MEDICAL MIMICS OF PSYCHIATRIC DISORDER SUSAN R REDMONDVAUGHT











- Slides: 52
MEDICAL MIMICS OF PSYCHIATRIC DISORDER SUSAN R. REDMOND-VAUGHT, PH. D.

DELIRIUM A CLINICAL STATE CHARACTERIZED BY AN ACUTE, FLUCTUATING CHANGE IN MENTAL STATUS, WITH INATTENTION AND ALTERED LEVELS OF CONSCIOUSNESS. Primary Source: Merck Manual of Geriatrics, 3 rd Edition;

DELIRIUM (CONTINUED) “THE HALLMARK OF DELIRIUM IS ACUTE COGNITIVE DYSFUNCTION WITH IMPAIRED ATTENTIVENESS, WHICH DEVELOPS SUDDENLY OR OVER A SHORT TIME (USUALLY HOURS TO DAYS). ” AN INDIVIDUAL WITH DELIRIUM HAS SEVERE VARIATIONS IN THEIR MENTAL STATUS, WITH VARYING LEVELS OF INATTENTION AND ALTERED LEVELS OF CONSCIOUSNESS. OTHER SYMPTOMS INCLUDE: • CHANGES IN ORIENTATION, MEMORY, AND ABSTRACT THINKING • PSYCHOMOTOR ACTIVITY, OR LEVEL OF AROUSAL, MAY BE VARIABLY ABNORMAL • HALLUCINATIONS, • DELUSIONS, • TREMORS • ABNORMALITIES IN THE INDIVIDUAL’S SLEEP-WAKE CYCLE
DELIRIUM (CONTINUED) • IN SOME FRAIL, ELDERLY INDIVIDUALS, DELIRIUM PRECEDES THE APPEARANCE OF ANOTHER ILLNESS AND IS THE ONLY MANIFESTATION OF THAT ILLNESS • DELIRIUM MAY PERSIST FOR MANY WEEKS OR MONTHS • INFREQUENTLY IT NEVER CLEARLY RESOLVES, OR IT SHIFTS INTO TO CHRONIC COGNITIVE DYSFUNCTION
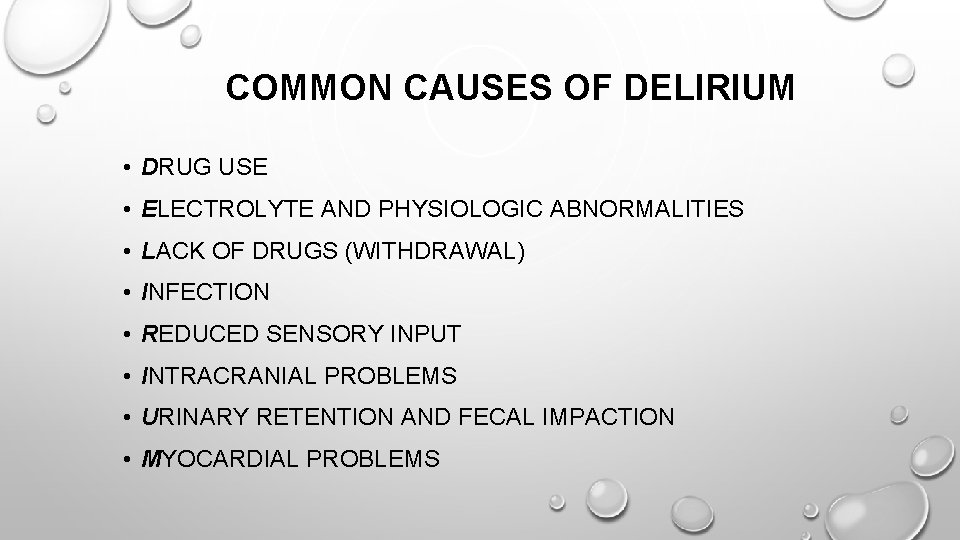
COMMON CAUSES OF DELIRIUM • DRUG USE • ELECTROLYTE AND PHYSIOLOGIC ABNORMALITIES • LACK OF DRUGS (WITHDRAWAL) • INFECTION • REDUCED SENSORY INPUT • INTRACRANIAL PROBLEMS • URINARY RETENTION AND FECAL IMPACTION • MYOCARDIAL PROBLEMS

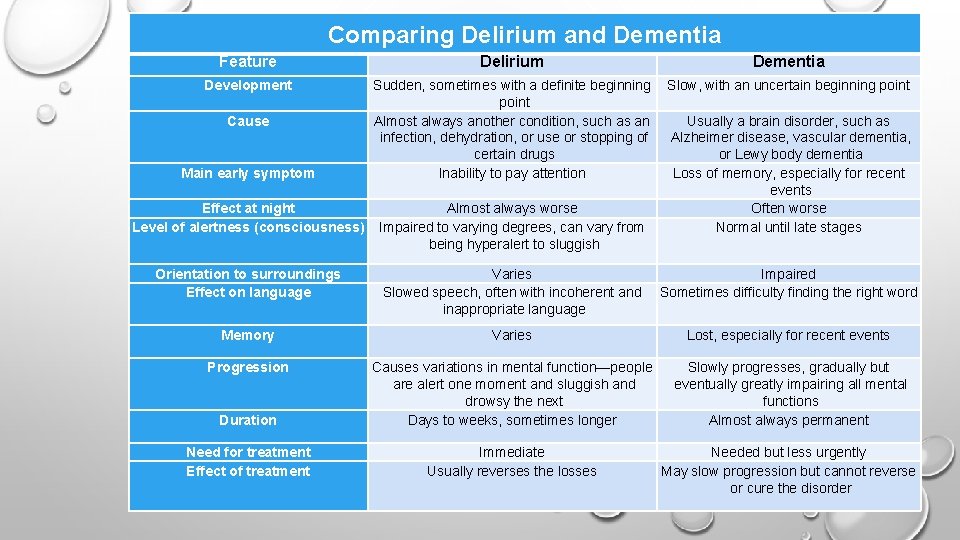
DELIRIUM VS. MAJOR NEUROCOGNITIVE DISORDER (DEMENTIA) “Delirium and dementia are the most common causes of mental (cognitive) dysfunction—the inability to acquire, retain, and use knowledge normally. Although delirium and dementia may occur together, they are quite different. Delirium begins suddenly, causes fluctuations in mental function, and is usually reversible. Dementia begins gradually, is slowly progressive, and is usually irreversible. Also, the two disorders affect mental function differently. Delirium affects mainly attention. Dementia affects mainly memory. Both delirium and dementia may occur at any age but are much more common among older people because of age-related changes in the brain. ” http: //www. merckmanuals. com/home/brain_spinal_cord_and_nerve_disorder s/delirium_and_dementia/overview_of_delirium_and_dementia. html
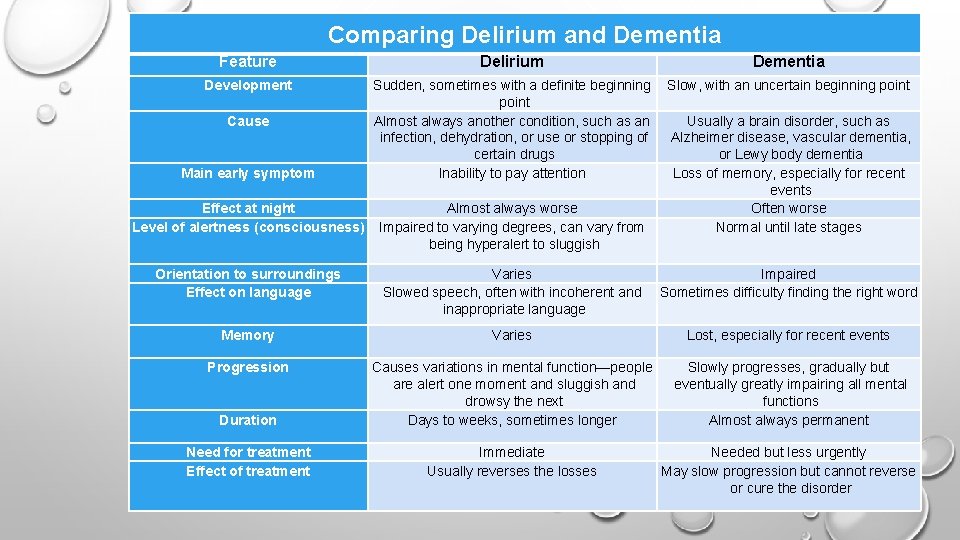
Comparing Delirium and Dementia Feature Delirium Dementia Development Sudden, sometimes with a definite beginning point Almost always another condition, such as an infection, dehydration, or use or stopping of certain drugs Inability to pay attention Slow, with an uncertain beginning point Cause Main early symptom Usually a brain disorder, such as Alzheimer disease, vascular dementia, or Lewy body dementia Loss of memory, especially for recent events Often worse Normal until late stages Effect at night Level of alertness (consciousness) Almost always worse Impaired to varying degrees, can vary from being hyperalert to sluggish Orientation to surroundings Effect on language Varies Slowed speech, often with incoherent and inappropriate language Impaired Sometimes difficulty finding the right word Memory Varies Lost, especially for recent events Progression Duration Causes variations in mental function—people are alert one moment and sluggish and drowsy the next Days to weeks, sometimes longer Slowly progresses, gradually but eventually greatly impairing all mental functions Almost always permanent Need for treatment Effect of treatment Immediate Usually reverses the losses Needed but less urgently May slow progression but cannot reverse or cure the disorder
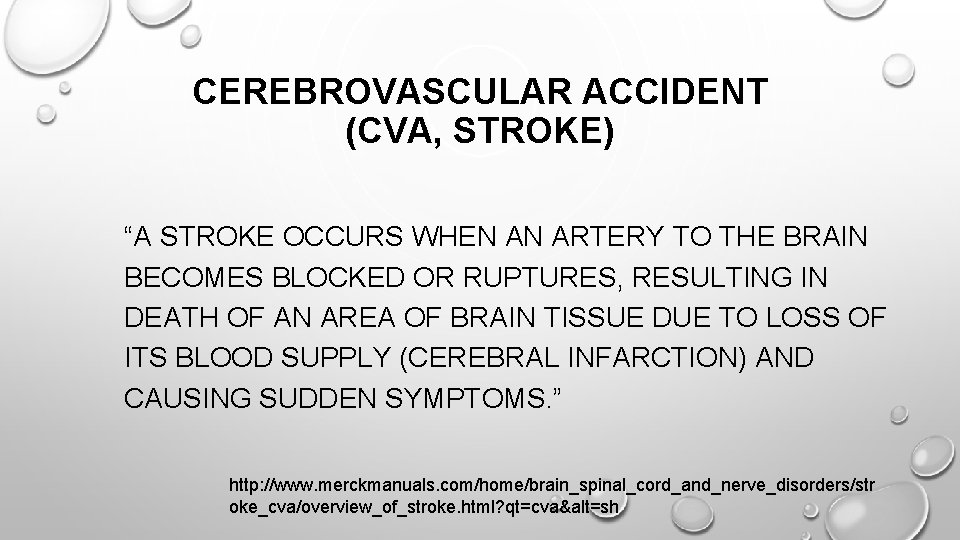
CEREBROVASCULAR ACCIDENT (CVA, STROKE) “A STROKE OCCURS WHEN AN ARTERY TO THE BRAIN BECOMES BLOCKED OR RUPTURES, RESULTING IN DEATH OF AN AREA OF BRAIN TISSUE DUE TO LOSS OF ITS BLOOD SUPPLY (CEREBRAL INFARCTION) AND CAUSING SUDDEN SYMPTOMS. ” http: //www. merckmanuals. com/home/brain_spinal_cord_and_nerve_disorders/str oke_cva/overview_of_stroke. html? qt=cva&alt=sh
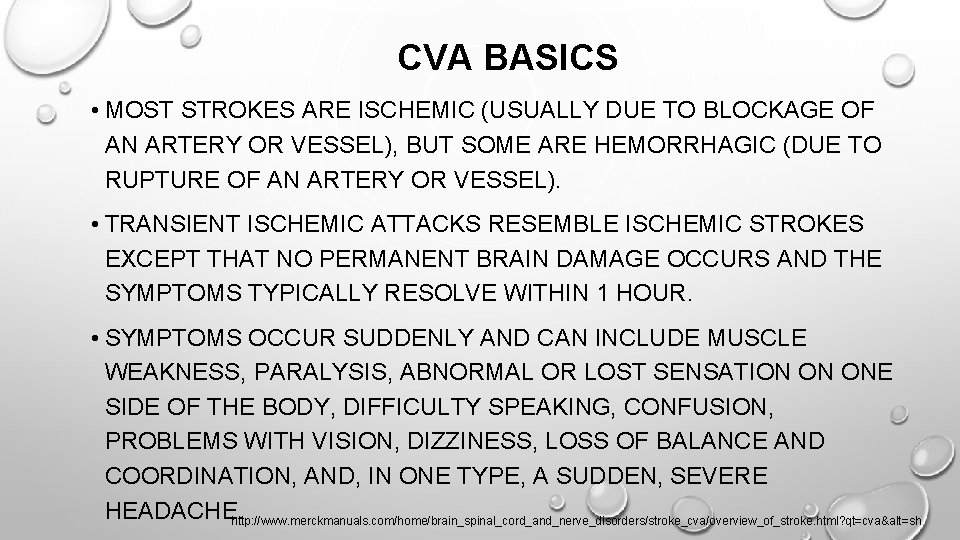
CVA BASICS • STROKES CAN HAPPEN TO PEOPLE OF ANY AGE. MOST STROKES ARE ISCHEMIC (USUALLY DUE TO BLOCKAGE OF AN ARTERY OR VESSEL), BUT SOME ARE HEMORRHAGIC (DUE TO RUPTURE OF AN ARTERY OR VESSEL). • TRANSIENT ISCHEMIC ATTACKS RESEMBLE ISCHEMIC STROKES EXCEPT THAT NO PERMANENT BRAIN DAMAGE OCCURS AND THE SYMPTOMS TYPICALLY RESOLVE WITHIN 1 HOUR. • SYMPTOMS OCCUR SUDDENLY AND CAN INCLUDE MUSCLE WEAKNESS, PARALYSIS, ABNORMAL OR LOST SENSATION ON ONE SIDE OF THE BODY, DIFFICULTY SPEAKING, CONFUSION, PROBLEMS WITH VISION, DIZZINESS, http: //www. merckmanuals. com/home/brain_spinal_cord_and_nerve_disorders/stroke_cva/overview_of_stroke. html? qt=cva&alt=sh LOSS OF BALANCE AND COORDINATION, AND, IN ONE TYPE, A SUDDEN, SEVERE HEADACHE.
CVA BASICS • MOST STROKES ARE ISCHEMIC (USUALLY DUE TO BLOCKAGE OF AN ARTERY OR VESSEL), BUT SOME ARE HEMORRHAGIC (DUE TO RUPTURE OF AN ARTERY OR VESSEL). • TRANSIENT ISCHEMIC ATTACKS RESEMBLE ISCHEMIC STROKES EXCEPT THAT NO PERMANENT BRAIN DAMAGE OCCURS AND THE SYMPTOMS TYPICALLY RESOLVE WITHIN 1 HOUR. • SYMPTOMS OCCUR SUDDENLY AND CAN INCLUDE MUSCLE WEAKNESS, PARALYSIS, ABNORMAL OR LOST SENSATION ON ONE SIDE OF THE BODY, DIFFICULTY SPEAKING, CONFUSION, PROBLEMS WITH VISION, DIZZINESS, LOSS OF BALANCE AND COORDINATION, AND, IN ONE TYPE, A SUDDEN, SEVERE HEADACHE. http: //www. merckmanuals. com/home/brain_spinal_cord_and_nerve_disorders/stroke_cva/overview_of_stroke. html? qt=cva&alt=sh
CVA BASICS • DIAGNOSIS IS BASED MAINLY ON SYMPTOMS, BUT IMAGING AND BLOOD TESTS ARE ALSO DONE. • RECOVERY AFTER A STROKE DEPENDS ON MANY FACTORS, SUCH AS THE LOCATION AND AMOUNT OF DAMAGE, THE PERSON'S AGE, AND THE PRESENCE OF OTHER DISORDERS. • CONTROLLING HIGH BLOOD PRESSURE, HIGH CHOLESTEROL LEVELS, AND HIGH BLOOD SUGAR LEVELS AND NOT SMOKING HELP PREVENT STROKES. • TREATMENT MAY INCLUDE DRUGS TO MAKE BLOOD LESS LIKELY TO CLOT OR TO BREAK UP CLOTS AND SOMETIMES SURGERY OR http: //www. merckmanuals. com/home/brain_spinal_cord_and_nerve_disorders/stroke_cva/overview_of_stroke. html? qt=cva&alt=sh ANGIOPLASTY.
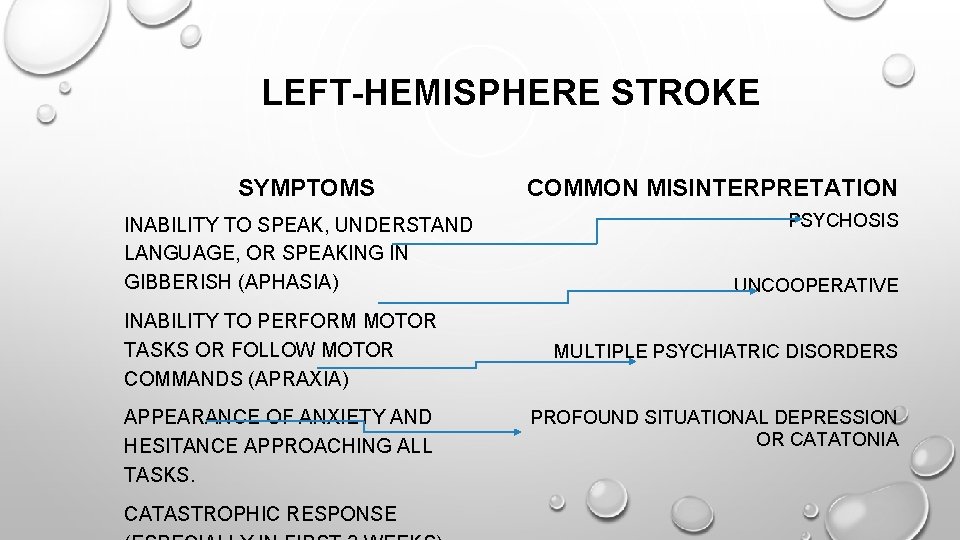
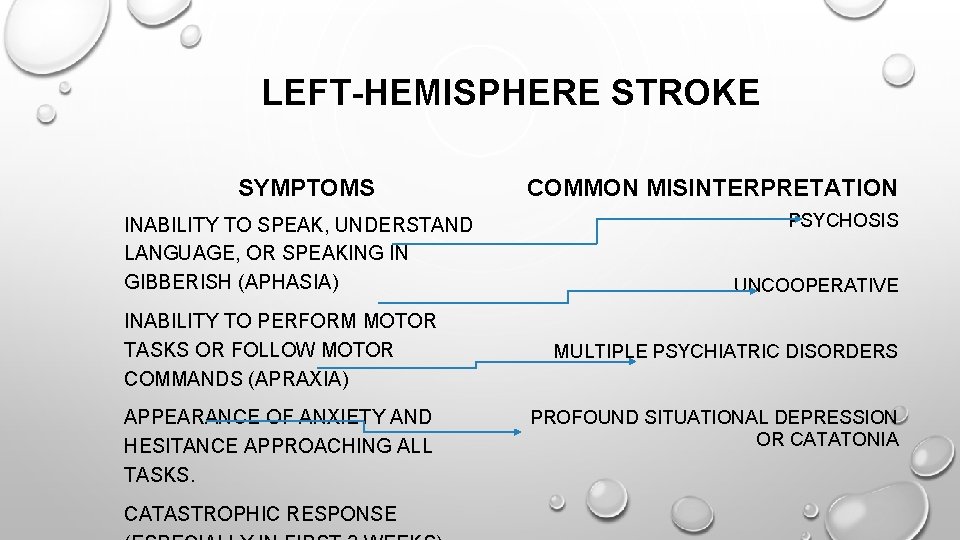
LEFT-HEMISPHERE STROKE SYMPTOMS INABILITY TO SPEAK, UNDERSTAND LANGUAGE, OR SPEAKING IN GIBBERISH (APHASIA) INABILITY TO PERFORM MOTOR TASKS OR FOLLOW MOTOR COMMANDS (APRAXIA) APPEARANCE OF ANXIETY AND HESITANCE APPROACHING ALL TASKS. CATASTROPHIC RESPONSE COMMON MISINTERPRETATION PSYCHOSIS UNCOOPERATIVE MULTIPLE PSYCHIATRIC DISORDERS PROFOUND SITUATIONAL DEPRESSION OR CATATONIA
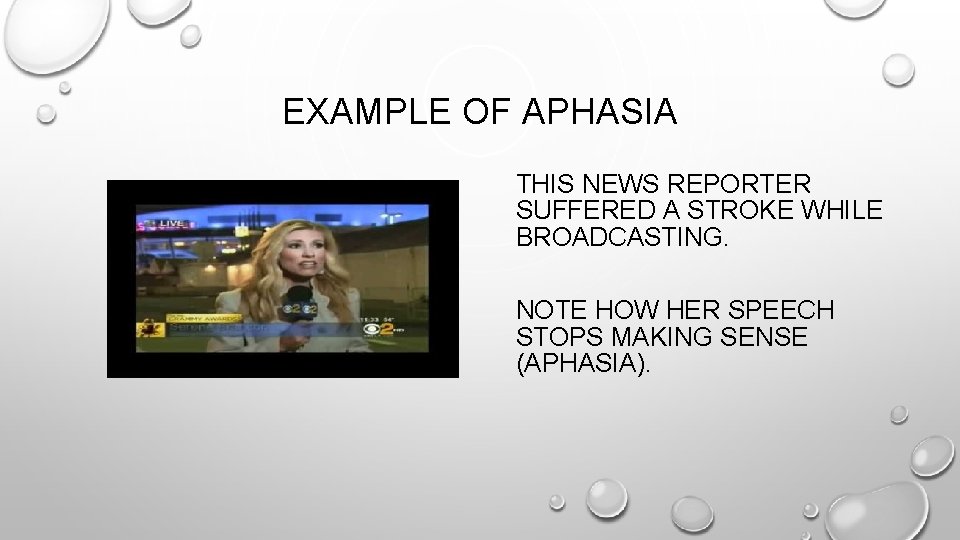
EXAMPLE OF APHASIA THIS NEWS REPORTER SUFFERED A STROKE WHILE BROADCASTING. NOTE HOW HER SPEECH STOPS MAKING SENSE (APHASIA).
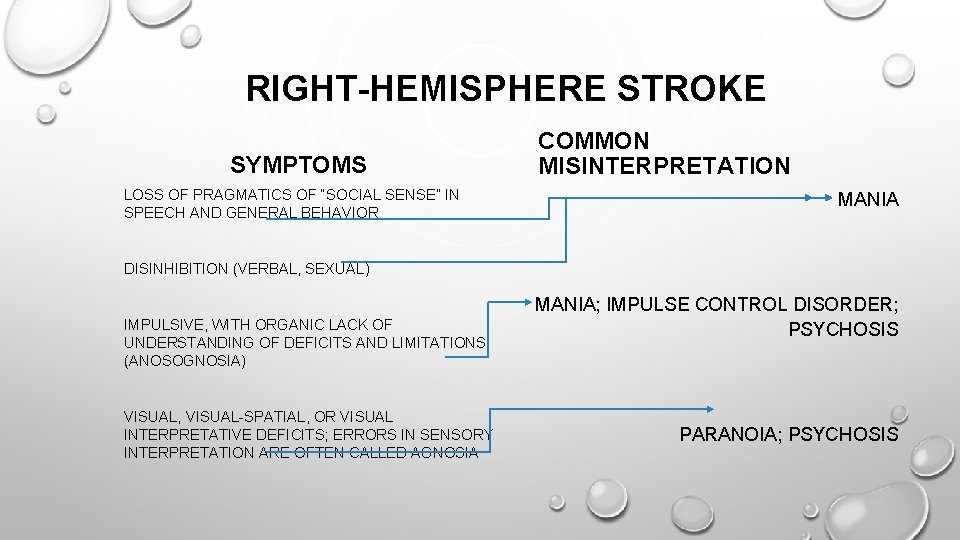
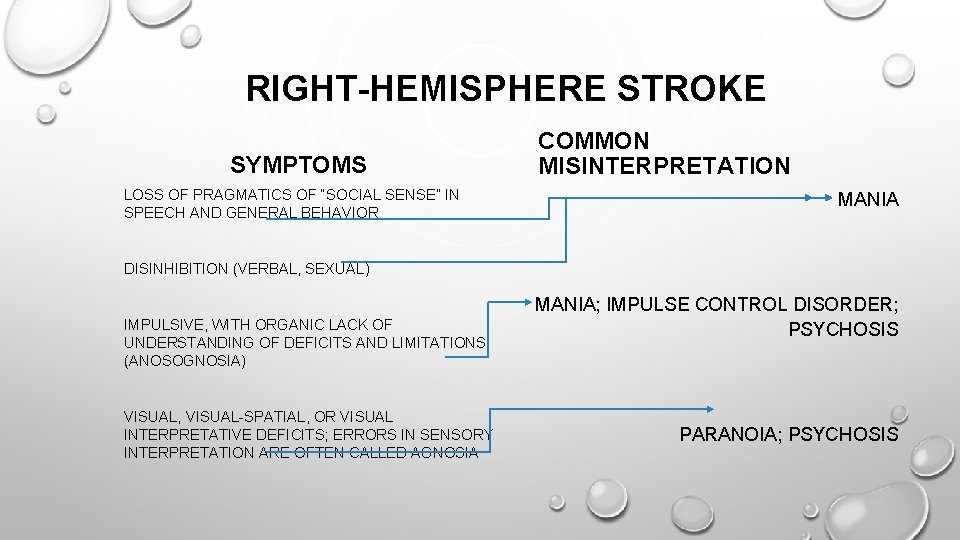
RIGHT-HEMISPHERE STROKE SYMPTOMS LOSS OF PRAGMATICS OF “SOCIAL SENSE” IN SPEECH AND GENERAL BEHAVIOR COMMON MISINTERPRETATION MANIA DISINHIBITION (VERBAL, SEXUAL) IMPULSIVE, WITH ORGANIC LACK OF UNDERSTANDING OF DEFICITS AND LIMITATIONS (ANOSOGNOSIA) VISUAL, VISUAL-SPATIAL, OR VISUAL INTERPRETATIVE DEFICITS; ERRORS IN SENSORY INTERPRETATION ARE OFTEN CALLED AGNOSIA MANIA; IMPULSE CONTROL DISORDER; PSYCHOSIS PARANOIA; PSYCHOSIS

ANY STROKE • DISORIENTATION AND DELIRIUM IN THE FIRST 14 -30 DAYS • FATIGUE • SUDDEN EPISODES OF CRYING OR SOBBING/MARKED EMOTIONAL LABILITY • REACTIONS TO SENSORY DEPRIVATION DUE TO LOSS OF VISION, HEARING, TACTILE INPUT, SMELL, OR TASTE, PLUS ISOLATION OF BEING HOSPITALIZED
GENERAL SUGGESTIONS • USE EXTREME CAUTION IN ASSUMING A PERSON IS HAVING PSYCHIATRIC SYMPTOMS IF THE STROKE OCCURRED <30 DAYS • CONSIDER CONSULTING NEUROLOGY OR SEEKING STROKE REHABILITATION VS. PSYCHIATRIC CARE IF PROBLEMATIC BEHAVIOR OR SYMPTOM PRESENTATION IS A DIRECT RESULT OF THE LOCATION OF THE STROKE • BEWARE OF USING AFFECT (FACIAL EXPRESSION) AS A MEASURE OF PSYCHIATRIC STABILITY OR MOOD STATE IN INDIVIDUALS WITH A HISTORY OF STROKE • ALWAYS BE AWARE THAT STATE PSYCHIATRIC FACILITIES DO NOT OFFER THERAPIES NECESSARY TO REHABILITATE
RECENT SURGERY - OVERVIEW • SOME PATIENTS DEVELOP POST-SURGICAL DELIRIUM (TYPICAL ONSET 0 -7 DAYS) IN 1 -2 WEEKS FOLLOWING A SURGICAL PROCEDURE • ACUTE AND OFTEN DANGEROUS CONDITION • MORE COMMON IN: • ELDERLY PATIENTS OR • PATIENTS WITH KNOWN BRAIN INJURY OR • PATIENTS WITH INTELLECTUAL DISABILITY • FIRST NOTED IN 1891 BY PROFESSOR LE DENTU • MODERN STATISTICS SUGGEST THAT 8%, OR ROUGHLY 1 IN 10 PATIENTS WITH POST-SURGICAL DELIRIUM WILL DIE, OFTEN WITHIN 90 DAYS OF THE SURGERY • CAUSES OF DEATH USUALLY TRACE TO SUDDEN ALTERATIONS IN BLOOD PRESSURES, CARDIAC ABNORMALITIES, STROKE, OR OTHER METABOLIC DERANGEMENT
RECENT SURGERY -TREATMENT • DEBATES CENTER AROUND USE OF CHEMICAL OR PHYSICAL RESTRAINTS TO CONTAIN PATIENTS DURING THE WORST OF THE POST-SURGICAL DELIRIUM • “SOCIAL RESTRAINT” OR THE USE OF SITTERS IS ALSO ADVOCATED • TYPICALLY, BETTER OUTCOMES RESULT FROM SOCIAL RESTRAINT • RESEARCH SUGGESTS THAT THE LESS MEDICATION GIVEN, AND THE MORE MEDICATIONS REMOVED, THE BETTER THE OUTCOME • CLOSE MEDICAL MONITORING WITH IMMEDIATE RESPONSE TO OFTEN RAPIDLY-DEVELOPING CONDITIONS IS IMPORTANT. THESE CONDITIONS INCLUDE: • HYPOTENSION • HYPERTENSION • RENAL INSUFFICIENCY • RENAL FAILURE • ARRHYTHMIAS • STROKE

RECENT SURGERY -TREATMENT • PHYSICIANS MAY PROCEED WITH COMMITMENT REQUESTS • NOT APPROPRIATE TO REFER PATIENTS TO FACILITIES SUCH AS WESTERN STATE HOSPITAL, EASTERN STATE HOSPITAL, CENTRAL STATE HOSPITAL, APPALACHIAN REGIONAL HOSPITAL, OAKWOOD, OR OUTWOOD • POST-SURGICAL DELIRIUM TREATMENT WOULD ENTAIL MULTIPLE RETRANSFERS BACK TO ACUTE MEDICAL CARE • WHAT HAPPENS TO THE INDIVIDUAL? • • MULTIPLE ENVIRONMENTAL CHANGES DISORGANIZATION IN MEDICAL APPROACHES PROLONGED DELIRIOUS STATE SIGNIFICANT WORSEN OUTCOME
ENVIRONMENTAL MANAGEMENT TIPS • USE MAXIMUM FALLS PRECAUTIONS AND PROTECTIONS • CONSIDER PLACING THE PATIENT IN A ROOM CLOSE TO THE NURSING STATION • AVOID PLACING THE PATIENT IN BUSY, LOUD, OR CHAOTIC THERAPY ROOMS OR SETTINGS (OVERSTIMULATION) • IF THE PATIENT IS HALLUCINATING, CONSIDER ADDING CONTROLLED VISUAL STIMULI (MOVIES, SCREEN SAVERS) AND LOW TO MODERATE VOLUME MUSIC • KEEP LIGHTING ADEQUATE BOTH DAY AND NIGHT – DO NOT PLACE THE PATIENT IN THE DARK • MAKE CERTAIN HEARING AIDS, EYEGLASSES, AND OTHER DEVICES THAT ASSIST SENSORY PERCEPTION ARE USED AS MUCH AS POSSIBLE AND
MORE ENVIRONMENTAL MANAGEMENT TIPS • ADD AN EASILY-SEEN CLOCK OR CALENDAR • REORIENT IN ALL SPHERES MULTIPLE TIMES ACROSS THE DAY, PREFERABLY EACH TIME STAFF INTERACTS WITH THE PATIENT • DO NOT DIRECTLY REFUTE, ARGUE WITH, OR DENY DELUSIONS • OFFER ALTERNATIVE EXPLANATIONS AND REASSURE THE PATIENT • AS A RULE, THE SINGLE BEST ENVIRONMENTAL INTERVENTION IS ASKING SUPPORTIVE FAMILY MEMBERS OR A SUPPORTIVE FRIEND TO STAY WITH THE PATIENT
COMMON CONDITIONS: UTI • CONFUSION, COMBATIVENESS, AND PARANOIA OFTEN ONSET 48 -72 HOURS BEFORE CONFIRMATORY LABORATORY FINDINGS • DELIRIUM IS MOST COMMON COMPLICATION OF UTI • SHOULD ALWAYS BE A FIRST SUSPECT IN NEW-ONSET DELIRIUM • AFFECTS BOTH MALES AND FEMALES • FOLLOWING ONSET OF TREATMENT, DELIRIUM AND OTHER BEHAVIORAL SYMPTOMS TYPICALLY WILL BEGIN TO CLEAR (48 -72 HOURS)
COMMON CONDITIONS: PNEUMONIA • CONFUSION, STUPOR, AND DELIRIUM ARE COMMON CONSEQUENCES, ESPECIALLY IN ELDERLY PATIENTS, PATIENTS WITH KNOWN BRAIN COMPROMISE, AND INDIVIDUALS WITH MAJOR NEUROCOGNITIVE DISORDER (DEMENTIA) • LOW O 2 SATURATION ON ROOM AIR OR WITH EXERTION MAY BE PREDICTIVE OF DELIRIUM AND CONFUSION • INDIVIDUALS REQUIRING STEROIDS MAY DEVELOP ACUTE AND SEVERE PSYCHOSIS RELATED TO THESE MEDICATIONS • CONFUSED INDIVIDUALS WITH PNEUMONIA ARE OFTEN PHYSICALLY COMBATIVE DURING PERSONAL CARE, DUE TO SENSATIONS OF SMOTHERING AND THE CONFUSION ITSELF • COGNITIVE AND BEHAVIORAL SYMPTOMS TYPICALLY CLEAR AT AROUND THE SAME PACE AS THE CHEST X-RAY
• COMMON CONDITIONS: RENAL FAILURE/DIALYSIS ABNORMALITIES IN BUN AND CREATININE FREQUENTLY RESULT IN PARANOIA, WHICH MAY BE CHRONIC OR ACUTE -- THIS IS OFTEN NOT TREATABLE DUE TO RENAL STATUS • INDIVIDUALS ON REGULAR DIALYSIS, ESPECIALLY IN LATER STAGE DISEASE, WILL SHOW COGNITIVE, BEHAVIORAL AND EMOTIONAL DECOMPENSATION AS TIME FOR DIALYSIS APPROACHES • DELIRIUM IS COMMON IN RENAL FAILURE, AND CAN BECOME CHRONIC IN DIALYSIS PATIENTS • ENCEPHALOPATHY, OR GRADUAL SLOWING OF BRAIN FUNCTIONS, AT TIMES WITH SIGNIFICANT MOTOR SYMPTOMS SUCH AS TICS, MYOCLONIC JERKS, OR OTHER MOVEMENT DISORDERS IS A RELATIVELY COMMON OCCURRENCE IN LATER-STAGE RENAL DISEASE AND LONG-TERM DIALYSIS PATIENTS • END-STAGE RENAL PATIENTS ON LONG-TERM DIALYSIS WHO ASK TO STOP TREATMENT ARE NOT NECESSARILY DEPRESSED OR SUICIDAL. • IF THEY ARE COMPETENT, ASSESSMENT SHOULD CONSIDER LENGTH OF DISEASE AND ILLNESS AND REALISTIC PROGNOSIS • THIS IS FREQUENTLY AN END-OF-LIFE ISSUE, MUCH AS CANCER PATIENTS REFUSING CHEMOTHERAPY, AND SHOULD BE TREATED AS SUCH
SEIZURE DISORDER (EPILEPSY) • PRE-ICTAL (ALSO SPELLED PRE-ICTAL) IS THE PERIOD OF TIME, USUALLY RELATIVELY SHORT, BUT POSSIBLY AS MUCH AS 24 HOURS, PRIOR TO THE ONSET OF SEIZURE ACTIVITY. EEG ABNORMALITIES ARE OFTEN SEEN, BUT DO NOT RISE TO THE ICTAL LEVELS • ICTAL IS THE PERIOD OF TIME DURING WHICH EEG IS ABNORMAL AND REFLECTIVE OF SEIZURE ACTIVITY • POST-ICTAL (ALSO SPELLED POSTICTAL) IS THE PERIOD OF TIME FROM 5 -15 MINUTES (ACUTE, EEG NORMALIZATION OCCURRING) TO SEVERAL HOURS (POST-ACUTE RECOVERY, WHEN THE INDIVIDUAL IS USUALLY SLEEPING AND IRRITABLE OR CONFUSED IF ROUSED) AFTER A SEIZURE • INTER-ICTAL IS THE PERIOD OF TIME BETWEEN POSTICTAL AND PRE-ICTAL STATES
SEIZURE DISORDER GENERAL INFO • MOST INDIVIDUALS WITH A KNOWN EPILEPTIC CONDITION WILL BE UNDER THE TREATMENT OF A NEUROLOGIST OR PRIMARY CARE PHYSICIAN (PCP) AND NEVER REFERRED FOR BEHAVIORAL HEALTH CARE • PRESENCE OF SEIZURE DISORDER IS NOT PREDICTIVE OF MENTAL ILLNESS, THOUGH INCIDENCE OF MENTAL ILLNESS IS HIGHER IN INDIVIDUALS WITH EPILEPSY • DEPRESSION WITH BOTH FUNCTIONAL AND ORGANIC CAUSATION IS THE MOST COMMON ISSUE • PROVIDED SEIZURES ARE CONTROLLED, INDIVIDUALS CAN BE TREATED IN INPATIENT PSYCHIATRIC SETTINGS IF NECESSARY—FOR EMOTIONAL ISSUES, NOT FOR THE SEIZURES THEMSELVES • INDIVIDUALS WITH UNTREATED OR POORLY TREATED SEIZURES OFTEN BEHAVE IN A CONFUSED, IMPULSIVE, OR DISORGANIZED FASHION DURING PRE-
SEIZURE DISORDER POTENTIAL ISSUES • INDIVIDUALS WITH TRUE POST-ICTAL DELIRIUM ARE RARE; HOWEVER, INDIVIDUALS DO STOP TREATMENT, OR UNFORTUNATELY, MAY NOT BE ABLE TO AFFORD TREATMENT • INDIVIDUALS WITH POST-ICTAL DELIRIUM CAN PRESENT SIGNIFICANT DANGER TO THEMSELVES OR OTHERS DUE TO EXTREME CONFUSION AND CONFUSION-RELATED VIOLENCE • VIOLENCE IS TYPICALLY UNPROVOKED, SUDDEN AND EXTREME, AND IS USUALLY PRECEDED BY RAPID PUPILLARY DILATION • POST-ICTAL DELIRIUM CAN ALSO BE ASSOCIATED WITH MASSIVE AND COMPLEX VISUAL HALLUCINATIONS • INDIVIDUALS WITH UNCONTROLLED OR POORLY CONTROLLED SEIZURES ARE NOT APPROPRIATELY FOR INPATIENT PSYCHIATRIC HOSPITALIZATION, EVEN IF THE ABOVEDESCRIBED DANGEROUS SYMPTOMS ARE OCCURRING. THIS IS A LIFE-THREATENING SITUATION, BOTH DUE TO THE BEHAVIORAL FACTORS AND THE RISK FROM THE SEIZURES THEMSELVES. • LOCKED SEIZURE UNITS ARE AVAILABLE AT MANY MAJOR MEDICAL CENTERS IF

OVER 40 TYPES OF SEIZURES This is a seizure (Complex Partial). Simple Partial seizures can look like tics. Absence seizures are easy to miss. Many seizures, like this Myoclonic Absence seizure, happen so fast people never notice.
COMPLEX-PARTIAL SEIZURES • ALSO CALLED PARTIAL COMPLEX • OLDER OR RELATED TERMS: PSYCHOMOTOR SEIZURE OR TEMPORAL LOBE EPILEPSY • USUALLY BEGIN BETWEEN LATE CHILDHOOD AND EARLY THIRTIES • CAN ONSET FOLLOWING BRAIN TRAUMA AT ANY AGE • OCCUR IN 65% OF INDIVIDUALS WITH EPILEPSY • MORE LIKELY TO BE REFERRED TO A BEHAVIORAL HEALTH PROFESSION FOR TREATMENT

COMPLEX PARTIAL SEIZURES • A SMALL PERCENTAGE OF INDIVIDUALS DEVELOP INTER-ICTAL PSYCHOTIC STATES AND THIS MOST OFTEN OCCURS WHEN SEIZURES ARE POORLY CONTROLLED • INDIVIDUALS WHO EXPERIENCE HALLUCINATIONS ONLY DURING PRE-ICTAL, OR POST-ICTAL STATES DO NOT NECESSARILY HAVE PSYCHIATRIC DISORDER, AND IN FACT, MOST DO NOT • INDIVIDUALS IN COMPLEX PARTIAL ICTAL STATES CAN ENGAGE IN SIMPLE ACTIVITIES SUCH AS STANDING, WALKING, PACING AND DRIVING • INDIVIDUALS IN ICTAL STATES CAN RESPOND VERBALLY WITH SIMPLISTIC OR TELEGRAPHIC ANSWERS, OFTEN ACCURATELY. • MANY INDIVIDUALS EXPERIENCE ABDOMINAL SENSATIONS PRIOR TO SEIZURE, AND MAY MAKE CONFUSIONAL COMPLAINTS OF SNAKES OR OTHER ANIMALS IN THEIR STOMACH • ICTAL SEX, OR COMPLETE SEXUAL ACTS WHILE IN AN ICTAL STATE, WHILE POPULAR IN MOVIES AND LITERATURE, IS EXCEEDINGLY RARE • ICTAL VIOLENCE IS EXCEEDINGLY RARE
SOURCES OF INFORMATION FOR SEIZURE DISORDER SECTION • KAUFMAN, DAVID (1990). CLINICAL NEUROLOGY FOR PSYCHIATRISTS, 3 RD EDITION. PHILADELPHIA: HARCOURT BRACE JOVANOVICH • NIEDERMEYER, ERNST (1990). THE EPILEPSIES: DIAGNOSIS AND MANAGEMENT. BALTIMORE: URBAN & SCHWARZENBERG
END-STAGE ORGAN FAILURE • INDIVIDUALS WITH END-STAGE ORGAN FAILURE, OR ANY END-STATE MEDICAL ILLNESS, MAY NOT BE APPROPRIATE FOR INPATIENT PSYCHIATRIC ADMISSION • CARDIAC DISEASE • INDIVIDUALS WITH END-STAGE CARDIAC DISEASE ARE FREQUENTLY SHORT OF BREATH, DELIRIOUS, CONFUSED, AND COMBATIVE • DEMENTIA IS OFTEN PRESENT • LUCID PATIENTS WITH END-STAGE CARDIAC DISEASE OFTEN STATE A WISH TO DIE DUE TO MARKED LIFE LIMITATIONS • PULMONARY DISEASE • INDIVIDUALS WITH END-STAGE LUNG DISEASE FREQUENTLY SHOW PSYCHOSIS, PROLONGED PANIC, AND INCREASING DELIRIUM, STUPOR, AND COGNITIVE DEFICITS • LUCID PATIENTS WITH END-STAGE PULMONARY DISEASE OFTEN EXPRESS A WISH TO DIE, OR FOR THE SENSATIONS TO STOP AT ANY COST

END-STAGE ORGAN FAILURE • HEPATIC DISEASE • INDIVIDUALS WITH END-STAGE LIVER DISEASE OFTEN SHOW: • MARKED DELIRIUM; • INTERMITTENT COMA; • SEVERE COMBATIVENESS WHEN AWAKE; • MOVEMENT DISORDER • ASTERIXIS OR FLAPPING OF THE WRISTS/HANDS USUALLY ACCOMPANIED BY SHORT ARRHYTHMIC LOSSES OF VOLUNTARY MUSCLE CONTRACTIONS ); AND • ASSOCIATED SHORT, QUICK LAPSES OF POSTURE • EVEN WHEN AWAKE, THESE INDIVIDUALS CAN BE EVALUATED WITH THE GLASGOW COMA SCALE
END OF LIFE AGITATION • END OF LIFE AGITATION: • CONFUSIONAL AND DELIRIOUS STATES THAT OCCUR AS AN INDIVIDUAL APPROACHES DEATH • SENSITIVE ISSUE FOR BOTH PHYSICIANS AND FAMILIES • MANY FAMILIES AND MEDICAL PROFESSIONALS PREFER NOT TO DISCUSS OR ADDRESS THESE ISSUES • MANY NURSING FACILITIES FAIL TO RECOGNIZE THE DIFFERENCE BETWEEN EVOLVING BEHAVIORAL AND PSYCHIATRIC DISORDERS AND THE ONSET OF END OF LIFE AGITATION • REFERRALS FOR INPATIENT CARE MAY BE BASED IN DENIAL, LACK OF KNOWLEDGE, OR UNCERTAINTY ABOUT THE INDIVIDUAL’S STATUS
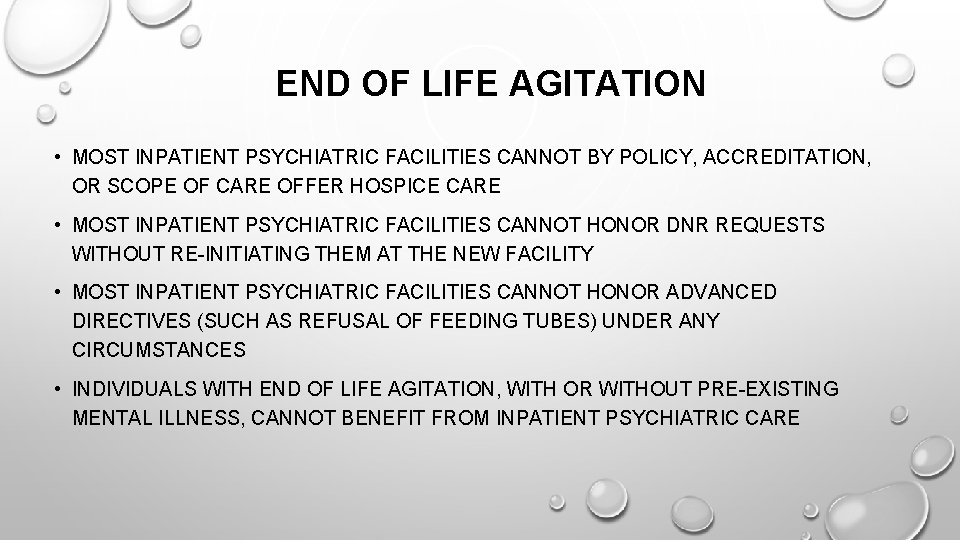
END OF LIFE AGITATION • MOST INPATIENT PSYCHIATRIC FACILITIES CANNOT BY POLICY, ACCREDITATION, OR SCOPE OF CARE OFFER HOSPICE CARE • MOST INPATIENT PSYCHIATRIC FACILITIES CANNOT HONOR DNR REQUESTS WITHOUT RE-INITIATING THEM AT THE NEW FACILITY • MOST INPATIENT PSYCHIATRIC FACILITIES CANNOT HONOR ADVANCED DIRECTIVES (SUCH AS REFUSAL OF FEEDING TUBES) UNDER ANY CIRCUMSTANCES • INDIVIDUALS WITH END OF LIFE AGITATION, WITH OR WITHOUT PRE-EXISTING MENTAL ILLNESS, CANNOT BENEFIT FROM INPATIENT PSYCHIATRIC CARE
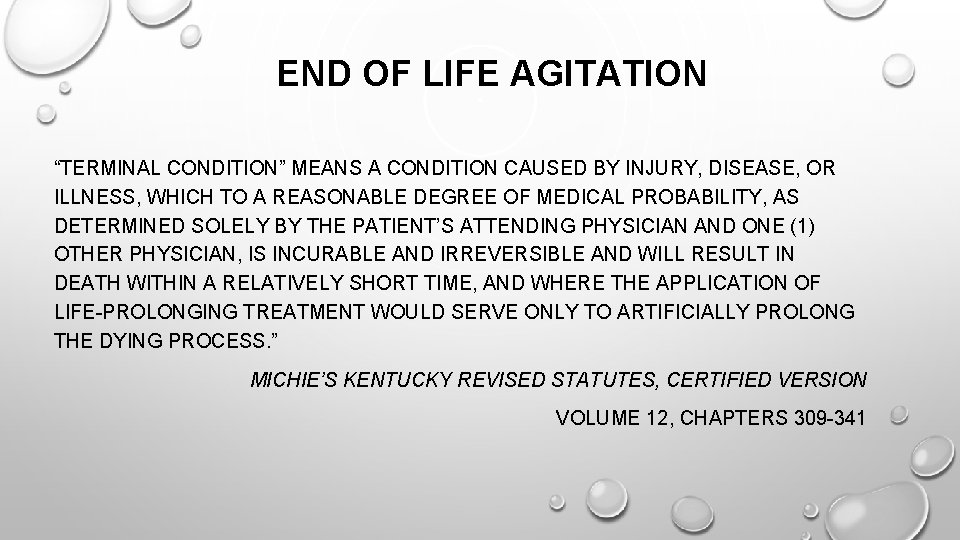
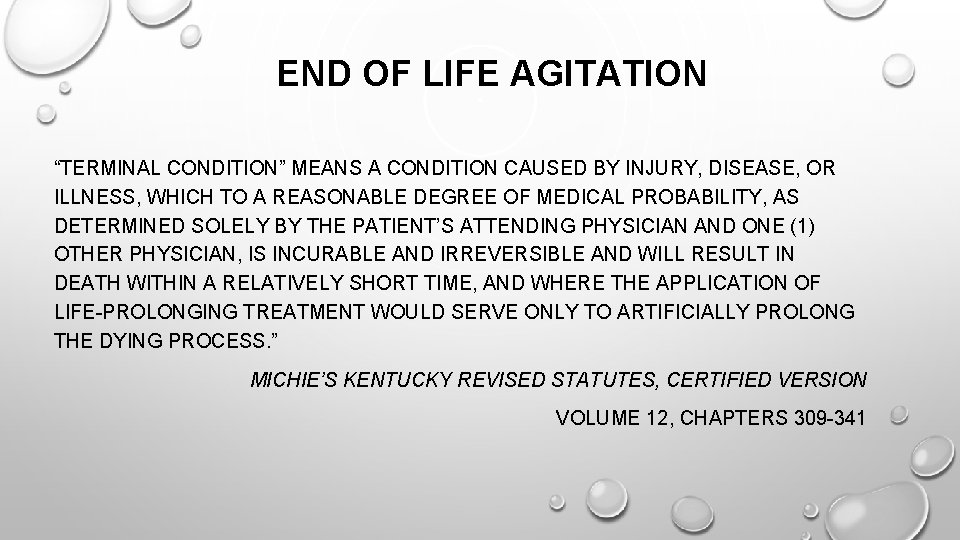
END OF LIFE AGITATION “TERMINAL CONDITION” MEANS A CONDITION CAUSED BY INJURY, DISEASE, OR ILLNESS, WHICH TO A REASONABLE DEGREE OF MEDICAL PROBABILITY, AS DETERMINED SOLELY BY THE PATIENT’S ATTENDING PHYSICIAN AND ONE (1) OTHER PHYSICIAN, IS INCURABLE AND IRREVERSIBLE AND WILL RESULT IN DEATH WITHIN A RELATIVELY SHORT TIME, AND WHERE THE APPLICATION OF LIFE-PROLONGING TREATMENT WOULD SERVE ONLY TO ARTIFICIALLY PROLONG THE DYING PROCESS. ” MICHIE’S KENTUCKY REVISED STATUTES, CERTIFIED VERSION VOLUME 12, CHAPTERS 309 -341
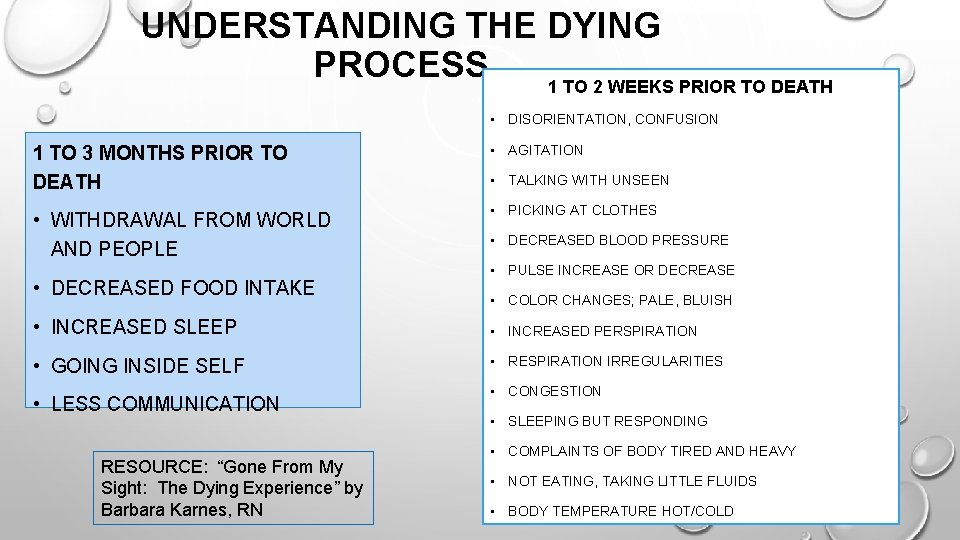
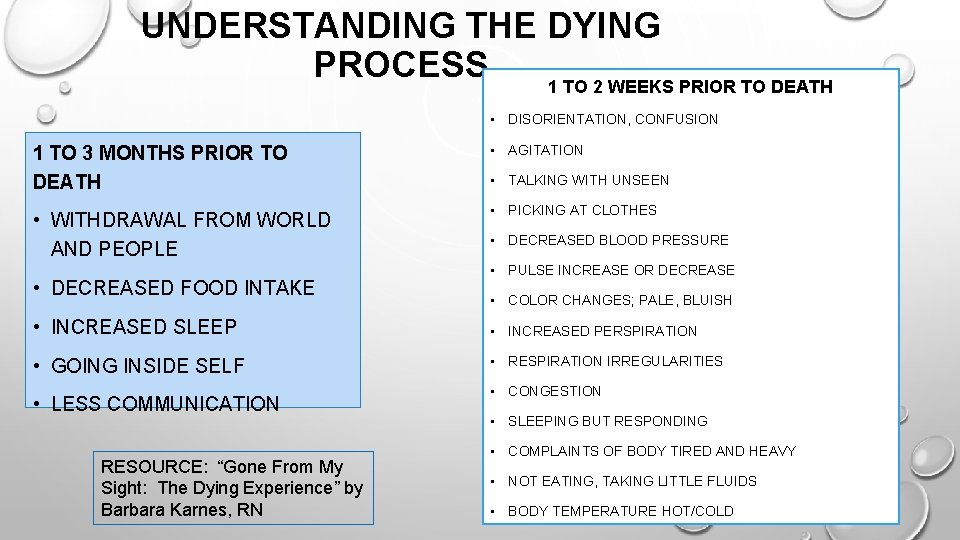
UNDERSTANDING THE DYING PROCESS 1 TO 2 WEEKS PRIOR TO DEATH • DISORIENTATION, CONFUSION 1 TO 3 MONTHS PRIOR TO DEATH • AGITATION • WITHDRAWAL FROM WORLD AND PEOPLE • PICKING AT CLOTHES • DECREASED FOOD INTAKE • TALKING WITH UNSEEN • DECREASED BLOOD PRESSURE • PULSE INCREASE OR DECREASE • COLOR CHANGES; PALE, BLUISH • INCREASED SLEEP • INCREASED PERSPIRATION • GOING INSIDE SELF • RESPIRATION IRREGULARITIES • LESS COMMUNICATION RESOURCE: “Gone From My Sight: The Dying Experience” by Barbara Karnes, RN • CONGESTION • SLEEPING BUT RESPONDING • COMPLAINTS OF BODY TIRED AND HEAVY • NOT EATING, TAKING LITTLE FLUIDS • BODY TEMPERATURE HOT/COLD
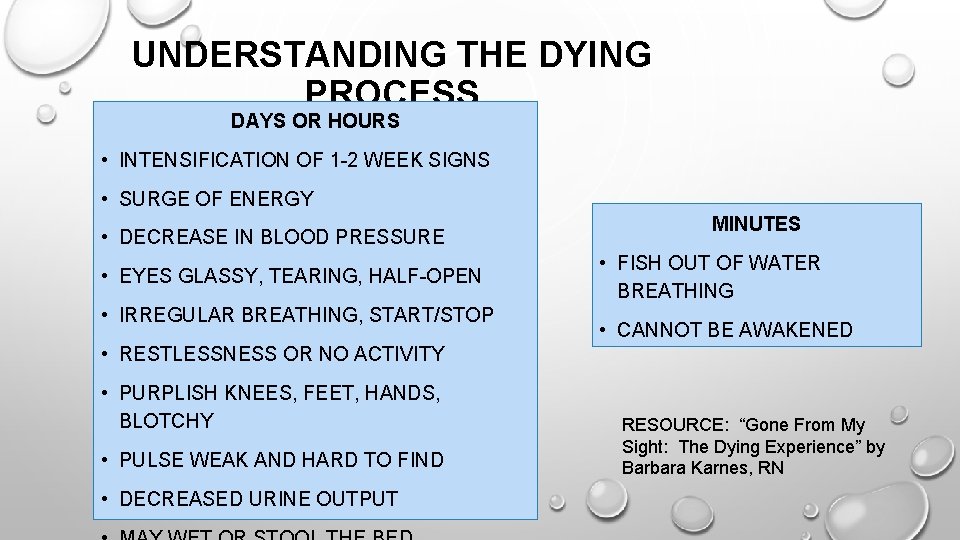
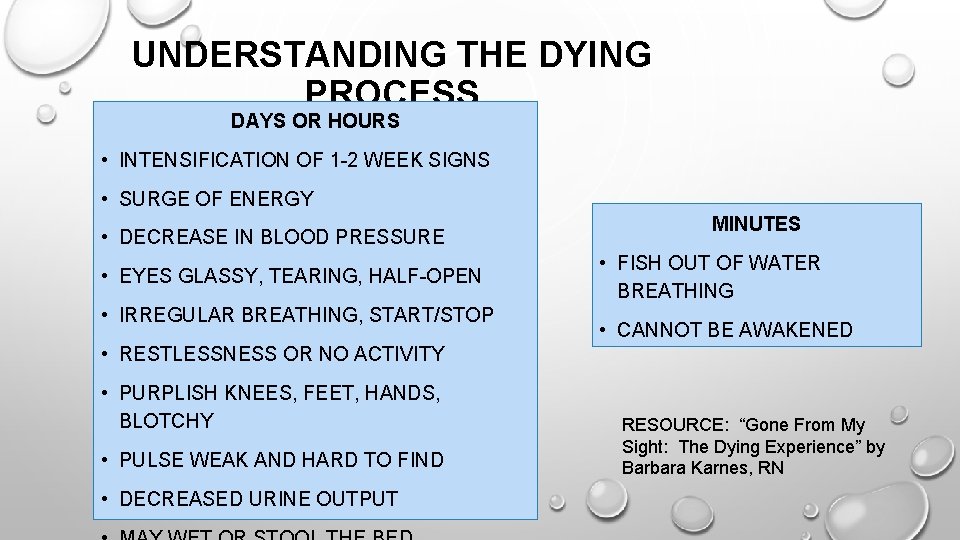
UNDERSTANDING THE DYING PROCESS DAYS OR HOURS • INTENSIFICATION OF 1 -2 WEEK SIGNS • SURGE OF ENERGY • DECREASE IN BLOOD PRESSURE • EYES GLASSY, TEARING, HALF-OPEN • IRREGULAR BREATHING, START/STOP MINUTES • FISH OUT OF WATER BREATHING • CANNOT BE AWAKENED • RESTLESSNESS OR NO ACTIVITY • PURPLISH KNEES, FEET, HANDS, BLOTCHY • PULSE WEAK AND HARD TO FIND • DECREASED URINE OUTPUT RESOURCE: “Gone From My Sight: The Dying Experience” by Barbara Karnes, RN

THE LAST STAGES OF LIFE • MANY PHYSICAL CHANGES OCCUR DURING THE PROCESS OF DYING THAT AFFECT THE EMOTIONAL, SOCIAL, AND SPIRITUAL ASPECTS OF AN INDIVIDUAL’S LIFE. • THERE ARE SOME SIGNS AND SYMPTOMS OF DYING THAT ARE OBSERVABLE, ALTHOUGH NOT EVERYONE FOLLOWS A PREDICTABLE SEQUENCE OF EVENTS OR STAGES • HEALTH PROFESSIONALS SPEAK OF “DYING TRAJECTORIES” THAT SUGGEST HOW INDIVIDUALS WITH SPECIFIC DISEASES WILL DIE: • THOSE WITH A TERMINAL ILLNESS, SUCH AS ADVANCED CANCER, WILL SHOW A STEADY DECLINE TOWARD DEATH • THOSE WITH SERIOUS CHRONIC ILLNESSES MAY HAVE PEAKS AND VALLEYS THAT SOMETIMES GIVE THE IMPRESSION OF RECOVERY SOURCE: http: //kokuamau. org/resources/last-stages-life • REMEMBER EACH INDIVIDUAL’S DEATH IS UNIQUE
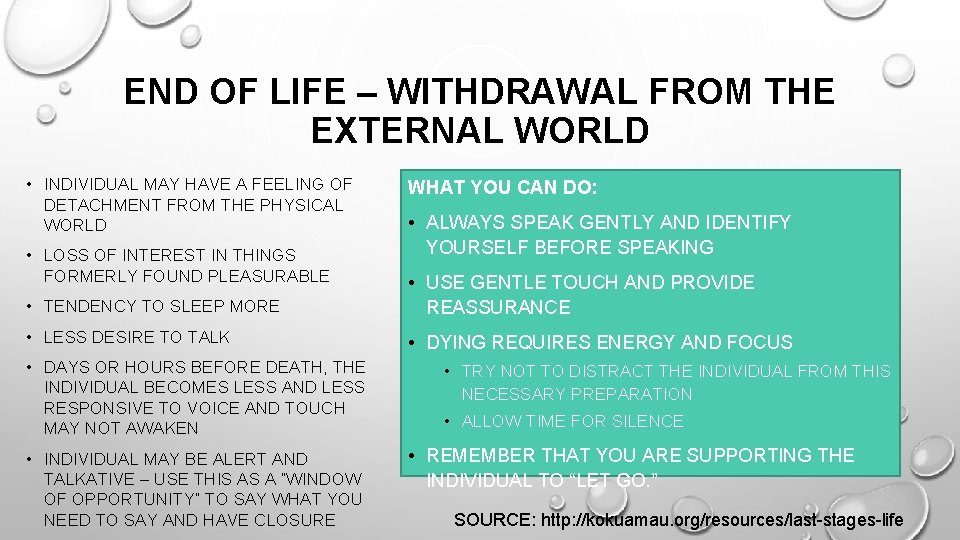
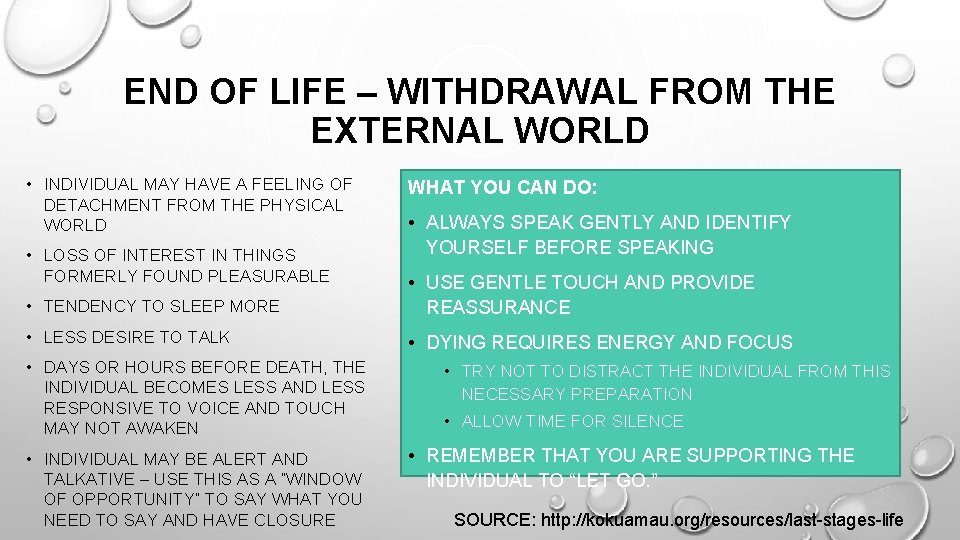
END OF LIFE – WITHDRAWAL FROM THE EXTERNAL WORLD • INDIVIDUAL MAY HAVE A FEELING OF DETACHMENT FROM THE PHYSICAL WORLD • LOSS OF INTEREST IN THINGS FORMERLY FOUND PLEASURABLE WHAT YOU CAN DO: • ALWAYS SPEAK GENTLY AND IDENTIFY YOURSELF BEFORE SPEAKING • TENDENCY TO SLEEP MORE • USE GENTLE TOUCH AND PROVIDE REASSURANCE • LESS DESIRE TO TALK • DYING REQUIRES ENERGY AND FOCUS • DAYS OR HOURS BEFORE DEATH, THE INDIVIDUAL BECOMES LESS AND LESS RESPONSIVE TO VOICE AND TOUCH MAY NOT AWAKEN • INDIVIDUAL MAY BE ALERT AND TALKATIVE – USE THIS AS A “WINDOW OF OPPORTUNITY” TO SAY WHAT YOU NEED TO SAY AND HAVE CLOSURE • TRY NOT TO DISTRACT THE INDIVIDUAL FROM THIS NECESSARY PREPARATION • ALLOW TIME FOR SILENCE • REMEMBER THAT YOU ARE SUPPORTING THE INDIVIDUAL TO “LET GO. ” SOURCE: http: //kokuamau. org/resources/last-stages-life
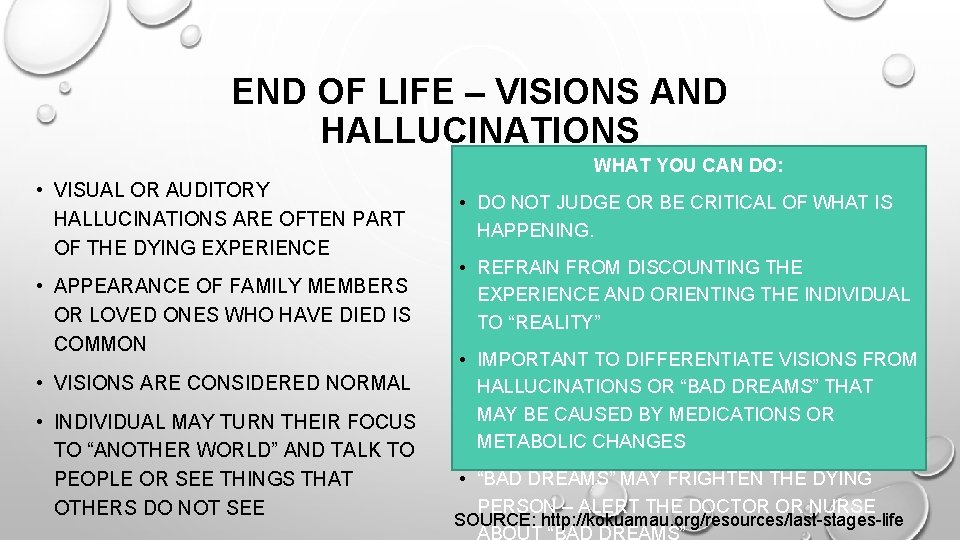
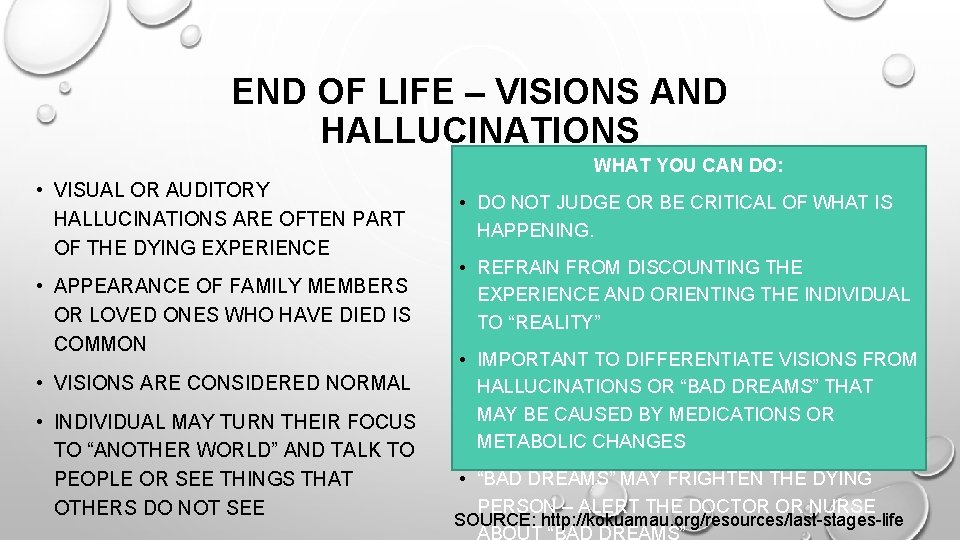
END OF LIFE – VISIONS AND HALLUCINATIONS WHAT YOU CAN DO: • VISUAL OR AUDITORY HALLUCINATIONS ARE OFTEN PART OF THE DYING EXPERIENCE • APPEARANCE OF FAMILY MEMBERS OR LOVED ONES WHO HAVE DIED IS COMMON • VISIONS ARE CONSIDERED NORMAL • INDIVIDUAL MAY TURN THEIR FOCUS TO “ANOTHER WORLD” AND TALK TO PEOPLE OR SEE THINGS THAT OTHERS DO NOT SEE • DO NOT JUDGE OR BE CRITICAL OF WHAT IS HAPPENING. • REFRAIN FROM DISCOUNTING THE EXPERIENCE AND ORIENTING THE INDIVIDUAL TO “REALITY” • IMPORTANT TO DIFFERENTIATE VISIONS FROM HALLUCINATIONS OR “BAD DREAMS” THAT MAY BE CAUSED BY MEDICATIONS OR METABOLIC CHANGES • “BAD DREAMS” MAY FRIGHTEN THE DYING PERSON – ALERT THE DOCTOR OR NURSE SOURCE: http: //kokuamau. org/resources/last-stages-life
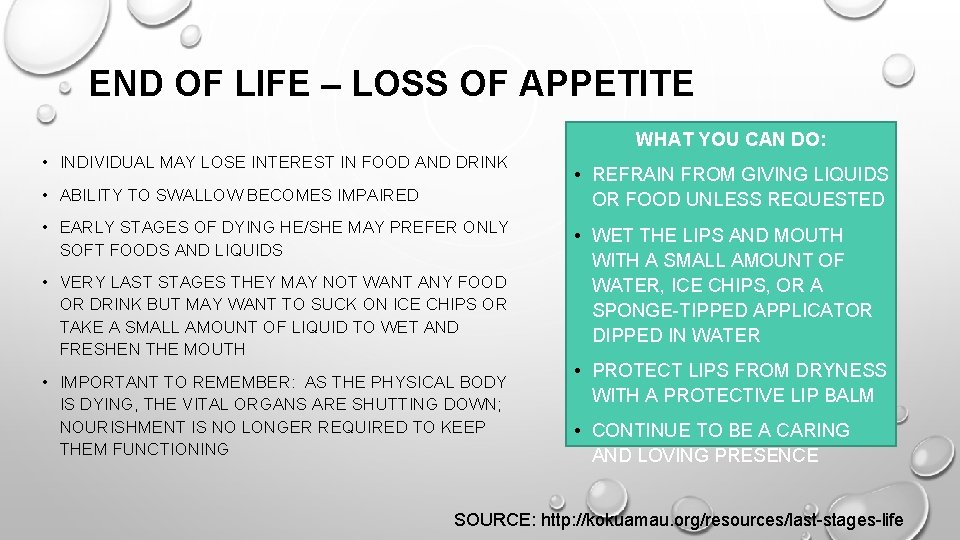
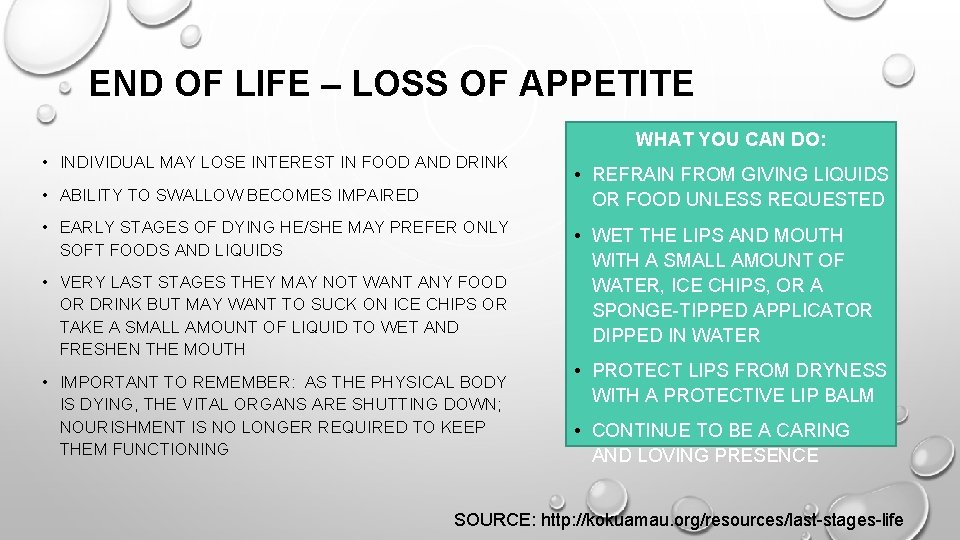
END OF LIFE – LOSS OF APPETITE WHAT YOU CAN DO: • INDIVIDUAL MAY LOSE INTEREST IN FOOD AND DRINK • ABILITY TO SWALLOW BECOMES IMPAIRED • EARLY STAGES OF DYING HE/SHE MAY PREFER ONLY SOFT FOODS AND LIQUIDS • VERY LAST STAGES THEY MAY NOT WANT ANY FOOD OR DRINK BUT MAY WANT TO SUCK ON ICE CHIPS OR TAKE A SMALL AMOUNT OF LIQUID TO WET AND FRESHEN THE MOUTH • IMPORTANT TO REMEMBER: AS THE PHYSICAL BODY IS DYING, THE VITAL ORGANS ARE SHUTTING DOWN; NOURISHMENT IS NO LONGER REQUIRED TO KEEP THEM FUNCTIONING • REFRAIN FROM GIVING LIQUIDS OR FOOD UNLESS REQUESTED • WET THE LIPS AND MOUTH WITH A SMALL AMOUNT OF WATER, ICE CHIPS, OR A SPONGE-TIPPED APPLICATOR DIPPED IN WATER • PROTECT LIPS FROM DRYNESS WITH A PROTECTIVE LIP BALM • CONTINUE TO BE A CARING AND LOVING PRESENCE SOURCE: http: //kokuamau. org/resources/last-stages-life
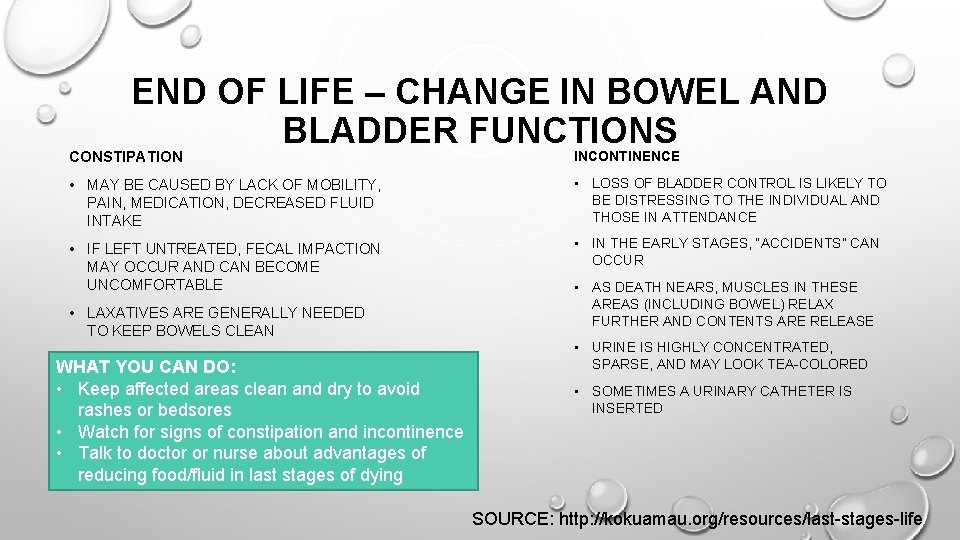
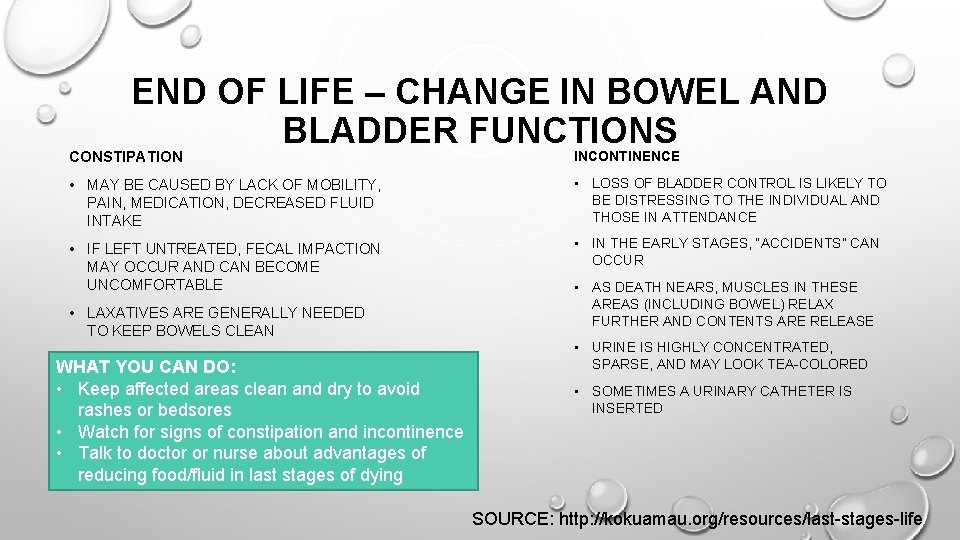
END OF LIFE – CHANGE IN BOWEL AND BLADDER FUNCTIONS CONSTIPATION INCONTINENCE • MAY BE CAUSED BY LACK OF MOBILITY, PAIN, MEDICATION, DECREASED FLUID INTAKE • LOSS OF BLADDER CONTROL IS LIKELY TO BE DISTRESSING TO THE INDIVIDUAL AND THOSE IN ATTENDANCE • IF LEFT UNTREATED, FECAL IMPACTION MAY OCCUR AND CAN BECOME UNCOMFORTABLE • IN THE EARLY STAGES, “ACCIDENTS” CAN OCCUR • LAXATIVES ARE GENERALLY NEEDED TO KEEP BOWELS CLEAN WHAT YOU CAN DO: • Keep affected areas clean and dry to avoid rashes or bedsores • Watch for signs of constipation and incontinence • Talk to doctor or nurse about advantages of reducing food/fluid in last stages of dying • AS DEATH NEARS, MUSCLES IN THESE AREAS (INCLUDING BOWEL) RELAX FURTHER AND CONTENTS ARE RELEASE • URINE IS HIGHLY CONCENTRATED, SPARSE, AND MAY LOOK TEA-COLORED • SOMETIMES A URINARY CATHETER IS INSERTED SOURCE: http: //kokuamau. org/resources/last-stages-life
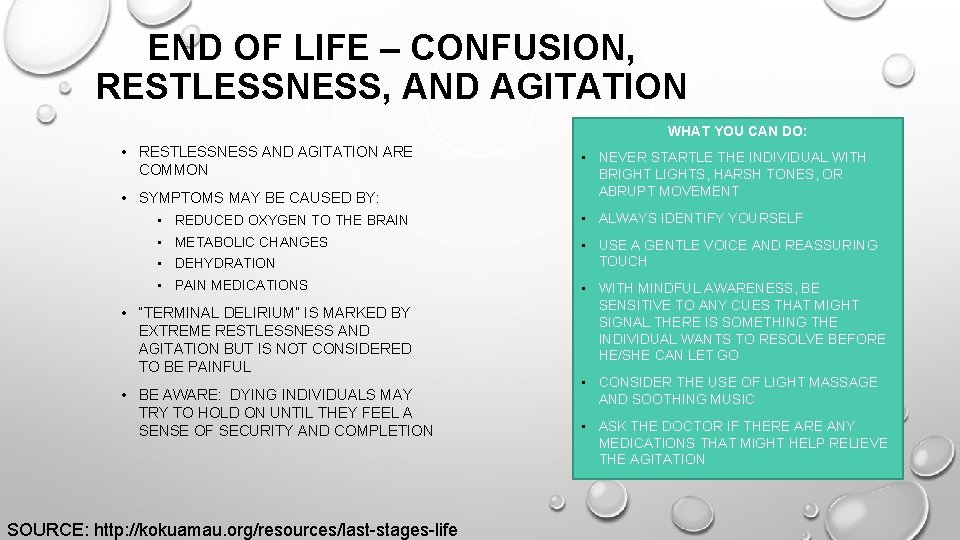
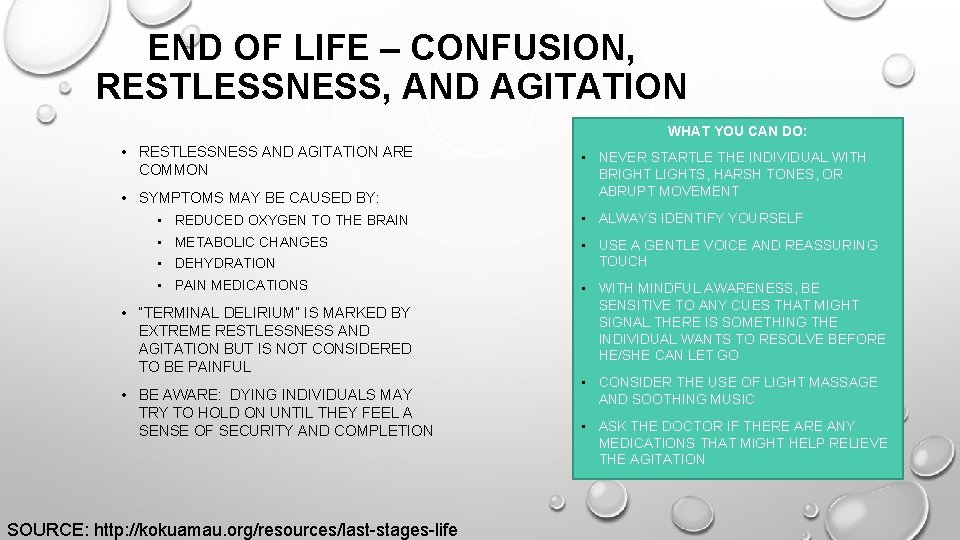
END OF LIFE – CONFUSION, RESTLESSNESS, AND AGITATION WHAT YOU CAN DO: • RESTLESSNESS AND AGITATION ARE COMMON • SYMPTOMS MAY BE CAUSED BY: • NEVER STARTLE THE INDIVIDUAL WITH BRIGHT LIGHTS, HARSH TONES, OR ABRUPT MOVEMENT • REDUCED OXYGEN TO THE BRAIN • ALWAYS IDENTIFY YOURSELF • METABOLIC CHANGES • USE A GENTLE VOICE AND REASSURING TOUCH • DEHYDRATION • PAIN MEDICATIONS • “TERMINAL DELIRIUM” IS MARKED BY EXTREME RESTLESSNESS AND AGITATION BUT IS NOT CONSIDERED TO BE PAINFUL • BE AWARE: DYING INDIVIDUALS MAY TRY TO HOLD ON UNTIL THEY FEEL A SENSE OF SECURITY AND COMPLETION SOURCE: http: //kokuamau. org/resources/last-stages-life • WITH MINDFUL AWARENESS, BE SENSITIVE TO ANY CUES THAT MIGHT SIGNAL THERE IS SOMETHING THE INDIVIDUAL WANTS TO RESOLVE BEFORE HE/SHE CAN LET GO • CONSIDER THE USE OF LIGHT MASSAGE AND SOOTHING MUSIC • ASK THE DOCTOR IF THERE ANY MEDICATIONS THAT MIGHT HELP RELIEVE THE AGITATION
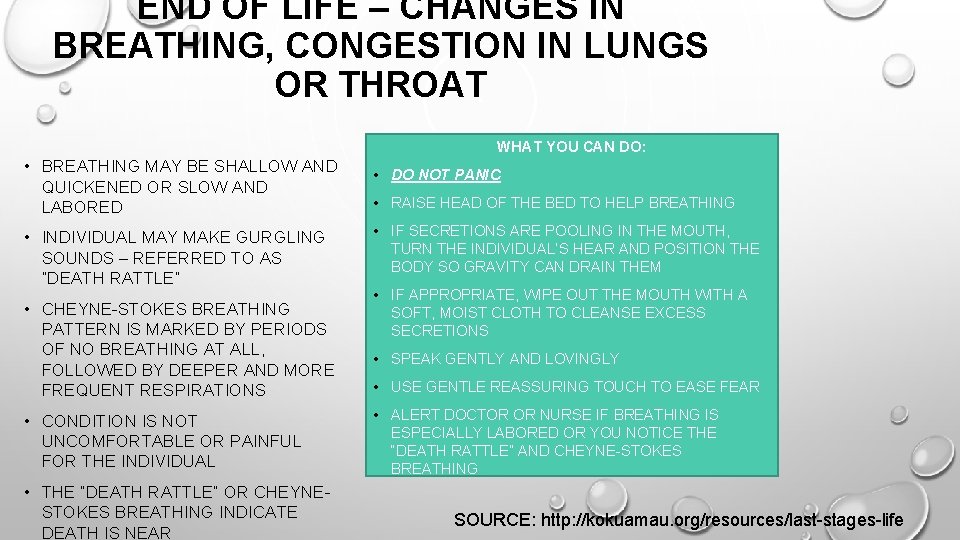
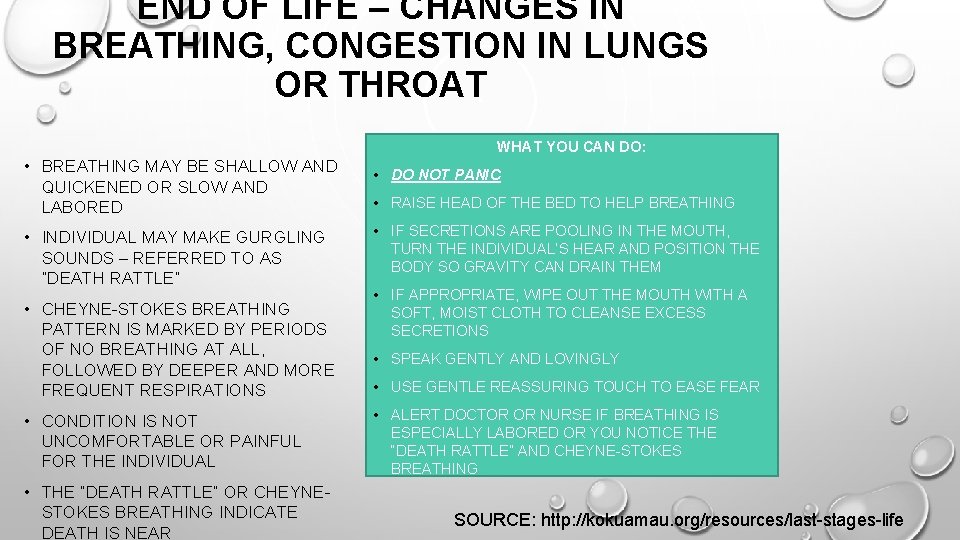
END OF LIFE – CHANGES IN BREATHING, CONGESTION IN LUNGS OR THROAT WHAT YOU CAN DO: • BREATHING MAY BE SHALLOW AND QUICKENED OR SLOW AND LABORED • INDIVIDUAL MAY MAKE GURGLING SOUNDS – REFERRED TO AS “DEATH RATTLE” • CHEYNE-STOKES BREATHING PATTERN IS MARKED BY PERIODS OF NO BREATHING AT ALL, FOLLOWED BY DEEPER AND MORE FREQUENT RESPIRATIONS • CONDITION IS NOT UNCOMFORTABLE OR PAINFUL FOR THE INDIVIDUAL • THE “DEATH RATTLE” OR CHEYNESTOKES BREATHING INDICATE DEATH IS NEAR • DO NOT PANIC • RAISE HEAD OF THE BED TO HELP BREATHING • IF SECRETIONS ARE POOLING IN THE MOUTH, TURN THE INDIVIDUAL’S HEAR AND POSITION THE BODY SO GRAVITY CAN DRAIN THEM • IF APPROPRIATE, WIPE OUT THE MOUTH WITH A SOFT, MOIST CLOTH TO CLEANSE EXCESS SECRETIONS • SPEAK GENTLY AND LOVINGLY • USE GENTLE REASSURING TOUCH TO EASE FEAR • ALERT DOCTOR OR NURSE IF BREATHING IS ESPECIALLY LABORED OR YOU NOTICE THE “DEATH RATTLE” AND CHEYNE-STOKES BREATHING SOURCE: http: //kokuamau. org/resources/last-stages-life

END OF LIFE – CHANGE IN SKIN TEMPERATURE AND COLOR WHAT YOU CAN DO • TRY TO KEEP THE INDIVIDUAL AS COMFORTABLE AS POSSIBLE • USE A DAMP, COOL WASHCLOTH TO COOL A PERSON WHO FEELS TOO HOT • COVER THE INDIVIDUAL WITH A BLANKET IF HE/SHE FEELS TOO COLD • ALERT THE DOCTOR/NURSE IF NOTICE CHANGES IN SKIN COLOR • USE A FAN TO CIRCULATE AIR MAY MAKE INDIVIDUAL MORE • AS THE BODY DIES, THE BLOOD MOVES AWAY FROM THE EXTREMITIES TOWARD THE VITAL ORGANS • EXTREMITIES MAY BE COOL WHILE ABDOMEN IS WARM • INDIVIDUAL MAY FEEL HOT ONE MINUTE AND COLD THE NEXT • AS DEATH APPROACHES, THERE MAY BE HIGH FEVER • MAY ALSO SEE PURPLISH-BLUISH BLOTCHES AND MOTTLING ON LEGS, ARMS, OR UNDERSIDE OF BODY • AS DEATH NEARS, THE BODY MAY APPEAR YELLOWISH OR WAXEN IN COLOR SOURCE: http: //kokuamau. org/resources/last-stages-life
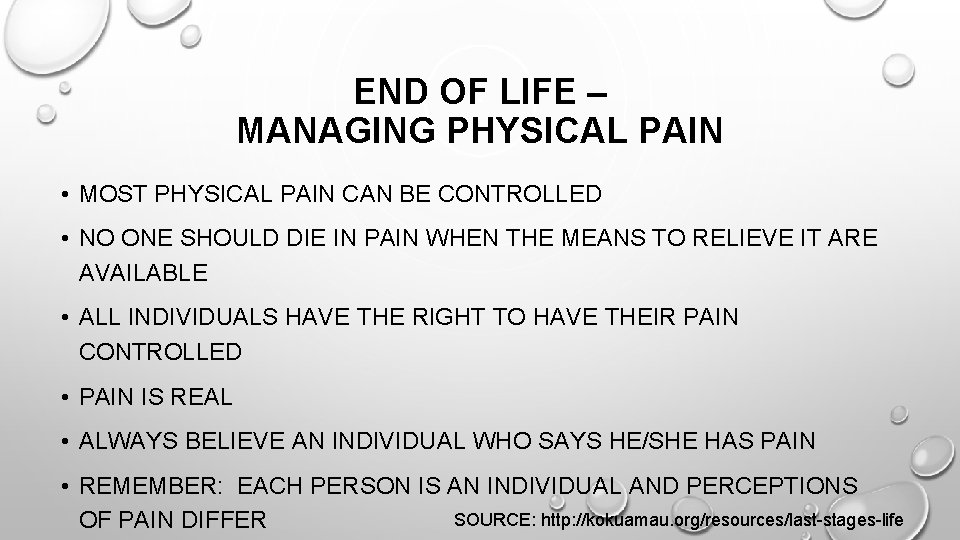
END OF LIFE – MANAGING PHYSICAL PAIN • MOST PHYSICAL PAIN CAN BE CONTROLLED • NO ONE SHOULD DIE IN PAIN WHEN THE MEANS TO RELIEVE IT ARE AVAILABLE • ALL INDIVIDUALS HAVE THE RIGHT TO HAVE THEIR PAIN CONTROLLED • PAIN IS REAL • ALWAYS BELIEVE AN INDIVIDUAL WHO SAYS HE/SHE HAS PAIN • REMEMBER: EACH PERSON IS AN INDIVIDUAL AND PERCEPTIONS SOURCE: http: //kokuamau. org/resources/last-stages-life OF PAIN DIFFER
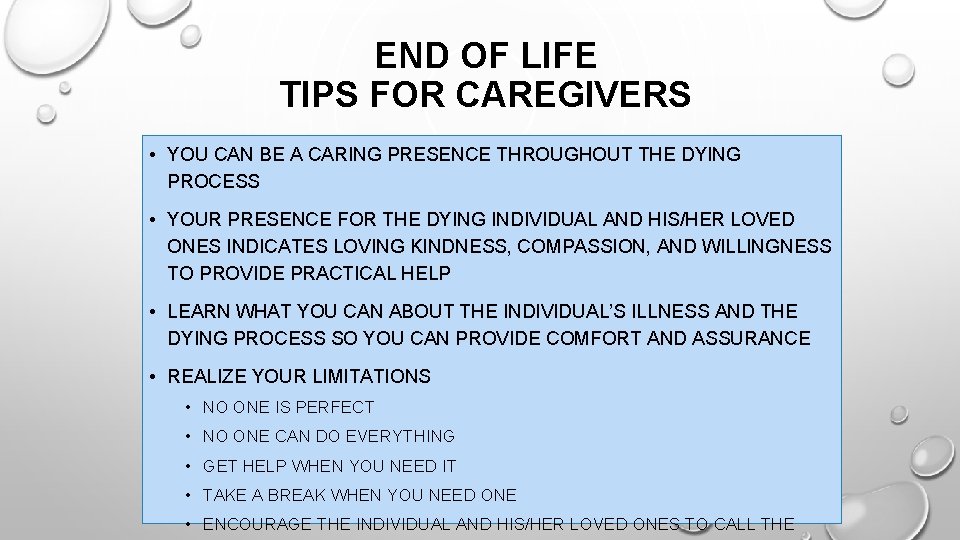
END OF LIFE TIPS FOR CAREGIVERS • YOU CAN BE A CARING PRESENCE THROUGHOUT THE DYING PROCESS • YOUR PRESENCE FOR THE DYING INDIVIDUAL AND HIS/HER LOVED ONES INDICATES LOVING KINDNESS, COMPASSION, AND WILLINGNESS TO PROVIDE PRACTICAL HELP • LEARN WHAT YOU CAN ABOUT THE INDIVIDUAL’S ILLNESS AND THE DYING PROCESS SO YOU CAN PROVIDE COMFORT AND ASSURANCE • REALIZE YOUR LIMITATIONS • NO ONE IS PERFECT • NO ONE CAN DO EVERYTHING • GET HELP WHEN YOU NEED IT • TAKE A BREAK WHEN YOU NEED ONE • ENCOURAGE THE INDIVIDUAL AND HIS/HER LOVED ONES TO CALL THE

“SAYING GOODBYE” INDIVIDUALS WHO ARE DYING OFTEN WANT “PERMISSION TO DIE” FROM THOSE THEY LOVE. OFTEN, THEY WANT TO BE ASSURED OF FIVE THINGS: • THINGS THEY WERE ONCE RESPONSIBLE FOR WILL BE TAKEN CARE OF. • THE SURVIVORS WILL SURVIVE WITHOUT THEM. • ALL IS FORGIVEN. • THEIR LIFE HAD MEANING. • THEY WILL BE REMEMBERED. SOURCE: http: //kokuamau. org/resources/last-stages-life
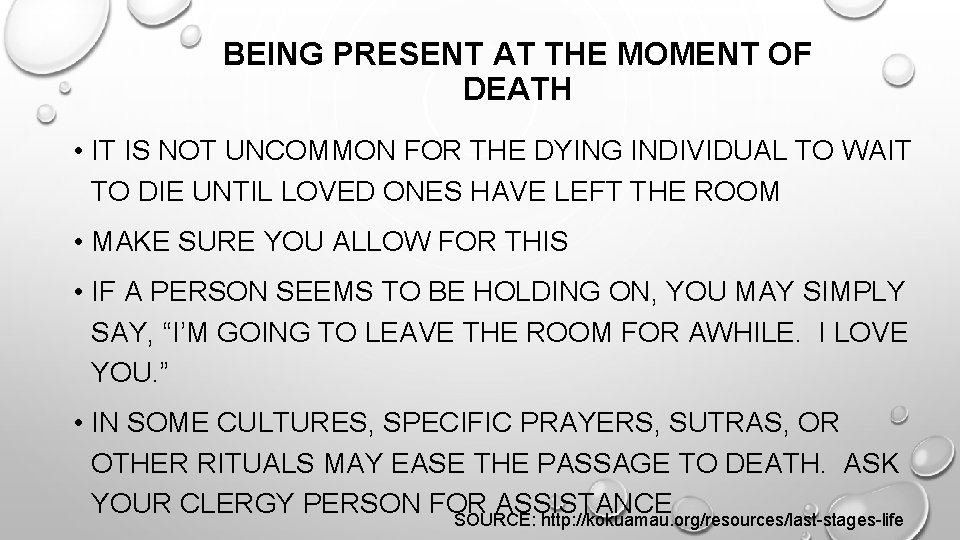
BEING PRESENT AT THE MOMENT OF DEATH • IT IS NOT UNCOMMON FOR THE DYING INDIVIDUAL TO WAIT TO DIE UNTIL LOVED ONES HAVE LEFT THE ROOM • MAKE SURE YOU ALLOW FOR THIS • IF A PERSON SEEMS TO BE HOLDING ON, YOU MAY SIMPLY SAY, “I’M GOING TO LEAVE THE ROOM FOR AWHILE. I LOVE YOU. ” • IN SOME CULTURES, SPECIFIC PRAYERS, SUTRAS, OR OTHER RITUALS MAY EASE THE PASSAGE TO DEATH. ASK YOUR CLERGY PERSON FOR ASSISTANCE SOURCE: http: //kokuamau. org/resources/last-stages-life
AFTERCARE FOR YOURSELF AND OTHERS • FOLLOWING THE DEATH OF A PERSON YOU SUPPORT, IT IS NORMAL TO GRIEVE. ALLOW YOURSELF TO REST AND GRIEVE IN THE WAYS HEALTHIEST FOR YOU. • YOUR AGENCY MAY WISH TO CONSIDER A TIME-LIMITED GRIEF SUPPORT GROUP, OR A FEW SESSIONS OF DEBRIEFING. • IF CARE STAFF CANNOT BE INVOLVED IN FUNERAL OR MEMORIAL SERVICES, IT MAY BE USEFUL TO HAVE A PRIVATE MEMORIAL OR CELEBRATION OF LIFE.
DEATH AND DYING: CONCLUSION • DYING IS A NATURAL PART OF ANY LIFE, AND YOU MAY SUPPORT PEOPLE IN CARE SETTINGS AND HOME SETTINGS DURING THEIR DYING PROCESS. • YOUR GENTLENESS AND CARING DURING THESE LAST MONTHS, WEEKS, DAYS, AND MOMENTS OF LIFE IS A GIFT TO THE PERSON SUPPORTED, AND CAN ALSO BE A GIFT TO YOU. • EDUCATING YOURSELF AND OTHERS IN THE CARE ENVIRONMENT MAY BE VERY BENEFICIAL. • RESPECT YOUR OWN NEED TO GRIEVE WHEN THE PROCESS ENDS.
 Provoked seizure
Provoked seizure Tnfp
Tnfp Malingering
Malingering Southern psychiatric association
Southern psychiatric association Role of psychiatric nurse
Role of psychiatric nurse Psychiatric emergency
Psychiatric emergency Psychiatric nurse conference
Psychiatric nurse conference Father of psychiatric nursing
Father of psychiatric nursing Sleep disorders
Sleep disorders During a psychiatric emergency the emt should be able to
During a psychiatric emergency the emt should be able to Mental health definition in nursing
Mental health definition in nursing Psychiatric emergency
Psychiatric emergency Northeast florida psychiatric associationinc
Northeast florida psychiatric associationinc American psychiatric association annual meeting 2020
American psychiatric association annual meeting 2020 Psychiatric disorders
Psychiatric disorders Ethical and legal issues in psychiatric nursing
Ethical and legal issues in psychiatric nursing Psychiatric security review board
Psychiatric security review board Mse assessment
Mse assessment Calgary family assessment model
Calgary family assessment model Psychiatric services liberty hill
Psychiatric services liberty hill Cmc psychiatric hospital
Cmc psychiatric hospital Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Psychiatric rehabilitation
Psychiatric rehabilitation Psychiatric nursing process
Psychiatric nursing process Ethical issues in psychiatric nursing
Ethical issues in psychiatric nursing Torrance memorial cardiac rehab
Torrance memorial cardiac rehab California medical license for foreign medical graduates
California medical license for foreign medical graduates Cartersville medical center medical records
Cartersville medical center medical records Greater baltimore medical center medical records
Greater baltimore medical center medical records Hepburn osteometric board
Hepburn osteometric board Susan burgoyne
Susan burgoyne Makalah ruang lingkup psikologi komunikasi
Makalah ruang lingkup psikologi komunikasi Alla dudina
Alla dudina Working principle of gi-fi technology
Working principle of gi-fi technology Susan bogart
Susan bogart Unsustainable behavior examples
Unsustainable behavior examples Susan ibach
Susan ibach Susan rodger duke
Susan rodger duke Susan kurrle
Susan kurrle Susan kinard
Susan kinard James w nilsson
James w nilsson Susan gauch
Susan gauch Susan entwistle
Susan entwistle Susan pojer
Susan pojer No summit out of sight
No summit out of sight Susan langford
Susan langford Swot havaianas
Swot havaianas If with past perfect and would be able/would have been able
If with past perfect and would be able/would have been able Susan bidel
Susan bidel The lightweight fighter lost so much weight
The lightweight fighter lost so much weight Karen woodall
Karen woodall Dr nolan cardiologist
Dr nolan cardiologist Susan kuklin wiki
Susan kuklin wiki