Medicolegal aspects of peripheral nerve injury Alistair Ross




- Slides: 51
Medicolegal aspects of peripheral nerve injury Alistair Ross MB FRCS Consultant Orthopaedic Surgeon, Bath, UK Associate Editor The Bone & Joint Journal Cambridge Annual Medico-Legal Conference Peterhouse, Cambridge, 2016
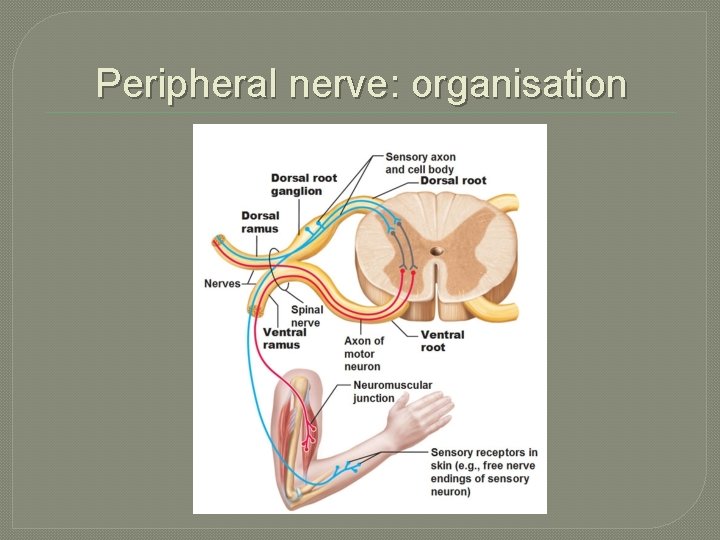
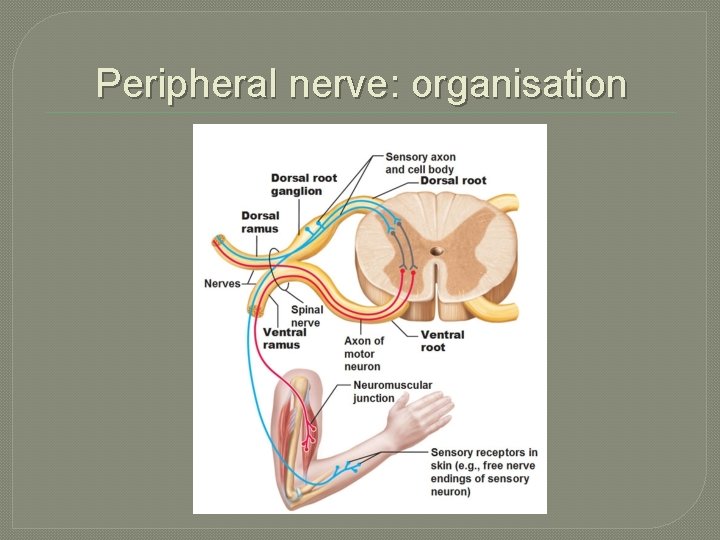
Peripheral nerve: organisation
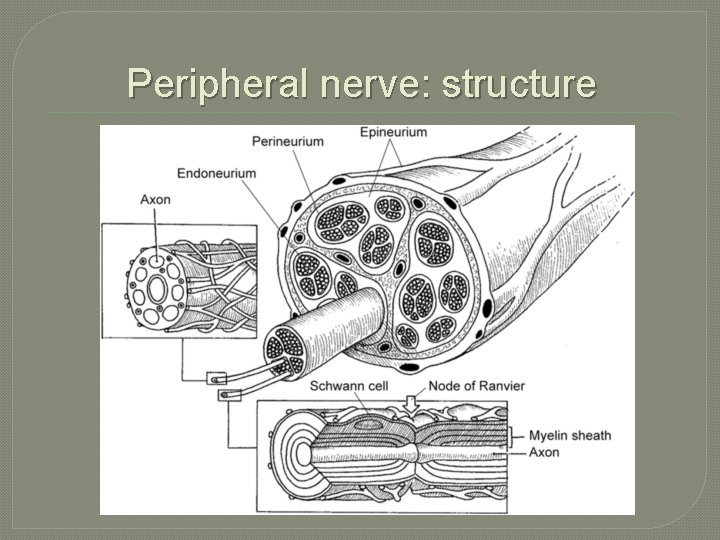
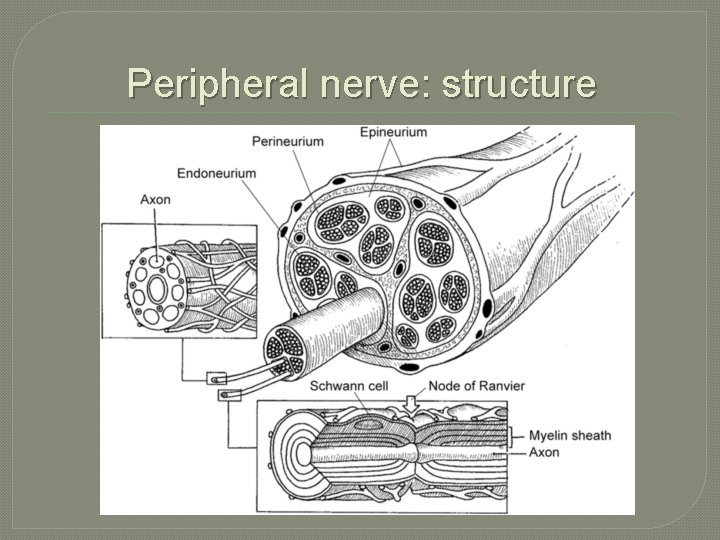
Peripheral nerve: structure
Peripheral nerve injury: classification � � � Neurapraxia Axonotmesis Neurotmesis ἀπραξία: inaction τμησις: a cutting (of) Seddon HJ Three types of nerve injury Brain 1943, 66 (4): 238 -283
Peripheral nerve injury: neurapraxia Neurapraxia: a non-degenerative lesion of a nerve characterised by a complete or partial failure to propagate an action potential (conduction defect) along the nerve resulting in motor and/or sensory loss.
Peripheral nerve injury: neurapraxia � Usually caused by compression or ischaemia, resulting in ischaemia of the myelin sheath. � Can be reversed if the injurious agent is removed. � Nerve remains intact. Wallerian degeneration does not occur.
Peripheral nerve injury: neurapraxia � Stimulation of the distal segment of the nerve evokes a response. � Normal motor action potential expected distal to the site of injury by day 10. � Recovers by re-myelination of distal segment � Time to recovery: 2 -12 weeks
Peripheral nerve injury: neurapraxia � The assumption that a lesion is a neurapraxia rather than a more severe injury leads to delay in diagnosis and a poorer outcome. � A potentially dangerous diagnosis to make particularly in the presence of persistent pain which suggests that the injurious agent is continuing to act. � Diagnosis should not be made in the presence of a strong Tinel test which indicates that axons have been ruptured.
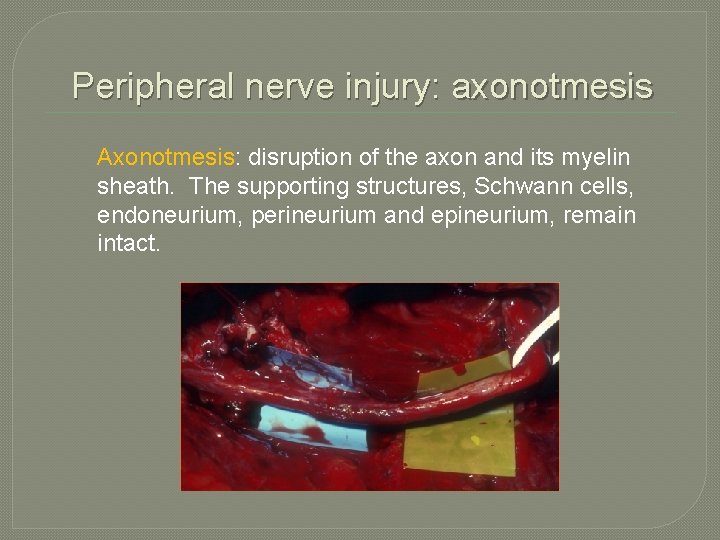
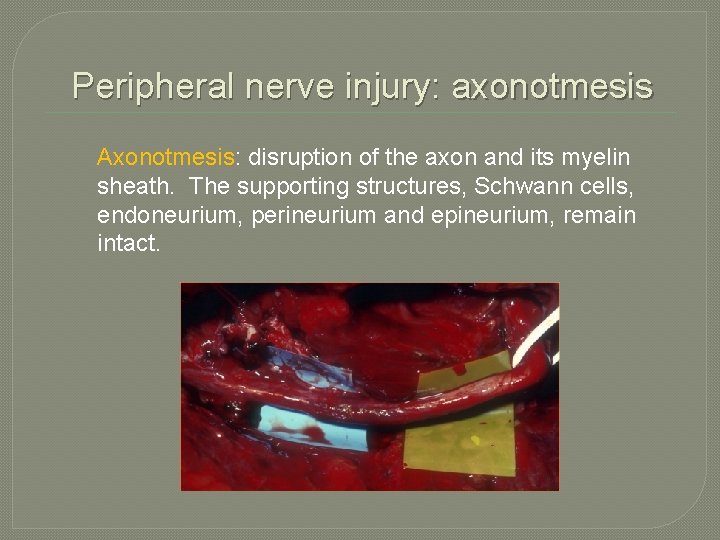
Peripheral nerve injury: axonotmesis Axonotmesis: disruption of the axon and its myelin sheath. The supporting structures, Schwann cells, endoneurium, perineurium and epineurium, remain intact.
Peripheral nerve injury: axonotmesis � Usually the result of severe compression or crush. � Wallerian degeneration occurs distally and proximally to the closest node of Ranvier. � Repair is by a combination of collateral sprouting in lesser injuries and axonal regeneration in more severe injuries. The latter occurs at 1 -2 mm per day. � Time to recovery: 2 to 6 months
Peripheral nerve injury: axonotmesis � Nerve conduction studies show a loss of conduction in the distal segment 3 -4 days after injury (demyelination). � Small or absent compound muscle or sensory nerve action potentials (axon loss) � EMG studies show fibrillation potentials and sharp waves 2 -3 weeks after injury (axon loss). � Degree of recovery depends on the age of the patient, the site of injury and the amount of fibrosis that occurs.
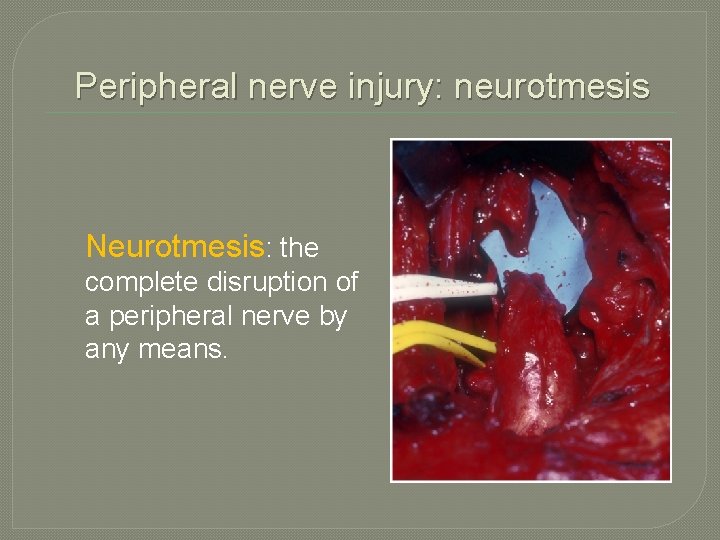
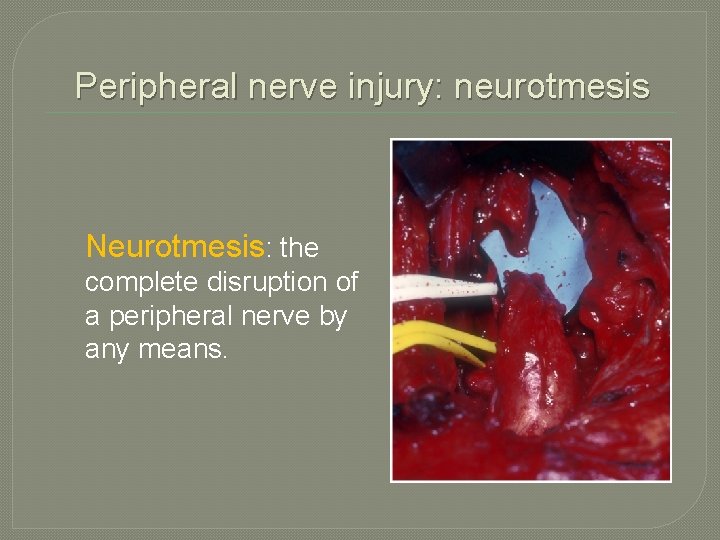
Peripheral nerve injury: neurotmesis Neurotmesis: the complete disruption of a peripheral nerve by any means.
Peripheral nerve injury: neurotmesis � Wallerian degeneration occurs distal to the lesion. � Nerve conduction studies show a loss of conduction in the distal segment 3 -4 days after injury. � EMG studies show fibrillation potentials and sharp waves 2 -3 weeks after injury. � Surgical intervention is required to repair the nerve, whether by direct suture or grafting. � Time to recovery 2 to 18 months
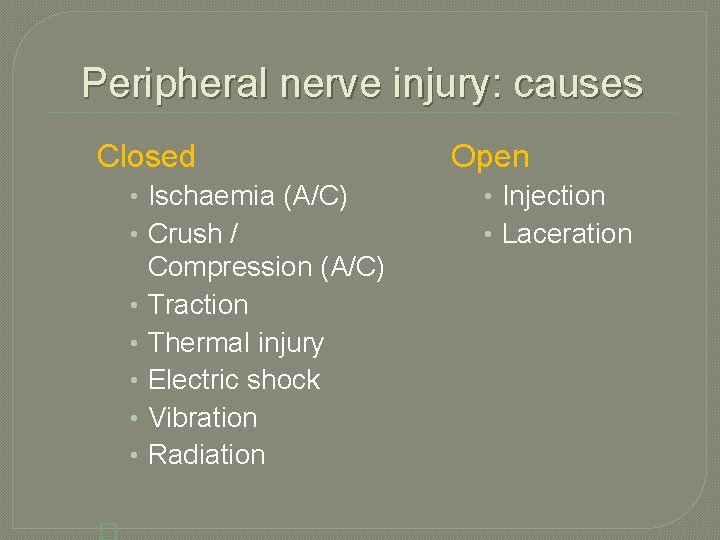
Peripheral nerve injury: causes Closed • Ischaemia (A/C) • Crush / • • • Compression (A/C) Traction Thermal injury Electric shock Vibration Radiation Open • Injection • Laceration
Iatrogenic peripheral nerve injury �…or iatropathic �…or iatrogenous �…but caused by those treating a patient
Iatrogenic peripheral nerve injury “When a patient enters hospital without a nerve lesion and emerges with one, it is seldom possible to resist an allegation of negligence. ” Bonney GLW Iatrogenic injuries of nerves J Bone Joint Surg 1986; 68 B: 9 -13
Iatrogenic peripheral nerve injury “If there is an incision over the line of a main nerve and if, after operation, there is complete paralysis (including vasomotor and sudomotor paralysis) in the distribution of that nerve, speculation is unnecessary: the nerve has been cut, and there will be no recovery unless it is explored and repaired. ” Bonney GLW Iatrogenic injuries of nerves J Bone Joint Surg 1986; 68 B: 9 -13
Iatrogenic peripheral nerve injury “When pressure on a nerve has been followed by partial paralysis in its distribution, but stimulation below the level of the lesion produces a motor response, it is reasonable to assume that there has been a conduction block which will recover. ” Bonney GLW Iatrogenic injuries of nerves J Bone Joint Surg 1986; 68 B: 9 -13
Iatrogenic peripheral nerve injury “Between these extremes, precise diagnosis is much more difficult. ” Bonney GLW Iatrogenic injuries of nerves J Bone Joint Surg 1986; 68 B: 9 -13
Iatrogenic peripheral nerve injury “Failure to make the diagnosis of a nerve injury, and failure to treat that complication of the first surgery, the iatrogenic nerve injury, is as much a cause for concern as the initial injury to the peripheral nerve. ” Dellon AL Invited discussion: management strategies for iatrogenic peripheral nerve lesions. Annals of Plastic Surgery 2005, 54: 140 -42
Iatrogenic PNI: incidence �Overall �NHS incidence unknown Litigation Authority does not specifically record cases under the heading ‘peripheral nerve injury’
Iatrogenic PNI: incidence � 1990 to 1998 � 722 consecutive cases of peripheral nerve injury � 126 iatrogenic (17. 5%) � Usually resulting from orthopaedic surgery, trauma or hand surgery � ‘Lumps and bumps’ surgery Kretschmer T et al Evaluation of iatrogenic lesions in 722 surgically treated cases of peripheral nerve trauma J Neurosurg 94: 905– 912, 2001
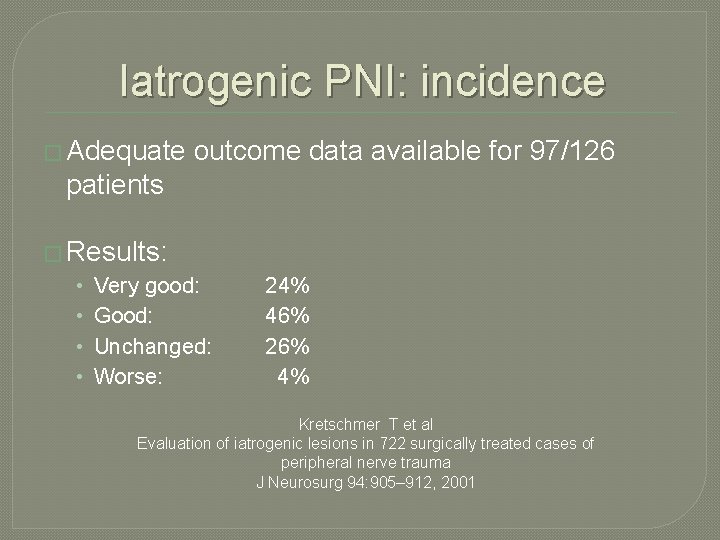
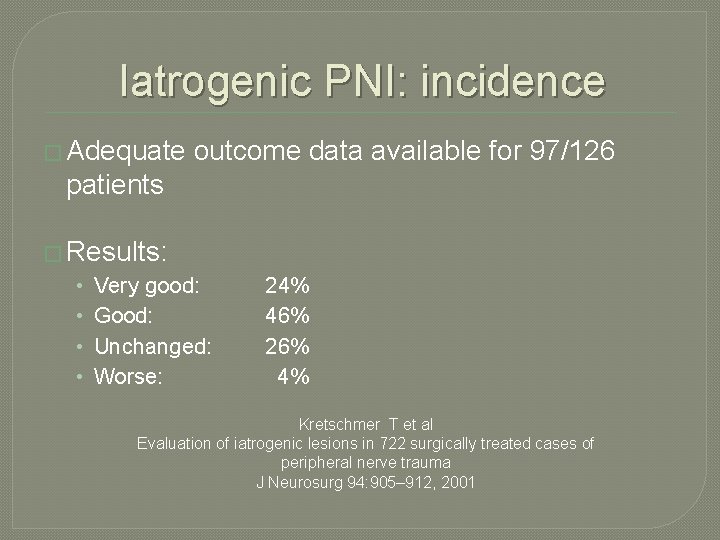
Iatrogenic PNI: incidence � Adequate outcome data available for 97/126 patients � Results: • • Very good: Good: Unchanged: Worse: 24% 46% 26% 4% Kretschmer T et al Evaluation of iatrogenic lesions in 722 surgically treated cases of peripheral nerve trauma J Neurosurg 94: 905– 912, 2001
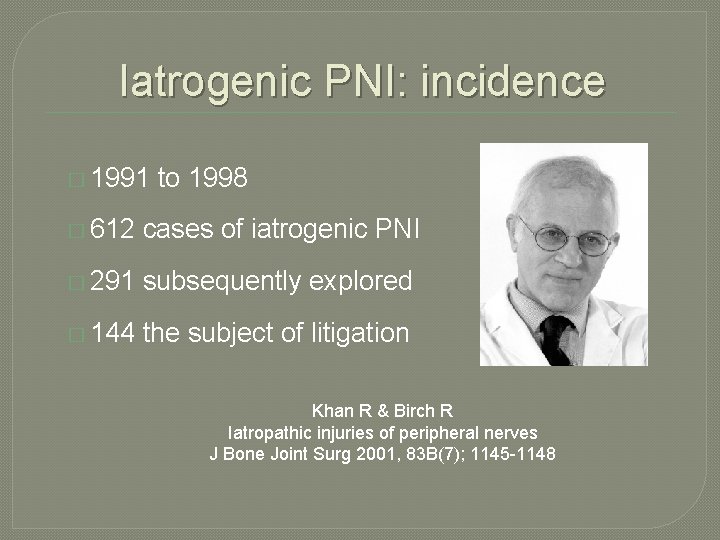
Iatrogenic PNI: incidence � 1991 to 1998 � 612 cases of iatrogenic PNI � 291 subsequently explored � 144 the subject of litigation Khan R & Birch R Iatropathic injuries of peripheral nerves J Bone Joint Surg 2001, 83 B(7); 1145 -1148
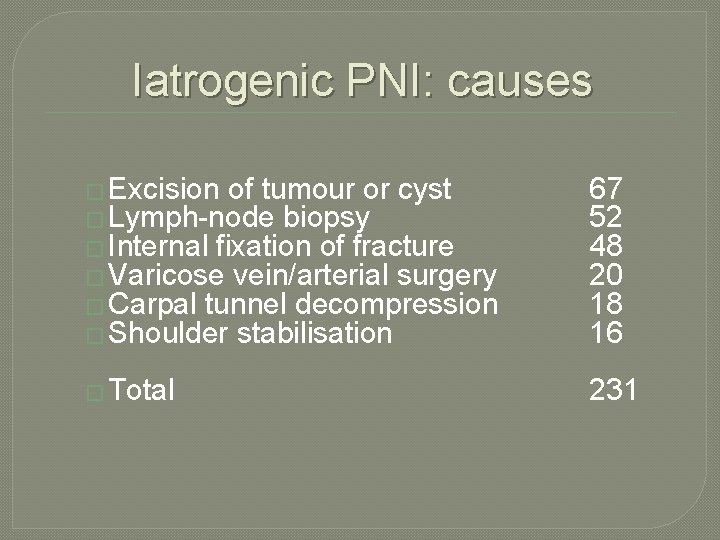
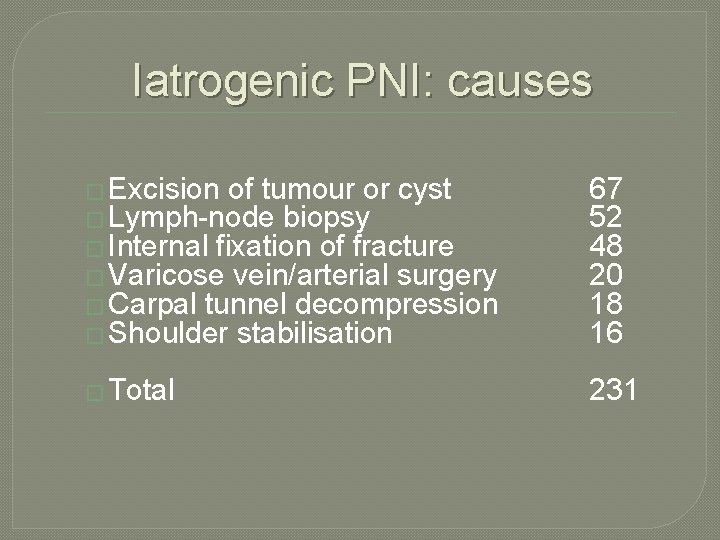
Iatrogenic PNI: causes � Excision of tumour or cyst � Lymph-node biopsy � Internal fixation of fracture � Varicose vein/arterial surgery � Carpal tunnel decompression � Shoulder stabilisation 67 52 48 20 18 16 � Total 231

‘Lumps and bumps’: Schwannoma
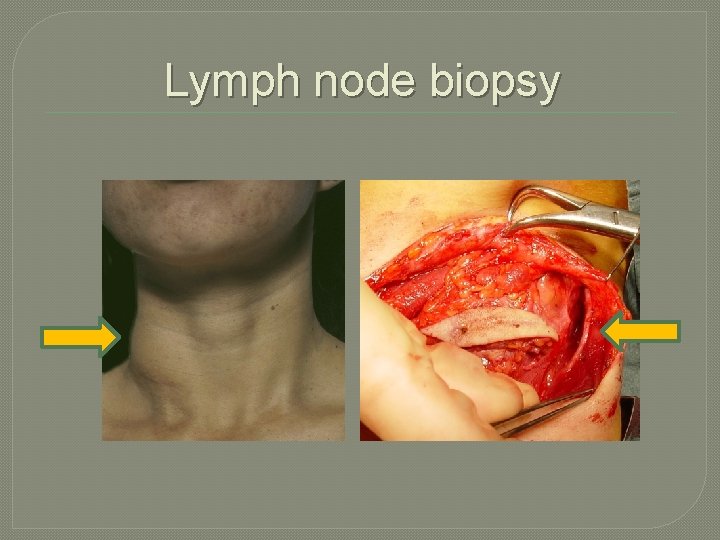
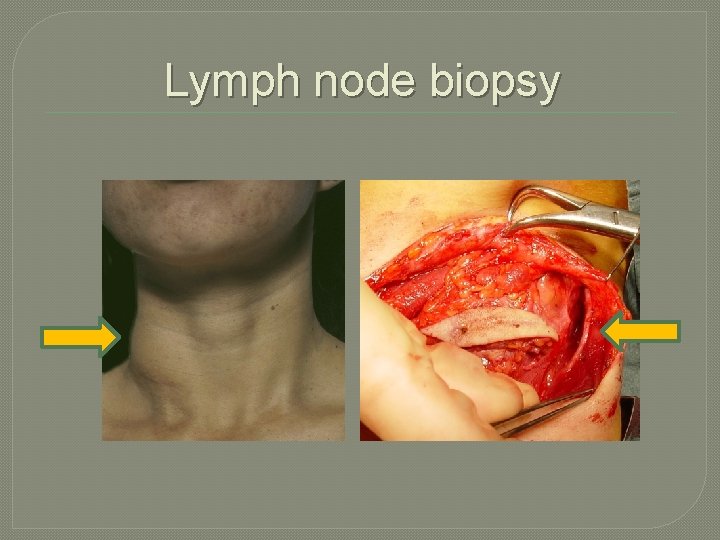
Lymph node biopsy

Iatrogenic PNI: by specialty Orthopaedics 174 � General surgery 70 � Vascular surgery 11 � Obs / Gynae 9 � Plastic surgery 7 � Cardiothoracic 5 � ENT surgery 5 � Anaesthetics 4 � Neurosurgery 4 � Maxillofacial surgery 2 � � Total 291
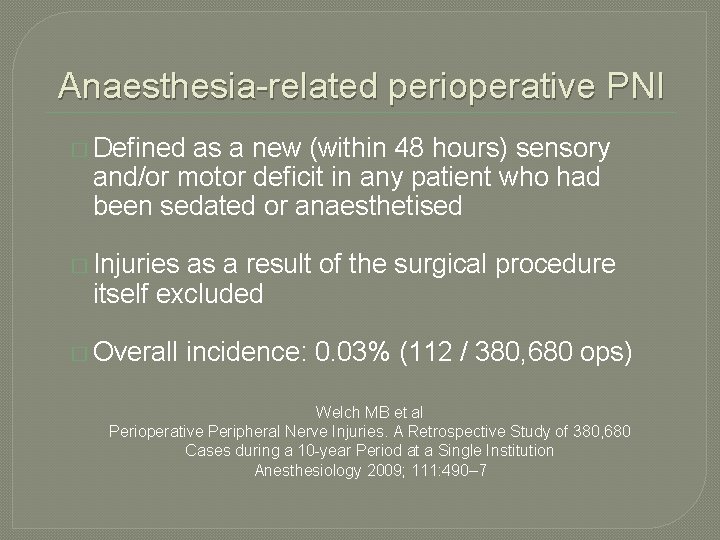
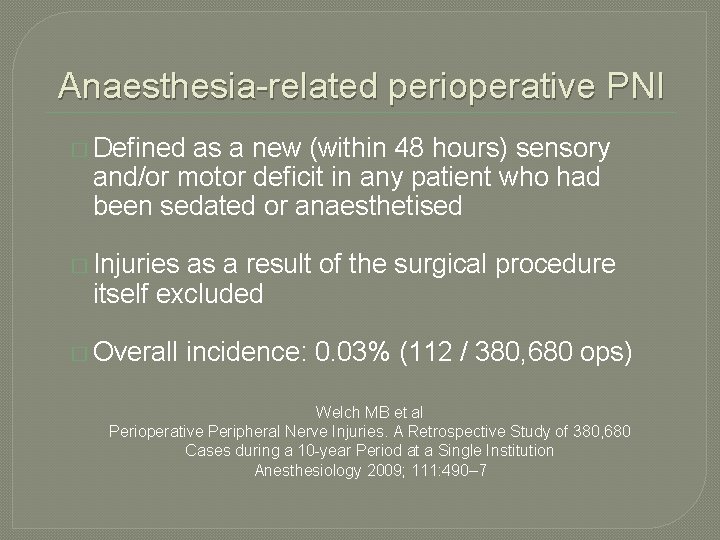
Anaesthesia-related perioperative PNI � Defined as a new (within 48 hours) sensory and/or motor deficit in any patient who had been sedated or anaesthetised � Injuries as a result of the surgical procedure itself excluded � Overall incidence: 0. 03% (112 / 380, 680 ops) Welch MB et al Perioperative Peripheral Nerve Injuries. A Retrospective Study of 380, 680 Cases during a 10 -year Period at a Single Institution Anesthesiology 2009; 111: 490– 7
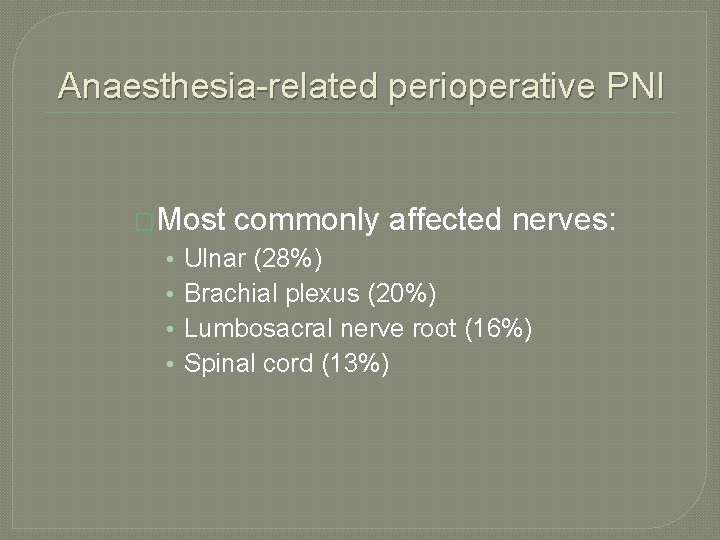
Anaesthesia-related perioperative PNI �Most • • commonly affected nerves: Ulnar (28%) Brachial plexus (20%) Lumbosacral nerve root (16%) Spinal cord (13%)
Anaesthesia-related perioperative PNI: principal causes � Poor padding and positioning of limbs � Needle trauma secondary to regional anaesthesia � Haematoma � Local surrounding a nerve anaesthetic agents: toxicity and direct damage from intraneural injection
Anaesthesia-related perioperative PNI: principal causes � Pre-existing disease • • � Diabetes Smoking Hypertension Pre-existing neuropathy Perioperative problems • Hypovolaemia, dehydration, hypotension, • Hypoxaemia, electrolyte disturbance & hypothermia
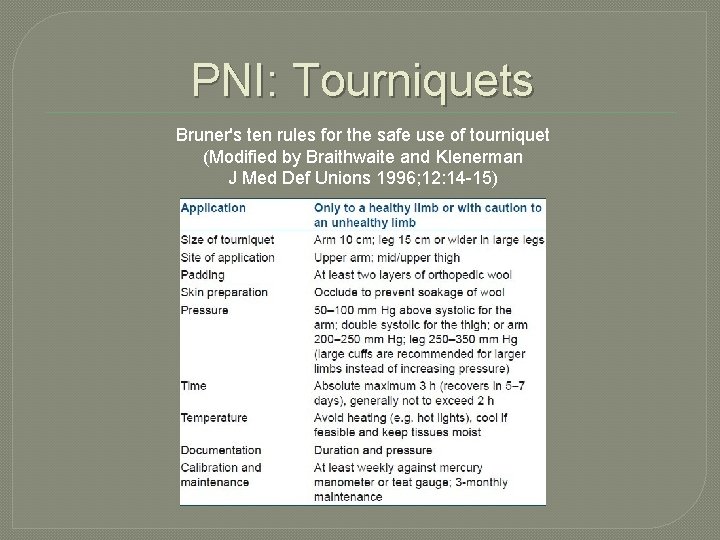
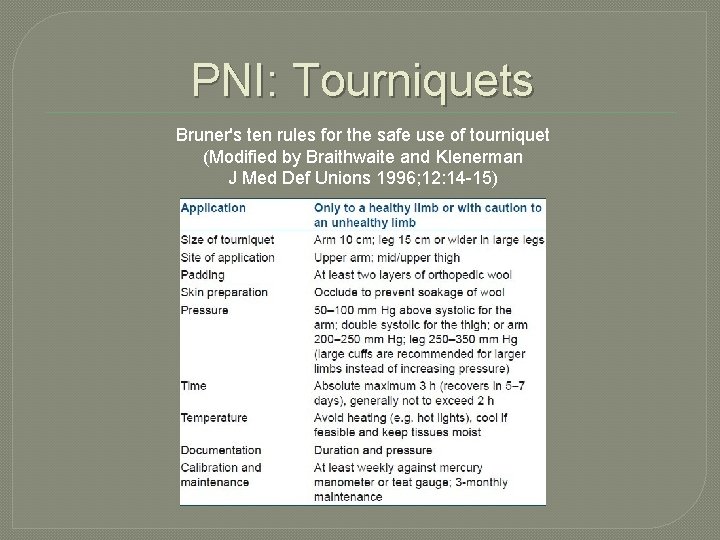
PNI: Tourniquets Bruner's ten rules for the safe use of tourniquet (Modified by Braithwaite and Klenerman J Med Def Unions 1996; 12: 14 -15)
Peripheral nerve injury: management � Diagnosis is the responsibility of the treating clinician. � Nerve repair is the business of a sub-specialist.
Peripheral nerve injury: management The earlier a peripheral nerve injury is diagnosed and treated the better � Ease of recognition of injury � Ease with which the nerve stumps can be mobilised and approximated � Lack of scarring and distortion of the anatomy � Best results achieved by early direct nerve repair
PNI: delay in repair � A delay of two months halves the number of axons crossing a repair and halves their rate of growth. � Further deterioration occurs with longer delay. � Motor end plate loss progresses even after repair and is near total after one year (for a proximal repair). � Central cord changes also progress prior to repair and become less reversible with time. British Orthopaedic Association ‘Blue Book’ 2011
PNI: management of neurotmesis If complete or partial laceration to nerve identified at operation (whether the result of trauma or iatrogenic injury): • Trained nerve surgeon: primary epineural suture. • Untrained surgeon: attempt to oppose ends; gentle mobilisation of nerve if necessary; tag nerve end/s with coloured epineural sutures.
PNI: management of neurotmesis � Clear, accurate documentation of the injury and action taken. � Prompt discussion with, and referral to, a nerve surgeon. � Discussion � Accurate with/explanation to patient early postoperative assessment and documentation of neurological deficit
Peripheral nerve injury: management If patient found to have neurological deficit postoperatively: � Clear, accurate documentation of neurological deficit � Inform patient of possible nerve injury � Discussion with/referral to nerve surgeon
Peripheral nerve injury: management If patient found to have neurological deficit postoperatively: � At this stage it is unclear of the nature of the lesion � If the nerve is thought to have been divided (cf Bonney) : re-explore with a view to repair � If not, EMG and NCS at three weeks
Iatrogenic PNI: indications for surgery �Clinical evidence of neurotmesis �Failure of recovery from presumed axonotmesis at the predicted time �Deterioration of lesion while under observation �Persistent, intractable pain

Iatrogenic PNI: aim of surgery � Establish diagnosis � Relieve pain � Improve function
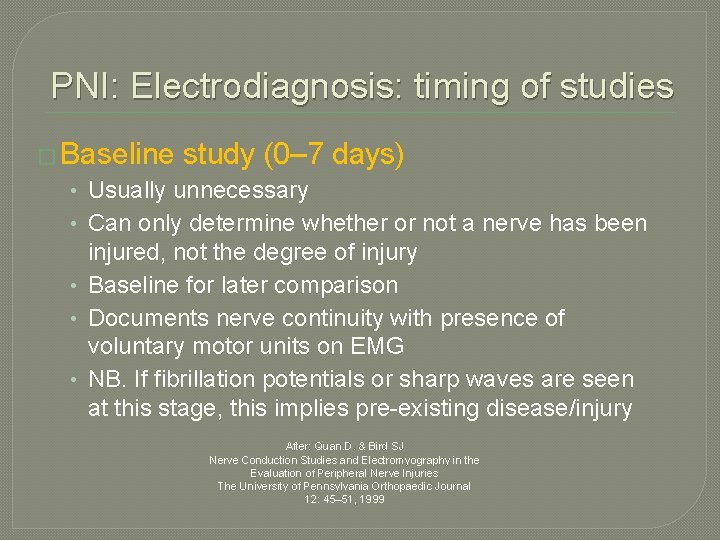
PNI: Electrodiagnosis: timing of studies � Baseline study (0– 7 days) • Usually unnecessary • Can only determine whether or not a nerve has been injured, not the degree of injury • Baseline for later comparison • Documents nerve continuity with presence of voluntary motor units on EMG • NB. If fibrillation potentials or sharp waves are seen at this stage, this implies pre-existing disease/injury After: Quan. D. & Bird SJ Nerve Conduction Studies and Electromyography in the Evaluation of Peripheral Nerve Injuries The University of Pennsylvania Orthopaedic Journal 12: 45– 51, 1999
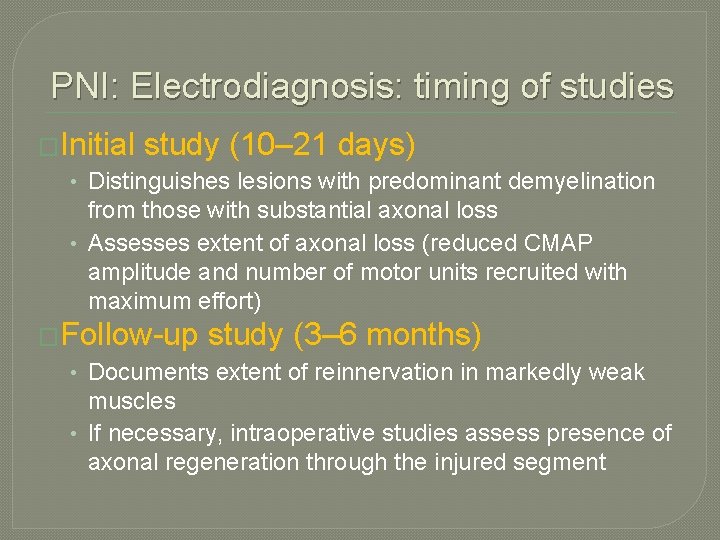
PNI: Electrodiagnosis: timing of studies �Initial study (10– 21 days) • Distinguishes lesions with predominant demyelination from those with substantial axonal loss • Assesses extent of axonal loss (reduced CMAP amplitude and number of motor units recruited with maximum effort) �Follow-up study (3– 6 months) • Documents extent of reinnervation in markedly weak muscles • If necessary, intraoperative studies assess presence of axonal regeneration through the injured segment
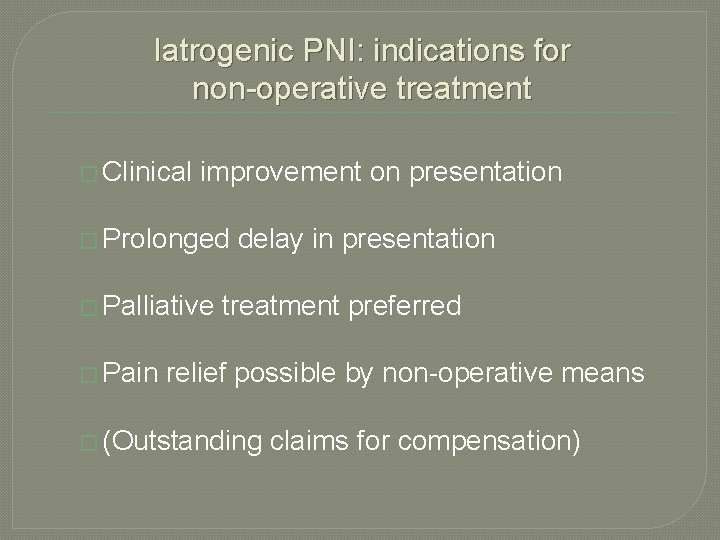
Iatrogenic PNI: indications for non-operative treatment � Clinical improvement on presentation � Prolonged � Palliative � Pain delay in presentation treatment preferred relief possible by non-operative means � (Outstanding claims for compensation)

Peripheral nerve injury: mismanagement � Inadequate informed consent � Avoidable damage to nerves/nerves � Delay in diagnosis / missed diagnosis � Delay in referral � Delay in treatment � Inappropriate treatment
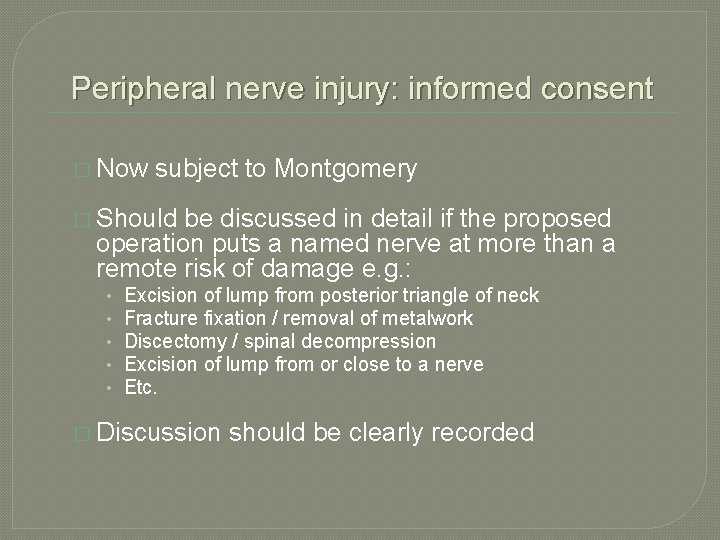
Peripheral nerve injury: informed consent � Now subject to Montgomery � Should be discussed in detail if the proposed operation puts a named nerve at more than a remote risk of damage e. g. : • • • Excision of lump from posterior triangle of neck Fracture fixation / removal of metalwork Discectomy / spinal decompression Excision of lump from or close to a nerve Etc. � Discussion should be clearly recorded
Intraoperative PNI need not be negligent “It must be accepted that despite careful surgery nerve injury during operation may occur. Recognition and prompt remedial action after the event are the keys. ” British Orthopaedic Association ‘Blue Book’ 2011
Iatrogenic PNI: Conclusions � Properly informed consent more important than ever � A thorough knowledge of the local anatomy reduces the risk of inadvertent nerve damage � Identify any PNI promptly � Document neurology accurately � Discuss situation with patient � Discuss with / refer to an expert early
Iatrogenic PNI: Conclusions � Inadequate � Avoidable nerves consent damage to trunk / sensory � Delay in diagnosis /missed diagnosis � Delay in referral to expert � Delay in treatment � Inappropriate treatment