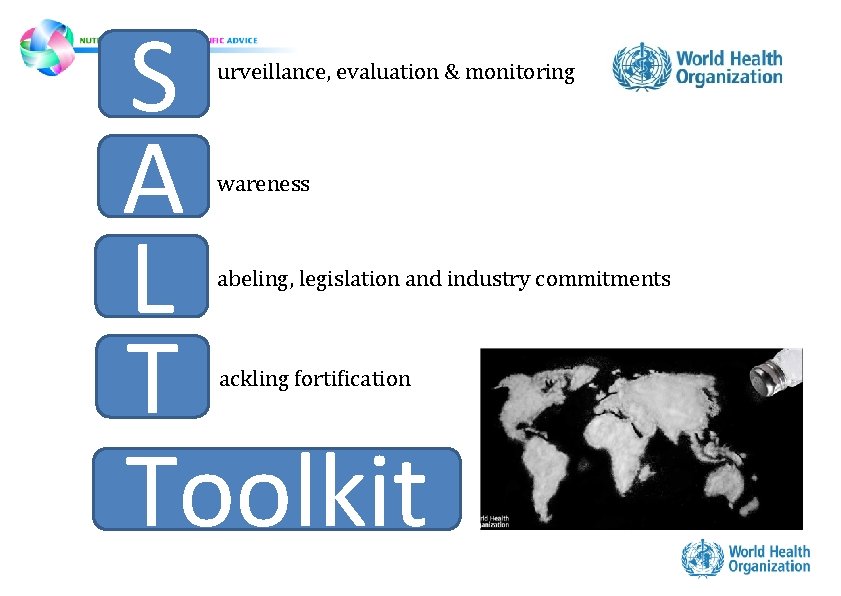
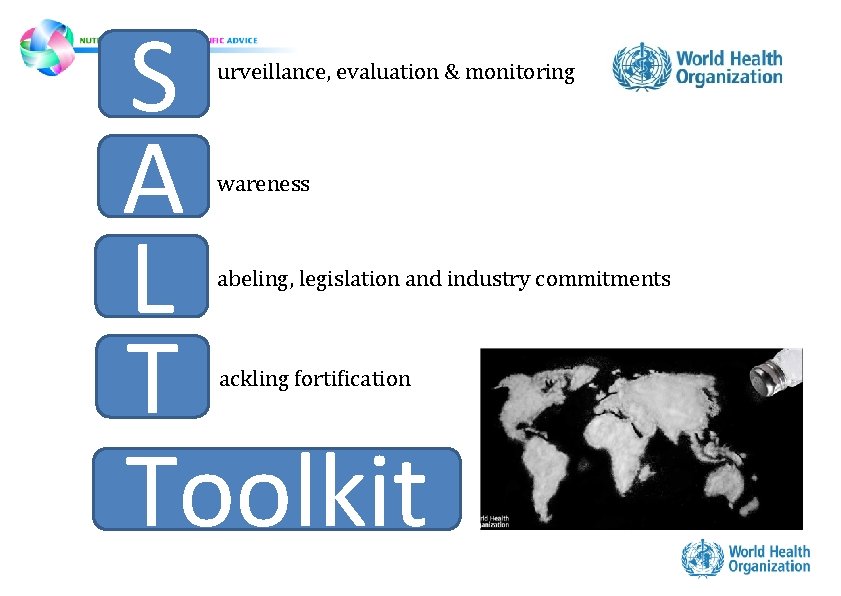
S A L T Toolkit urveillance, evaluation & monitoring wareness abeling, legislation and industry commitments ackling fortification
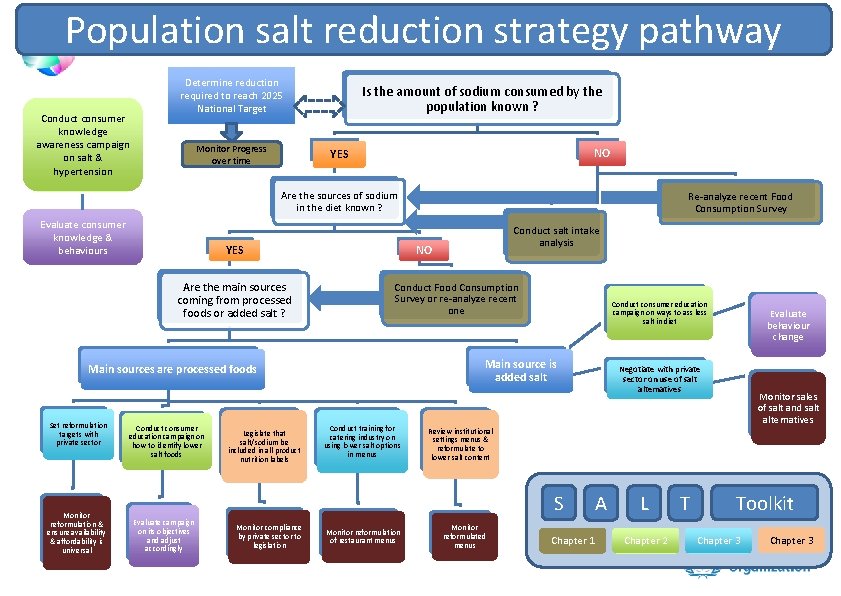
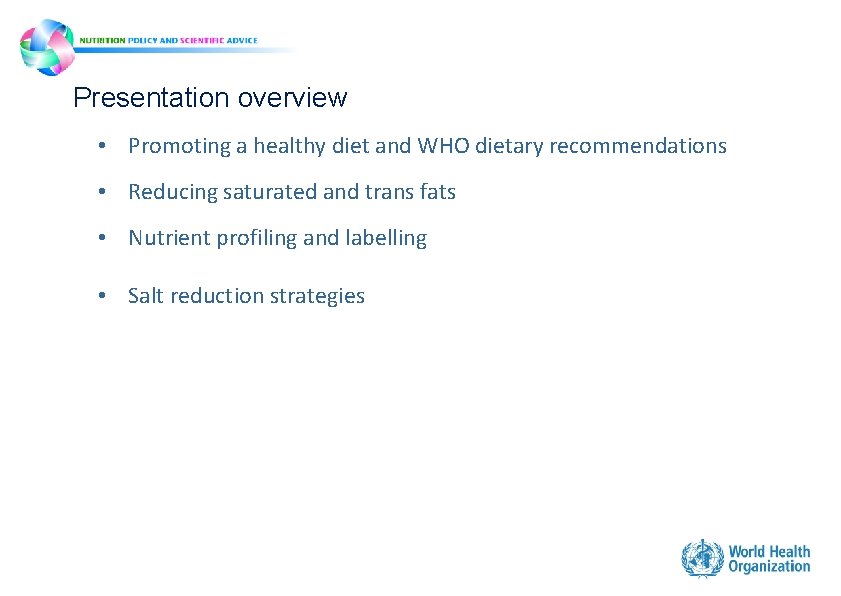
Population salt reduction strategy pathway Conduct consumer knowledge awareness campaign on salt & hypertension Determine reduction required to reach 2025 National Target Monitor Progress over time Is the amount of sodium consumed by the population known ? NO YES Are the sources of sodium in the diet known ? Evaluate consumer knowledge & behaviours YES Are the main sources coming from processed foods or added salt ? Monitor reformulation & ensure availability & affordability is universal Conduct consumer education campaign on how to identify lower salt foods Legislate that salt/sodium be included in all product nutrition labels Conduct salt intake analysis NO Conduct Food Consumption Survey or re-analyze recent one Conduct consumer education campaign on ways to ass less salt in diet Main source is added salt Main sources are processed foods Set reformulation targets with private sector Re-analyze recent Food Consumption Survey Conduct training for catering industry on using lower salt options in menus Monitor compliance by private sector to legislation Monitor reformulation of restaurant menus Negotiate with private sector on use of salt alternatives Monitor sales of salt and salt alternatives Review institutional settings menus & reformulate to lower salt content S Evaluate campaign on its objectives and adjust accordingly Evaluate behaviour change Monitor reformulated menus Chapter 1 A L Chapter 2 T Toolkit Chapter 3
Thank you