Medicare Recovery Audit Process TARA WALKER PRACTICUM PROJECT


- Slides: 23
Medicare Recovery Audit Process TARA WALKER PRACTICUM PROJECT - HCMT 2030
Medicare Fee For Service Recovery Audit Program Tax Relief and Health Care Act of 2006 required CMS to implement Medicare recovery auditing in all states. Recovery auditing began in 2010 and could audit records from 2007. Purpose- To identify and correct improper Medicare paymentsoverpayments/underpayments and use this information to implement actions that will prevent future improper payments. Medicare Parts A & B Four regional RACs, Ohio is in Region 1 (Performant)
Medicare Fee For Service Recovery Audit Program Can only audit approved issues Can only request a specific number of records to audit every 45 days. Limits for inpatient, outpatient, reviews (type of bill). Reviews claims post payment Can only audit records within three years from last paid date. Audits can be appealed
Performant RAC for Region 1, which includes Ohio, Indiana, Kentucky, Connecticut, Main, Michigan, Massachusetts, New Hampshire, Rhode Island, and Vermont Also reviews Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) and Home Health / Hospice for all 50 states.

Complex and Automated Reviews Complex Review- The RAC will request specific parts of the medical record and reviews them to make clinical determination or coding validation. The provider will receive a review of results letter (RRL). Automated Review- The RAC analyzes the claims data for errors and makes a determination. No records are requested. The provider will then receive an initial findings letter.
Approved Issues RAC can only audit approved issues Approved issues for Region 1 can be found at https: //performantrac. com/audit-regions/region-1/ Issues are listed with issue number, type of audit (complex or automated), provider type the issue applies to, and date the issue was approved.

CMS Approved Audits
Additional Documentation Request (ADR) Provider has 30 days to submit documentation RAC has 60 days to respond after documentation is submitted. Response will be in the form of an Initial Findings letter or Review of Results Letter Results of ADR request may be: § No Findings § Under Payment § Overpayment, may be related to: o DRG o Documentation didn’t meet medical necessity o Billing related o Charge master Organization reviews findings and then agrees or disagrees with findings.
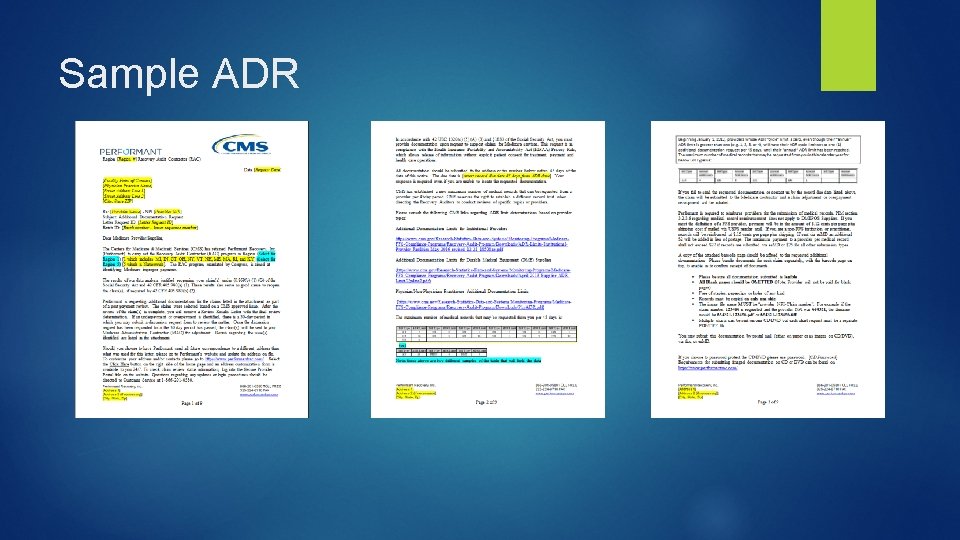
Sample ADR
Sample ADR
Discussion Period This is a request for the RAC to review the audit. * Requests may be submitted within 30 days of Initial findings letter or Review of Results Letter(RRL). Discussion Period is with the RAC. If the audit is overturned at the Discussion Level, the audit will be closed and the provider will not be turned over to the MAC for adjustment. RAC will respond within 30 days of the Discussion Period with a decision letter.
Sample Discussion Period Request
Demand Letter This letter demands repayment for specific records. RAC demand letter starts time limit for appeal period. The organization may be asked to submit additional records. The organization has 120 days from date on Demand letter to submit an appeal.
Appeals The appeals process starts once the demand letter has been received. This process has five levels: Redetermination, Reconsideration, ALJ Hearing, Medicare Appeals Council Review, and Judicial Review. This process can take months and even years to resolve depending on the levels are appealed.
Appeals: Redetermination 1 st Level Performed by MAC (Medicare Authorized Contractor) Documentation review of initial claim determination Request appeal up to 120 days after initial determination Decision within 60 days
Appeals: Reconsideration 2 nd Level Performed by QIC (Qualified Independent Contractor) Document review of redetermination Request appeal up to 180 days after receiving MRN (Medicare Redetermination Notice) Decision within 90 days
Appeals: ALJ Hearing 3 rd Level Performed by ALJ May be an on the record review or may be an interactive hearing between parties Request appeal up to 60 days after notice of QIC decision or after expiration of applicable QIC reconsideration timeframe if decision is not received. Decision may be delayed due to volume
Appeals: Medicare Appeals Council Review 4 th Level Medicare Appeals Council Review Performed by Appeals Council Document review of ALJs decision or dismissal but may request oral arguments Request for appeal must be within 60 days after you receive notice of ALJs decision or after expiration of the applicable ALJ hearing timeframe if you do not receive a decision. Decisions should be received within 90 days if appealing an ALJ decision or 180 days if ALJ time expired without a decision.
Appeals: Judicial Review 5 th Level U. S. District Court Judicial Review Requests for appeal must be up to 60 days after notice of Appeals Council decision or after expiration of the applicable Appeals Council reviews timeframe if you do not receive a decision.
Organizational Response to Audits Unfavorable audits have a direct affect on an organization’s bottom line. Healthcare organizations must be proactive in their preparation for audits. Education programs should be implemented to ensure proper documentation. Education programs should be developed for each department in the revenue cycle and their role in the audit process. The audit process should be outlined including who will be involved in each step. Regular internal audits will help prevent improper payments
Reference AHIMA Practice Brief. “Understanding Governmental Audits(2013 Update)” Updated November 2013 http: //bok. ahima. org/doc? oid=302441#. XLff. K 6 Rry. M 8 CMS. gov. Original Medicare (fee-for-service) Appeals. https: //www. cms. gov/Medicare/Appeals-and. Grievances/Org. Med. FFSAppeals/Redeterminationbya. Medicare. Contractor. html
Reference CMS. gov. Provider Options- RAC Overpayment Determination. https: //www. cms. gov/Research-Statistics-Data-and-Systems/Monitoring. Programs/Medicare-FFS-Compliance-Programs/Recovery-Audit. Program/Downloads/Provider. Options. Chart_508 cleared_7 -28 -2017. pdf Performent. Region 1 Resources. https: //performantrac. com/region-1/