Medicare Part D The New Prescription Drug Benefit
Medicare Part D The New Prescription Drug Benefit and Implications for CARE Act Clients Mary Vienna Division of Training and Technical Assistance HIV/AIDS Bureau Health Resources and Services Administration Department of Health and Human Services 1
Medicare Part D and Ryan White Overview Ø The new Medicare benefit called Medicare Part D Ø How that will change care for our clients on Medicare Ø How it will impact grantees 2
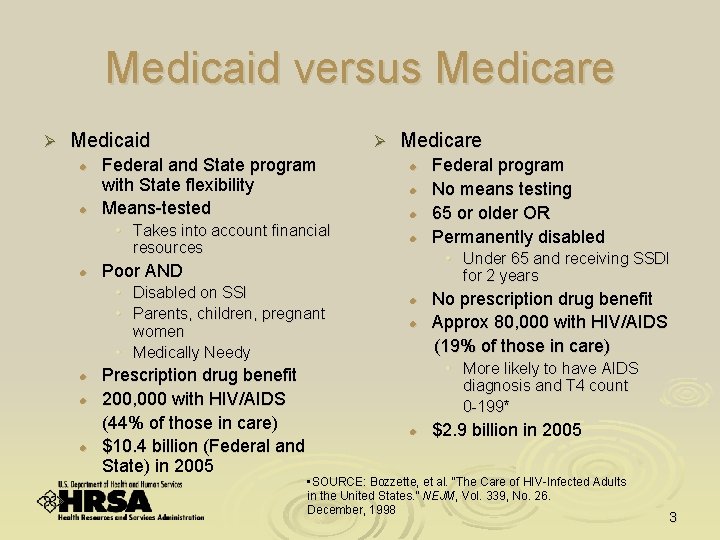
Medicaid versus Medicare Ø Medicaid l l Ø Federal and State program with State flexibility Means-tested • Takes into account financial resources l l l l Prescription drug benefit 200, 000 with HIV/AIDS (44% of those in care) $10. 4 billion (Federal and State) in 2005 Federal program No means testing 65 or older OR Permanently disabled • Under 65 and receiving SSDI for 2 years Poor AND • Disabled on SSI • Parents, children, pregnant women • Medically Needy l Medicare l l No prescription drug benefit Approx 80, 000 with HIV/AIDS (19% of those in care) • More likely to have AIDS diagnosis and T 4 count 0 -199* l $2. 9 billion in 2005 • SOURCE: Bozzette, et al. “The Care of HIV-Infected Adults in the United States. ” NEJM, Vol. 339, No. 26. December, 1998 3
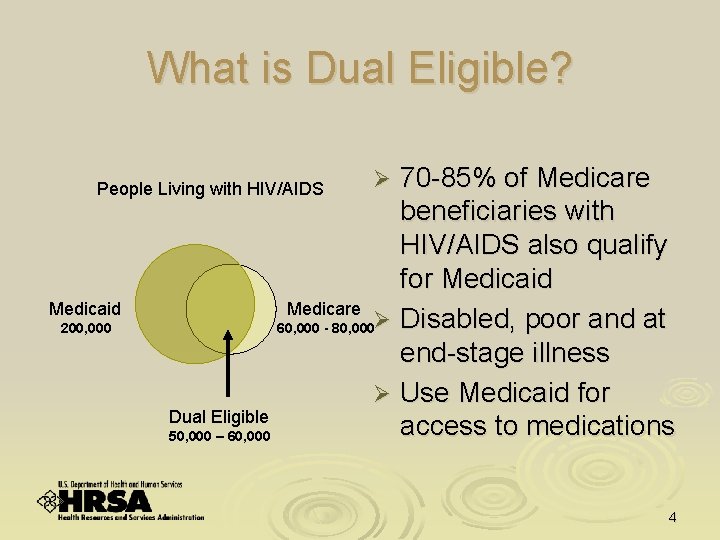
What is Dual Eligible? 70 -85% of Medicare beneficiaries with HIV/AIDS also qualify for Medicaid Medicare 60, 000 - 80, 000Ø Disabled, poor and at end-stage illness Ø Use Medicaid for Dual Eligible access to medications 50, 000 – 60, 000 People Living with HIV/AIDS Medicaid 200, 000 Ø 4
Medicare Modernization Act Ø Medicare Prescription Drug, Improvement and Modernization Act (MMA) of 2003 signed into law on December 8, 2003 Ø Biggest change to Medicare in 40 years Ø Adds a prescription drug benefit to Medicare called Medicare Part D Ø Benefit starts January 1, 2006 5
Basic Prescription Drug Benefit Ø Enrollment period from November 15, 2005 to May 15, 2006 l Medicare beneficiary chooses to enroll in Medicare Part D l Medicare beneficiary then chooses either: • A stand-alone prescription drug plan [PDP] for those in traditional fee-for -service (Part A and B) Medicare • A managed care plan (Medicare Advantage) that includes a prescription drug plan [MA-PD] for those in Part C Beneficiaries will have a choice of at least two prescription drug plans l Choices and plans will vary between regions Ø Plans have flexibility (subject to certain constraints) to establish varying features: l Levels of cost-sharing requirements and coverage limits other than “standard” coverage l Lists of drugs to include on their formulary, and on which tier l Cost management tools l 6
Basic Prescription Drug Benefit Generally, people are enrolled in a plan for a year. In special circumstances people can change plans. Dual eligibles can change plans at any time. Ø Expected premium in 2006 of $32. 20 per month but will vary by plan Ø Basic benefit will have deductibles, coinsurance and copays Ø People with limited resources will receive low-income subsidies (LIS) for these costs Ø l l Ø Most Medicare beneficiaries with HIV/AIDS will qualify for some type of LIS CMS pays subsidies directly to the plan All beneficiary costs and subsidy eligibility will be adjusted annually 7
Basic Prescription Drug Benefit Ø This benefit is different for Medicare l l Subsidies are means tested Benefit will vary by region Implementation requires coordination between CMS, the Social Security Administration and State Medicaid Agencies Many Medicare beneficiaries have other drug coverage--requires coordination (e. g. , retiree plans, VA, Tricare) 8
Medicare Part D and Dual Eligibles Ø As of January 1, 2006, Medicaid will no longer provide federal matching funds for Medicare beneficiaries’ prescription drug coverage Ø Dual eligibles will be switched to Medicare for drug coverage Ø Impact dependent on differences between previous State Medicaid plan and Medicare drug plans available in the area 9
Medicare Part D and Dual Eligibles Ø The switch from Medicaid to Medicare will take place on January 1, 2006 l No transitional period Ø To ensure continuity of drug coverage, CMS will auto-enroll all dual eligibles and notify them of their plan assignment in October Ø Dual eligibles can choose another plan at any time – no annual election period 10
Ensuring a Smoother Transition Ø Letter to State Medicaid Directors promising Federal matching funds for early refills and 30 -90 day prescriptions near the end of 2005 Ø PDPs must have a transition process for new enrollees, with outreach efforts and a transition timeframe to introduce formulary requirements 11
Standard Benefit: Beneficiary Cost Per Year (for 2006), Excluding LIS Expected monthly premium of $32. 20 $250 deductible 25% coinsurance from $251 to $2, 250* 100% coinsurance from $2, 251 to $5, 100 (coverage gap commonly referred to as the “donut hole”) Ø Catastrophic coverage level: co-pay of 5% or $2/$5 (whichever is greater) after total drug costs reach $5, 100 AND beneficiary has paid $3, 600 in true out-of-pocket costs (Tr. OOP) Ø Ø • Coinsurance is a term used in Medicare Part D that refers to the beneficiary’s contribution toward prescription drug costs until the catastrophic coverage limit has been reached 12
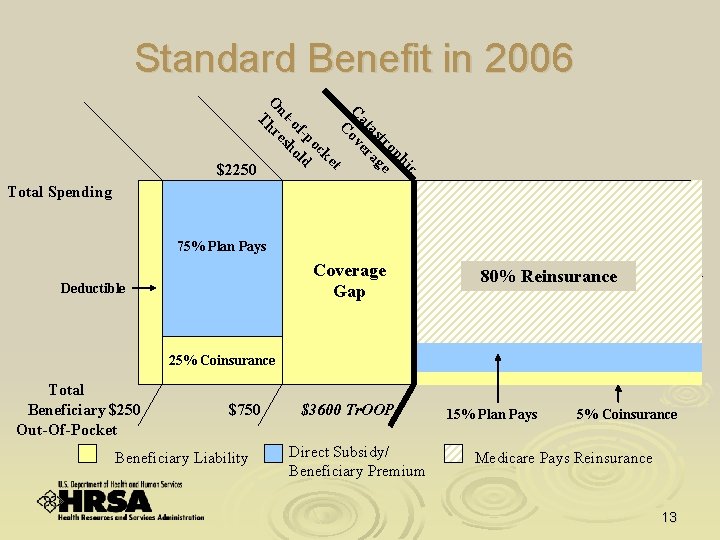
Standard Benefit in 2006 c hi op tr e as ag at er C ov C t ke oc f-p ld -o ho ut es O hr T $250 Total Spending $2250 $5100 75% Plan Pays Coverage Gap Deductible 80% Reinsurance $+ ≈ 95% 25% Coinsurance Total Beneficiary $250 Out-Of-Pocket $750 Beneficiary Liability $3600 Tr. OOP Direct Subsidy/ Beneficiary Premium 15% Plan Pays 5% Coinsurance Medicare Pays Reinsurance 13
Case Study: Peter Jones Ø Ø Ø 65 years old, HIV positive, aged into Medicare Income $1, 600 per month (200% FPL) Antiretroviral regimen is Efavirenz (Sustiva) + FTC/TDF (Truvada) Drugs cost $1, 300 per month Peter pays: l l l Ø $32. 20 per month in premiums Month 1: $250 deductible plus $262 (25% coinsurance) towards $1050 balance Month 2: $237 coinsurance (25% of $950 balance to reach $2250 co-insurance limit) plus $350 (100% coinsurance for balance of $1300 pharmacy cost) Month 3: $1, 300 prescription cost (100% coinsurance) [Peter has now paid $2, 399 out-of-pocket towards his drugs] Month 4: $1, 201 prescription cost (100% coinsurance for a total of $3, 600 in outof-pocket costs). Total drug costs are also $5, 200 (above the $5, 100 limit) so the catastrophic coverage level has been reached. Months 5 -12: $65 per month (5% co-pay) Peter pays $4, 506. 40 for the year [$386. 40 in premiums, $3600 out-ofpocket and $520 in co-pays] 14

Who Qualifies for a Low Income Subsidy (LIS)? Ø Medicare beneficiaries who are automatically qualified for a full subsidy (known as “deemed eligible”) are : l Dual eligible (receive full Medicaid benefits) • 70 -85% of Medicare beneficiaries living with HIV/AIDS l In a Medicare Savings Program • Qualified Medicare Beneficiary (QMB) • Specified Low-Income Medicare Beneficiary (SLMB) • Qualifying Individual (QI) l Ø Receiving SSI benefits Medicare will notify them May-June l Dual eligibles will be auto-enrolled in October and may choose a different plan 15

Who Qualifies for a Low Income Subsidy (LIS)? Ø Other Medicare beneficiaries who qualify for a full or partial subsidy, but not automatically, are: l l Single with an annual income below $14, 355 and resources less than $11, 500 in 2005* Married with a combined annual income below $19, 245 and resources less than $23, 000 in 2005* These individuals must apply to the Social Security Administration or Medicaid State Agency to qualify Ø SSA sending nearly 19 million letters and applications this summer. Can apply by mail, SSA’s 1 -800, online, or in person. Ø Medicaid State Agencies who qualify Medicare beneficiaries for LIS must also screen them for eligibility for Medicaid and Medicare Savings Programs Ø Medicare will enroll those who don’t choose a plan by May 15 Ø *Higher in Alaska, Hawaii and for certain reasons 16
LIS for Dual Eligibles Ø No premiums unless beneficiary chooses an above-average cost PDP l Ø Ø Then pay balance of premium cost No deductible or coinsurance Prescription co-pay • • Below 100% FPL: $1 generic/$3 brand drug co-pay Above 100% FPL: $2 generic/$5 brand drug co-pay No cost after total drug costs of $5, 100 and $3, 600 out-of-pocket limit is reached Ø Subsidy counts toward out-of-pocket costs Ø l What someone pays out-of-pocket + what Medicare pays as the extra help = $3, 600 17
Case Study: Jane Matthews Ø Ø Ø Ø On SSDI, Medicare and Medicaid (dual eligible) SSDI benefit $780/month (less than 100% FPL) Antiretroviral regimen is Sustiva + Truvada Drugs cost $1, 300 per month Jane pays $6 in co-pays per month for two scripts (income < 100% FPL so $3 brand name co-pay applies) for three months By 4 th month, total drug costs of $5, 200 exceeds $5, 100 catastrophic coverage level ($1, 300 x 4) No cost to Jane after that Jane pays $18 for the year [3 months of $6 co-pay] 18
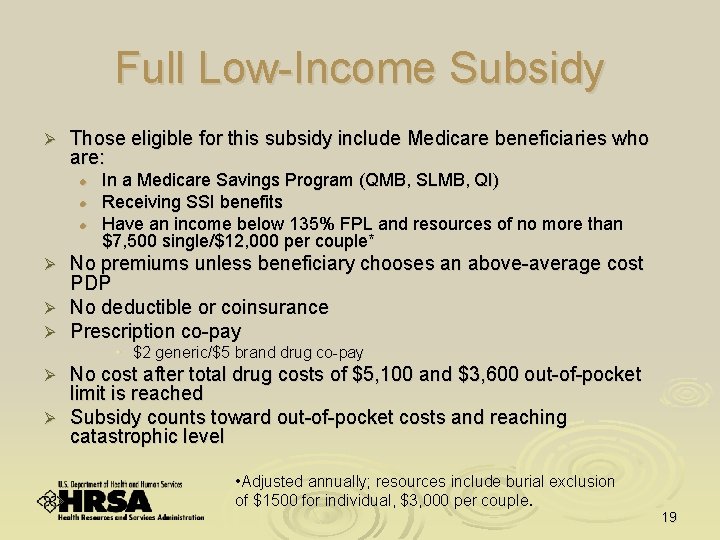
Full Low-Income Subsidy Ø Those eligible for this subsidy include Medicare beneficiaries who are: l l l In a Medicare Savings Program (QMB, SLMB, QI) Receiving SSI benefits Have an income below 135% FPL and resources of no more than $7, 500 single/$12, 000 per couple* No premiums unless beneficiary chooses an above-average cost PDP Ø No deductible or coinsurance Ø Prescription co-pay Ø • $2 generic/$5 brand drug co-pay No cost after total drug costs of $5, 100 and $3, 600 out-of-pocket limit is reached Ø Subsidy counts toward out-of-pocket costs and reaching catastrophic level Ø • Adjusted annually; resources include burial exclusion of $1500 for individual, $3, 000 per couple. 19
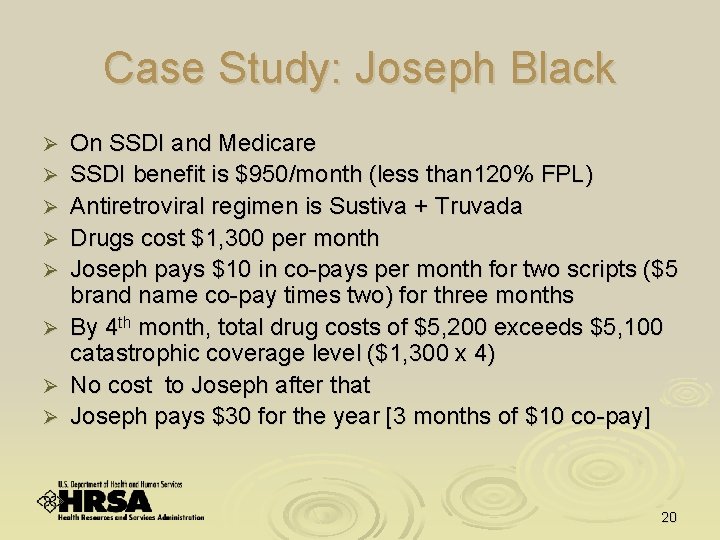
Case Study: Joseph Black Ø Ø Ø Ø On SSDI and Medicare SSDI benefit is $950/month (less than 120% FPL) Antiretroviral regimen is Sustiva + Truvada Drugs cost $1, 300 per month Joseph pays $10 in co-pays per month for two scripts ($5 brand name co-pay times two) for three months By 4 th month, total drug costs of $5, 200 exceeds $5, 100 catastrophic coverage level ($1, 300 x 4) No cost to Joseph after that Joseph pays $30 for the year [3 months of $10 co-pay] 20

Partial Low Income Subsidy (2006)* Ø Those eligible for this subsidy include Medicare beneficiaries who are: l Ø Benefit l l Ø Below 150% FPL and with resources of no more $11, 500 (individuals) and $23, 000 (couples) Sliding scale premium $50 deductible 15% coinsurance up to catastrophic coverage level $2 generic/$5 brand name drug co-pay after total drug costs of $5, 100 and $3, 600 out-of-pocket limit is reached Subsidy counts toward out-of-pocket costs and reaching catastrophic coverage level * Adjusted annually 21
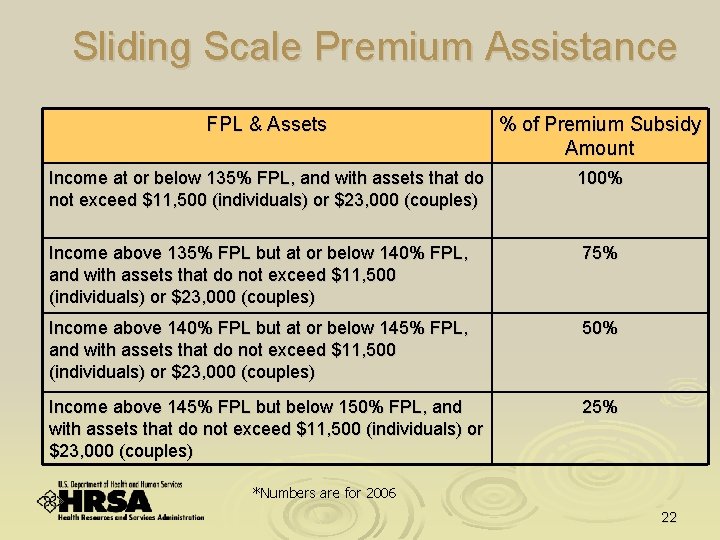
Sliding Scale Premium Assistance FPL & Assets % of Premium Subsidy Amount Income at or below 135% FPL, and with assets that do not exceed $11, 500 (individuals) or $23, 000 (couples) 100% Income above 135% FPL but at or below 140% FPL, and with assets that do not exceed $11, 500 (individuals) or $23, 000 (couples) 75% Income above 140% FPL but at or below 145% FPL, and with assets that do not exceed $11, 500 (individuals) or $23, 000 (couples) 50% Income above 145% FPL but below 150% FPL, and with assets that do not exceed $11, 500 (individuals) or $23, 000 (couples) 25% *Numbers are for 2006 22
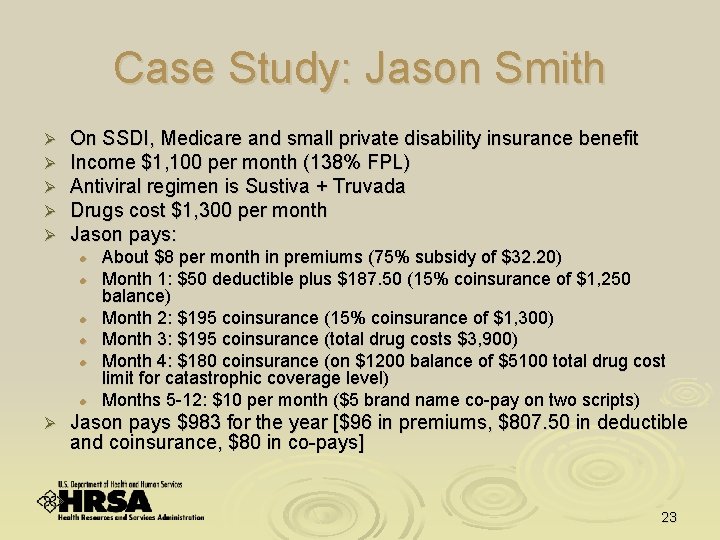
Case Study: Jason Smith Ø Ø Ø On SSDI, Medicare and small private disability insurance benefit Income $1, 100 per month (138% FPL) Antiviral regimen is Sustiva + Truvada Drugs cost $1, 300 per month Jason pays: l l l Ø About $8 per month in premiums (75% subsidy of $32. 20) Month 1: $50 deductible plus $187. 50 (15% coinsurance of $1, 250 balance) Month 2: $195 coinsurance (15% coinsurance of $1, 300) Month 3: $195 coinsurance (total drug costs $3, 900) Month 4: $180 coinsurance (on $1200 balance of $5100 total drug cost limit for catastrophic coverage level) Months 5 -12: $10 per month ($5 brand name co-pay on two scripts) Jason pays $983 for the year [$96 in premiums, $807. 50 in deductible and coinsurance, $80 in co-pays] 23
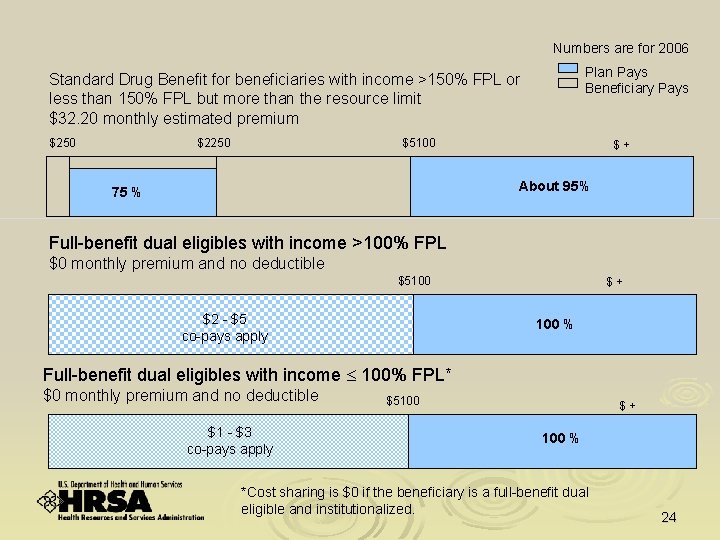
Numbers are for 2006 Plan Pays Beneficiary Pays Standard Drug Benefit for beneficiaries with income >150% FPL or less than 150% FPL but more than the resource limit $32. 20 monthly estimated premium $250 $2250 $5100 $+ About 95% 75 % Full-benefit dual eligibles with income >100% FPL $0 monthly premium and no deductible $5100 $2 - $5 co-pays apply $+ 100 % Full-benefit dual eligibles with income 100% FPL* $0 monthly premium and no deductible $1 - $3 co-pays apply $5100 $+ 100 % *Cost sharing is $0 if the beneficiary is a full-benefit dual eligible and institutionalized. 24
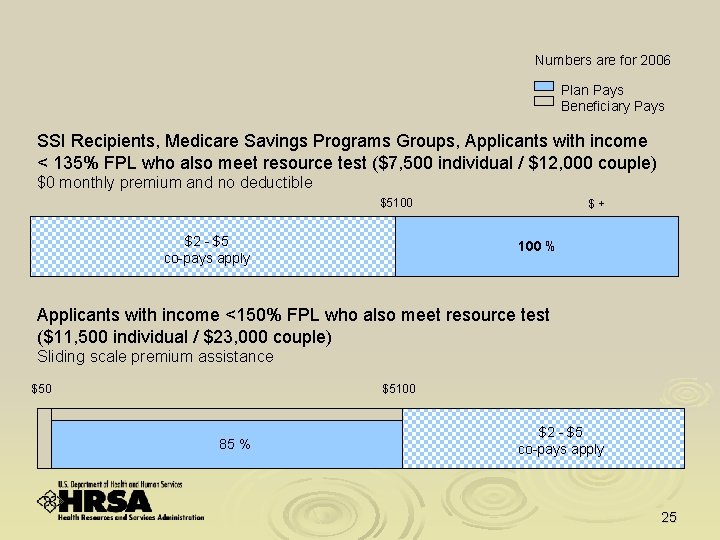
Numbers are for 2006 Plan Pays Beneficiary Pays SSI Recipients, Medicare Savings Programs Groups, Applicants with income < 135% FPL who also meet resource test ($7, 500 individual / $12, 000 couple) $0 monthly premium and no deductible $5100 $2 - $5 co-pays apply $+ 100 % Applicants with income <150% FPL who also meet resource test ($11, 500 individual / $23, 000 couple) Sliding scale premium assistance $50 $5100 85 % $2 - $5 co-pays apply 25
How to Apply for Help Ø The Social Security Administration (SSA) will mail applications to people who may qualify • Those who think they may qualify should • Complete the application form l Mail it to the address on the back of the form l Use the enclosed postage-paid envelope l Use original forms only l Do not photocopy the application l Photocopying the application could delay timely processing • Apply--even if they’re not sure they qualify 26
Other Ways to Apply for Extra Help Apply on the Social Security website at http: //www. socialsecurity. gov Ø Apply at a Social Security sponsored event Ø Apply by phone by calling Social Security at 1 -800 -772 -1213 Ø Apply at a State Medicaid Office Ø Apply at a community event that will offer opportunities to apply Ø State Health Insurance Program (SHIP) counselors will offer free personalized counseling starting in the fall of 2005 Ø 27
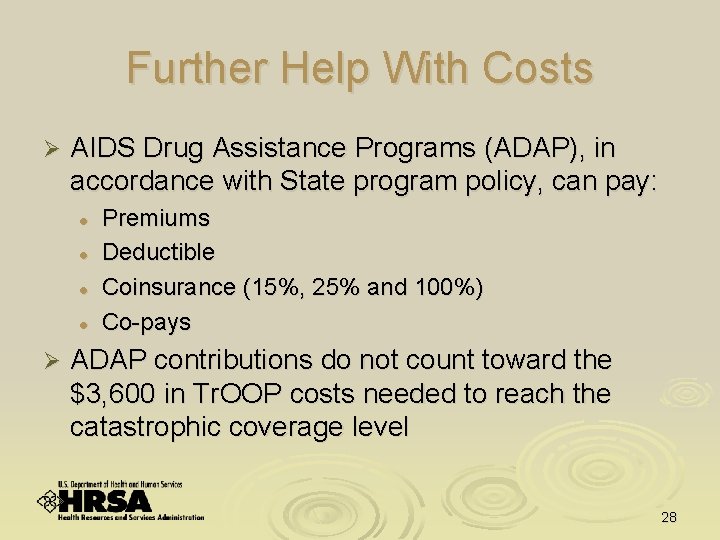
Further Help With Costs Ø AIDS Drug Assistance Programs (ADAP), in accordance with State program policy, can pay: l l Ø Premiums Deductible Coinsurance (15%, 25% and 100%) Co-pays ADAP contributions do not count toward the $3, 600 in Tr. OOP costs needed to reach the catastrophic coverage level 28
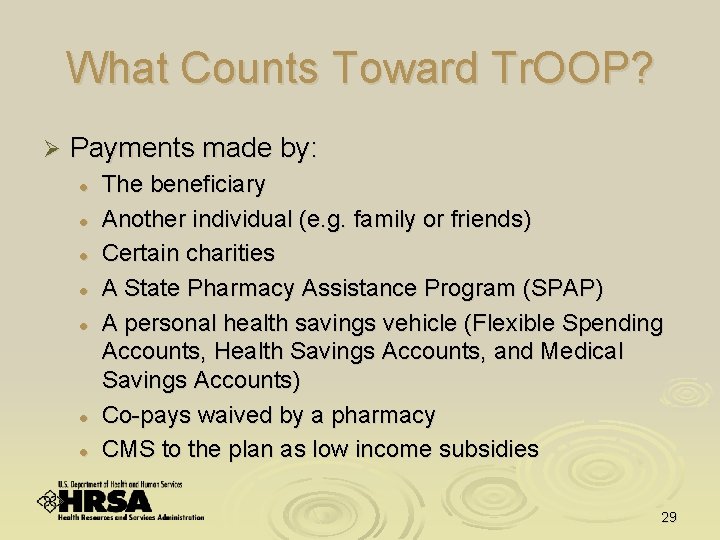
What Counts Toward Tr. OOP? Ø Payments made by: l l l l The beneficiary Another individual (e. g. family or friends) Certain charities A State Pharmacy Assistance Program (SPAP) A personal health savings vehicle (Flexible Spending Accounts, Health Savings Accounts, and Medical Savings Accounts) Co-pays waived by a pharmacy CMS to the plan as low income subsidies 29
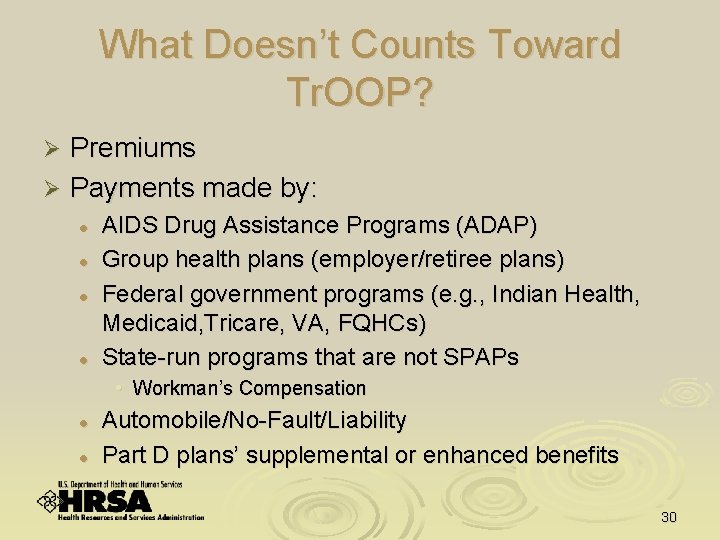
What Doesn’t Counts Toward Tr. OOP? Premiums Ø Payments made by: Ø l l AIDS Drug Assistance Programs (ADAP) Group health plans (employer/retiree plans) Federal government programs (e. g. , Indian Health, Medicaid, Tricare, VA, FQHCs) State-run programs that are not SPAPs • Workman’s Compensation l l Automobile/No-Fault/Liability Part D plans’ supplemental or enhanced benefits 30
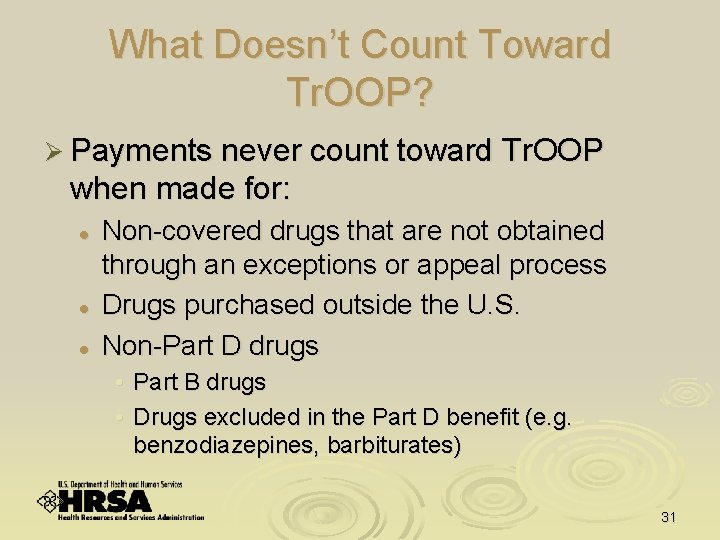
What Doesn’t Count Toward Tr. OOP? Ø Payments never count toward Tr. OOP when made for: l l l Non-covered drugs that are not obtained through an exceptions or appeal process Drugs purchased outside the U. S. Non-Part D drugs • Part B drugs • Drugs excluded in the Part D benefit (e. g. benzodiazepines, barbiturates) 31
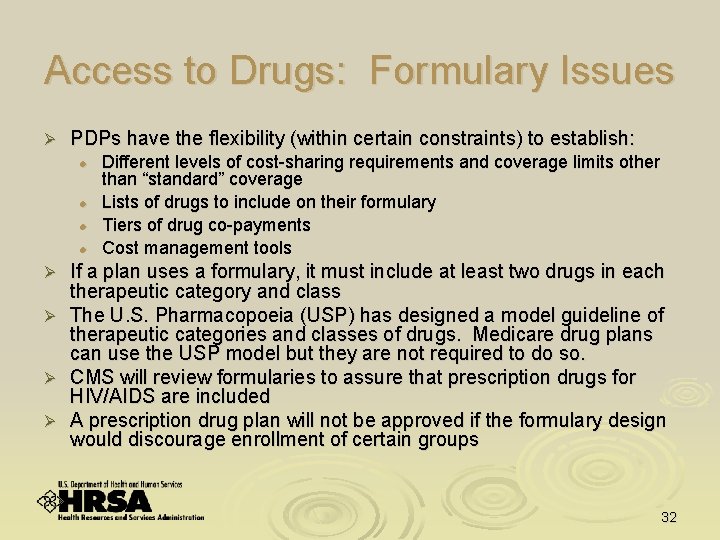
Access to Drugs: Formulary Issues Ø PDPs have the flexibility (within certain constraints) to establish: l l Ø Ø Different levels of cost-sharing requirements and coverage limits other than “standard” coverage Lists of drugs to include on their formulary Tiers of drug co-payments Cost management tools If a plan uses a formulary, it must include at least two drugs in each therapeutic category and class The U. S. Pharmacopoeia (USP) has designed a model guideline of therapeutic categories and classes of drugs. Medicare drug plans can use the USP model but they are not required to do so. CMS will review formularies to assure that prescription drugs for HIV/AIDS are included A prescription drug plan will not be approved if the formulary design would discourage enrollment of certain groups 32
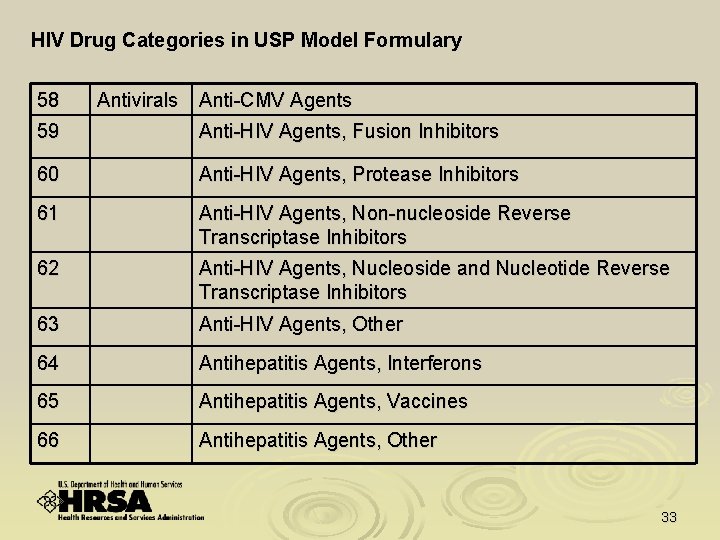
HIV Drug Categories in USP Model Formulary 58 Antivirals Anti-CMV Agents 59 Anti-HIV Agents, Fusion Inhibitors 60 Anti-HIV Agents, Protease Inhibitors 61 Anti-HIV Agents, Non-nucleoside Reverse Transcriptase Inhibitors 62 Anti-HIV Agents, Nucleoside and Nucleotide Reverse Transcriptase Inhibitors 63 Anti-HIV Agents, Other 64 Antihepatitis Agents, Interferons 65 Antihepatitis Agents, Vaccines 66 Antihepatitis Agents, Other 33
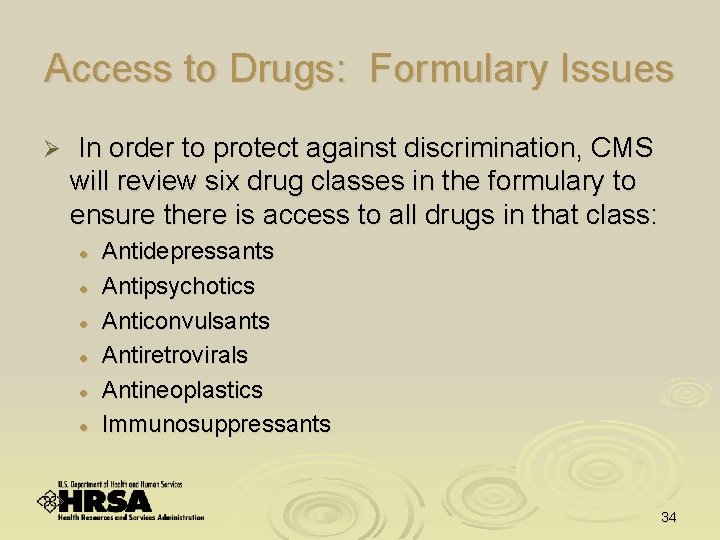
Access to Drugs: Formulary Issues Ø In order to protect against discrimination, CMS will review six drug classes in the formulary to ensure there is access to all drugs in that class: l l l Antidepressants Antipsychotics Anticonvulsants Antiretrovirals Antineoplastics Immunosuppressants 34
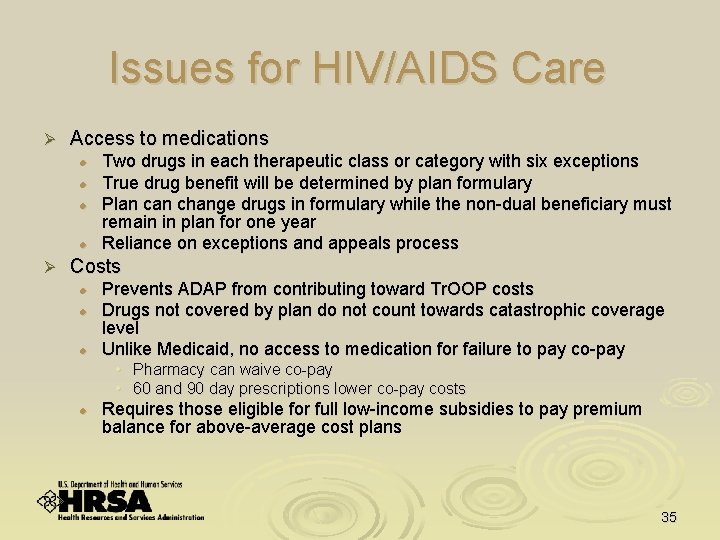
Issues for HIV/AIDS Care Ø Access to medications l l Ø Two drugs in each therapeutic class or category with six exceptions True drug benefit will be determined by plan formulary Plan change drugs in formulary while the non-dual beneficiary must remain in plan for one year Reliance on exceptions and appeals process Costs l l l Prevents ADAP from contributing toward Tr. OOP costs Drugs not covered by plan do not count towards catastrophic coverage level Unlike Medicaid, no access to medication for failure to pay co-pay • Pharmacy can waive co-pay • 60 and 90 day prescriptions lower co-pay costs l Requires those eligible for full low-income subsidies to pay premium balance for above-average cost plans 35
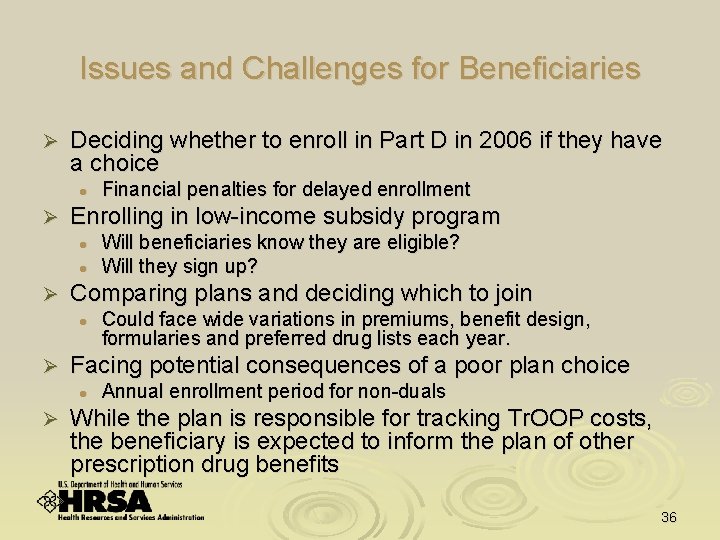
Issues and Challenges for Beneficiaries Ø Deciding whether to enroll in Part D in 2006 if they have a choice l Ø Enrolling in low-income subsidy program l l Ø Could face wide variations in premiums, benefit design, formularies and preferred drug lists each year. Facing potential consequences of a poor plan choice l Ø Will beneficiaries know they are eligible? Will they sign up? Comparing plans and deciding which to join l Ø Financial penalties for delayed enrollment Annual enrollment period for non-duals While the plan is responsible for tracking Tr. OOP costs, the beneficiary is expected to inform the plan of other prescription drug benefits 36
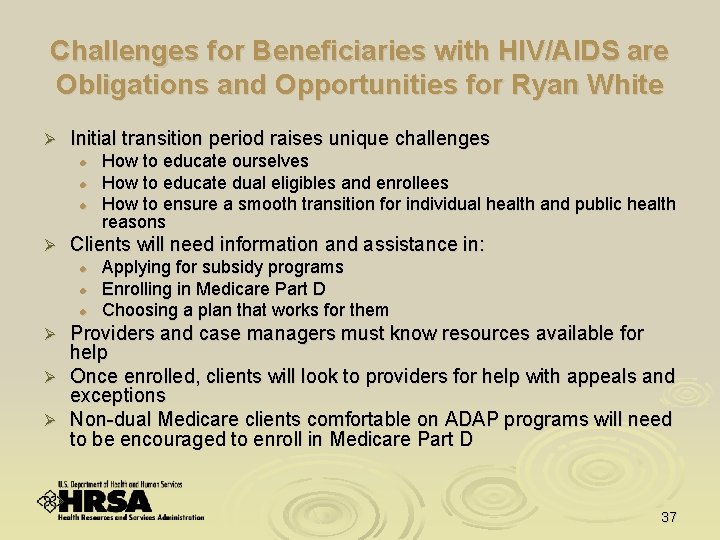
Challenges for Beneficiaries with HIV/AIDS are Obligations and Opportunities for Ryan White Ø Initial transition period raises unique challenges l l l Ø How to educate ourselves How to educate dual eligibles and enrollees How to ensure a smooth transition for individual health and public health reasons Clients will need information and assistance in: l l l Applying for subsidy programs Enrolling in Medicare Part D Choosing a plan that works for them Providers and case managers must know resources available for help Ø Once enrolled, clients will look to providers for help with appeals and exceptions Ø Non-dual Medicare clients comfortable on ADAP programs will need to be encouraged to enroll in Medicare Part D Ø 37
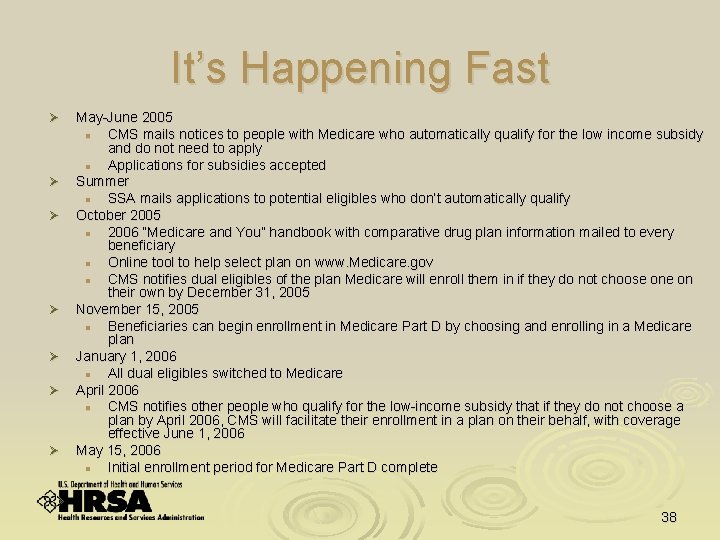
It’s Happening Fast Ø Ø Ø Ø May-June 2005 l CMS mails notices to people with Medicare who automatically qualify for the low income subsidy and do not need to apply l Applications for subsidies accepted Summer l SSA mails applications to potential eligibles who don’t automatically qualify October 2005 l 2006 “Medicare and You” handbook with comparative drug plan information mailed to every beneficiary l Online tool to help select plan on www. Medicare. gov l CMS notifies dual eligibles of the plan Medicare will enroll them in if they do not choose on their own by December 31, 2005 November 15, 2005 l Beneficiaries can begin enrollment in Medicare Part D by choosing and enrolling in a Medicare plan January 1, 2006 l All dual eligibles switched to Medicare April 2006 l CMS notifies other people who qualify for the low-income subsidy that if they do not choose a plan by April 2006, CMS will facilitate their enrollment in a plan on their behalf, with coverage effective June 1, 2006 May 15, 2006 l Initial enrollment period for Medicare Part D complete 38
What’s HAB Doing? Ø HAB Medicare Workgroup l Expertise and resource to programs and project officers on Medicare Part D Ø Technical assistance and outreach plan Ø Venues to reach grantees Ø HAB project officer training Ø HAB website information Ø Qs & As 39
Who Do I Go To For Answers? l l l l HAB Project Officers CMS Regional Office Medicaid State Agency Social Security Administration State Health Insurance Program State ADAP Title I and II programs HIV and Professional Organizations 40
Website Resources Ø http: //hab. hrsa. gov/specialprojects. htm l l l Ø http: //www. cms. hhs. gov/medicarereform/pdbma l Ø Information about Medicare Part D http: //www. cms. hhs. gov/medicarereform/AIDS. pdf l Ø Medicare Part D webpage Qs & As http: //www. hrsa. gov/medicare/HIV/qa. htm Links Medicare HIV/AIDS Fact Sheet http: //www. medicare. gov l l Click on “Learn About Your Medicare Prescription Coverage Options” Information for Medicare beneficiaries 41
- Slides: 41