MEDICARE SAVINGS PROGRAM MSP Health Insurance Training Center

- Slides: 34
MEDICARE SAVINGS PROGRAM (MSP) Health Insurance Training Center (HITC) New York State Public Health Insurance Programs Sponsored by the New York State Department of Health through a training and administrative services agreement with CAI Global
2 Medicare Savings Program (MSP) • Explanation of Medicare • MSP Categories o Qualified Medicare Beneficiaries (QMB) o Specified Low Income Medicare Beneficiaries (SLMB) o Qualified Individuals (QI) o Qualified Disabled and Working Individuals (QDWI) • Program Benefits

3 What Is Medicare • A federal health insurance program available to individuals receiving Social Security Benefits • Criteria to participate in Medicare: o o 65 yrs or older On SSD for 24 months Renal Dialysis for 3 months ALS - Amyotrophic Lateral Sclerosis § (AKA Lou Gehrig’s disease)
4 4 Parts to Medicare • Medicare Part A (Inpatient Coverage) o Free for most people • Medicare Part B (Outpatient Coverage) o Has a premium • Medicare Part C (Medicare Advantage Plans) o Cost varies based on the type of plan purchased • Medicare Part D (Prescription Coverage) o Premiums vary by health plan
6 Medicare Savings Program • A program that can assist individuals/couples in paying for their Medicare Premiums
7 Medicare Savings Programs • 4 Medicare Savings Programs o o Qualified Medicare Beneficiaries (QMB) Specified Low Income Medicare Beneficiaries (SLMB) Qualified Individuals (QI) Qualified Disabled and Working Individual (QDWI)
8 MSP Application • MSP applicants may complete DOH-4328 (shortened application) • QMB and SLMB applicants that are also applying for Medicaid must follow Medicaid eligibility rules and: o Complete the “Access New York Application” (DOH-4220) and “Supplement A” (DOH-5178 A) o May complete the “PA, Medicaid, FS, Services” combined application (LDSS-2921)
9 MSP Application, cont’d. • All MSP applications received at the LDSS must first be checked for eligibility on the Marketplace • Eligibility can be check by utilizing the “Client Search” tab in e. Med. NY o Search by SSN • If active on the Marketplace, fax the MSP application to the Third Party Liability unit o (518)473 -0601 • Third Party unit will process for a MIPP payment
10 MSP Eligibility Criteria • New York State Resident • Citizen or have satisfactory Immigration Status • Must apply for available Social Security benefits when applying for Medicare
11 MSP Eligibility Criteria, cont’d. • QMB o Must have Medicare Part A or be eligible for Medicare Part A • SLMB & QI o Must have Medicare Part A
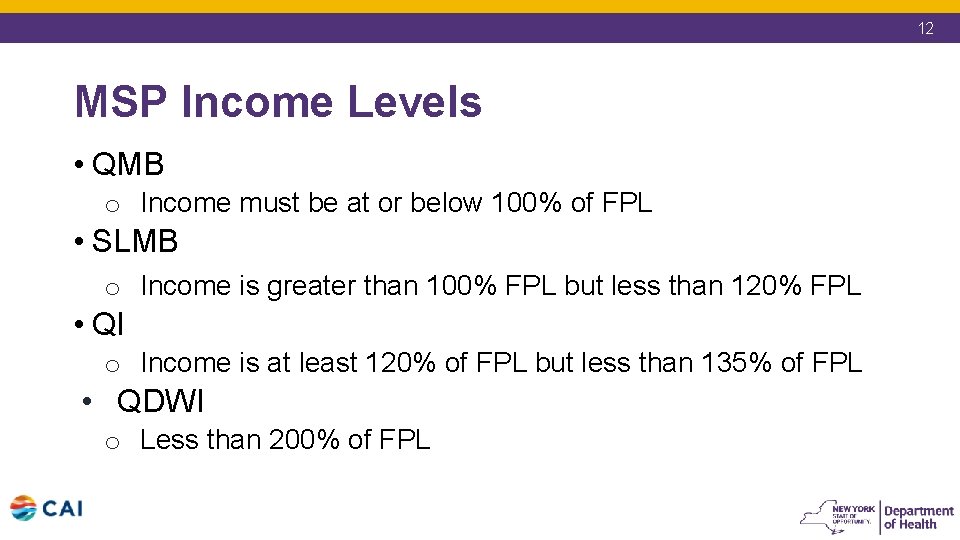
12 MSP Income Levels • QMB o Income must be at or below 100% of FPL • SLMB o Income is greater than 100% FPL but less than 120% FPL • QI o Income is at least 120% of FPL but less than 135% of FPL • QDWI o Less than 200% of FPL
13 MSP Resources • QMB, SLMB and QI o No Resource Test • QDWI A/Rs may attest to resources o Individual Level - $4000 o Couple Level - $6000
14 QMB Benefits • Medicare Part A & B premiums reimbursed • Deemed eligible for the Low Income Subsidy (LIS) Part D benefit • Medicare Co-Insurances and Deductibles paid including: o Chiropractor o Podiatry o Clinical Social Worker • Can be fully eligible for Medicaid or can spend down to the Medically Needy (MN) level
17 SLMB Benefits • Medicare Part B premium is reimbursed • Deemed eligible for the Low Income Subsidy (LIS) Part D benefit • Can spend down to the Medically Needy (MN) level
19 QI Benefits • Medicare Part B premium is reimbursed • Deemed eligible Low Income Subsidy (LIS) Part D benefit • Cannot spend down to be Medicaid eligible o Must choose between QI or Medicaid • Auto renewals based on WMS, e. Med. NY and MABEL
20 QDWI • Reimbursement of their Part A Premium
21 MSP Budgeting • SSI-R Budget (04) • Buy in indicator “A” • Household size 1 or 2 o Based on Buy-In Indicator and LA code: 1 or 2 • Use gross Social Security income • Do not allow Medicare Part B premium as a deduction
24 MSP Eligibility • QMB: o o Eligibility must be prospective Reimbursement begins the month after Medicaid eligibility starts • SLMB: o Eligibility may be determined 3 months retro • QI: o Eligibility may be determined 3 months retro but MUST be within the same calendar year
25 QMB Application Date – 7/5/19 QMB starts – 8/1/19 3209 screens 1 & 5 – 7/1/19 – 6/30/20 e. Med. NY – 8/1/19 Auth “From” date MUST be one month prior to QMB enrollment in e. Med. NY
26 SLMB Application Date – 6/15/19 Requesting 3 months Retro Coverage • March-May 3209 screens 1 & 5 – 3/1/19 to 5/31/20 e. Med. NY – 3/1/19
27 QI Application Date – 3/7/19 Requesting 3 months Retro Coverage • December - February 3209 screens 1 & 5 – 1/1/19 to 12/31/49 e. Med. NY – 1/1/19 Retro must be in the same calendar year
28 QMB Coverage Codes • Income below the MN Level o Coverage Code as appropriate § See Attestation of Resources 04 ADM/06 • Income above the MN Level but less than or equal to 100% FPL o Coverage Code 09 • May spend down to the MN Level for Medicaid eligibility
29 SLMB Coverage Codes • Coverage Code 09 • May spend down to the MN Level for Medicaid eligibility
30 QI Coverage • Coverage Code 09 • Cannot spend down for Medicaid eligibility
31 MSP and MA Eligibility for SSI-R and Non SSI-R Spouses • A two step process must be used o GIS 10 MA/10 o For MSP eligibility, enter the Buy-In Indicator of an “A” in the Buy-In field in MABEL § Print and store the MSP budget in the case record o For Medicaid eligibility, remove the Buy-In Indicator of an “A” § Store the Medicaid budget in MABEL
32 e. Med. NY • e. Med. NY entries must be done before reimbursement will begin o QMB – P o SLMB – L o QI – U o QDWI – X
34 e. Med. NY, cont’d. • Certain closing transactions in WMS will trigger the closing of the Buy-In span in e. Med. NY o GIS 14 MA/20 o Buy-In span closed at the end of the clock down period • Closing codes other than those listed in GIS 14 MA/20, span must be ended manually in e. Med. NY
35 The Medicare Improvements for Patients and Providers Act of 2008 (MIPPA)
36 MIPPA • Effective January 1, 2010, an application for the Medicare Part D Low Income Subsidy will be considered an application for the Medicare Savings Program • MSP applications will be transmitted daily via a file transferred from SSA to NYS
37 MIPPA, cont’d. • Currently no automated process • Interim procedures implemented • 10 OHIP/ADM-3
38 MIPPA Interim Procedures • File will be provided to the LDSS o Application date is the date they applied for the LIS o 45 days for processing begins when the State receives the file from SSA • If LIS applicant has an active MSP case there is no further action
39 MIPPA Interim Procedures, cont’d. • If LIS applicant has an active or pending Medicaid Case with no active MSP then the LDSS must make an MSP determination o Send notice
40 MIPPA Interim Procedures, cont’d. • If LIS applicant has an active Medicaid case with a spenddown or is only eligible for Medicaid because they are using the Part B premium as a deduction the LDSS must send a letter giving them the choice of MSP or spenddown o Recipient indicates choice and returns letter
41 MIPPA Interim Procedures, cont’d. • If LIS applicant does not have an active or pending Medicaid case the LDSS must send a cover letter and Request for Information form o If form is returned determine MSP eligibility and send notice o If form is not returned send denial for failure to return information