Medications used to Treat Pain Opioid and Adjunct











- Slides: 59
Medications used to Treat Pain: Opioid and Adjunct Agents Gillian Tufts, DNP, FNP-BC
The Opioid drugs "Among the remedies which it has pleased Almighty God to give to man to relieve his sufferings, none is so universal and so efficacious as opium. “ Goodman, Gilman. (2010) The Pharmacological Basis of Therapeutics.
Opioid Pain Agents Morphine Codeine Meperedine Methadone Hydromorphone Hydrocodone Oxycodone Fentanyl Propoxyphene – withdrawn from the market 2010 Tramadol and Tapentadol
Opioid Pain Agents Naturally occurring opioid neurotransmitters n Endorphins n Enkephalins n Dysnorphins Effect via the opioid receptors n Mu n Delta n Kappa
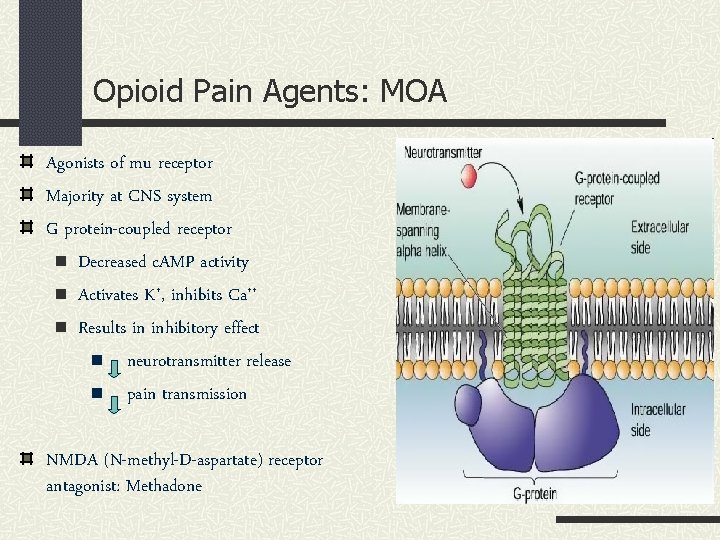
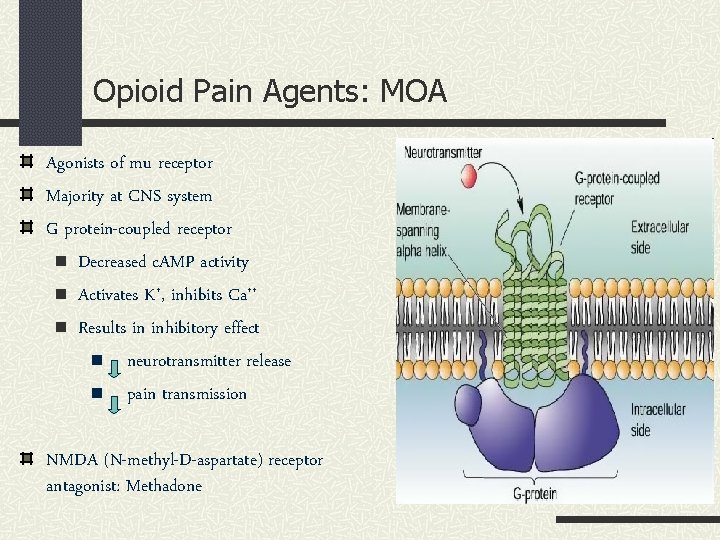
Opioid Pain Agents: MOA Agonists of mu receptor Majority at CNS system G protein-coupled receptor n Decreased c. AMP activity n Activates K+, inhibits Ca++ n Results in inhibitory effect n neurotransmitter release n pain transmission NMDA (N-methyl-D-aspartate) receptor antagonist: Methadone
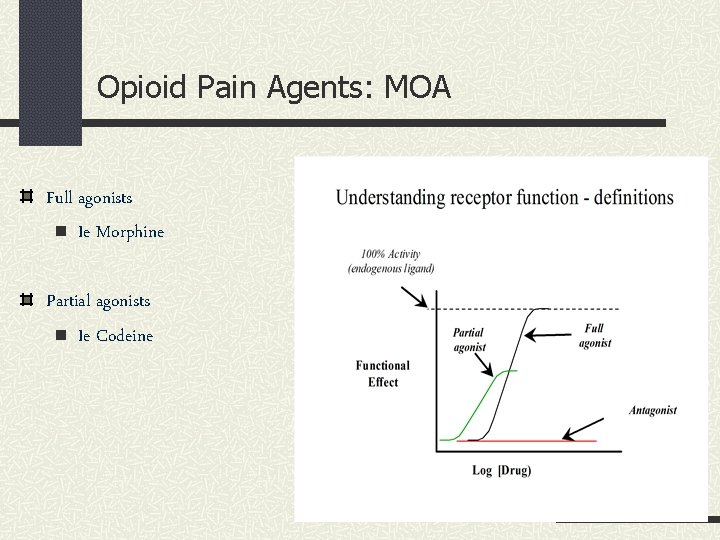
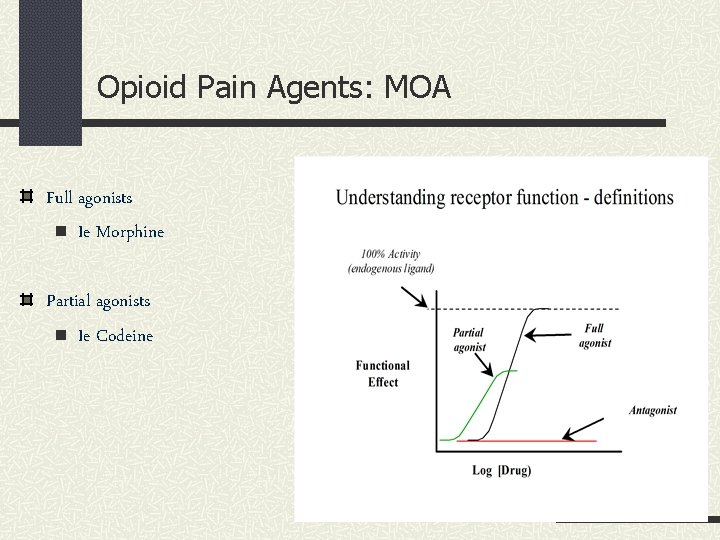
Opioid Pain Agents: MOA Full agonists n Ie Morphine Partial agonists n Ie Codeine

Opioid Pain Agents Naturally occurring in opium n Morphine, Codeine Semisynthetic derivatives n Hydrocodone, oxycodone, hydromorphone n Heroin (diacetylmorphine) Synthetic n Fentanyl, Meperidine, Methadone n Loperamide, Diphenoxylate n Tramadol n Tapentadol
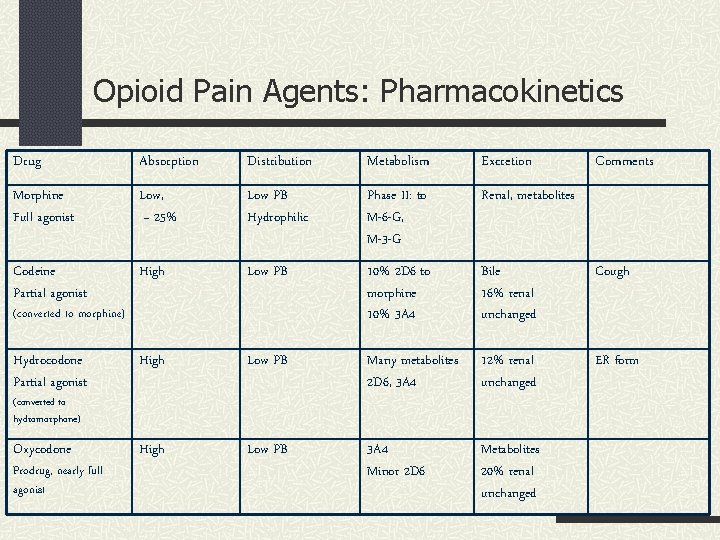
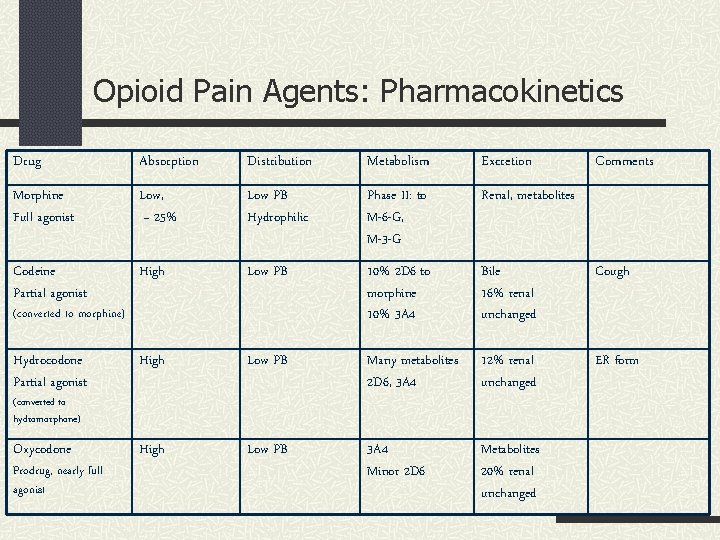
Opioid Pain Agents: Pharmacokinetics Drug Absorption Distribution Metabolism Excretion Morphine Full agonist Low, ~ 25% Low PB Hydrophilic Phase II: to M-6 -G, M-3 -G Renal, metabolites Codeine Partial agonist High Low PB 10% 2 D 6 to morphine 10% 3 A 4 Bile 16% renal unchanged Cough Hydrocodone Partial agonist High Low PB Many metabolites 2 D 6, 3 A 4 12% renal unchanged ER form Oxycodone High Low PB 3 A 4 Minor 2 D 6 Metabolites 20% renal unchanged (converted to morphine) (converted to hydromorphone) Prodrug, nearly full agonist Comments
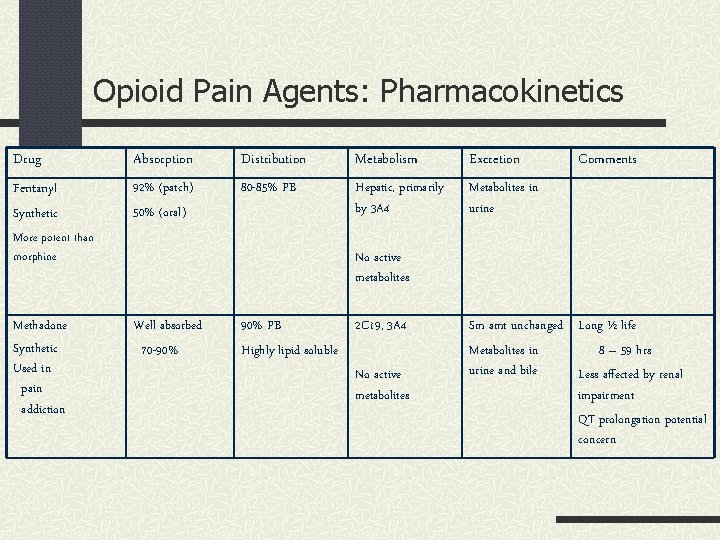
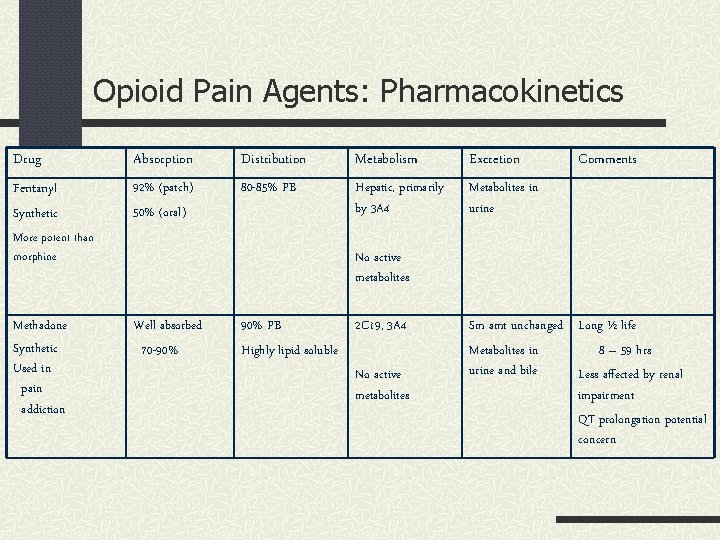
Opioid Pain Agents: Pharmacokinetics Drug Absorption Distribution Metabolism Excretion Fentanyl 92% (patch) 50% (oral) 80 -85% PB Hepatic, primarily by 3 A 4 Metabolites in urine Synthetic More potent than morphine Methadone Synthetic Used in pain addiction Comments No active metabolites Well absorbed 70 -90% PB Highly lipid soluble 2 C 19, 3 A 4 No active metabolites Sm amt unchanged Long ½ life Metabolites in 8 – 59 hrs urine and bile Less affected by renal impairment QT prolongation potential concern
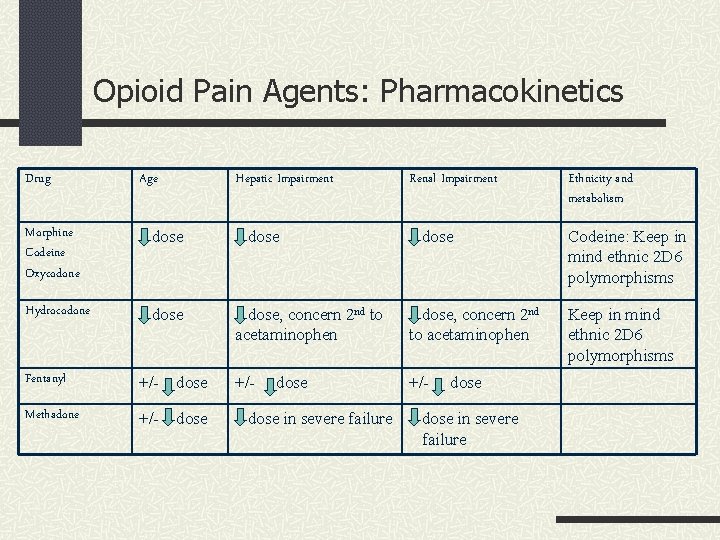
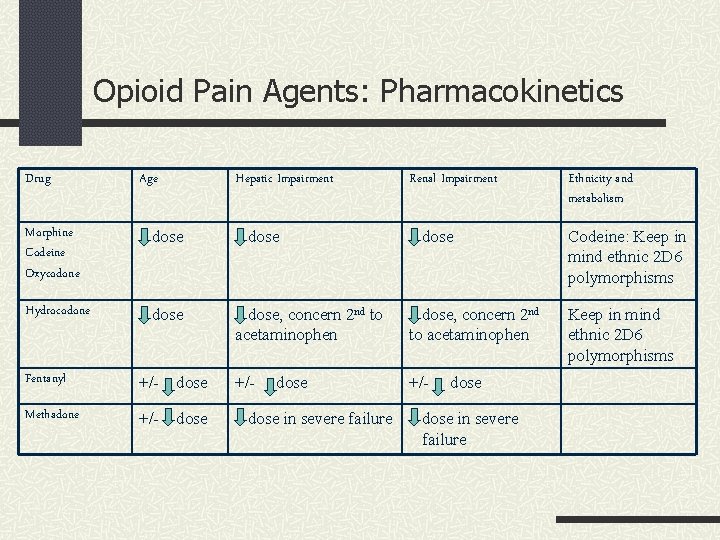
Opioid Pain Agents: Pharmacokinetics Drug Age Hepatic Impairment Morphine Codeine Oxycodone dose Hydrocodone dose Fentanyl +/- dose Methadone +/- dose Renal Impairment dose, concern 2 nd to acetaminophen +/- dose in severe failure Ethnicity and metabolism Codeine: Keep in mind ethnic 2 D 6 polymorphisms
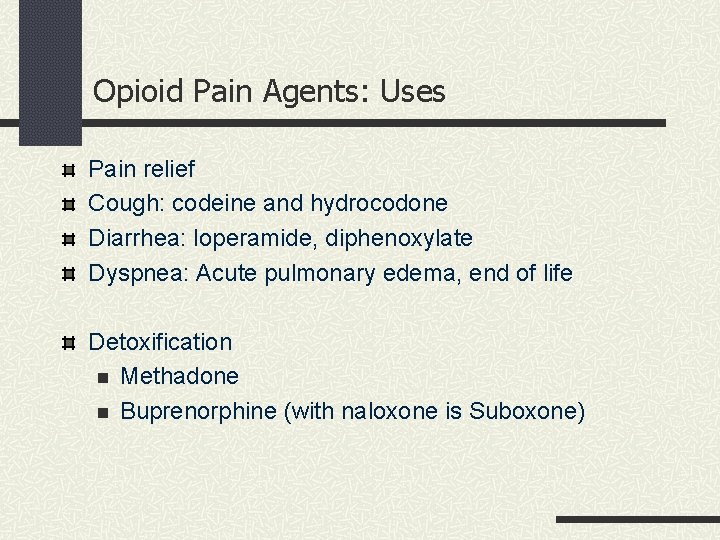
Opioid Pain Agents: Uses Pain relief Cough: codeine and hydrocodone Diarrhea: loperamide, diphenoxylate Dyspnea: Acute pulmonary edema, end of life Detoxification n Methadone n Buprenorphine (with naloxone is Suboxone)
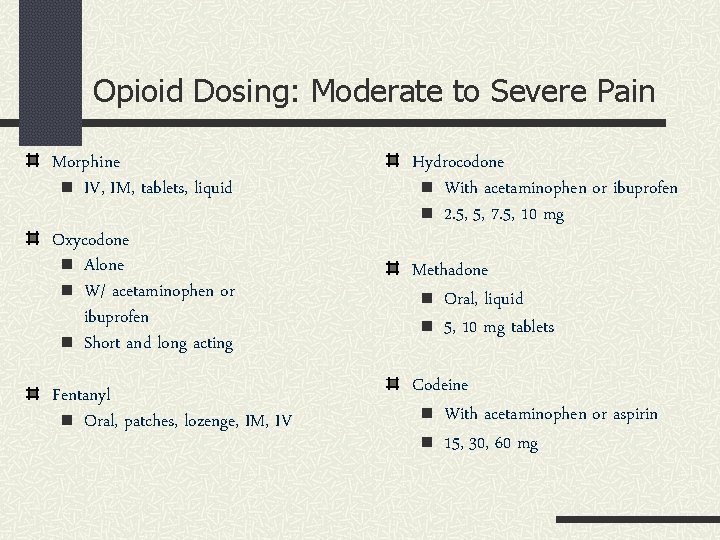
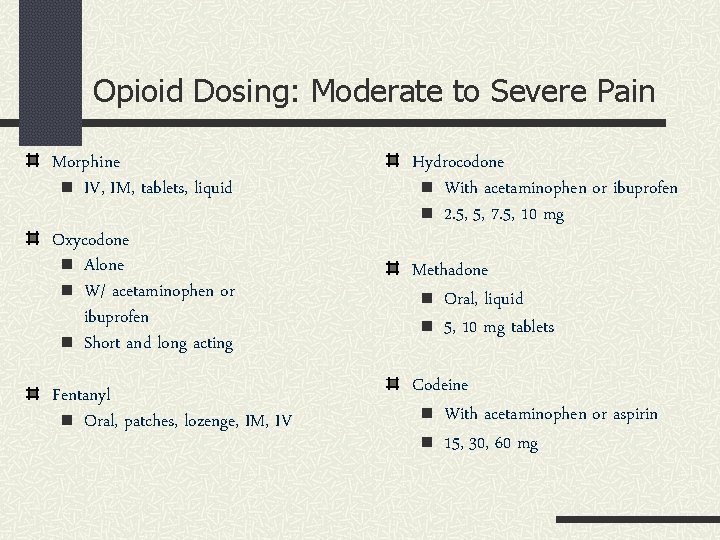
Opioid Dosing: Moderate to Severe Pain Morphine n IV, IM, tablets, liquid Oxycodone n Alone n W/ acetaminophen or ibuprofen n Short and long acting Fentanyl n Oral, patches, lozenge, IM, IV Hydrocodone n With acetaminophen or ibuprofen n 2. 5, 5, 7. 5, 10 mg Methadone n Oral, liquid n 5, 10 mg tablets Codeine n With acetaminophen or aspirin n 15, 30, 60 mg
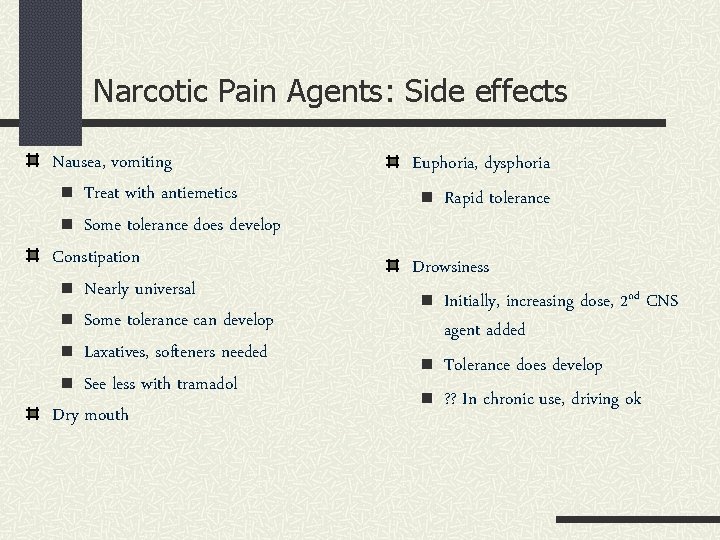
Narcotic Pain Agents: Side effects Nausea, vomiting n Treat with antiemetics n Some tolerance does develop Constipation n Nearly universal n Some tolerance can develop n Laxatives, softeners needed n See less with tramadol Dry mouth Euphoria, dysphoria n Rapid tolerance Drowsiness n Initially, increasing dose, 2 nd CNS agent added n Tolerance does develop n ? ? In chronic use, driving ok

Narcotic Pain Agents: Side effects Respiratory depression n in opioid-naïve patient n Remains #1 reason for morbidity in chronic use n Precaution in those with underlying pulmonary disease n See less with tramadol Itching (not true allergy) n From histamine release n Rapid tolerance n Antihistamines Reduced hormone levels n Ie low T in males
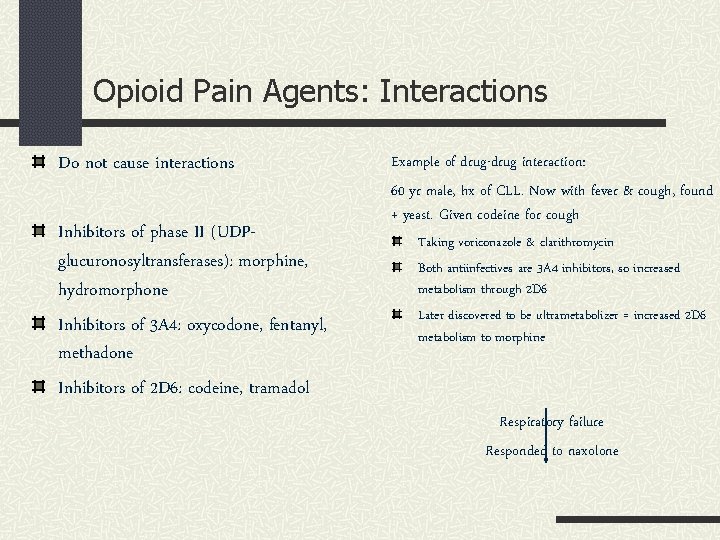
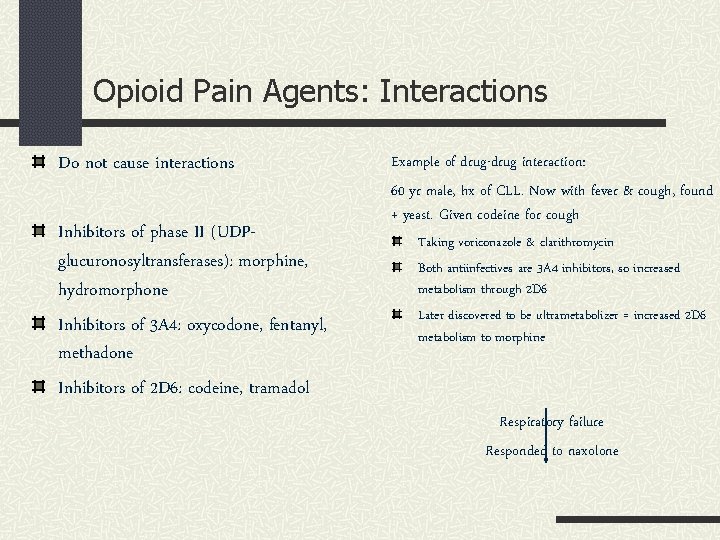
Opioid Pain Agents: Interactions Do not cause interactions Inhibitors of phase II (UDPglucuronosyltransferases): morphine, hydromorphone Inhibitors of 3 A 4: oxycodone, fentanyl, methadone Inhibitors of 2 D 6: codeine, tramadol Example of drug-drug interaction: 60 yr male, hx of CLL. Now with fever & cough, found + yeast. Given codeine for cough Taking voriconazole & clarithromycin Both antiinfectives are 3 A 4 inhibitors, so increased metabolism through 2 D 6 Later discovered to be ultrametabolizer = increased 2 D 6 metabolism to morphine Respiratory failure Responded to naxolone
Other Opioid Pain Agents The opioid agents n Tramadol (Ultram, Ultram ER) n Tapentadol (Nucynta, Nucynta ER ) Mu agonist and inhibition of norepinephrine / serotonin reuptake n Tramadol n Tapentadol (no serotonin affect)
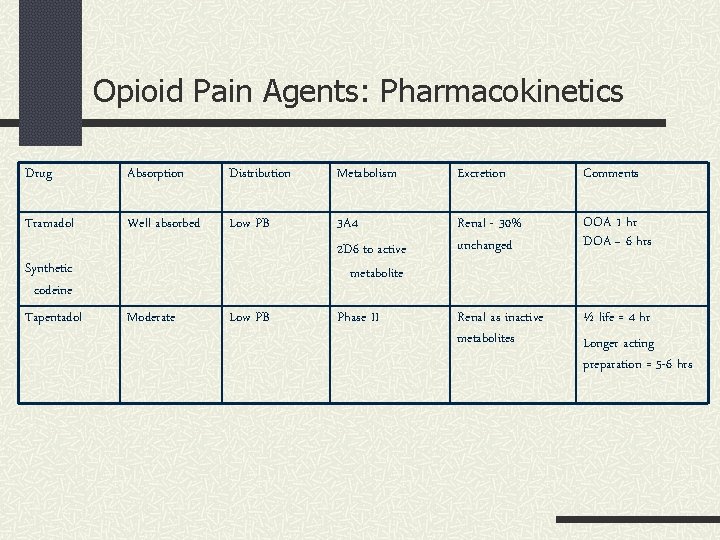
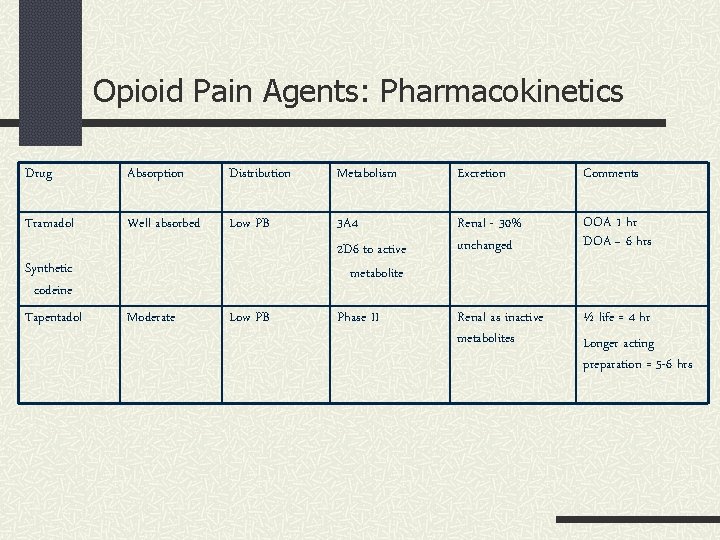
Opioid Pain Agents: Pharmacokinetics Drug Absorption Distribution Metabolism Excretion Comments Tramadol Well absorbed Low PB Renal - 30% unchanged OOA 1 hr DOA ~ 6 hrs Synthetic codeine Tapentadol 3 A 4 2 D 6 to active metabolite Moderate Low PB Phase II Renal as inactive metabolites ½ life = 4 hr Longer acting preparation = 5 -6 hrs

Opioid Pain Agents: Uses and dosing Drug and Use Dosing forms / dosing Dosing adjustment Tramadol IR: every 4 to 6 hrs tabs Max 400 mg daily Reduced liver or renal function: Patients with seizure disorder Lower dose Use caution with other No ER use serotonergic agents For mild to moderate pain Ultracet: tramadol / acetaminophen Precautions Risk for abuse exists Tramadol ER: once daily Tapentadol Moderate to severe pain 50, 75, or 100 mg every 4 to 6 hrs Renal as inactive metabolites tabs Less concern with other serotonergic agents Abuse potential = Schedule II drug
In-class exercise: Opioid use issues In same discussion group 2. Discuss and write down your group’s definition of a. Tolerance b. Dependence c. Addiction d. Abuse 3. Submit as group 1.
Issues with Opioid use
Opioid use issues Desensitization: See decrease effectiveness n Short-term effect, begins with minutes to hours Tolerance: Progressive loss of drug effect n Tendency to adapt to presence of opioids n Loss of drug effectiveness, both analgesia and side effects n Is reversible n Definition: MS 60 mg, oxycodone 30 mg, or hydromorphone 8 mg daily for > 1 week Hyperalgesia: State of nociceptive sensitization 2 nd to opioids n Characterized by paradoxical response, see increased sensitivity to painful stimuli

Opioid use issues Dependence n n n See when drug is discontinued = withdrawal syndrome Symptoms 2 nd to activation Ie agitation, dilated pupils, elevated temp, HTN, diarrhea Addiction n Psychological craving See with recreational use Not caused by tolerance or dependence Abuse = Misuse of opioids n See unacceptable behaviors n Stealing drugs n Forging prescriptions n Buying drugs on street n Diversion and selling
Opioid use issues Medical work-up n History, exam, x-rays, blood work Consider psychological evaluation Approach n Non-pharm modalities n Combo medications n Lowest dose Pain contract Monitoring n Pain relief n Ability to maintain daily activities n Abuse behaviors
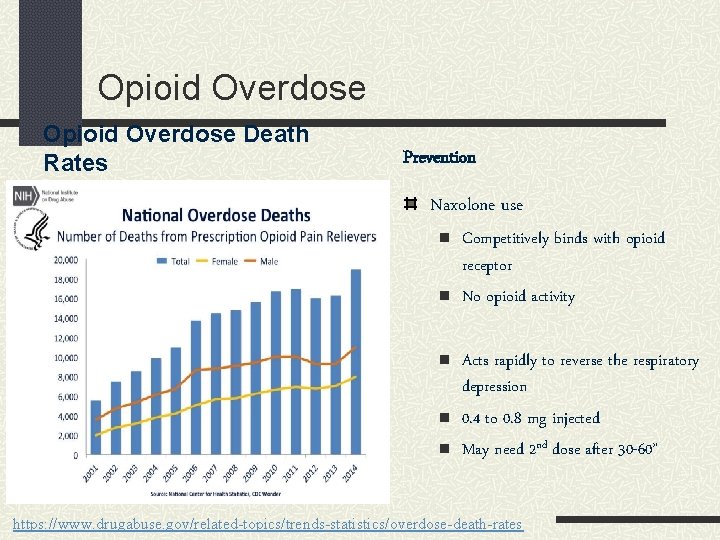
Opioid Pain Agents in Utah In 2015, 12. 6 per 100, 00 adults died 2 nd to prescription opioids Utah ranked 7 th in U. S. for drug poisoning deaths (20132015) Utah experienced a nearly 400% increase in deaths from 2000 to 2014 2 nd to misuse and abuse of prescription drugs Since 2002, deaths 2 nd to opiate outnumbered deaths due to n All other prescriptions n MVA, falls, or firearms Deaths due to oxycontin/percocet accounted for 55%
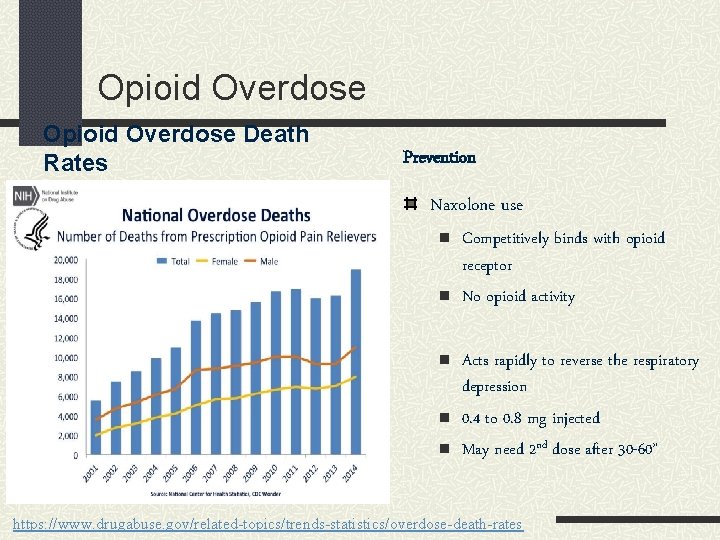
Opioid Overdose Death Rates Prevention Naxolone use n n n Competitively binds with opioid receptor No opioid activity Acts rapidly to reverse the respiratory depression 0. 4 to 0. 8 mg injected May need 2 nd dose after 30 -60” https: //www. drugabuse. gov/related-topics/trends-statistics/overdose-death-rates

In Utah 2010, H. B. 28: Requires controlled substance prescribers to register to use the controlled substance database. 2011, S. B. 61: Requires prescribers renewing or applying for a controlled substance license to take controlled substance prescribing classes. 2014, H. B. 11: Enables bystanders to report an overdose without fear of criminal prosecution for illegal possession of a controlled substance or illicit drug. 2014, H. B. 119: Permits physicians to prescribe naloxone to third parties. Permits individuals to administer naloxone without legal liability.

Opioid Overdose: Naxolone Pretty simple, as read directly from Utah HB (now law) 119: HB 119 permits dispensing and administration of an opiate antagonist to a person who is reasonably believed to be experiencing an opiate-related drug overdose event; establishes immunity for good faith administration of an opiate antagonist; clarifies that it is not unlawful or unprofessional conduct for certain health professionals to prescribe an opiate antagonist to: a person at increased risk of experiencing an opiate-related drug overdose event; or a family member, friend, or other person in a position to assist a person who is at increased risk of experiencing and requires a person who prescribes or dispenses an opiate antagonist to advise a person to seek a medical evaluation after experiencing a drug overdose and taking an opiate antagonist

Opioid Overdose: Naxolone Pharmacies with Naloxone Rescue Kits The Apothecary Shoppe. Located within the Salt Lake Regional Medical Center, The Apothecary Shoppe has Naloxone Rescue Kits readily available. They also offer training on recognizing signs of an opiate overdose, and how to administer Naloxone. They have a Collaborative Practice Agreement (CPA) in place which means that you can get a kit without a prescription. Intermountain Healthcare Pharmacies Greenwood and Redwood Health Centers – Pharmacy Veterans Affairs Medical Center Pharmacy (VA)
In Utah: Naxolone http: //www. utahnaloxone. org
Adjunct Pain Medications
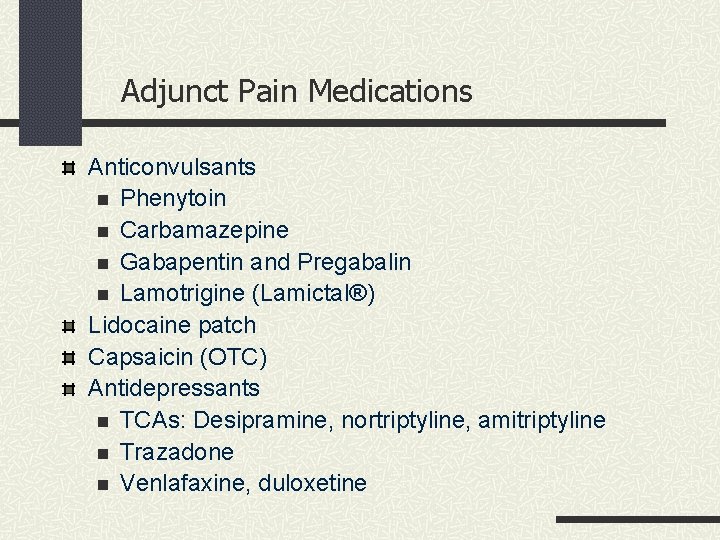
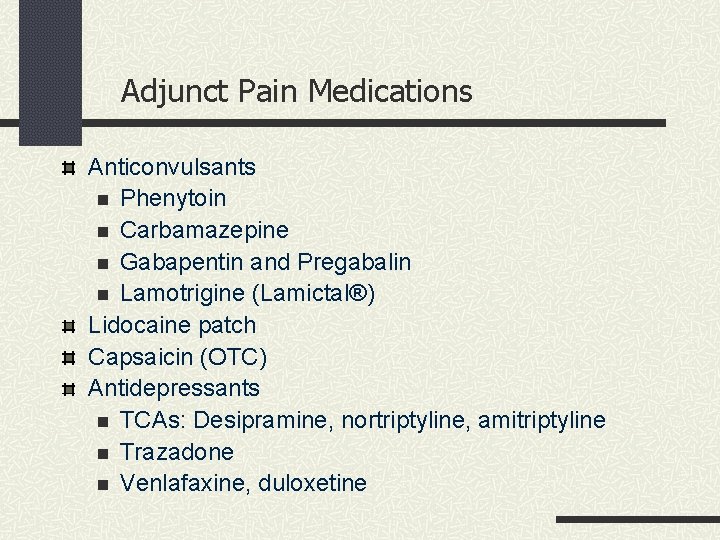
Adjunct Pain Medications Anticonvulsants n Phenytoin n Carbamazepine n Gabapentin and Pregabalin n Lamotrigine (Lamictal®) Lidocaine patch Capsaicin (OTC) Antidepressants n TCAs: Desipramine, nortriptyline, amitriptyline n Trazadone n Venlafaxine, duloxetine

Adjunct Pain Medications: Anticonvulsants FDA alert 2008 Increased risk of suicidal behavior with antiepileptic medications as compared to placebo MOA of Anticonvulsants Modulate voltage-dependent ion (Na, Ca, K, Cl) channels Inhibit activity of excitatory neurotransmitters (glutamate, Ach) Enhance activity of GABA
Adjunct Pain Medications: Phenytoin Dilantin, Phenytek Useful for partial, generalized seizures Other uses: Chronic pain syndromes (neuropathic) MOA n Blocks voltage-dependent sodium channels n Extends the inactivated phase

Adjunct Pain Medications: Phenytoin Pharmacokinetics 70 -100% bioavailable 90 -95% (adults), > 85% (infants) protein binding n Small Vd n Obtain free serum concentrations Substrate of CYP 2 C 9, 2 C 19 n Dose-dependent kinetics, capacity-limited n Small in dose, non-proportional in drug concentration Excretion n < 5% as unchanged drug n Glucuronide ½ life – average 22 hours
Adjunct Pain Medications: Phenytoin Usual dosage n 100 /300 mg capsules (extended and immediate release), chewable tablets, suspension 125 mg/5 ml, IV n Given daily or BID dosing What happens when a patient’s dose is 300 mg/day of phenytoin and a serum concentration of 8 ng/ml is still resulting in seizures? What should be done? Double the dose? Increase the dose by 30 -50 mg/day? Increase the dose by 100 mg/day?
Adjunct Pain Medications: Phenytoin Systemic side effects n Acne, gingival hyperplasia, facial coarsening, osteopenia, folate, CBC changes Neurotoxic side effects n n Nystagmus, ataxia, mental clouding, slurred speech > 20 ng/ml – see Nystagmus > 30 ng/ml – see Ataxia > 40 ng/ml – see Mental clouding ADRs: Steven-Johnson syndrome / toxic epidermal necrolysis Drug-drug interactions n Is an inducer of 2 C 9, 2 C 19, 3 A 4 n Interacts with highly protein bound drugs
Adjunct Pain Medications: Carbamazepine Tegretol, Carbatrol Indications: partial & generalized seizures Other uses n Pain n Bipolar disorder n Agitation in the elderly Works in similar manner to phenytoin, blocks voltagedependent sodium channels
Adjunct Pain Medications: Carbamazepine Pharmacokinetics 80% bioavailibility ~70% protein bound Metabolism by 3 A 4 Excretion n 1 – 3% as unchanged drug, rest as metabolite ½ life: depends on dosing n Initially, 18 -55 hours n Maintenance, children: 8 -14 hrs, Adults: 12 -17 hrs
Adjunct Pain Medications: Carbamazepine Usual dosage n Immediate and extended release Monitor n Serum drug concentration n More frequently initially 2 nd to autoinduction n CBC n Leukopenia (~12% children, 7% adults) n Typically occurs during first months of use n Aplastic anemia (rare) n Monitor for symptoms
Adjunct Pain Medications: Carbamazepine Side effect and ADRs n Systemic: GI upset, rashes, SIADH (dilutional hyponatremia) n Neurotoxic: drowsiness, dizziness, double vision, lethargy, headache n ADRs: steven-johnson syndrome / toxic epidermal necrolysis Drug-drug interactions n Strong inducer of CYP 1 A 2, 2 C 9, 3 A 4 n Autoinducer
Adjunct Pain Medications: Gabapentin Neurontin Useful n Add-on therapy for refractory partial seizures Use for other conditions n Neuropathic/other pain syndromes n Restless leg syndrome n Migraine n Bipolar n Elderly agitation
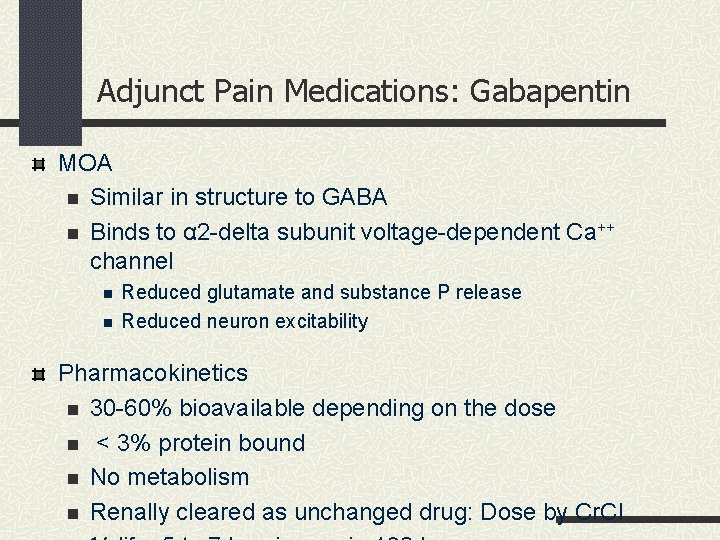
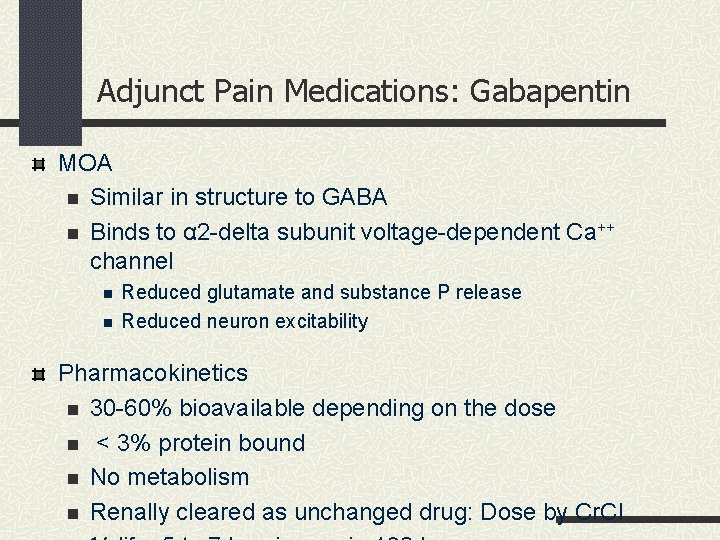
Adjunct Pain Medications: Gabapentin MOA n Similar in structure to GABA n Binds to α 2 -delta subunit voltage-dependent Ca++ channel n n Reduced glutamate and substance P release Reduced neuron excitability Pharmacokinetics n 30 -60% bioavailable depending on the dose n < 3% protein bound n No metabolism n Renally cleared as unchanged drug: Dose by Cr. Cl

Adjunct Pain Medications: Gabapentin Dosage n Initial dose 300 mg/day, the BID, then TID n Increased to 1800 mg/day, doses up to 3600 mg/day used n Renal function dependent (in divided doses) Side effects n Peripheral edema (2%), pruritus (1%) n Neuro side effects: Fatigue, ataxia, drowsiness n In children: hostility/emotional lability 4 to 8% Does not induce/inhibit metabolism
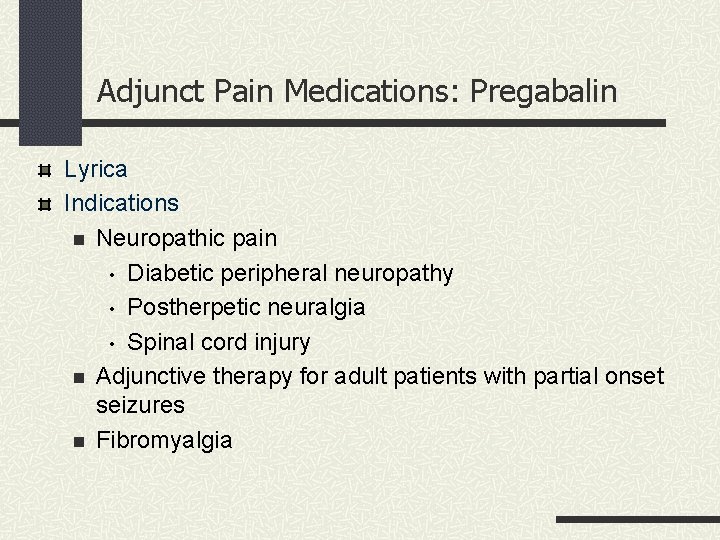
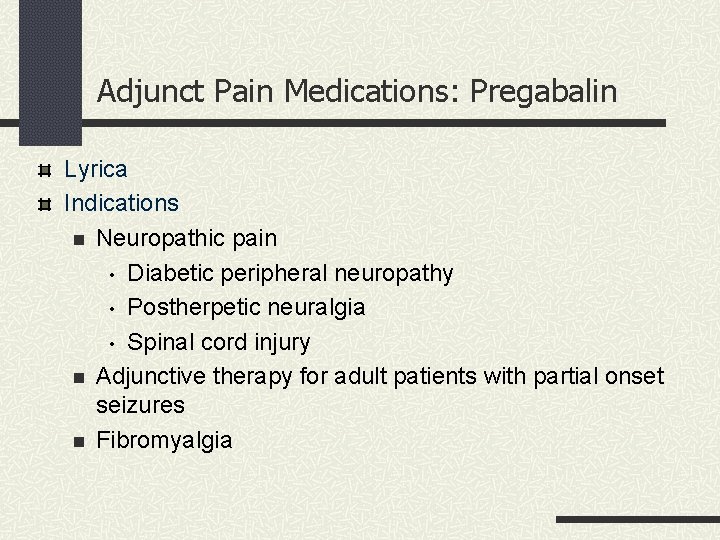
Adjunct Pain Medications: Pregabalin Lyrica Indications n Neuropathic pain • Diabetic peripheral neuropathy • Postherpetic neuralgia • Spinal cord injury n Adjunctive therapy for adult patients with partial onset seizures n Fibromyalgia
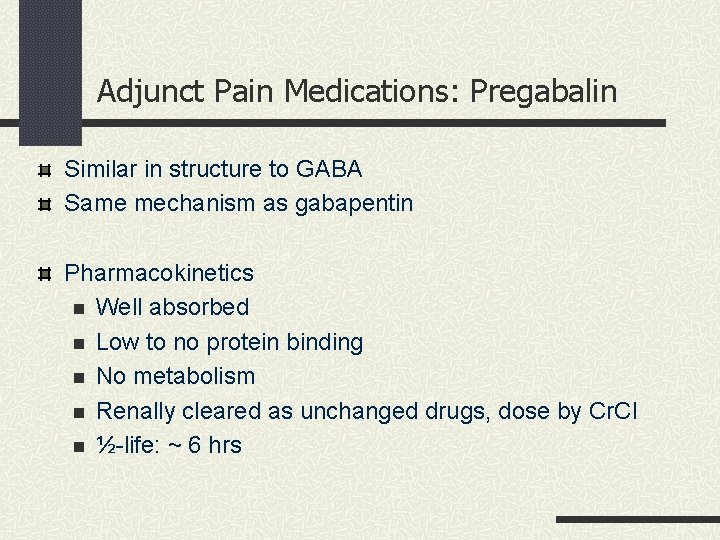
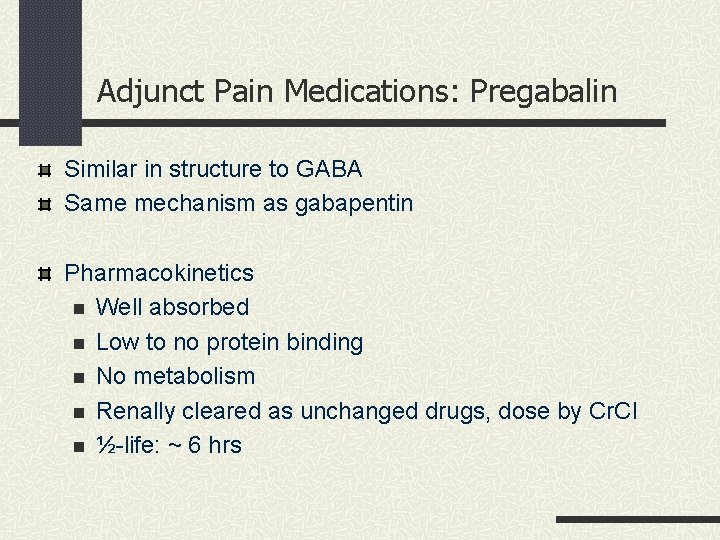
Adjunct Pain Medications: Pregabalin Similar in structure to GABA Same mechanism as gabapentin Pharmacokinetics n Well absorbed n Low to no protein binding n No metabolism n Renally cleared as unchanged drugs, dose by Cr. Cl n ½-life: ~ 6 hrs
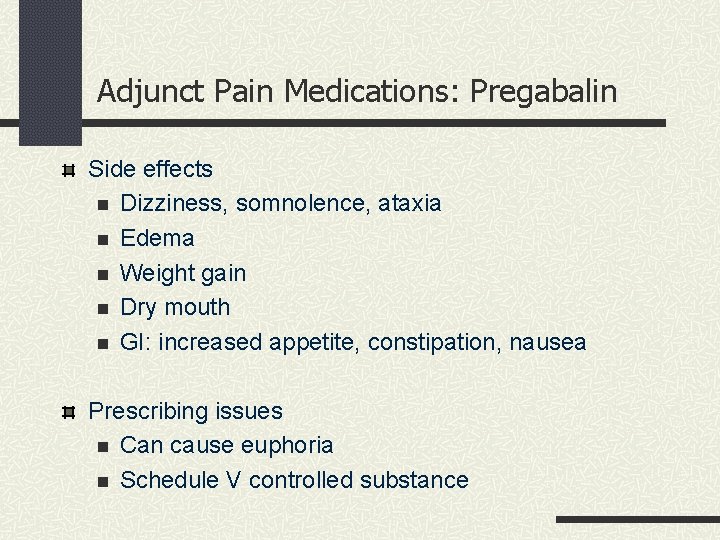
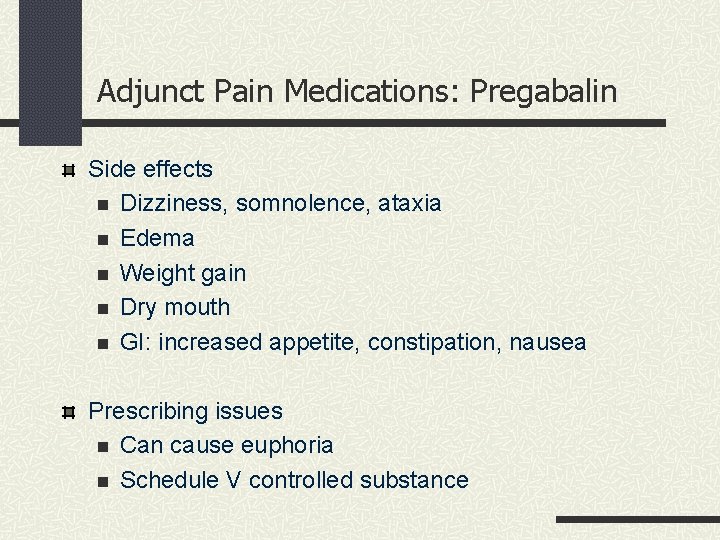
Adjunct Pain Medications: Pregabalin Side effects n Dizziness, somnolence, ataxia n Edema n Weight gain n Dry mouth n GI: increased appetite, constipation, nausea Prescribing issues n Can cause euphoria n Schedule V controlled substance
Adjunct Pain Medications: Lamotrigine Lamictal® Use n Adjunct agent for seizures: Partial, generalized tonicclonic n Bipolar disease n Pain syndromes MOA n Appears to also inactive voltage-dependent Na channels n May also decrease synthesis of excitatory neurotransmitters n Glutamate and aspartate
Adjunct Pain Medications: Lamotrigine Pharmacokinetics 98% bioavailability Not highly-protein bound (55%) Metabolized to glucuronide conjugate Urine excretion n 94% as conjugate Does not induce/inhibit metabolism But may be induced/inhibited by other meds n Estrogens induce metabolism
Adjunct Pain Medications: Lamotrigine Dosing n Initial dose is 25 mg BID n Extended-release form available for once daily dose n Can be titrated up n If on valproate, lower initial dose • Ie 12. 5 to 25 mg QOD, then increasing by 25 mg every 2 wks
Adjunct Pain Medications: Lamotrigine Side effects n Systemic: rash, nausea n Neurotoxic: dizziness, somnolence ADRs • Life threatening rash if titrated too quickly • ~ 1 in 1000 patients will experience • Or, combined with valproic acid (inhibits metabolism) • Stop drug if occurs
Adjunct Pain Medications: Lidocaine patch 5% Comprised of an adhesive material containing 5% lidocaine Applied to a non-woven polyester felt backing and covered with a polyethylene terephthalate (PET) film release liner Patch is 10 cm x 14 cm Indications and usage n Pain associated with post-herpetic neuralgia
Adjunct Pain Medications: Lidocaine patch Dosage and administration n Apply LIDODERM to intact skin to cover most painful area n Apply up to three patches, only once for up to 12 hours within a 24 -hour period n Patches may be cut into smaller sizes n Clothing may be worn over the area of application

Adjunct Pain Medications: Lidocaine patch Side effects n Application Site Reactions n Reactions generally mild/transient n Resolves spontaneously within a few minutes to hours Allergic Reactions n Rarely, allergic and anaphylactic reactions
Adjunct Pain Medications: Capsaicin (OTC Chemical compound capsaicin (8 -methyl-N-vanillyl-6 -nonenamide) Is active component of chili peppers (belongs to genus Capsicum) Appears to deplete local substance P Indications n To relieve chronic pain n Arthritis n Post-herpetic n Diabetic neuralgia neuropathy Cream, lotion, patch, liquid, gel, solution, ointment, etc n Topical: Apply 3 to 4 times daily n Careful to wash fingers after applying
Treatment Always include non-pharmacological method Use one or several modalities Centrally versus peripherally acting drugs n Combinations of non-opiate and opiates n Peripherally: NSAIDs n Central: Opiates, tramadol n Examples • Acetaminophen or NSAID with opiate • Tramadol with acetaminophen
Treatment Advantages Increased pain relief, drugs work via different MOA Rates of onset of activity or duration of activity differ May be able to use less of both drugs May see less adverse reactions or effects
Treatment Approach to Nociceptive Pain Chronic pain Typically due to MS, inflammation, mechanical causes Assess severity of pain and impact on function/QOL Medication used along with nonpharmacological approaches Mild to moderate pain n Acetaminophen n NSAIDs (consider with PPI) or COX 2 inhibitors n Topical agents Moderate to severe pain n Acetaminophen, NSAIDs, COX-2 inhibitor n TCAs or SNRI
Treatment Approach to Neuropathic Pain Chronic Pain Typically due to damage or pathology w/in nervous system Important to distinguish from nociceptive pain First-line agents n Antidepressants: TCAs, SNRIs n Anticonvulsant drugs: gabapentin, pregablin n Topical agents Second-line agents n Other anticonvulsant drugs: carbamezapine, valproic acid n Tramadol Third-line agents
Last In-class assignment In same discussion groups Assignment 3 Create an acute pain scenario. Pick a medication to treat your patient's pain. Discuss why you chose this medication. Assignment 4 Create a chronic pain scenario. Pick 2 medications to treat your patient's pain. Discuss why you chose these medications.
 How do we treat the life the life how we treat
How do we treat the life the life how we treat Ward basket system
Ward basket system Mad pain
Mad pain Is pregnancy pain same as period pain
Is pregnancy pain same as period pain Chapter 11 medications and drugs
Chapter 11 medications and drugs Which seedless plants have been used to treat bee stings?
Which seedless plants have been used to treat bee stings? Is byetta used to treat pcos
Is byetta used to treat pcos Why are seedless plants important
Why are seedless plants important Pms vs pregnancy
Pms vs pregnancy Common pediatric medications
Common pediatric medications Epidural needle markings
Epidural needle markings Hepatitis c symtoms
Hepatitis c symtoms List of high-alert medications jci
List of high-alert medications jci Mock code steps
Mock code steps 5 rights of medication
5 rights of medication Chapter 30 administering medications
Chapter 30 administering medications Medications
Medications Sick day medication
Sick day medication Medication reconciliation معني
Medication reconciliation معني High risk medications
High risk medications Chapter 30 administering medications
Chapter 30 administering medications Peripheral nervous system medications
Peripheral nervous system medications Poss scale
Poss scale Karma etkili opioidler
Karma etkili opioidler Bromazepam umrechnungstabelle
Bromazepam umrechnungstabelle Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Non-opioid
Non-opioid Mechanism of action of opioid analgesics
Mechanism of action of opioid analgesics What is pain
What is pain Opioid receptors location
Opioid receptors location Brian erickson md
Brian erickson md Opioid settlement calculator
Opioid settlement calculator Non-opioid
Non-opioid Kentucky opioid response effort
Kentucky opioid response effort Who is mr. kirwin and how does he treat victor?
Who is mr. kirwin and how does he treat victor? Adjunct to secondary survey
Adjunct to secondary survey Primary survey adjuncts
Primary survey adjuncts Ample history
Ample history Mood adjunct
Mood adjunct Adjunct model content-based instruction
Adjunct model content-based instruction What is an adjunct display
What is an adjunct display Properties of adjoint
Properties of adjoint Examples of adjunct
Examples of adjunct Adjunct professor
Adjunct professor Perbedaan complement dan adjunct
Perbedaan complement dan adjunct Adjunct adverbial
Adjunct adverbial Adjunct poverty definition
Adjunct poverty definition Innovative staff solution
Innovative staff solution Mercy college adjunct positions
Mercy college adjunct positions Chapter 4 section 3 the persian empire
Chapter 4 section 3 the persian empire Equation for number needed to treat
Equation for number needed to treat Invitation to treat
Invitation to treat Romeo and juliet jokes
Romeo and juliet jokes Number needed to treat calculation
Number needed to treat calculation Invitation to treat
Invitation to treat Mylantah
Mylantah Calculate number needed to harm
Calculate number needed to harm How to calculate number needed to treat
How to calculate number needed to treat