Medical University of Sofia Faculty of M Department


- Slides: 21

Medical University of Sofia, Faculty of M Department of Pharmacology and Toxico Antidislipidemic drugs (Summary) © Dr Ivan Lambev, Ph. D E-mail: itlambev@mail. bg
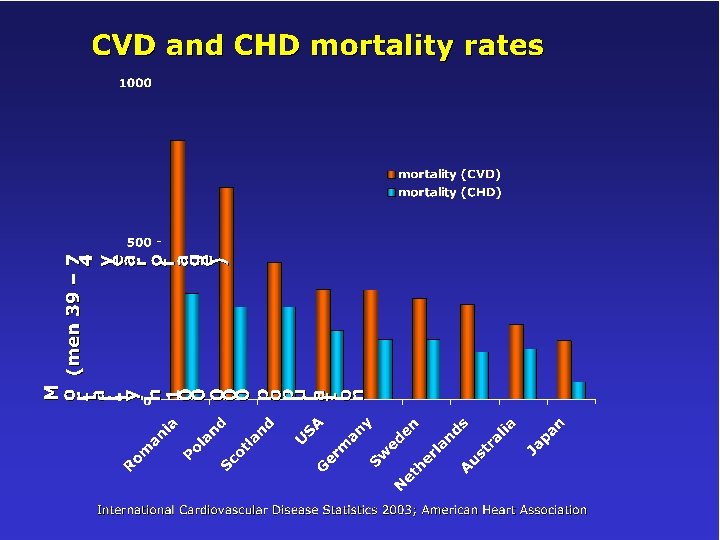
• CVD (cardiovascular disease) is the leading cause of death among the adult population in the world. • CHD (coronary heart disease) is the main cause of death in patients with CVD. • Total plasma cholesterol, high plasma levels of LDL, low levels of HDL are important risk factors for CHD.
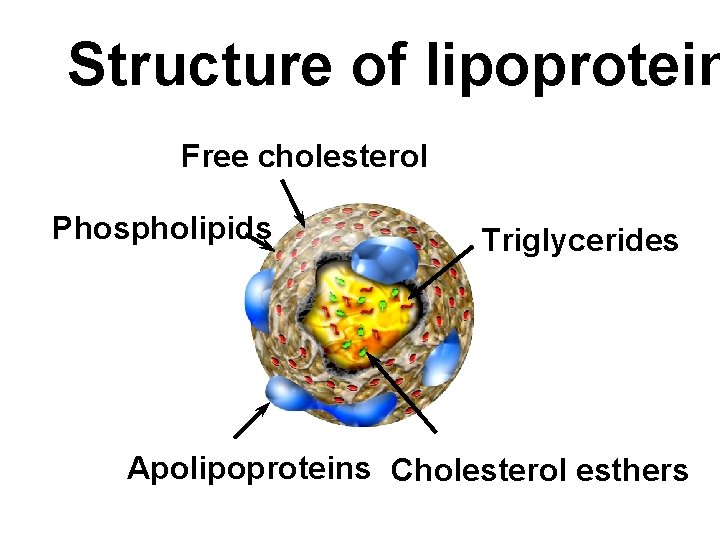
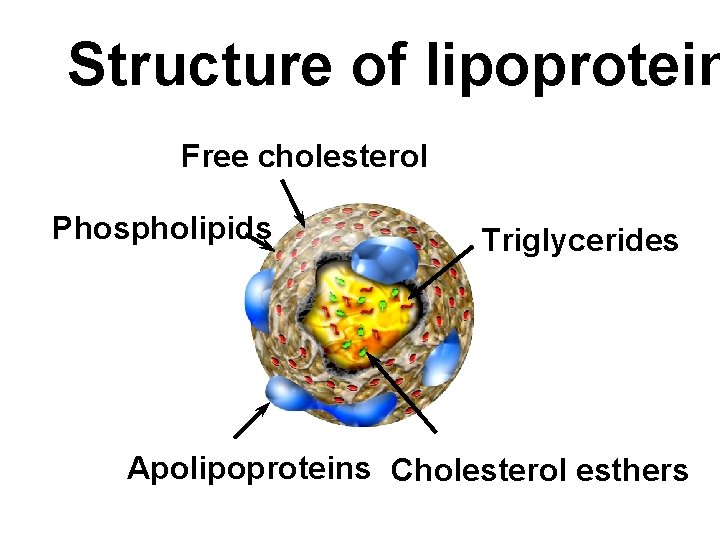
Structure of lipoprotein Free cholesterol Phospholipids Triglycerides Apolipoproteins Cholesterol esthers
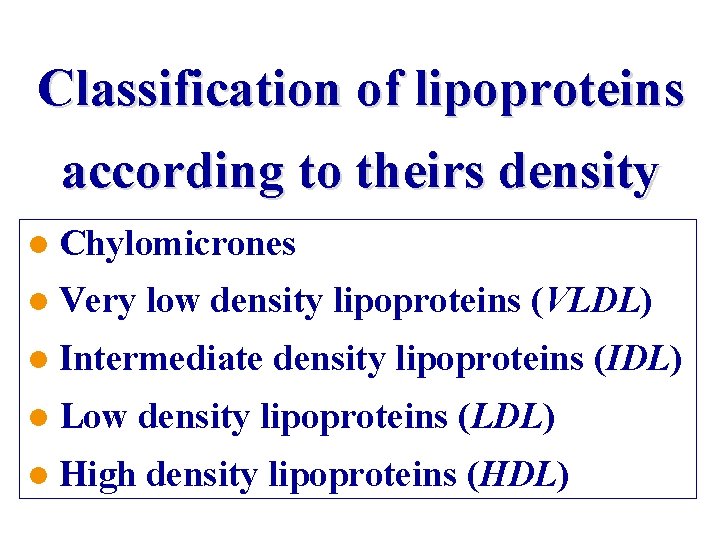
Classification of lipoproteins according to theirs density l Chylomicrones l Very low density lipoproteins (VLDL) l Intermediate density lipoproteins (IDL) l Low density lipoproteins (LDL) l High density lipoproteins (HDL)
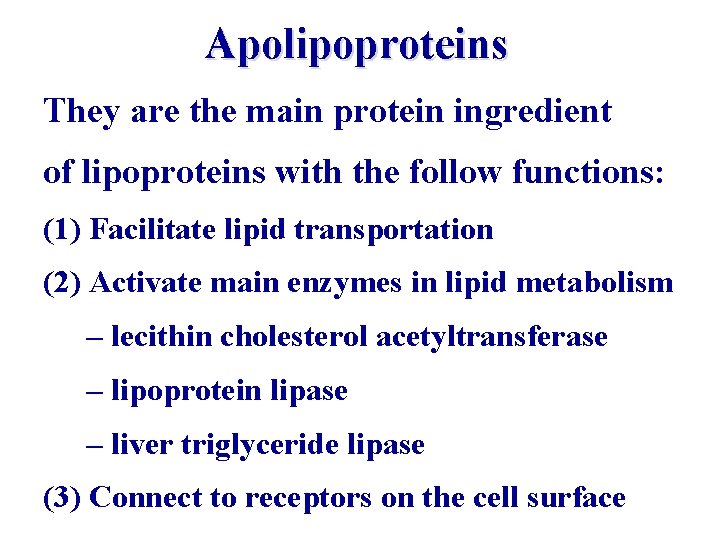
Apolipoproteins They are the main protein ingredient of lipoproteins with the follow functions: (1) Facilitate lipid transportation (2) Activate main enzymes in lipid metabolism – lecithin cholesterol acetyltransferase – lipoprotein lipase – liver triglyceride lipase (3) Connect to receptors on the cell surface
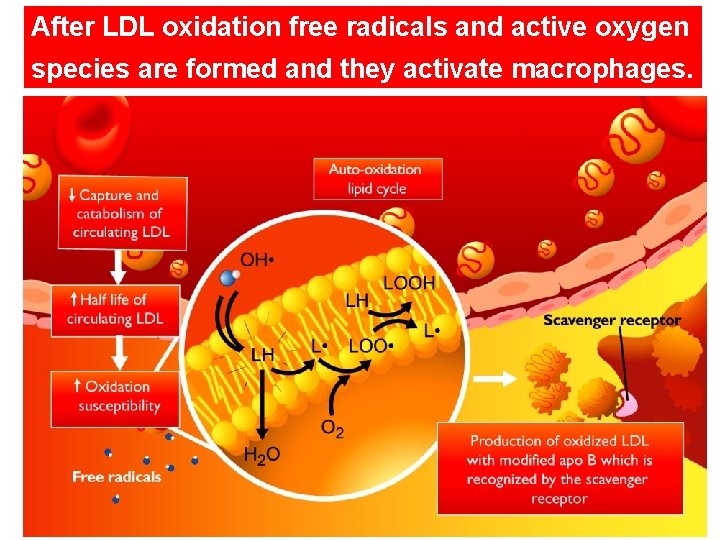
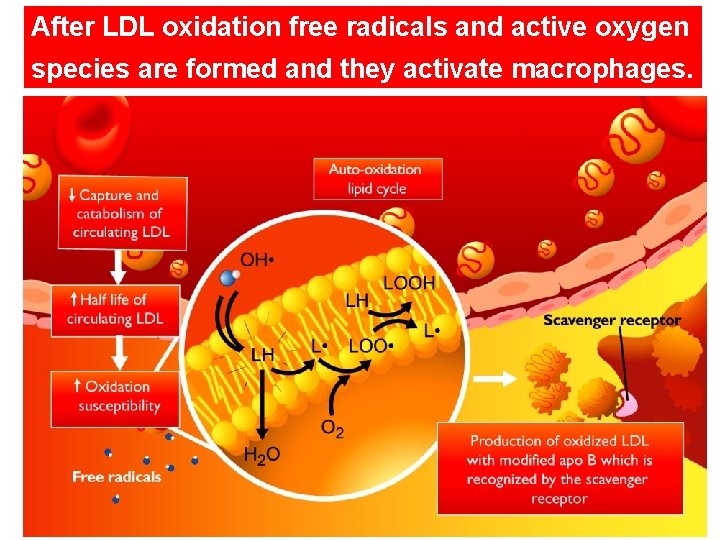
After LDL oxidation free radicals and active oxygen species are formed and they activate macrophages.
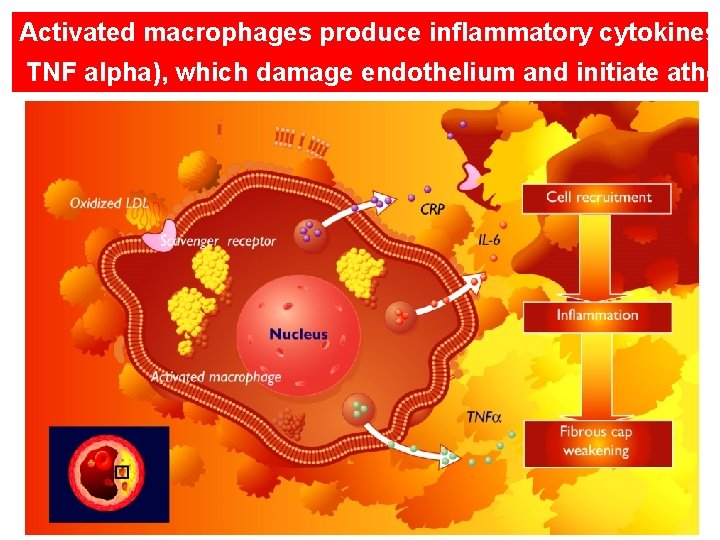
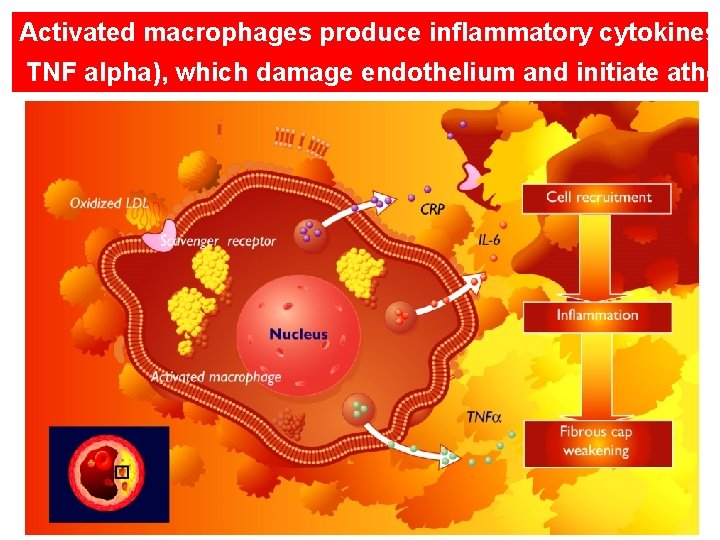
Activated macrophages produce inflammatory cytokines TNF alpha), which damage endothelium and initiate athe
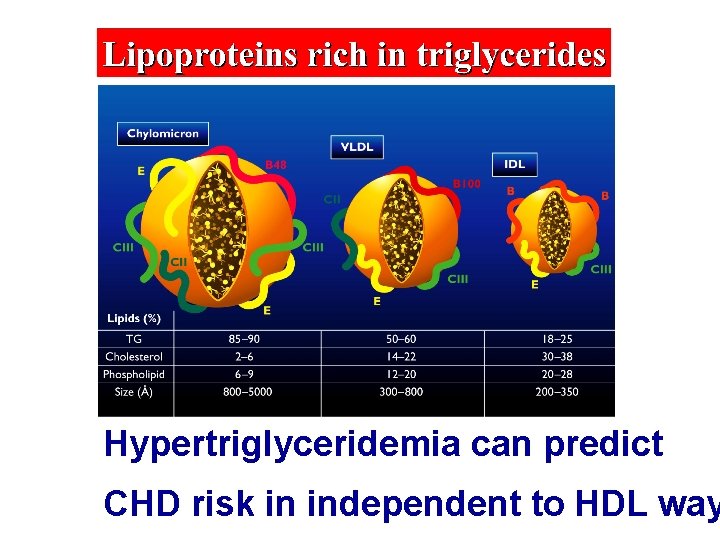
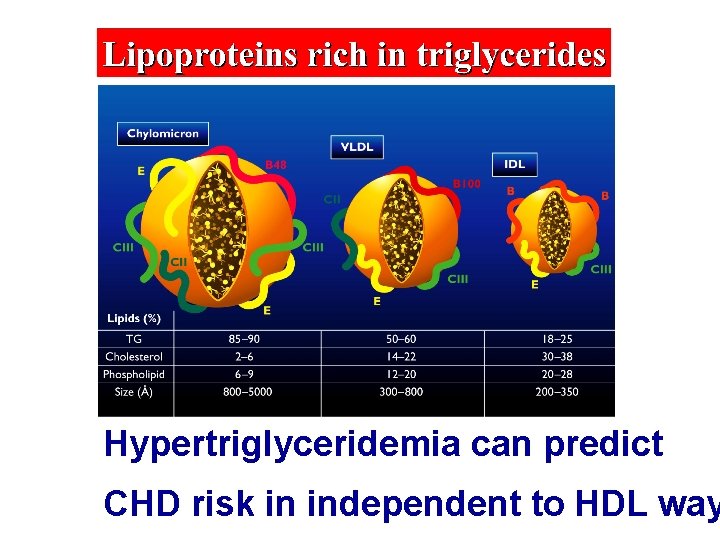
Hypertriglyceridemia can predict CHD risk in independent to HDL way
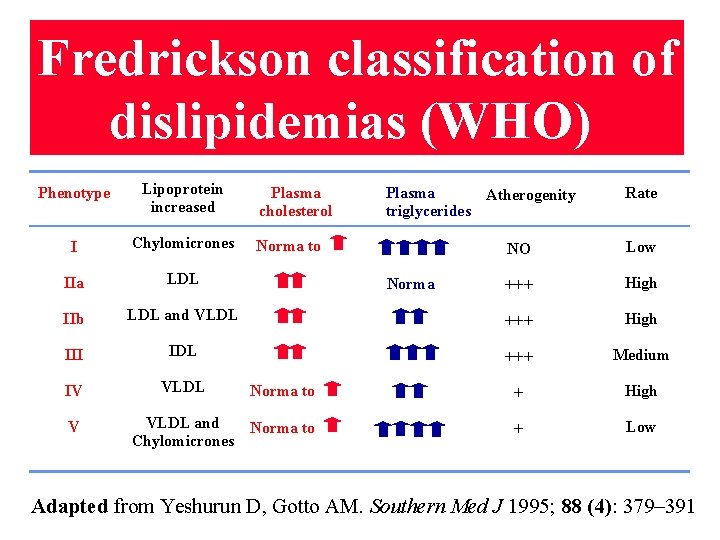
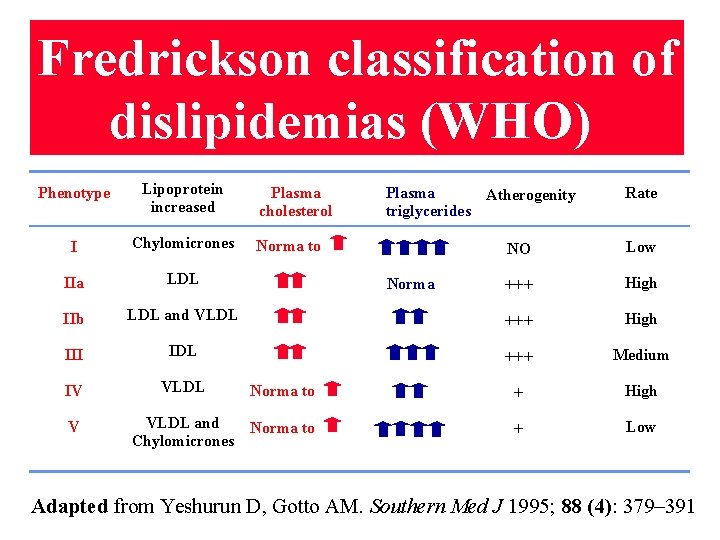
Fredrickson classification of dislipidemias (WHO) Phenotype Lipoprotein increased I Chylomicrones IIa LDL IIb Plasma cholesterol Plasma Atherogenity triglycerides Norma to Rate NO Low +++ High LDL and VLDL +++ High III IDL +++ Medium IV VLDL Norma to + High VLDL and Norma to Chylomicrones + Low V Norma Adapted from Yeshurun D, Gotto AM. Southern Med J 1995; 88 (4): 379– 391
Notes 1. Fredrickson classification does not take in account HDL-C (cholesterol in HDL), whose low plasma level have significant atherogenic role. 2. Homocysteine (norm 5– 15 mmol/l) is produced in methionine metabolism. Increased plasma levels of homocysteine is an independent risk factor for the development of atherosclerosis and CVD, even in normal lipid status. High homocysteine plasma levels are reduced by folic acid (vitamin B 3), pyridoxine (vitamin B 6) and vitamin B 12.
I. Drugs, inhibiting cholester and lipoprotein synthesis • Statins • Fibrates • Nicotinic acids
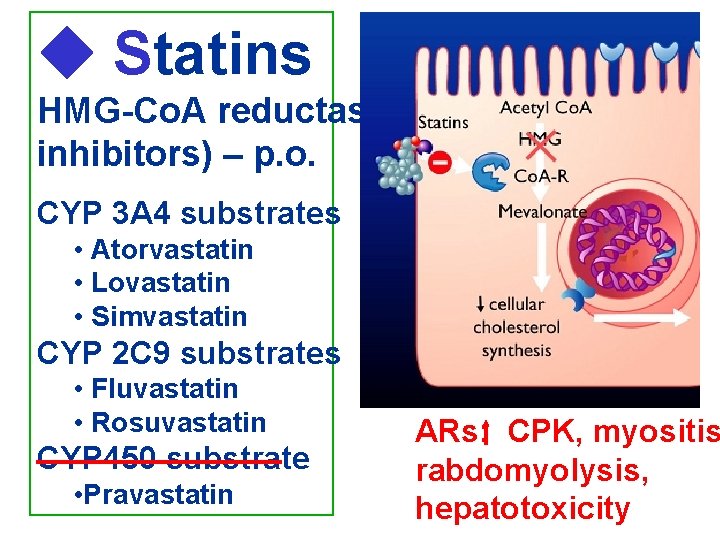
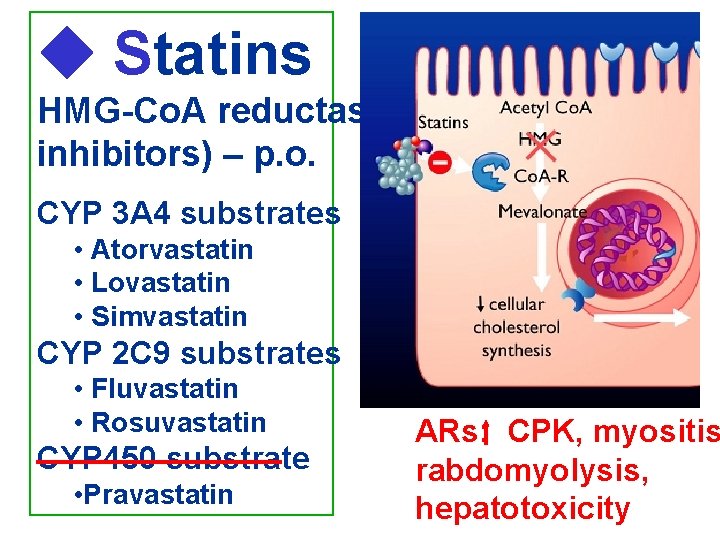
Statins HMG-Co. A reductase inhibitors) – p. o. CYP 3 A 4 substrates • Atorvastatin • Lovastatin • Simvastatin CYP 2 C 9 substrates • Fluvastatin • Rosuvastatin CYP 450 substrate • Pravastatin ARs: CPK, myositis rabdomyolysis, hepatotoxicity
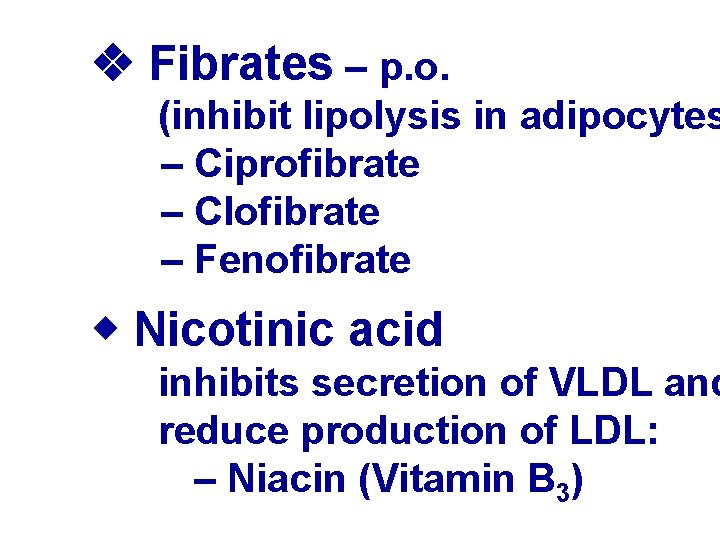
Fibrates – p. o. (inhibit lipolysis in adipocytes – Ciprofibrate – Clofibrate – Fenofibrate Nicotinic acid inhibits secretion of VLDL and reduce production of LDL: – Niacin (Vitamin B 3)
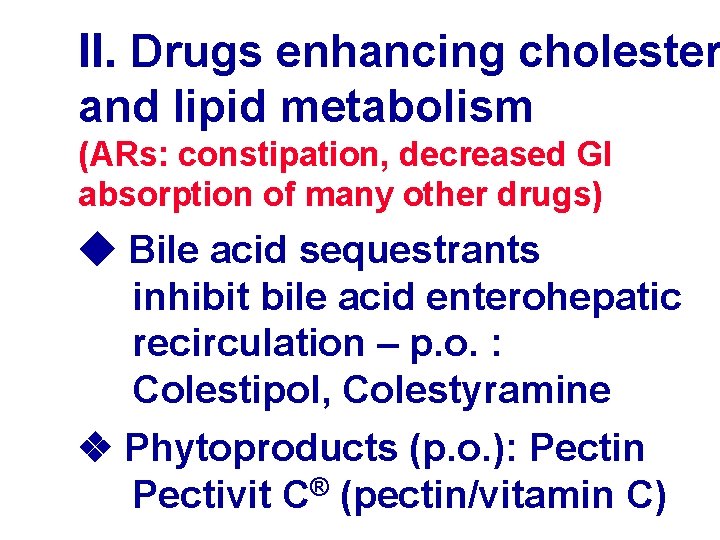
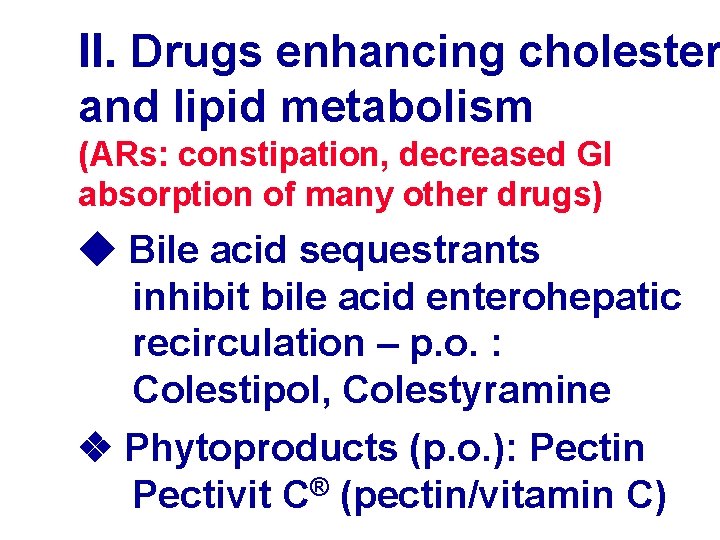
II. Drugs enhancing cholester and lipid metabolism (ARs: constipation, decreased GI absorption of many other drugs) Bile acid sequestrants inhibit bile acid enterohepatic recirculation – p. o. : Colestipol, Colestyramine Phytoproducts (p. o. ): Pectin Pectivit C® (pectin/vitamin C)
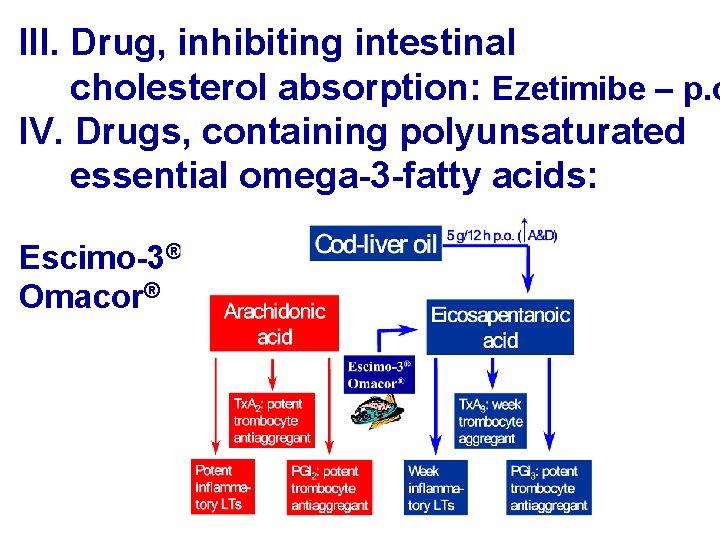
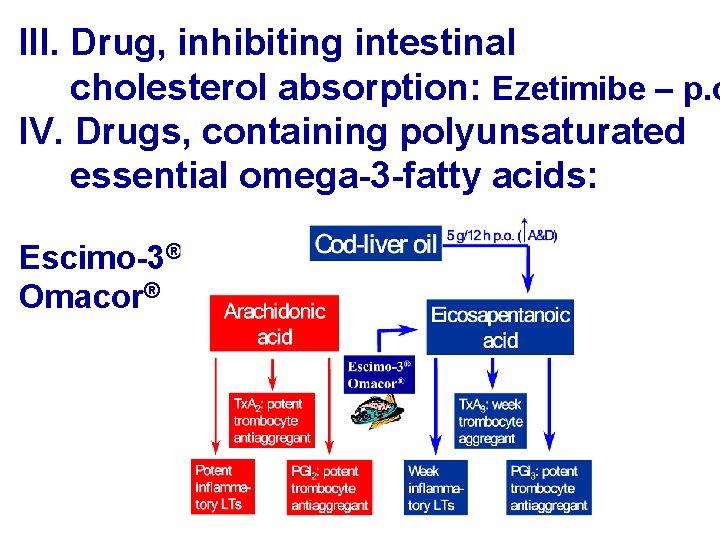
III. Drug, inhibiting intestinal cholesterol absorption: Ezetimibe – p. o IV. Drugs, containing polyunsaturated essential omega-3 -fatty acids: Escimo-3® Omacor®
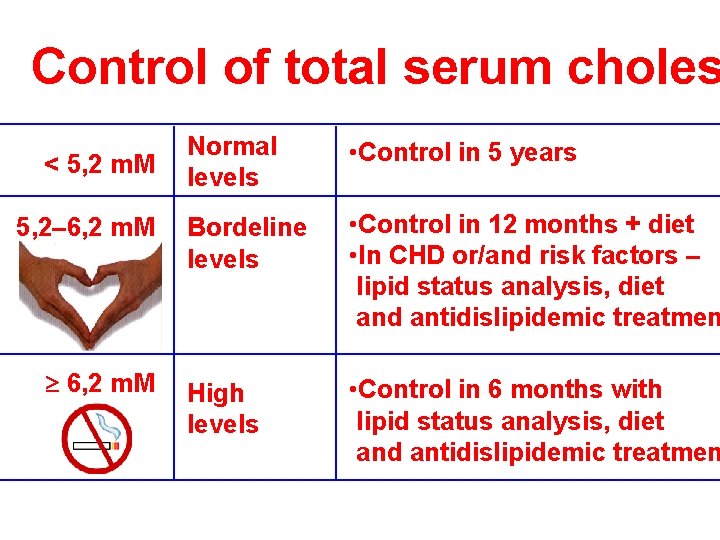
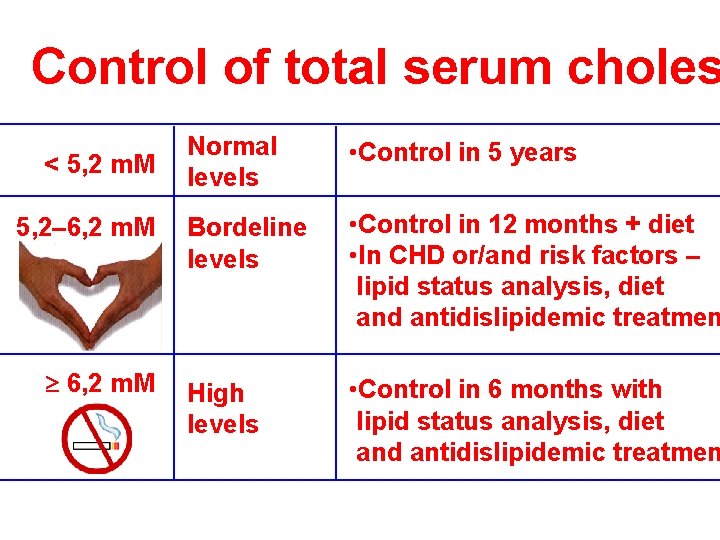
Control of total serum choles < 5, 2 m. M 5, 2– 6, 2 m. M Normal levels • Control in 5 years Bordeline levels • Control in 12 months + diet • In CHD or/and risk factors – lipid status analysis, diet and antidislipidemic treatmen High levels • Control in 6 months with lipid status analysis, diet and antidislipidemic treatmen

2/3 • Smoking of the • Lipid status risk Risk factor for CV • Homocysteine >15 mmol/l • Diabetes mellitus • Metabolic syndrome • Sedentary life style • BMI >30: >>> saturated fatty acids > >>salt and >>> sugar >>> (or <<<) alcohol <<< fruits and vegetables • Stress
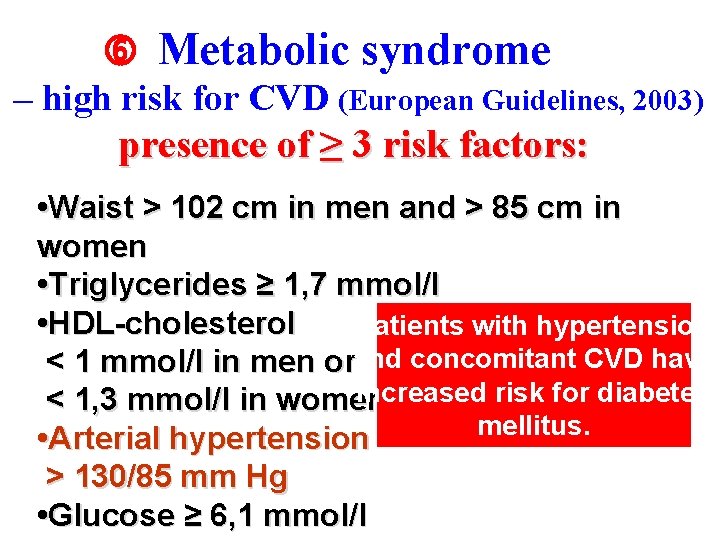
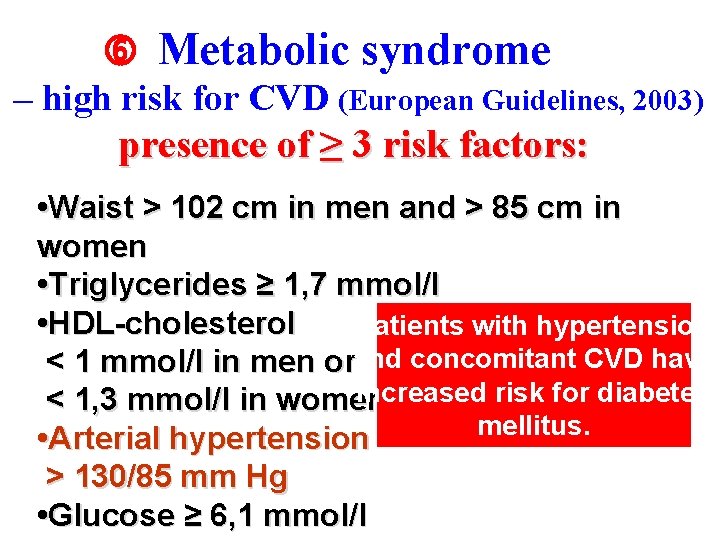
Metabolic syndrome – high risk for CVD (European Guidelines, 2003) presence of ≥ 3 risk factors: • Waist > 102 cm in men and > 85 cm in women • Triglycerides ≥ 1, 7 mmol/l • HDL-cholesterol Patients with hypertension < 1 mmol/l in men orand concomitant CVD have increased risk for diabetes < 1, 3 mmol/l in women mellitus. • Arterial hypertension > 130/85 mm Hg • Glucose ≥ 6, 1 mmol/l
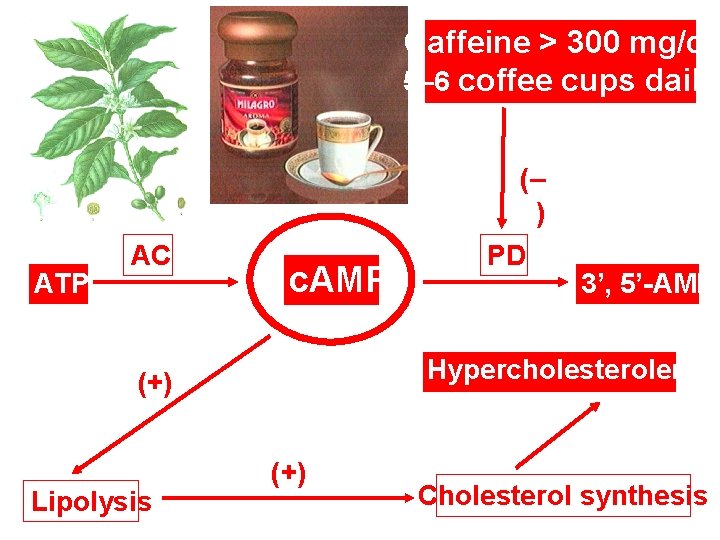
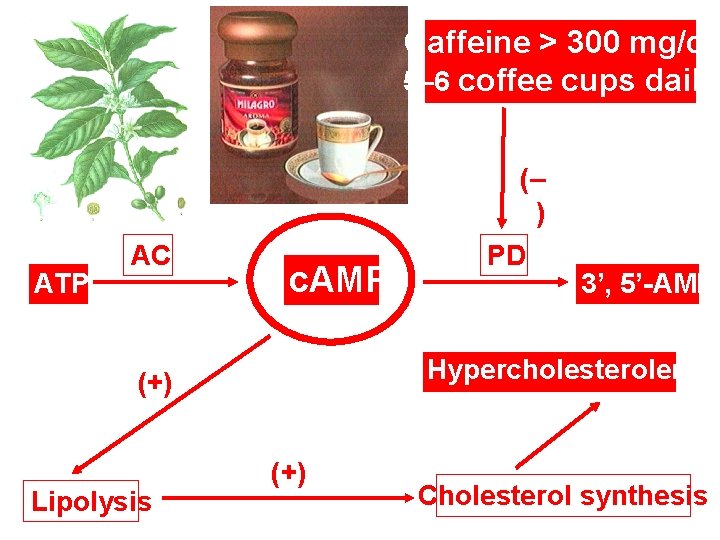
Caffeine > 300 mg/d: 5– 6 coffee cups daily (– ) ATP AC c. AMP 3’, 5’-AMP Hypercholesterolemia (+) Lipolysis PD (+) Cholesterol synthesis
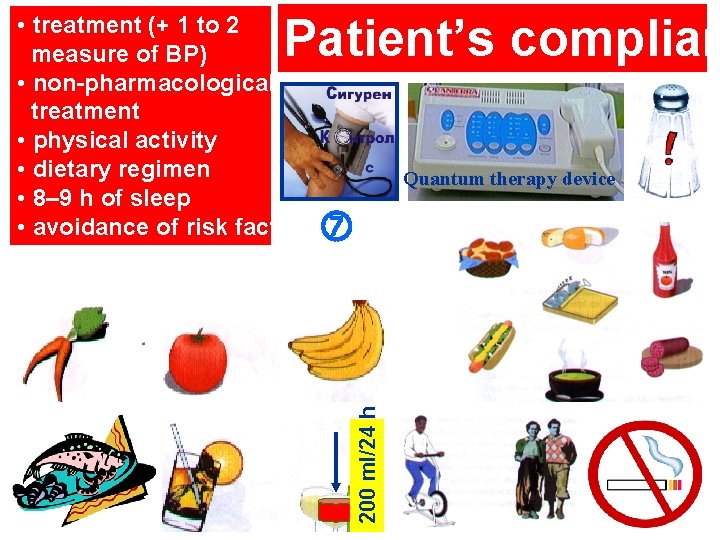
Patient’s complian Quantum therapy device 200 ml/24 h • treatment (+ 1 to 2 measure of BP) • non-pharmacological treatment • physical activity • dietary regimen • 8– 9 h of sleep • avoidance of risk factors