Medicare Dual Eligibles This Module Will Explain Why
Medicare Dual Eligibles
This Module Will Explain: • • Why a Dual-eligible Special Needs Plan (D-SNP)? Definitions Special Needs Plans Meridian. Care D-SNP Plan Medicare Savings Programs Low Income Subsidy MMP Information
Why Enroll Someone Into a D -SNP? • Beneficiaries enrolled in a D-SNP can receive enhanced benefits compared to Original Medicare or regular Medicaid – Example; vision, dental, hearing and OTC benefits • Beneficiaries can enroll year-round; not limited to Annual Enrollment Period • Coordination of care that is not offered through Original Medicare
CMS Data Seniors & Medicare and Medicaid Enrollees Medicaid provides health coverage to more than 7 million lowincome seniors who are also enrolled in Medicare. Medicaid also provides coverage to 4. 8 million people with disabilities who are enrolled in Medicare. In total, 12 million people are "dually eligible" and enrolled in both Medicaid and Medicare, composing more than 15% of all Medicaid enrollees. Source: https: //www. medicaid. gov/medicaid/eligibility/medicaid-enrollees

Definitions
Medicare and Medicaid • Medicare: Health insurance for people age 65 or older, certain people under 65 with disabilities, and people of any age with End Stage Renal Disease (ESRD) • Medicaid: Funded by Federal and State governments to pay for medical costs for certain individuals and families with low incomes and, in some cases, limited resources
Medicare • Medicare : Beneficiaries can obtain their coverage by receiving Part A and Part B services through Original Medicare. To obtain Part D coverage they must join a stand-alone Prescription Drug Plan; or receive Part A and Part B services from a Medicare Advantage Plan. Most MA plans include Part D coverage.
Medicaid • Medicaid: Within broad national guidelines established by Federal statutes, each state: – – Establishes its own eligibility standards Determines the type, amount, duration and scope of services Sets the rate of payment for services Administers its own program
Medicaid Coverage for Medicare Enrollees What Medicaid Covers for Medicare Enrollees • Part A: Pays for hospitalization costs • Part B: Pays for physician services, lab and x-ray services, DME, outpatient & other services • Part C: Medicare Advantage Plan offered by private companies approved by Medicare • Part D: Assists with the cost of prescription drugs

Special Needs Plans

What is a Special Needs Plan? • A Special Needs Plan (SNP) is a Medicare Advantage (MA) coordinated care plan (CCP) designed to provide targeted care and services to individuals with unique needs. • "Special needs individuals" have been defined as: – I-SNP: Institutionalized beneficiaries (nursing home, etc) – C-SNP: Individuals with severe or disabling chronic conditions, as specified by the Centers for Medicare and Medicaid Services – D-SNP: Medicare-Medicaid enrollees
SNP Enrollment • SNPs may only enroll individuals who meet the plan’s specific eligibility criteria and enrollment requirements. • All SNPs are required to verify the applicant’s special needs status. SNPs must include elements on the enrollment application (online, paper, etc. ) that correspond to the special needs focus of the particular SNP. – If someone is applying for a D-SNP they must provide their Medicaid number on the application, to be validated by the Plan.
Dual Eligible Special Needs Plan • “Dual eligible” is a term used to encompass all Medicare beneficiaries who also receive Medicaid assistance, ranging from full Medicaid benefits, to assistance only with Medicare premiums or cost sharing. Dual eligible coverage is dependent on beneficiaries’ income and asset thresholds. • Dual Eligible Special Needs Plans (D-SNPs) enroll beneficiaries who are entitled to both Medicare and Medicaid and offer the opportunity of enhanced benefits by combining those available through Medicare and Medicaid.
Medicare – Medicaid Coordination • Medicare pays first for Medicare covered services; Medicaid is generally the payer of last resort. • Medicaid may cover costs not covered or partially covered by Medicare, such as: – Nursing home care, personal care, home-and communitybased services, durable medical equipment • The options for a dual eligible to receive their Medicare and Medicaid benefits varies by state (managed care, fee-for-service, etc. )
D-SNP Enrollment • D-SNP beneficiaries qualify for special enrollment periods (SEPs) and are able to enroll and/or switch plans at the start of every month. – Example: Mary has just qualified for Medicaid and is now considered a “dual-eligible” beneficiary. Her Special Election Period begins once she qualifies for Medicaid, and continues as long as she receives Medicaid benefits. Therefore, she is able to enroll in a different D-SNP plan every month if she so chooses.

Medicare Savings Programs (MSP)
Medicare Savings Programs (MSP) • Medicare Savings Programs provide help from Medicaid to pay Medicare costs, including premiums, deductibles, and co-insurance – Often have higher income and resource guidelines than full Medicaid • MSP Categories: – – Qualified Medicare Beneficiaries (QMB) Specified Low-income Medicare Beneficiaries (SLMB) Qualifying Individuals (QI) Qualified Disabled Working Individuals (QDWI)
Medicare Savings Programs (MSP) • Persons eligible for an MSP such as QMBs or SLMBs and also eligible for full Medicaid benefits under another eligibility category – QMB Plus (means “plus” Medicaid) – SLMB Plus (means “plus” Medicaid) • People with Medicaid who also have Medicare but do not qualify for an MSP – Full Benefit Dual Eligibles (FBDE)
Medicare Savings Programs (MSP) • QMB only – Eligible for Medicaid payment of all Medicare premiums, deductibles, coinsurance and co-payments only, regardless of whether or not the services are included in the State Plan • QMB Plus – Eligible for Medicaid payment of all Medicare premiums, deductibles, coinsurance and co-payments, regardless of whether or not the services are included in the State Plan – Also eligible to receive all Medicaid state plan services
Medicare Savings Programs (MSP) • SLMB only – Receive Medicaid payment of Medicare Part B premiums only • SLMB Plus – Receive Medicaid payment of Medicare Part B premiums – Also eligible to receive all Medicaid state plan services – States may pay Medicare cost-sharing for all Medicare services or Medicaid state plan services only, as the state chooses

Dual Eligible Medicaid Programs 2019 Federal Poverty Level = $12, 490 • Full Medicaid = Determined by State • QMB and QMB Plus; less than or equal to 100% FPL • SLMB and SLMB Plus; greater than 100% FPL but less than 120% FPL • QI; greater than or equal to 120% FPL but less than 135% FPL • QDWI; less than or equal to 200% FPL
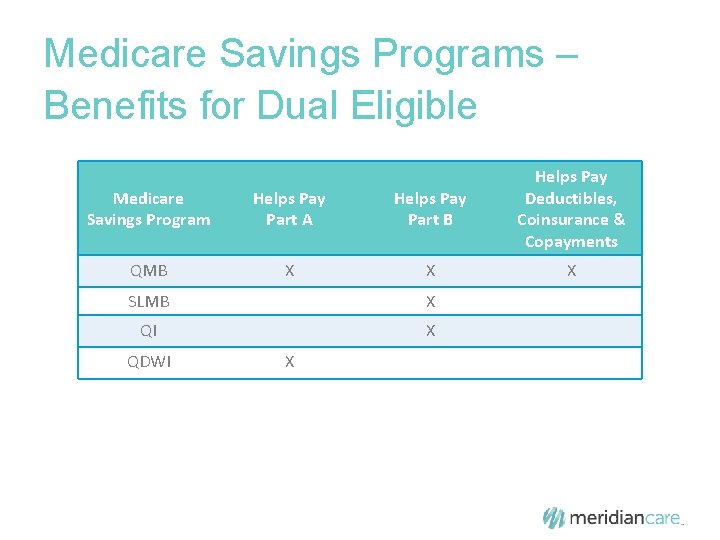
Medicare Savings Programs – Benefits for Dual Eligible Medicare Savings Program Helps Pay Part A Helps Pay Part B Helps Pay Deductibles, Coinsurance & Copayments QMB X X X SLMB X QI X QDWI X
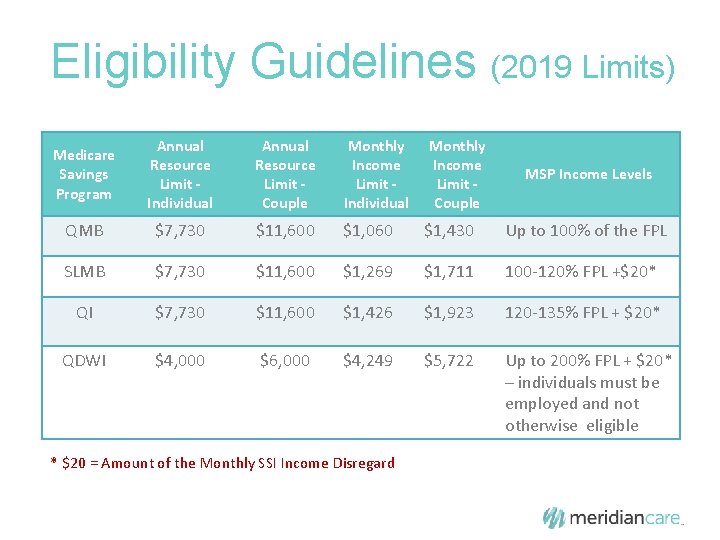
Eligibility Guidelines (2019 Limits) Medicare Savings Program Annual Resource Limit Individual Annual Resource Limit Couple Monthly Income Limit Individual QMB $7, 730 $11, 600 $1, 060 $1, 430 Up to 100% of the FPL SLMB $7, 730 $11, 600 $1, 269 $1, 711 100 -120% FPL +$20* QI $7, 730 $11, 600 $1, 426 $1, 923 120 -135% FPL + $20* QDWI $4, 000 $6, 000 $4, 249 $5, 722 Up to 200% FPL + $20* – individuals must be employed and not otherwise eligible * $20 = Amount of the Monthly SSI Income Disregard Monthly Income Limit Couple MSP Income Levels
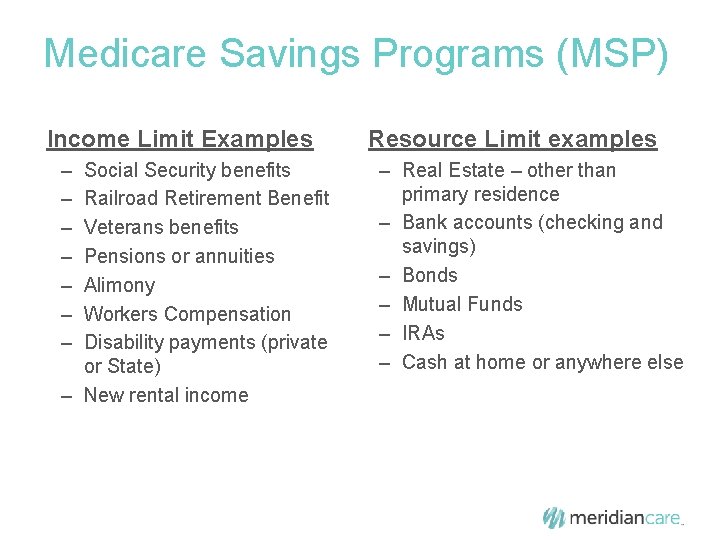
Medicare Savings Programs (MSP) Income Limit Examples – – – – Social Security benefits Railroad Retirement Benefit Veterans benefits Pensions or annuities Alimony Workers Compensation Disability payments (private or State) – New rental income Resource Limit examples – Real Estate – other than primary residence – Bank accounts (checking and savings) – Bonds – Mutual Funds – IRAs – Cash at home or anywhere else
Qualifications • Federal law defines income and resource standards for full Medicaid and the MSPs, but states have the discretion to raise those limits above the Federal floor • Income and resources levels for the MSPs are revised annually
How to Apply *From www. medicare. gov
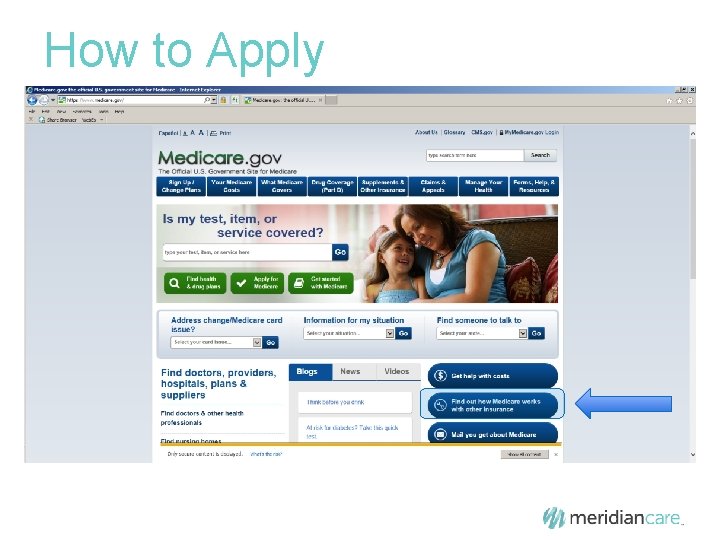
How to Apply
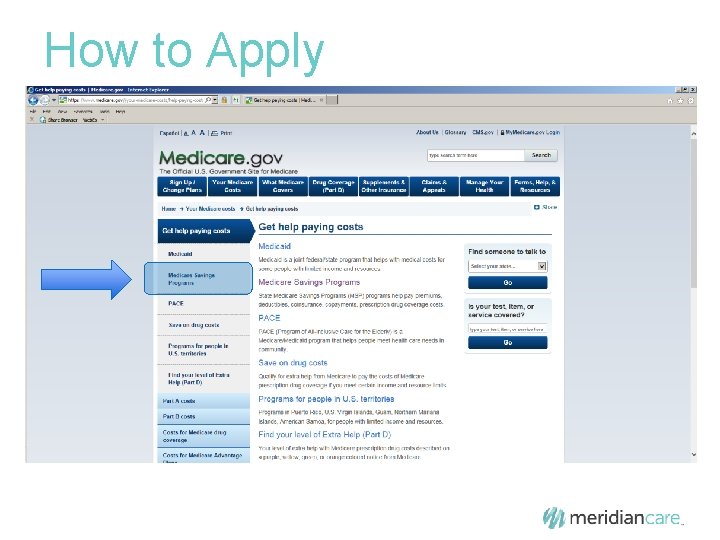
How to Apply
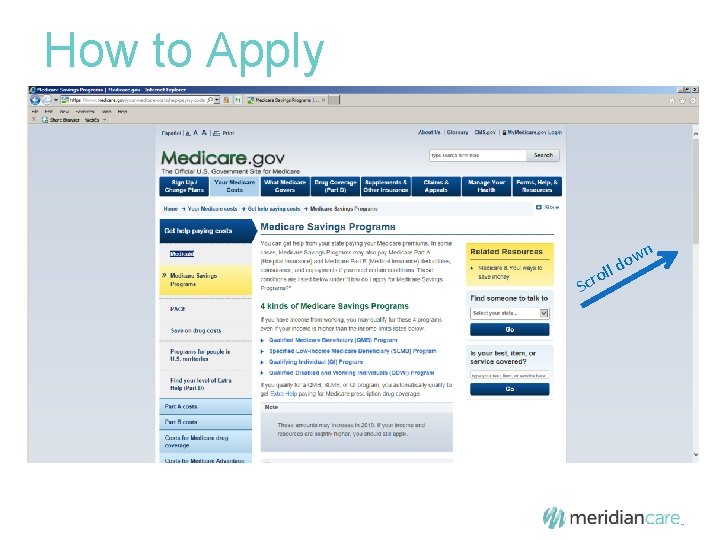
How to Apply Scr o wn o d ll
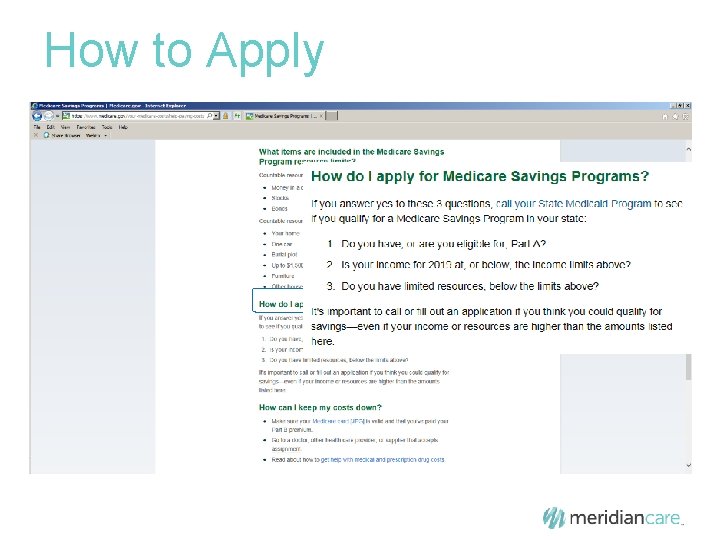
How to Apply
How to Apply • Individuals can also apply for an MSP while applying for a Low Income Subsidy
Low Income Subsidy (LIS) and Part D
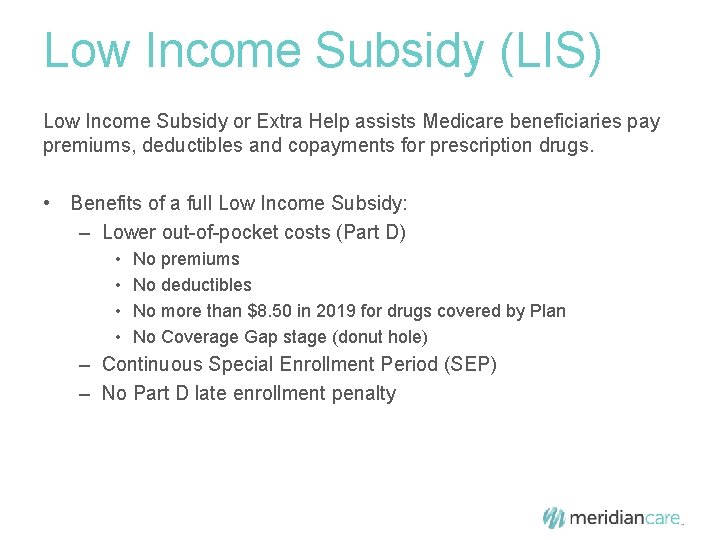
Low Income Subsidy (LIS) Low Income Subsidy or Extra Help assists Medicare beneficiaries pay premiums, deductibles and copayments for prescription drugs. • Benefits of a full Low Income Subsidy: – Lower out-of-pocket costs (Part D) • • No premiums No deductibles No more than $8. 50 in 2019 for drugs covered by Plan No Coverage Gap stage (donut hole) – Continuous Special Enrollment Period (SEP) – No Part D late enrollment penalty
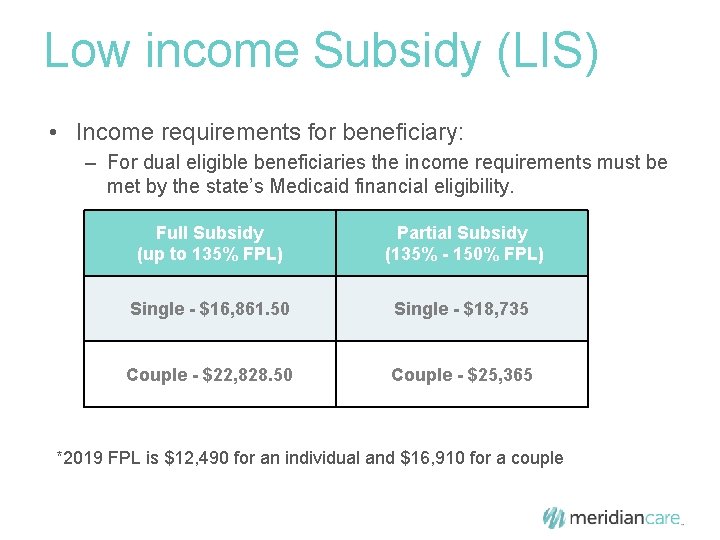
Low income Subsidy (LIS) • Income requirements for beneficiary: – For dual eligible beneficiaries the income requirements must be met by the state’s Medicaid financial eligibility. Full Subsidy (up to 135% FPL) Partial Subsidy (135% - 150% FPL) Single - $16, 861. 50 Single - $18, 735 Couple - $22, 828. 50 Couple - $25, 365 *2019 FPL is $12, 490 for an individual and $16, 910 for a couple
How to Apply for Extra Help • Contact the Social Security office: 1 -800 -325 -0778 www. socialsecurity. gov/prescriptionhelp

How To Apply
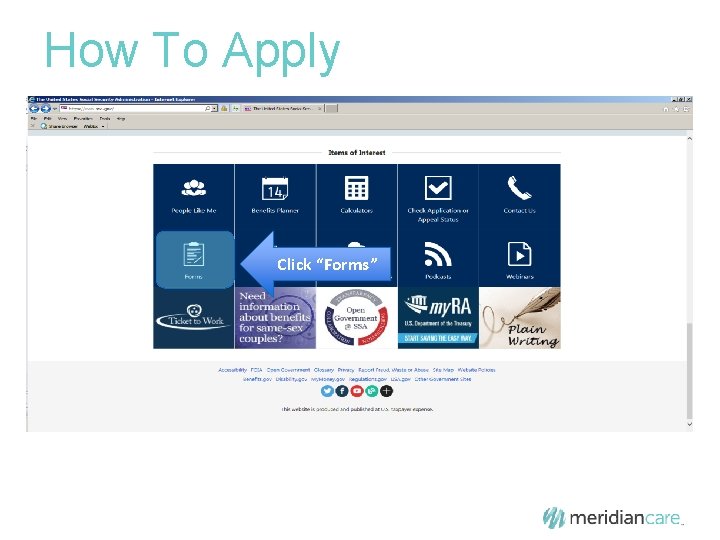
How To Apply Click “Forms”
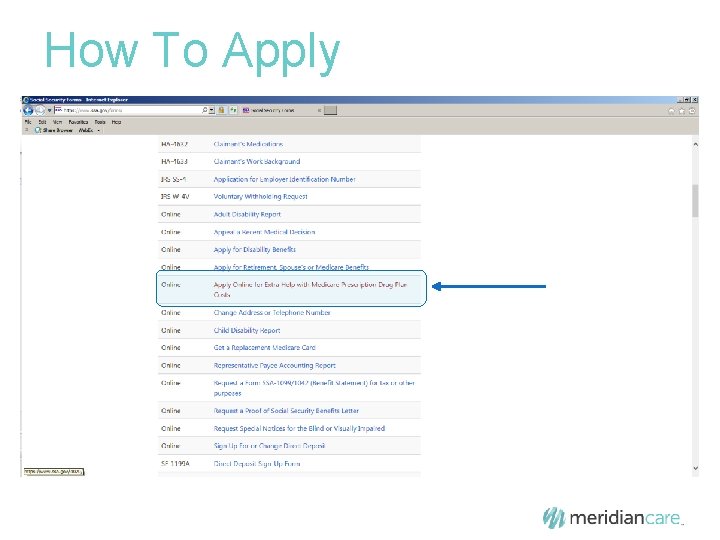
How To Apply
How To Apply
How To Apply
How To Apply
How To Apply
How To Apply

My. Care Ohio Medicare. Medicaid Program

My. Care Ohio: Integrating Medicare and Medicaid Benefits Ohio is home to approximately 182, 000 Ohioans who are covered by both Medicare and Medicaid. While each program provides individuals with access to critical services and care, coordination between the two programs is lacking. In late 2012, Ohio Medicaid became just the third state in the nation to receive federal approval for its plan to coordinate benefits for residents covered by Medicare and Medicaid. The result was My. Care Ohio, a three-year demonstration which uses a managed care approach to better connect services made available through each program. My. Care Ohio was launched in Northeast Ohio on May 1, 2014. The demonstration program is now serving more than 100, 000 residents in 29 Ohio counties.
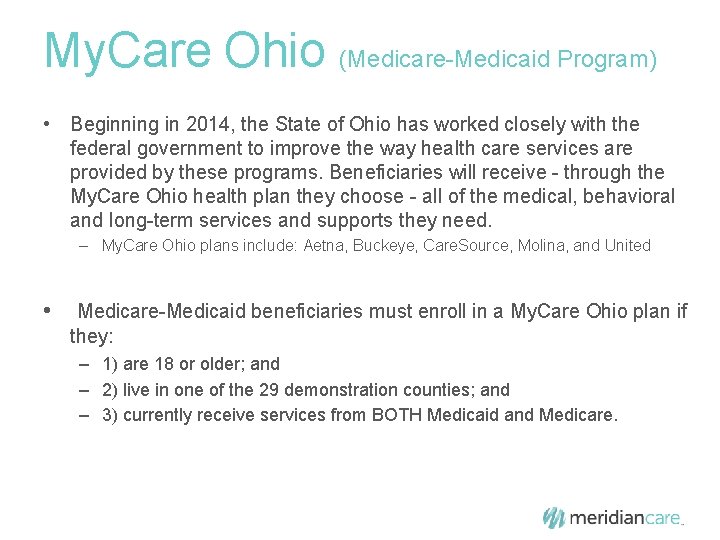
My. Care Ohio (Medicare-Medicaid Program) • Beginning in 2014, the State of Ohio has worked closely with the federal government to improve the way health care services are provided by these programs. Beneficiaries will receive - through the My. Care Ohio health plan they choose - all of the medical, behavioral and long-term services and supports they need. – My. Care Ohio plans include: Aetna, Buckeye, Care. Source, Molina, and United • Medicare-Medicaid beneficiaries must enroll in a My. Care Ohio plan if they: – 1) are 18 or older; and – 2) live in one of the 29 demonstration counties; and – 3) currently receive services from BOTH Medicaid and Medicare.
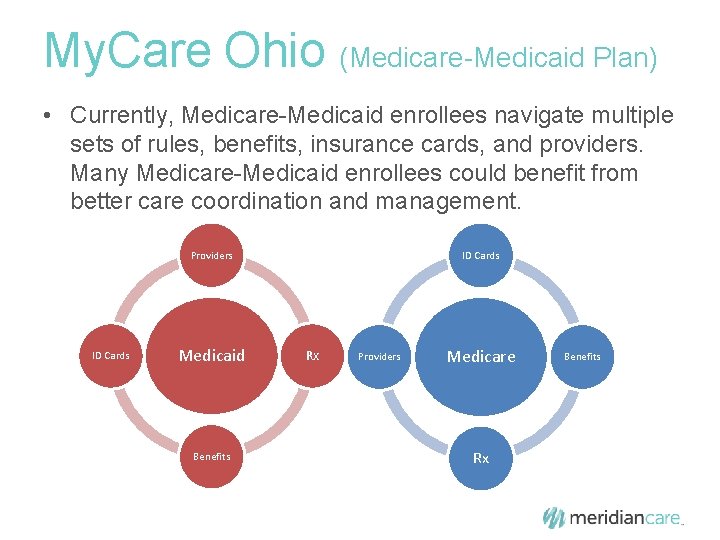
My. Care Ohio (Medicare-Medicaid Plan) • Currently, Medicare-Medicaid enrollees navigate multiple sets of rules, benefits, insurance cards, and providers. Many Medicare-Medicaid enrollees could benefit from better care coordination and management. Providers ID Cards Medicaid Benefits ID Cards Rx Providers Medicare Rx Benefits
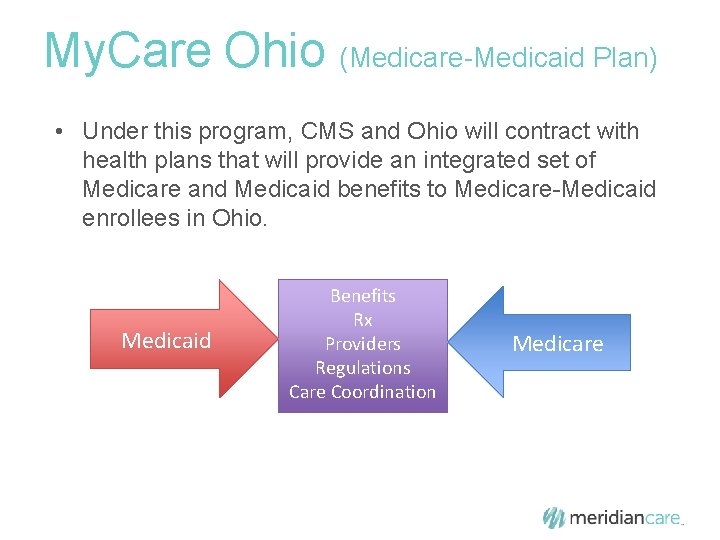
My. Care Ohio (Medicare-Medicaid Plan) • Under this program, CMS and Ohio will contract with health plans that will provide an integrated set of Medicare and Medicaid benefits to Medicare-Medicaid enrollees in Ohio. Medicaid Benefits Rx Providers Regulations Care Coordination Medicare
My. Care Ohio (Medicare-Medicaid Plan) • Beneficiaries will be auto-enrolled into a plan if they do not choose one, or they can choose to enroll into a plan. – After they are auto-enrolled, they will have 90 days to change their My. Care Ohio plan. • For more information, call the Ohio Medicaid Consumer Hotline: (800) 324 -8680 – M-F, 7 am to 8 pm; Saturday 8 am to 5 pm • Or visit online at www. ohiomh. com
One Last Thing! • People with Medicare should make sure their current address is correct with the Social Security Administration NOW, as needed • CMS mails cards based on the address of record at SSA • Can check address and make updates to it via My. Social. Security. gov – this is the fastest way to check and make changes • Can call SSA’s toll-free helpline or visit a local office. • People who lose their Medicare card will continue to be able to get a replacement (duplicate) card • People who believe they are victims of identity theft or Medicare fraud will be able to get a different new Medicare number by contacting 1800 -MEDICARE

Thank you for your time!
- Slides: 51