Medical Incident Report Form Education Module for 2011









- Slides: 38

Medical Incident Report Form Education Module for 2011 BLS Basic Training Course (Complete Dataset) Prepared by the Division of Emergency Medical Services
Education Module Goals • Train new EMS personnel • Provide a review for experienced EMS personnel
Education Module Contents • Basic information & general instructions • Aftercare Instructions Highlight • 2011 MIRF dataset
Basic Information & General Instructions
Why the MIRF is Important • Medical – The MIRF (both electronic and paper) is part of the patient’s medical file. – The MIRF transfers information between patient care providers. • Legal – Confidentiality – Patient Refusal – MIRF Signature
Why the MIRF is Important (continued) • Quality Review • Planning/Funding – Medic unit placement, levy funding • Research – Resuscitation Outcome Consortium (ROC) – Aftercare Instructions Pilot Project
Components of a Good Report • Completeness – All available information regarding the incident or patient care should be recorded. • Accuracy – Describe exactly what happened. • Correct spelling • Legibility (on paper forms)
Components of a Good Report (continued) • Narrative: use S. O. A. P format: – Subjective – Objective – Assessment – Plan
Basic Instructions • An electronic recordis created by CAD/Dispatch for every call/incident. • When completing the paper (short) form in the field, use a ball point pen and press hard enough to mark through all copies. • Complete the electronic record, verifying that the CAD information has been received, and augmenting this information where appropriate. • Refer to your agency protocols regarding exceptions to completing the paper (short) form. ******* • Agencies using the paper (long) formshould complete a form for every call/incident.
Paper MIRF Pages • Agency copy • EMS copy • Medical Review copy • Patient copy • Aftercare Instructions: The backer provides health information to patients.
Completing the MIRF The person who provided primary care should: • Sign your name • Printyour name • Write your EMS number

Patient Refusal • Follow the instructions on the back of the MIRF. • Fill in patient’s name, and the date. • Read the statement slowly & clearly to the patient. Ask if they understand what it says. • Have the patient/guardian sign in the appropriate spots. • If patient/guardian refuses or you are unable to obtain a signature, make a note to that effect. • Obtain a signature from a witness and note their EMS agency affiliation or address.

Aftercare Instructions Highlight
Aftercare Instructions Highlight The backer is to be given to ALL patients. Aftercare instructions are located on the back of last page of the MIRF (both short and long form) for a variety of health conditions. CHECKALL APPLICABLEboxes: • • • Patient was Not Transported Low Blood Sugar Information High Blood Pressure Information Falls Community Resources Information
Aftercare Instructions Highlight (cont. ) • Not Transported Patient left at scene or transported by a private occupancy vehicle. • Transported Patient transported by BLS, ALS, or a private ambulance.

Aftercare Instructions Highlight (cont. ) • Low Blood Sugar Patient was treated for hypoglycemia and not transported. • High Blood Pressure Patient with a systolic ≥ 160 OR diastolic ≥ 100. • Falls

Aftercare Instructions Highlight (cont. ) • Community Resources – Can be offered to any patient in need of social services including: • • Caregiver & Disability Resources Domestic Violence Emergency Shelter Financial Assistance for Rent or Utilities Food & Clothing Health Care & Support Groups Legal Help
2011 MIRF Dataset • Incident Data (in alphabetical order) • Patient Data (in alphabetical order)
Incident Data • Action Taken • Agency Incident Number • Aid Type
Incident Data (Cont. ) • • Date Time Scene • Date Time Arrived on Scene Dispatch Notified In Service Last Response Unit Leave Primary PSAP Notified Unit Notified by Dispatch Unit Responded

Incident Data (cont. ) • • First Agency on Scene ID First EMS Reporting Agency on Scene First Unit on Scene Geocode
Incident Data (cont. ) • • • Incident Incident Address City County State Type (NFIRS) Zip Code
Incident Data (cont. ) • • Initial (Incident) Dispatch Code (IDC) Location Type Outside Agency Incident Number Property Use (NFIRS) Reporting Agency Number Reporting Unit ID Number Responding from Quarters Responding in Fire District Code
Incident Data (cont. ) • Response Delay Type • Response Mode • Treatment Crew Member Name

Patient Data (Cont. ) • • Action Taken Allergies Date/Time Arrived at Patient’s Side Date/Time Arrived at Treatment Facility or Transfer Point • Date/Time Extrication is Completed • Date/Time Patient Left Scene • EMS ID Number of Person Completing Form
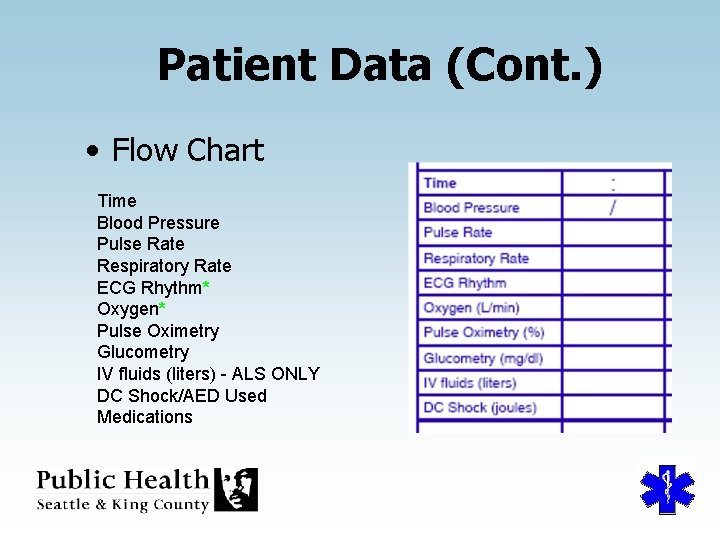
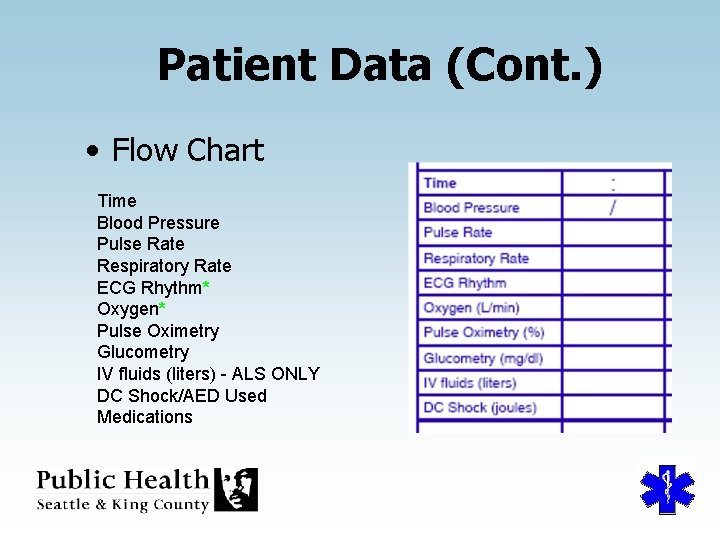
Patient Data (Cont. ) • Flow Chart Time Blood Pressure Pulse Rate Respiratory Rate ECG Rhythm* Oxygen* Pulse Oximetry Glucometry IV fluids (liters) - ALS ONLY DC Shock/AED Used Medications
Patient Data (Cont. ) • Flow Chart (cont. ) ECG Rhythm 01 Sinus Rhythm 02 Asystole 04 Other 11 Ventricular Fibrillation U 0 Unknown
Patient Data (Cont. ) • Flow Chart (cont. ) Oxygen Mechanism 1 Non-rebreather 2 Nasal Cannula 3 Bag Valve Mask 4 Blow-By 5 Other (see Narrative) 6 BVM + ITD The notes section of the flow chart can be used for notes or for extended flow chart information
Patient Data (Cont. ) • • Glasgow Coma Eye Opening Component Motor Response Verbal Response Score (GCS)
Patient Data (Cont. ) • • • Highest Level of Care Provided Mass Casualty Incident Medical Facility Contacted Name Medical Person Contacted Name MIRF Number
Patient Data (Cont. ) • Narrative Use the S. O. A. P. format: Subjective Objective Assessment Plan

Patient Data (Cont. ) • • Onset of Symptoms Patient Age, Units Patient Date of Birth Patient Street Address, City, County, State, Phone • Patient First Name, Middle Initial, Last Name • Patient Gender • Patient Health Care Provider, Phone
Patient Data (Cont. ) • Patient Mechanism Code (refer to the electronic pick list) • Patient Medications Taken at Home • Patient Parent or Legal Guardian • Patient Suspected Alcohol or Drug Use • Patient Type Code
Patient Data (Cont. ) • Procedures Check all boxes for procedures performed. For procedures 12 -31 only: write the procedure number and the EMS number of the person who performed the procedure • Treatment Crew Member Number for Procedure
Patient Data (Cont. ) • • • Safety Equipment Signature of Person Completing Form Transport Agency Number Transport Delay Type Transport Destination Transport Unit Number

2011 MIRF Changes
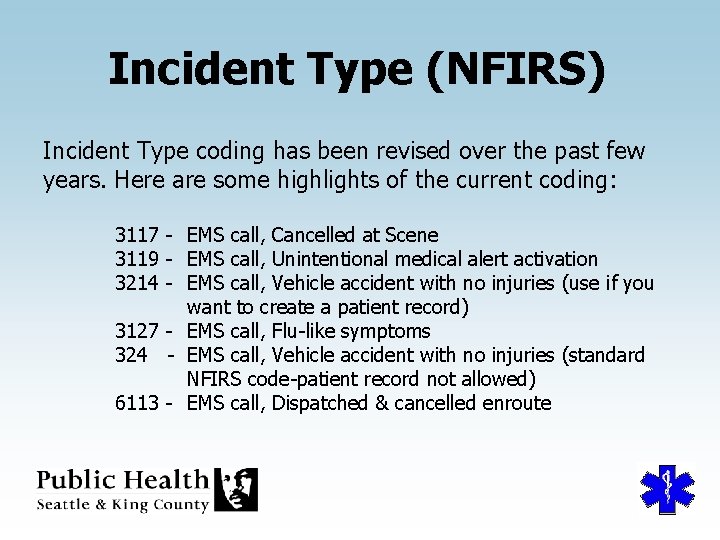
Incident Type (NFIRS) Incident Type coding has been revised over the past few years. Here are some highlights of the current coding: 3117 - EMS call, Cancelled at Scene 3119 - EMS call, Unintentional medical alert activation 3214 - EMS call, Vehicle accident with no injuries (use if you want to create a patient record) 3127 - EMS call, Flu-like symptoms 324 - EMS call, Vehicle accident with no injuries (standard NFIRS code-patient record not allowed) 6113 - EMS call, Dispatched & cancelled enroute
Medical Incident Report Form Education Module for 2011 BLS THE END Prepared by the Division of Emergency Medical Services