Medicare Part D Basic Training Part D Medicare
Medicare Part D Basic Training Part D Medicare prescription drug coverage Last Revised January 2021 GWAAR, Inc.
Medicare Part D Medicare’s Prescription Drug Program § Must be enrolled in Part A or Part B. Part D Medicare prescription drug coverage § Covers prescription medications. § Run by private companies that contract with Medicare. § Part D Plans are provided through: § Stand Alone Medicare Prescription Drug Plans (PDPs)—only covers prescriptions. § Medicare Advantage Prescription Drug Plans (MA-PDs)—health and drug coverage combined. § To receive Part D coverage, you must enroll in a Part D Plan. § Must live in the service area (county) of the Part D Plan. § Plan details change annually—Need to review plan every year! § “Voluntary”—But, if don’t enroll, late enrollment penalty may apply. § Compare plans and enroll on Medicare’s Plan Finder.
Medicare Part D Medicare’s Prescription Drug Program § All plans follow basic cost-sharing structures and include a certain level of coverage as required by Medicare. Part D Medicare prescription drug coverage § A “formulary” is a list of covered prescription drugs. § In 2021 there are 31 Part D plan options in Wisconsin. § Plans change their details each year: § Formulary § Costs § Utilization management tools § Best way to select a plan is to use Medicare’s official plan comparison tool known as the Plan Finder. (“Run a Plan. Finder. ”)
Medicare Part D Enrollment Opportunities § Initial Enrollment Period Part D Medicare prescription drug coverage § 3 months prior, month of, and 3 months after starting Medicare. § Annual Open Enrollment Period § Enroll October 15 - December 7 each year for coverage starting January 1 st. § Medicare Advantage Open Enrollment Period § January 1 – March 31—only for people already enrolled in MA plan. § Special Enrollment Period § In certain circumstances, you may be able to change your Medicare prescription drug coverage outside of the other enrollment periods.
Medicare Part D Initial Enrollment Period Part D Medicare prescription drug coverage § 7 -Month initial enrollment period— 3 months prior to eligibility, the month of eligibility (age 65 or 25 th SSDI payment month) and 3 months after. § If a person receives SSDI retroactively, then the person will receive a special enrollment period. § Once a person makes an election (enrolls in a plan) during the initial enrollment period, then the enrollment period ends.
Medicare Part D Annual Open Enrollment Period § Also called open enrollment period (OEP): October 15 – December 7. Part D Medicare prescription drug coverage § Every person with Part D should check his or her plan during this time. § During this period a person can: § § § Enroll in new prescription drug plan (PDP) Switch to a new PDP Switch from one Medicare Advantage Plan w/ drug coverage (MAPD) to another MAPD. If on a MAPD, move back to Original Medicare and a standalone PDP. Disenroll in PDP if, for example, enrollment in Senior. Care is an option. Ensure current plan is continuing into new year. § Even if a beneficiary prefers to stay in current plan, they should review their plan, note any changes and ensure it still provides cost-effective coverage for their current medications.
Medicare Part D Medicare Advantage Open Enrollment Period Part D Medicare prescription drug coverage § MA OEP: January 1 – March 31 § Only for people who are already enrolled in a Medicare Advantage plan. § During this period a person can: § Switch from one Medicare Advantage Plan to another Medicare Advantage Plan. § Drop current Medicare Advantage Plan and move back to Original Medicare and a stand-alone PDP.
Medicare Part D Special Enrollment Periods (SEPs) Part D Medicare prescription drug coverage Additional SEPs can be found online. Discuss with your program attorney. § Provides the beneficiary the ability to make one election, or choice, within a period of time not available to the general public. § Can be disenrollment or enrollment. § Typically, enrolling in a new plan automatically disenrolls a beneficiary from previous plan. (Some exceptions apply. ) § Common SEPs: § § § § Low-Income Subsidy (LIS) Eligibility Change in residence (move) Enter or exit long-term care facility Enrollment in State Pharmaceutical Assistance Program (SPAP)* Plan Termination/non-renewal Loss of LIS at end of year Other SEPs that coordinate with Medicare Advantage (Part C) enrollment periods 5 star plan
Medicare Part D – Costs Premiums, Deductibles, and Copays or Coinsurance § Costs vary by plan and change annually. § 2021 premiums range from $ 7. 30 to $ 132. 30 per month. § 2021 National base beneficiary premium is $33. 06 Part D Medicare prescription drug coverage § 2021 Limit for a Deductible is $445 (Not all plans have a deductible. ) § Copays and coinsurance may vary per drug, per plan, per pharmacy. Income Related Monthly Adjustment Amount (IRMAA) § People with Part D who have higher incomes will pay an additional amount on top of their premium. Income Thresholds: § Individuals: $88, 000 § Couples filing jointly: $176, 000 § This amount is based on their tax filing from two years prior (ie, 2021 amount is based on 2019 tax filing. ) Only about 5% of all Medicare beneficiaries are subject to IRMAA.
Medicare Part D – Costs Late Enrollment Penalty § A late-enrollment penalty applies for those who did not enroll in Part D during the IEP and did not have other creditable coverage. Part D Medicare prescription drug coverage § The penalty is 1% of the national base beneficiary premium for every month you delayed enrollment. 2021 base premium = $33. 06 § The penalty will be added to your monthly premium if and when you enroll in a Part D plan, and it will continue as long as you are enrolled. § A person receiving a low-income subsidy will not have a penalty. A person will incur a penalty if all of following are true: § § It has been 63 or more days since initial enrollment period ended or since person was last enrolled in a Part D plan and… Person was eligible for Part D, but did not enroll in Part D, Person did not enroll in other creditable coverage, and Person does not qualify under any penalty exceptions.
Medicare Part D – Costs Calculating late-enrollment penalty—Example Part D Medicare prescription drug coverage Mrs. Martinez was without creditable prescription drug coverage from June 2017 –December 2019, a period of 31 months. Her penalty is 31% (1% for each of the 31 months) of $33. 06 (the national base beneficiary premium for 2021) or $10. 25. Since the monthly penalty is always rounded to the nearest $0. 10, she will pay $10. 30 each month in addition to her plan’s monthly premium. Here’s the Math: 0. 31 (31% penalty) x $33. 06 (2021 base premium) = $10. 25 rounded to the nearest $0. 10 = $10. 30 = Mrs. Martinez’s monthly late enrollment penalty for 2021. For assistance with LEP calculations check with your program attorney.
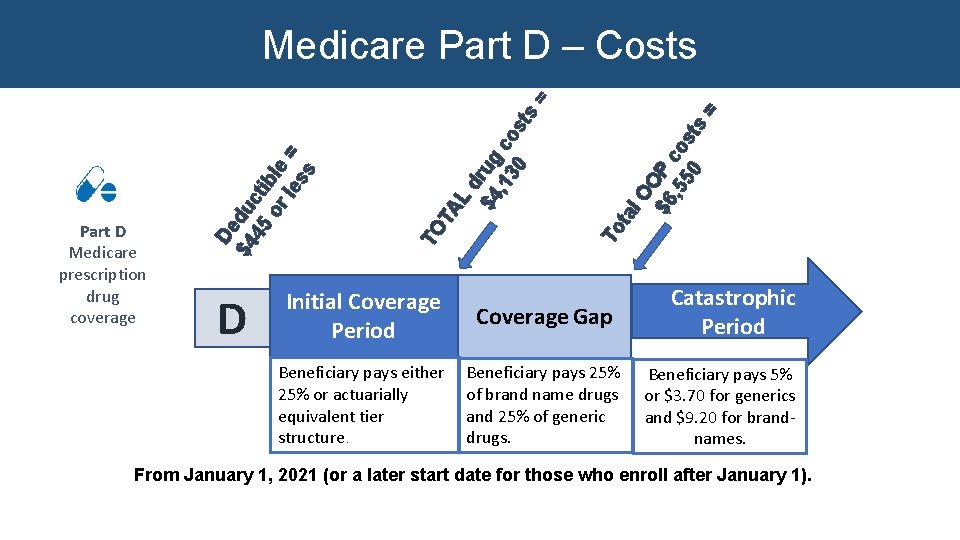
D s l. O O $6 P , 5 co 50 st ta To TA L dr $4 ug , 1 co 30 s TO Part D Medicare prescription drug coverage De $4 du 45 cti or ble le = ss ts = = Medicare Part D – Costs Initial Coverage Period Coverage Gap Beneficiary pays either 25% or actuarially equivalent tier structure. Beneficiary pays 25% of brand name drugs and 25% of generic drugs. Catastrophic Period Beneficiary pays 5% or $3. 70 for generics and $9. 20 for brandnames. From January 1, 2021 (or a later start date for those who enroll after January 1).
Medicare Part D What is Covered § Prescribed medications. Part D Medicare prescription drug coverage § Medications that are included in a plan’s formulary (Not all medications are covered by all plans. ) § The law excludes certain medications from coverage under Part D. § Medications must be for medically prescribed use. Drugs prescribed for off- label use are not covered. § Insulin and needles and syringes for the administration of insulin. If a client’s drug is not on a formulary, you may have to help your client request a formulary exception.
Medicare Part D What Is Not Covered? § § § § § Medications not on a plan’s formulary are usually not covered. Non-prescription, over-the-counter drugs Drugs that are not approved by the Federal Drug Administration (FDA) Prescription vitamins Drugs for relief of cough or cold Drugs for fertility, weight loss or erectile dysfunction Drugs for cosmetic purposes Drugs covered by Hospice (Covered by Part A) Drugs covered by Part B (certain injections, oral anti-cancer, and oral anti-rejection meds)
Medicare Part D Enhanced Coverage § Enhanced plans can offer coverage that INCLUDES: Part D Medicare prescription drug coverage § Part D-excluded drugs; § Vitamins or; § other benefits not part of Medicare Part D drug benefit. § Costs associated with enhanced benefits do NOT count toward Part D out-of-pocket cost-sharing, which is used to determine when a beneficiary meets his or her deductible, coverage gap and catastrophic coverage. § Enhanced plans do NOT always offer a more complete formulary, and are not always the most economical choice for clients.
Medicare Part D Utilization Management Tools § Prior Authorization. Plan will require a prior authorization before plan covers certain Part D Medicare prescription drug coverage medications. Notification of coverage will come through coverage determination. § Quantity Limits. A coverage determination is required if beneficiary requests an amount above the most common dosage level. Certain medications prescribed by a physician can exceed the most common dosage, but the plan will still require approval of the quantity. § Step Therapy. Plan may require evidence that a beneficiary has tried other medications before the plan will pay for name-brand drugs. A coverage determination is needed. § Medication Therapy Management. Designed to ensure beneficiaries with complex needs understand their medications and usage, possible adverse effects and drug interactions. Part D plans must offer annual comprehensive medication review to all eligible people as part of MTM. People can opt out of MTM. Plan. Finder has information on each plan’s MTM eligibility criteria.
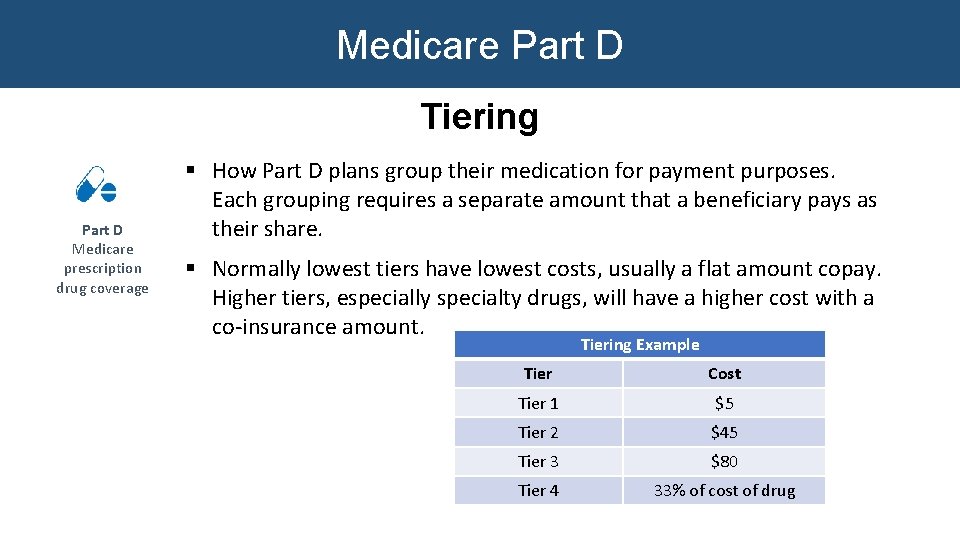
Medicare Part D Tiering Part D Medicare prescription drug coverage § How Part D plans group their medication for payment purposes. Each grouping requires a separate amount that a beneficiary pays as their share. § Normally lowest tiers have lowest costs, usually a flat amount copay. Higher tiers, especially specialty drugs, will have a higher cost with a co-insurance amount. Tiering Example Tier Cost Tier 1 $5 Tier 2 $45 Tier 3 $80 Tier 4 33% of cost of drug
Medicare Part D Low-Income Subsidy (LIS) / Extra Help Part D Medicare prescription drug coverage § A subsidy provided by the Federal government to the Part D plan that an eligible person is enrolled in. § Provides assistance with premium, deductible and copay costs. § People with LIS receive a Special Enrollment Period 1 x/calendar quarter during first 9 months of year. See Nutshell for eligibility requirements. § Three groups of people are eligible: § Those who applied for and are eligible for “Extra Help” through Social Security § Those who are “dual eligibles” § Those who are enrolled in a Medicare Savings Program (QMB, SLMB+)
Medicare Part D Low-Income Subsidy (LIS) / Extra Help Part D Medicare prescription drug coverage § Those who begin Medicare with a LIS or who have Medicare but not a Part D plan when they receive LIS will be randomly assigned a plan. This random plan can be declined, and a person can choose his/her own plan. § Those who have a Medicare Part D plan or a Medicare Advantage plan w/ drug coverage* when they become eligible for LIS will stay in their current plan with some premium and cost-sharing relief unless those people choose a new lowcost plan. § The date that a plan takes affect related to LIS can be hard to determine and changes depending on each client’s circumstances. Just like those without a low -income subsidy, those with LIS should use the Plan finder to determine the best plan options.
Medicare Part D When to Review a Part D Plan Part D Medicare prescription drug coverage § By September 30 th of each year, Part D/Medicare Advantage plan members will receive an Annual Notice of Change (ANOC) letter, which explains the changes to the plan. (May be sent electronically now. ) § Beneficiaries should review these letters carefully, as a plan could retain its name but change the costs, formularies and/or other plan details. § Plans can and will change, so every beneficiary should do a plan comparison annually to ensure his or her current plan is the best option.
Medicare Part D How to Select a Plan Part D Medicare prescription drug coverage § Plan Finder on Medicare. gov –Most effective way to choose a plan § 1 -800 -Medicare—good resource for those without a computer § Medigap Helpline: 1 -800 -242 -1060 § Medigap Precription Drug Helpline: 1 -855 -677 -2783
The Medicare Plan Finder § Compare plans based on star ratings, formularies, benefits, costs, and more. § Personalized search § Login to My. Medicare Account § Review/confirm med list § Anonymous search § Enter each prescription drug

The Medicare Plan Finder Access the Plan Finder Here. October 2018 Welcome to Medicare Presentation 23

The Medicare Plan Finder Option for personal search with beneficiary’s My. Medicare login information OR Anonymous Search
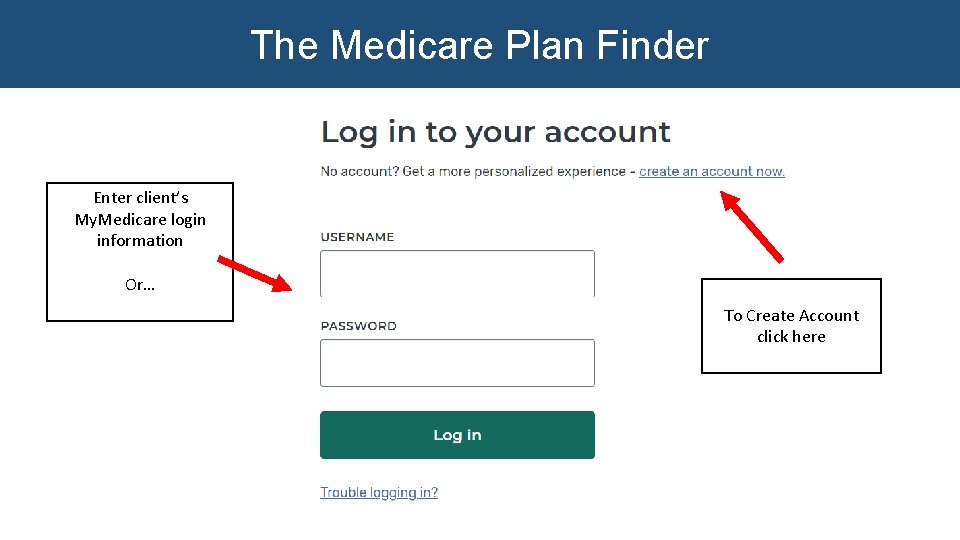
The Medicare Plan Finder Enter client’s My. Medicare login information Or… To Create Account click here
The Medicare Plan Finder IMPORTANT TO NOTE: § Search results default setting—lowest drug + premium cost § Can compare up to 5 pharmacies instead of 3 § Option for 6 and 12 month prescription refill § CMS adding footnote when PF does not have current pricing estimate for the drug and default pricing is used. § Adding a filter option for “Senior Savings Model”. Part D plans can offer lower drug pricing for people with Diabetes. Lower cost of insulin.
The Medicare Plan Finder Additional Resources for Consumer Education § Guide to Using the Medicare Plan Finder—Word Document § How to Create a My. Medicare Account § PPT and Video § Video Demonstration—How to use the Medicare Plan Finder (Coming Soon!) § Post link on your website § Email link to consumers
The Medicare Plan Finder Demonstration
Other Creditable Coverage Forms of Other Creditable Coverage for Part D (not Part B) § § Veterans drug coverage Senior. Care Some types of Employer Coverage (must ask) Some Marketplace policies “Creditable Coverage”: Other prescription drug coverage that is expected to pay, on average, at least as much as Medicare’s standard Part D coverage.
Senior. Care Wisconsin’s Prescription Drug Assistance Program § Available to Wisconsin residents age 65 and over who are U. S. citizens or have qualifying immigrant status. § $30 annual application fee. (No monthly premium. ) § No asset limit. § Creditable coverage. For more information or to access an § Annual income determines the level of coverage. § § § No deductible at Level 1. Level 2 a and 2 b have a deductible. Level 3 has a deductible and spenddown. § May use alone or in addition to Part D. application online: www. dhs. Wisconsin. gov/seniorcare Or call: 1 -800 -657 -2038
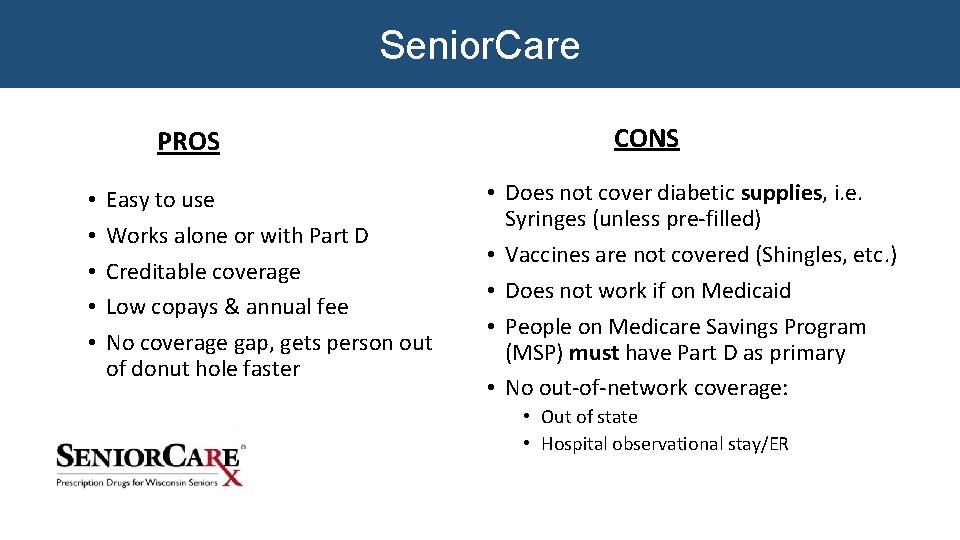
Senior. Care PROS • • • Easy to use Works alone or with Part D Creditable coverage Low copays & annual fee No coverage gap, gets person out of donut hole faster CONS • Does not cover diabetic supplies, i. e. Syringes (unless pre-filled) • Vaccines are not covered (Shingles, etc. ) • Does not work if on Medicaid • People on Medicare Savings Program (MSP) must have Part D as primary • No out-of-network coverage: • Out of state • Hospital observational stay/ER
Thank You! Debbie Bisswurm Medicare Outreach Coordinator, GWAAR Debbie. bisswurm@gwaar. org 608 -228 -8098
- Slides: 32