Medieval Medicine Key Points Ancient Ideas Hippocrates Galen
- Slides: 5
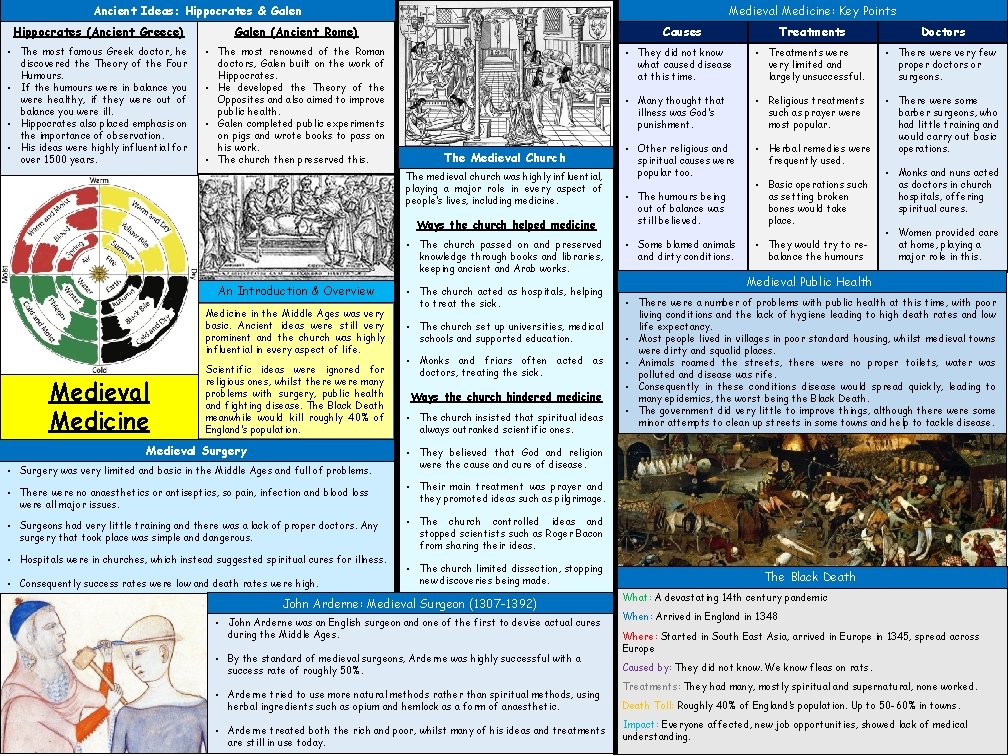
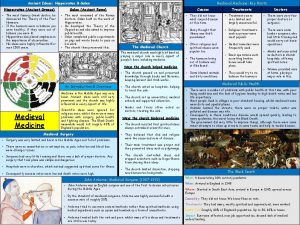
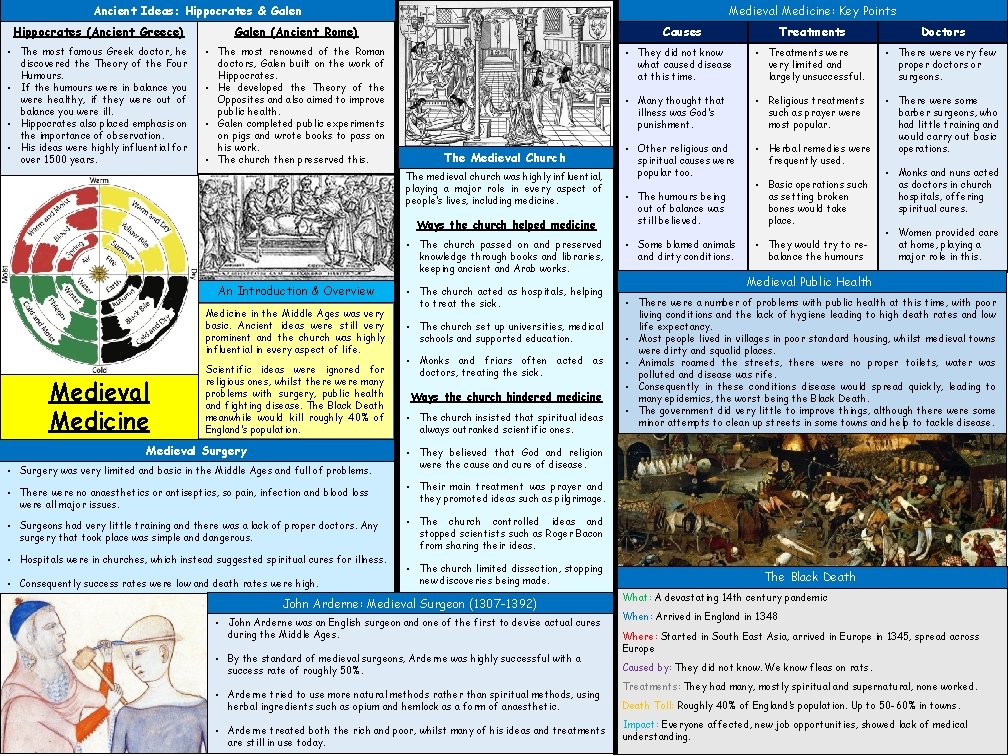
Medieval Medicine: Key Points Ancient Ideas: Hippocrates & Galen Hippocrates (Ancient Greece) Galen (Ancient Rome) • The most famous Greek doctor, he discovered the Theory of the Four Humours. • If the humours were in balance you were healthy, if they were out of balance you were ill. • Hippocrates also placed emphasis on the importance of observation. • His ideas were highly influential for over 1500 years. • The most renowned of the Roman doctors, Galen built on the work of Hippocrates. • He developed the Theory of the Opposites and also aimed to improve public health. • Galen completed public experiments on pigs and wrote books to pass on his work. • The church then preserved this. Causes The Medieval Church The medieval church was highly influential, playing a major role in every aspect of people’s lives, including medicine. Ways the church helped medicine • The church passed on and preserved knowledge through books and libraries, keeping ancient and Arab works. An Introduction & Overview Medicine in the Middle Ages was very basic. Ancient ideas were still very prominent and the church was highly influential in every aspect of life. Medieval Medicine z Scientific ideas were ignored for religious ones, whilst there were many problems with surgery, public health and fighting disease. The Black Death meanwhile would kill roughly 40% of England’s population. Medieval Surgery • Surgery was very limited and basic in the Middle Ages and full of problems. • There were no anaesthetics or antiseptics, so pain, infection and blood loss were all major issues. • Surgeons had very little training and there was a lack of proper doctors. Any surgery that took place was simple and dangerous. • Hospitals were in churches, which instead suggested spiritual cures for illness. • Consequently success rates were low and death rates were high. • The church acted as hospitals, helping to treat the sick. • The church set up universities, medical schools and supported education. • Monks and friars often acted as doctors, treating the sick. Ways the church hindered medicine • The church insisted that spiritual ideas always outranked scientific ones. Treatments Doctors • They did not know what caused disease at this time. • Treatments were very limited and largely unsuccessful. • There were very few proper doctors or surgeons. • Many thought that illness was God’s punishment. • Religious treatments such as prayer were most popular. • Other religious and spiritual causes were popular too. • Herbal remedies were frequently used. • There were some barber surgeons, who had little training and would carry out basic operations. • The humours being out of balance was still believed. • Basic operations such as setting broken bones would take place. • Some blamed animals and dirty conditions. • They would try to rebalance the humours • Monks and nuns acted as doctors in church hospitals, offering spiritual cures. • Women provided care at home, playing a major role in this. Medieval Public Health • There were a number of problems with public health at this time, with poor living conditions and the lack of hygiene leading to high death rates and low life expectancy. • Most people lived in villages in poor standard housing, whilst medieval towns were dirty and squalid places. • Animals roamed the streets, there were no proper toilets, water was polluted and disease was rife. • Consequently in these conditions disease would spread quickly, leading to many epidemics, the worst being the Black Death. • The government did very little to improve things, although there were some minor attempts to clean up streets in some towns and help to tackle disease. • They believed that God and religion were the cause and cure of disease. • Their main treatment was prayer and they promoted ideas such as pilgrimage. • The church controlled ideas and stopped scientists such as Roger Bacon from sharing their ideas. • The church limited dissection, stopping new discoveries being made. John Arderne: Medieval Surgeon (1307 -1392) • John Arderne was an English surgeon and one of the first to devise actual cures during the Middle Ages. • By the standard of medieval surgeons, Arderne was highly successful with a success rate of roughly 50%. • Arderne tried to use more natural methods rather than spiritual methods, using herbal ingredients such as opium and hemlock as a form of anaesthetic. • Arderne treated both the rich and poor, whilst many of his ideas and treatments are still in use today. The Black Death What: A devastating 14 th century pandemic When: Arrived in England in 1348 Where: Started in South East Asia, arrived in Europe in 1345, spread across Europe Caused by: They did not know. We know fleas on rats. Treatments: They had many, mostly spiritual and supernatural, none worked. Death Toll: Roughly 40% of England’s population. Up to 50 -60% in towns. Impact: Everyone affected, new job opportunities, showed lack of medical understanding.
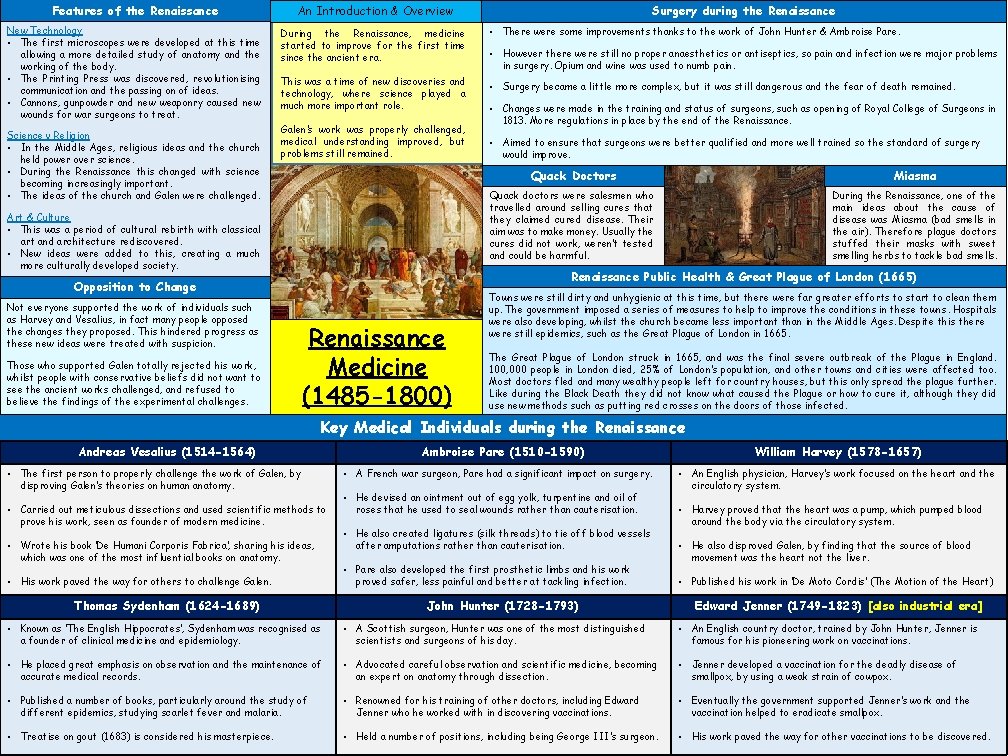
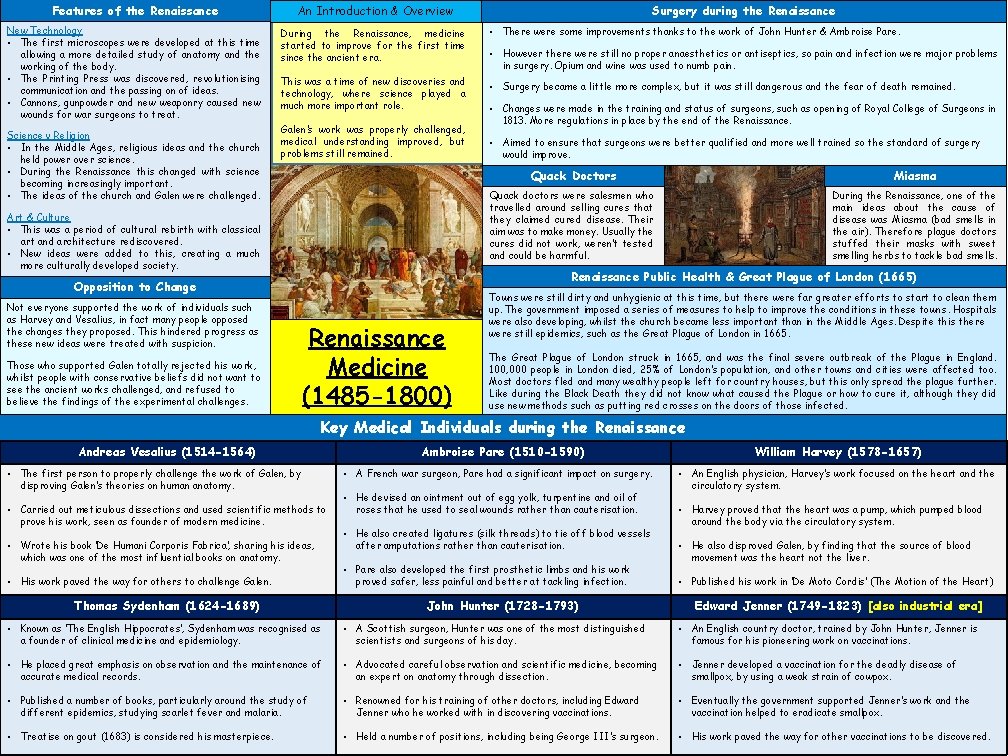
Features of the Renaissance An Introduction & Overview New Technology • The first microscopes were developed at this time allowing a more detailed study of anatomy and the working of the body. • The Printing Press was discovered, revolutionising communication and the passing on of ideas. • Cannons, gunpowder and new weaponry caused new wounds for war surgeons to treat. During the Renaissance, medicine started to improve for the first time since the ancient era. Science v Religion • In the Middle Ages, religious ideas and the church held power over science. • During the Renaissance this changed with science becoming increasingly important. • The ideas of the church and Galen were challenged. This was a time of new discoveries and technology, where science played a much more important role. Galen’s work was properly challenged, medical understanding improved, but problems still remained. Art & Culture • This was a period of cultural rebirth with classical art and architecture rediscovered. • New ideas were added to this, creating a much more culturally developed society. Those who supported Galen totally rejected his work, whilst people with conservative beliefs did not want to see the ancient works challenged, and refused to believe the findings of the experimental challenges. • There were some improvements thanks to the work of John Hunter & Ambroise Pare. • However there were still no proper anaesthetics or antiseptics, so pain and infection were major problems in surgery. Opium and wine was used to numb pain. • Surgery became a little more complex, but it was still dangerous and the fear of death remained. • Changes were made in the training and status of surgeons, such as opening of Royal College of Surgeons in 1813. More regulations in place by the end of the Renaissance. • Aimed to ensure that surgeons were better qualified and more well trained so the standard of surgery would improve. Quack Doctors Miasma Quack doctors were salesmen who travelled around selling cures that they claimed cured disease. Their aim was to make money. Usually the cures did not work, weren’t tested and could be harmful. During the Renaissance, one of the main ideas about the cause of disease was Miasma (bad smells in the air). Therefore plague doctors stuffed their masks with sweet smelling herbs to tackle bad smells. Renaissance Public Health & Great Plague of London (1665) Opposition to Change Not everyone supported the work of individuals such as Harvey and Vesalius, in fact many people opposed the changes they proposed. This hindered progress as these new ideas were treated with suspicion. Surgery during the Renaissance Medicine (1485 -1800) Towns were still dirty and unhygienic at this time, but there were far greater efforts to start to clean them up. The government imposed a series of measures to help to improve the conditions in these towns. Hospitals were also developing, whilst the church became less important than in the Middle Ages. Despite this there were still epidemics, such as the Great Plague of London in 1665. The Great Plague of London struck in 1665, and was the final severe outbreak of the Plague in England. 100, 000 people in London died, 25% of London’s population, and other towns and cities were affected too. Most doctors fled and many wealthy people left for country houses, but this only spread the plague further. Like during the Black Death they did not know what caused the Plague or how to cure it, although they did use new methods such as putting red crosses on the doors of those infected. Key Medical Individuals during the Renaissance Andreas Vesalius (1514 -1564) • The first person to properly challenge the work of Galen, by disproving Galen’s theories on human anatomy. • Carried out meticulous dissections and used scientific methods to prove his work, seen as founder of modern medicine. • Wrote his book ‘De Humani Corporis Fabrica’, sharing his ideas, which was one of the most influential books on anatomy. • His work paved the way for others to challenge Galen. Thomas Sydenham (1624 -1689) Ambroise Pare (1510 -1590) • A French war surgeon, Pare had a significant impact on surgery. • He devised an ointment out of egg yolk, turpentine and oil of roses that he used to seal wounds rather than cauterisation. • He also created ligatures (silk threads) to tie off blood vessels after amputations rather than cauterisation. • Pare also developed the first prosthetic limbs and his work proved safer, less painful and better at tackling infection. John Hunter (1728 -1793) William Harvey (1578 -1657) • An English physician, Harvey’s work focused on the heart and the circulatory system. • Harvey proved that the heart was a pump, which pumped blood around the body via the circulatory system. • He also disproved Galen, by finding that the source of blood movement was the heart not the liver. • Published his work in ‘De Moto Cordis’ (The Motion of the Heart) Edward Jenner (1749 -1823) [also industrial era] • Known as ‘The English Hippocrates’, Sydenham was recognised as a founder of clinical medicine and epidemiology. • A Scottish surgeon, Hunter was one of the most distinguished scientists and surgeons of his day. • An English country doctor, trained by John Hunter, Jenner is famous for his pioneering work on vaccinations. • He placed great emphasis on observation and the maintenance of accurate medical records. • Advocated careful observation and scientific medicine, becoming an expert on anatomy through dissection. • Jenner developed a vaccination for the deadly disease of smallpox, by using a weak strain of cowpox. • Published a number of books, particularly around the study of different epidemics, studying scarlet fever and malaria. • Renowned for his training of other doctors, including Edward Jenner who he worked with in discovering vaccinations. • Eventually the government supported Jenner’s work and the vaccination helped to eradicate smallpox. • Treatise on gout (1683) is considered his masterpiece. • Held a number of positions, including being George III’s surgeon. • His work paved the way for other vaccinations to be discovered.
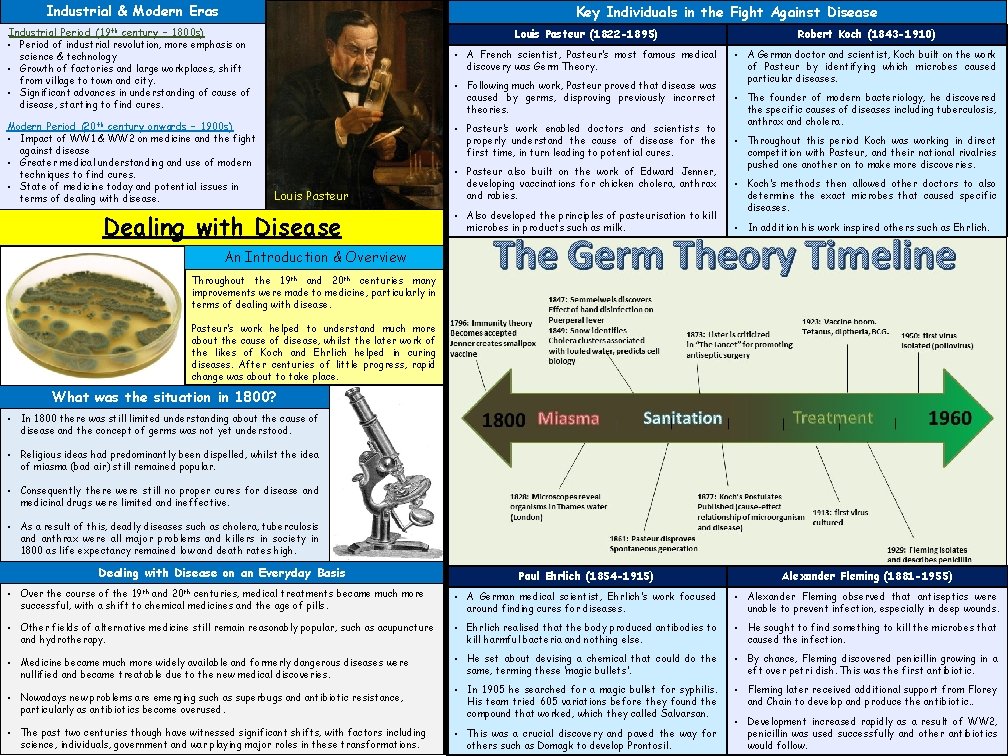
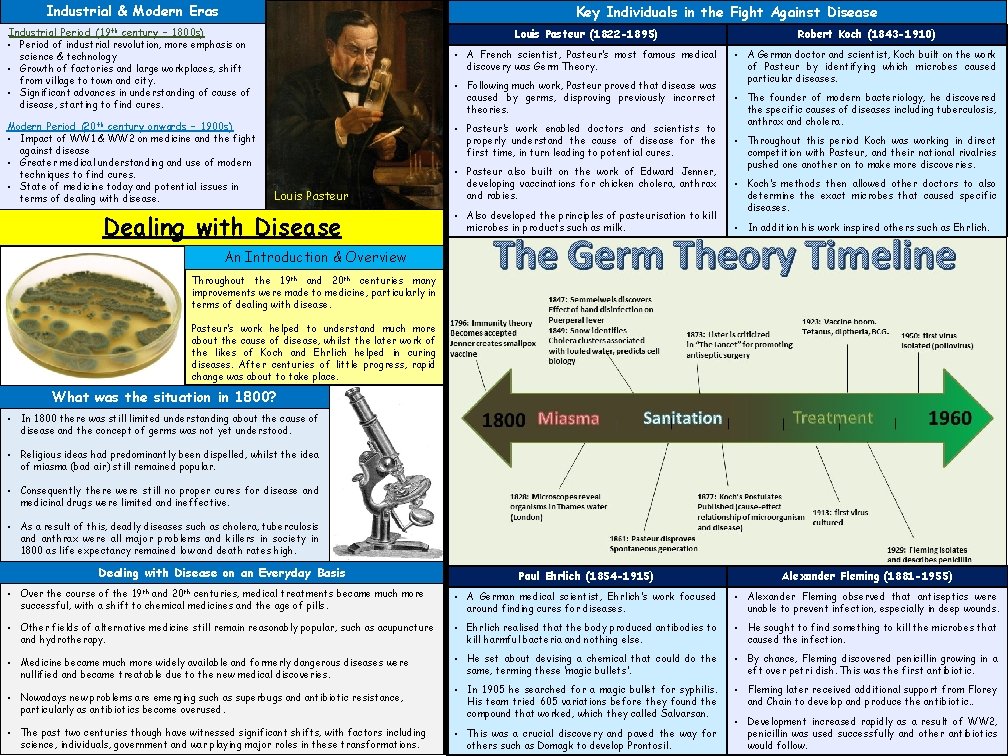
Industrial & Modern Eras Key Individuals in the Fight Against Disease . Industrial Period (19 th century – 1800 s) • Period of industrial revolution, more emphasis on science & technology • Growth of factories and large workplaces, shift from village to town and city. • Significant advances in understanding of cause of disease, starting to find cures. Modern Period (20 th century onwards – 1900 s) • Impact of WW 1 & WW 2 on medicine and the fight against disease • Greater medical understanding and use of modern techniques to find cures. • State of medicine today and potential issues in terms of dealing with disease. Louis Pasteur (1822 -1895) Robert Koch (1843 -1910) • A French scientist, Pasteur’s most famous medical discovery was Germ Theory. • A German doctor and scientist, Koch built on the work of Pasteur by identifying which microbes caused particular diseases. • Following much work, Pasteur proved that disease was caused by germs, disproving previously incorrect theories. • Pasteur’s work enabled doctors and scientists to properly understand the cause of disease for the first time, in turn leading to potential cures. Louis Pasteur Dealing with Disease • Pasteur also built on the work of Edward Jenner, developing vaccinations for chicken cholera, anthrax and rabies. • Also developed the principles of pasteurisation to kill microbes in products such as milk. • The founder of modern bacteriology, he discovered the specific causes of diseases including tuberculosis, anthrax and cholera. • Throughout this period Koch was working in direct competition with Pasteur, and their national rivalries pushed one another on to make more discoveries. • Koch’s methods then allowed other doctors to also determine the exact microbes that caused specific diseases. • In addition his work inspired others such as Ehrlich. An Introduction & Overview Throughout the 19 th and 20 th centuries many improvements were made to medicine, particularly in terms of dealing with disease. Pasteur’s work helped to understand much more about the cause of disease, whilst the later work of the likes of Koch and Ehrlich helped in curing diseases. After centuries of little progress, rapid change was about to take place. What was the situation in 1800? • In 1800 there was still limited understanding about the cause of disease and the concept of germs was not yet understood. • Religious ideas had predominantly been dispelled, whilst the idea of miasma (bad air) still remained popular. • Consequently there were still no proper cures for disease and medicinal drugs were limited and ineffective. • As a result of this, deadly diseases such as cholera, tuberculosis and anthrax were all major problems and killers in society in 1800 as life expectancy remained low and death rates high. Dealing with Disease on an Everyday Basis Paul Ehrlich (1854 -1915) Alexander Fleming (1881 -1955) • Over the course of the and centuries, medical treatments became much more successful, with a shift to chemical medicines and the age of pills. • A German medical scientist, Ehrlich’s work focused around finding cures for diseases. • Alexander Fleming observed that antiseptics were unable to prevent infection, especially in deep wounds. • Other fields of alternative medicine still remain reasonably popular, such as acupuncture and hydrotherapy. • Ehrlich realised that the body produced antibodies to kill harmful bacteria and nothing else. • He sought to find something to kill the microbes that caused the infection. • Medicine became much more widely available and formerly dangerous diseases were nullified and became treatable due to the new medical discoveries. • He set about devising a chemical that could do the same, terming these ‘magic bullets’. • By chance, Fleming discovered penicillin growing in a eft over petri dish. This was the first antibiotic. • Nowadays new problems are emerging such as superbugs and antibiotic resistance, particularly as antibiotics become overused. • In 1905 he searched for a magic bullet for syphilis. His team tried 605 variations before they found the compound that worked, which they called Salvarsan. • Fleming later received additional support from Florey and Chain to develop and produce the antibiotic. . • The past two centuries though have witnessed significant shifts, with factors including science, individuals, government and war playing major roles in these transformations. • This was a crucial discovery and paved the way for others such as Domagk to develop Prontosil. 19 th 20 th • Development increased rapidly as a result of WW 2, penicillin was used successfully and other antibiotics would follow.
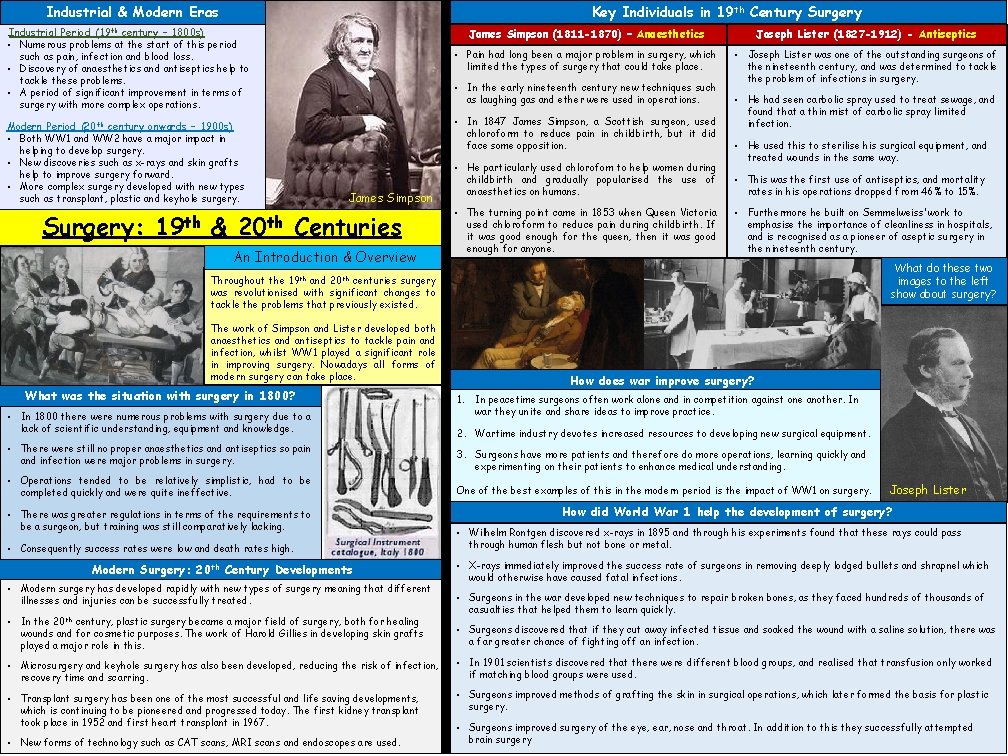
Key Individuals in 19 th Century Surgery Industrial & Modern Eras. Industrial Period (19 th century – 1800 s) • Numerous problems at the start of this period such as pain, infection and blood loss. • Discovery of anaesthetics and antiseptics help to tackle these problems. • A period of significant improvement in terms of surgery with more complex operations. Surgery: & Joseph Lister (1827 -1912) - Antiseptics • Pain had long been a major problem in surgery, which limited the types of surgery that could take place. • Joseph Lister was one of the outstanding surgeons of the nineteenth century, and was determined to tackle the problem of infections in surgery. • In the early nineteenth century new techniques such as laughing gas and ether were used in operations. • In 1847 James Simpson, a Scottish surgeon, used chloroform to reduce pain in childbirth, but it did face some opposition. Modern Period (20 th century onwards – 1900 s) • Both WW 1 and WW 2 have a major impact in helping to develop surgery. • New discoveries such as x-rays and skin grafts help to improve surgery forward. • More complex surgery developed with new types such as transplant, plastic and keyhole surgery. 19 th James Simpson (1811 -1870) – Anaesthetics James Simpson 20 th Centuries An Introduction & Overview 19 th • He particularly used chlorofom to help women during childbirth and gradually popularised the use of anaesthetics on humans. • The turning point came in 1853 when Queen Victoria used chloroform to reduce pain during childbirth. If it was good enough for the queen, then it was good enough for anyone. • He had seen carbolic spray used to treat sewage, and found that a thin mist of carbolic spray limited infection. • He used this to sterilise his surgical equipment, and treated wounds in the same way. • This was the first use of antiseptics, and mortality rates in his operations dropped from 46% to 15%. • Furthermore he built on Semmelweiss’ work to emphasise the importance of cleanliness in hospitals, and is recognised as a pioneer of aseptic surgery in the nineteenth century. What do these two images to the left show about surgery? 20 th Throughout the and centuries surgery was revolutionised with significant changes to tackle the problems that previously existed. The work of Simpson and Lister developed both anaesthetics and antiseptics to tackle pain and infection, whilst WW 1 played a significant role in improving surgery. Nowadays all forms of modern surgery can take place. What was the situation with surgery in 1800? • In 1800 there were numerous problems with surgery due to a lack of scientific understanding, equipment and knowledge. • There were still no proper anaesthetics and antiseptics so pain and infection were major problems in surgery. • Operations tended to be relatively simplistic, had to be completed quickly and were quite ineffective. • There was greater regulations in terms of the requirements to be a surgeon, but training was still comparatively lacking. • Consequently success rates were low and death rates high. Modern Surgery: 20 th Century Developments • Modern surgery has developed rapidly with new types of surgery meaning that different illnesses and injuries can be successfully treated. • In the 20 th century, plastic surgery became a major field of surgery, both for healing wounds and for cosmetic purposes. The work of Harold Gillies in developing skin grafts played a major role in this. How does war improve surgery? 1. In peacetime surgeons often work alone and in competition against one another. In war they unite and share ideas to improve practice. 2. Wartime industry devotes increased resources to developing new surgical equipment. 3. Surgeons have more patients and therefore do more operations, learning quickly and experimenting on their patients to enhance medical understanding. One of the best examples of this in the modern period is the impact of WW 1 on surgery. Joseph Lister How did World War 1 help the development of surgery? • Wilhelm Rontgen discovered x-rays in 1895 and through his experiments found that these rays could pass through human flesh but not bone or metal. • X-rays immediately improved the success rate of surgeons in removing deeply lodged bullets and shrapnel which would otherwise have caused fatal infections. • Surgeons in the war developed new techniques to repair broken bones, as they faced hundreds of thousands of casualties that helped them to learn quickly. • Surgeons discovered that if they cut away infected tissue and soaked the wound with a saline solution, there was a far greater chance of fighting off an infection. • Microsurgery and keyhole surgery has also been developed, reducing the risk of infection, recovery time and scarring. • In 1901 scientists discovered that there were different blood groups, and realised that transfusion only worked if matching blood groups were used. • Transplant surgery has been one of the most successful and life saving developments, which is continuing to be pioneered and progressed today. The first kidney transplant took place in 1952 and first heart transplant in 1967. • Surgeons improved methods of grafting the skin in surgical operations, which later formed the basis for plastic surgery. • New forms of technology such as CAT scans, MRI scans and endoscopes are used. • Surgeons improved surgery of the eye, ear, nose and throat. In addition to this they successfully attempted brain surgery
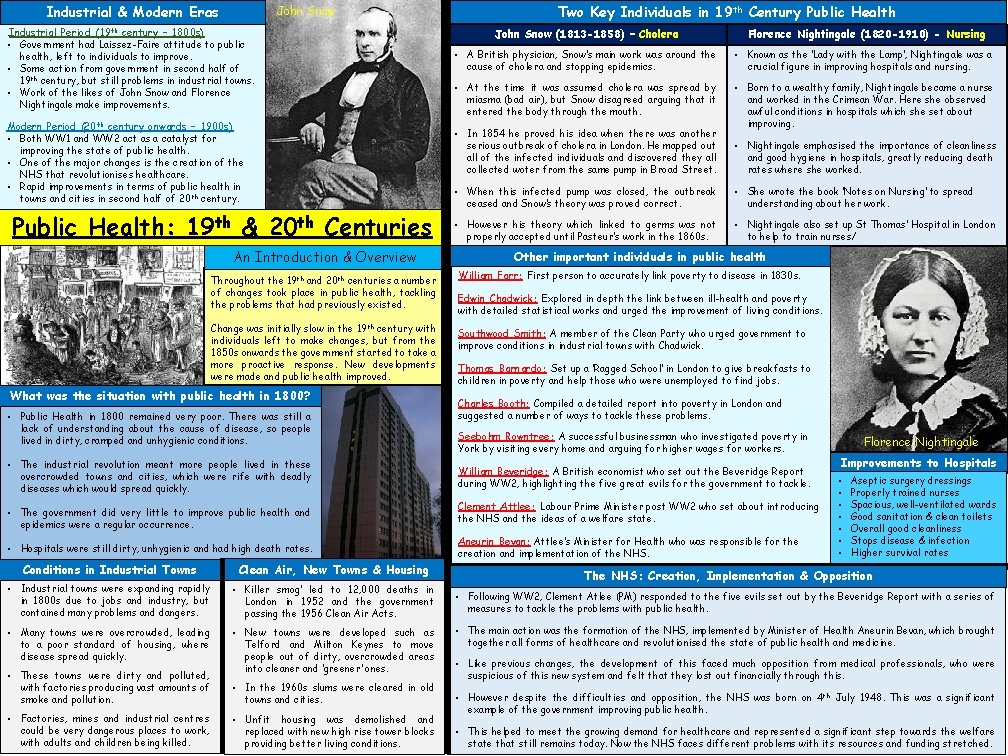
Industrial & Modern Eras John Snow . Industrial Period (19 th century – 1800 s) • Government had Laissez-Faire attitude to public health, left to individuals to improve. • Some action from government in second half of 19 th century, but still problems in industrial towns. • Work of the likes of John Snow and Florence Nightingale make improvements. Modern Period (20 th century onwards – 1900 s) • Both WW 1 and WW 2 act as a catalyst for improving the state of public health. • One of the major changes is the creation of the NHS that revolutionises healthcare. • Rapid improvements in terms of public health in towns and cities in second half of 20 th century. Public Health: 19 th & 20 th Centuries An Introduction & Overview Throughout the 19 th and 20 th centuries a number of changes took place in public health, tackling the problems that had previously existed. Change was initially slow in the 19 th century with individuals left to make changes, but from the 1850 s onwards the government started to take a more proactive response. New developments were made and public health improved. What was the situation with public health in 1800? • Public Health in 1800 remained very poor. There was still a lack of understanding about the cause of disease, so people lived in dirty, cramped and unhygienic conditions. • The industrial revolution meant more people lived in these overcrowded towns and cities, which were rife with deadly diseases which would spread quickly. • The government did very little to improve public health and epidemics were a regular occurrence. • Hospitals were still dirty, unhygienic and had high death rates. Conditions in Industrial Towns Clean Air, New Towns & Housing • Industrial towns were expanding rapidly in 1800 s due to jobs and industry, but contained many problems and dangers. • Killer smog’ led to 12, 000 deaths in London in 1952 and the government passing the 1956 Clean Air Acts. • Many towns were overcrowded, leading to a poor standard of housing, where disease spread quickly. • New towns were developed such as Telford and Milton Keynes to move people out of dirty, overcrowded areas into cleaner and ‘greener’ ones. • These towns were dirty and polluted, with factories producing vast amounts of smoke and pollution. • Factories, mines and industrial centres could be very dangerous places to work, with adults and children being killed. • In the 1960 s slums were cleared in old towns and cities. • Unfit housing was demolished and replaced with new high rise tower blocks providing better living conditions. Two Key Individuals in 19 th Century Public Health John Snow (1813 -1858) – Cholera Florence Nightingale (1820 -1910) - Nursing • A British physician, Snow’s main work was around the cause of cholera and stopping epidemics. • Known as the ‘Lady with the Lamp’, Nightingale was a crucial figure in improving hospitals and nursing. • At the time it was assumed cholera was spread by miasma (bad air), but Snow disagreed arguing that it entered the body through the mouth. • Born to a wealthy family, Nightingale became a nurse and worked in the Crimean War. Here she observed awful conditions in hospitals which she set about improving. • In 1854 he proved his idea when there was another serious outbreak of cholera in London. He mapped out all of the infected individuals and discovered they all collected woter from the same pump in Broad Street. • Nightingale emphasised the importance of cleanliness and good hygiene in hospitals, greatly reducing death rates where she worked. • When this infected pump was closed, the outbreak ceased and Snow’s theory was proved correct. • She wrote the book ‘Notes on Nursing’ to spread understanding about her work. • However his theory which linked to germs was not properly accepted until Pasteur’s work in the 1860 s. • Nightingale also set up St Thomas’ Hospital in London to help to train nurses/ Other important individuals in public health William Farr: First person to accurately link poverty to disease in 1830 s. Edwin Chadwick: Explored in depth the link between ill-health and poverty with detailed statistical works and urged the improvement of living conditions. Southwood Smith: A member of the Clean Party who urged government to improve conditions in industrial towns with Chadwick. Thomas Barnardo: Set up a ‘Ragged School’ in London to give breakfasts to children in poverty and help those who were unemployed to find jobs. Charles Booth: Compiled a detailed report into poverty in London and suggested a number of ways to tackle these problems. Seebohm Rowntree: A successful businessman who investigated poverty in York by visiting every home and arguing for higher wages for workers. William Beveridge: A British economist who set out the Beveridge Report during WW 2, highlighting the five great evils for the government to tackle. Clement Attlee: Labour Prime Minister post WW 2 who set about introducing the NHS and the ideas of a welfare state. Aneurin Bevan: Attlee’s Minister for Health who was responsible for the creation and implementation of the NHS. Florence Nightingale Improvements to Hospitals • • Aseptic surgery dressings Properly trained nurses Spacious, well-ventilated wards Good sanitation & clean toilets Overall good cleanliness Stops disease & infection Higher survival rates The NHS: Creation, Implementation & Opposition • Following WW 2, Clement Atlee (PM) responded to the five evils set out by the Beveridge Report with a series of measures to tackle the problems with public health. • The main action was the formation of the NHS, implemented by Minister of Health Aneurin Bevan, which brought together all forms of healthcare and revolutionised the state of public health and medicine. • Like previous changes, the development of this faced much opposition from medical professionals, who were suspicious of this new system and felt that they lost out financially through this. • However despite the difficulties and opposition, the NHS was born on 4 th July 1948. This was a significant example of the government improving public health. • This helped to meet the growing demand for healthcare and represented a significant step towards the welfare state that still remains today. Now the NHS faces different problems with its resources and funding stretched.