Medical Futility A guide to understanding the nature
- Slides: 34
Medical Futility A guide to understanding the nature of medical futility, identifying conflicts it presents, and working to resolution. Sponsored by -- The Jason Program creating a community of care
Objectives Define & recognize futility situations Understand how to recognize different points of view assess futility situations create a fair processes to resolve intractable conflict Understand our values & feelings
Outline Definitions of Futility Points of View Differential Diagnosis Case Resolution Caregiver survival
Definitions of Futile Interventions Won’t achieve the patient’s goal Serves no legitimate goal of medical practice Ineffective more than 99% of the time Does not conform to accepted community standards
Do Semantics Matter? Unequivocal cases of medical futility are rare – example? Miscommunication, value differences are more common Case resolution more important than definitions
Points of View Family wants care the medical team views as futile - 10 Medical team wants to provide care the family refuses - 20 Any party may perceive futility or be invested in interventions
Differential Dx of Futility Situations Misunderstanding Inappropriate surrogate Personal factors Values conflict
Human Sources Sleep deprivation Stress Denial Psychologically unprepared Inadequate cognitive ability
Communication Sources Inadequate information given Diagnosis, Prognosis, Options Conflicting Information Previous overoptimistic prognosis Poor Communication Language (“Do Everything”), Context, etc. Too much jargon
Assessment & Response Good communication skills
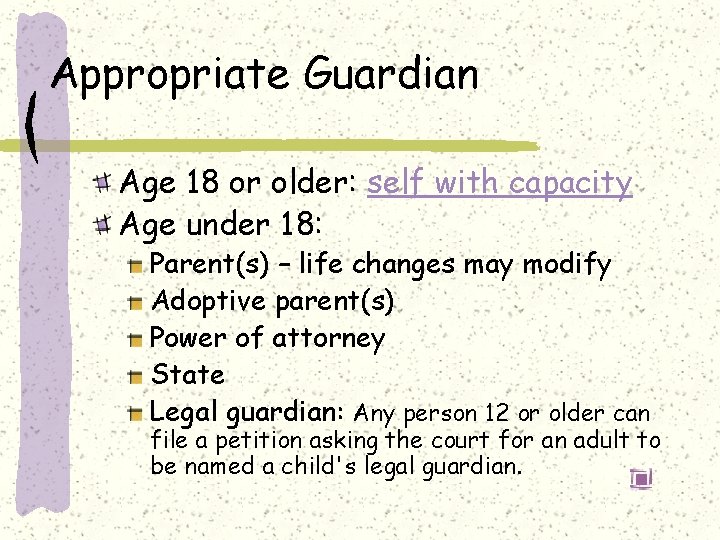
Appropriate Guardian Age 18 or older: self with capacity Age under 18: Parent(s) – life changes may modify Adoptive parent(s) Power of attorney State Legal guardian: Any person 12 or older can file a petition asking the court for an adult to be named a child's legal guardian.
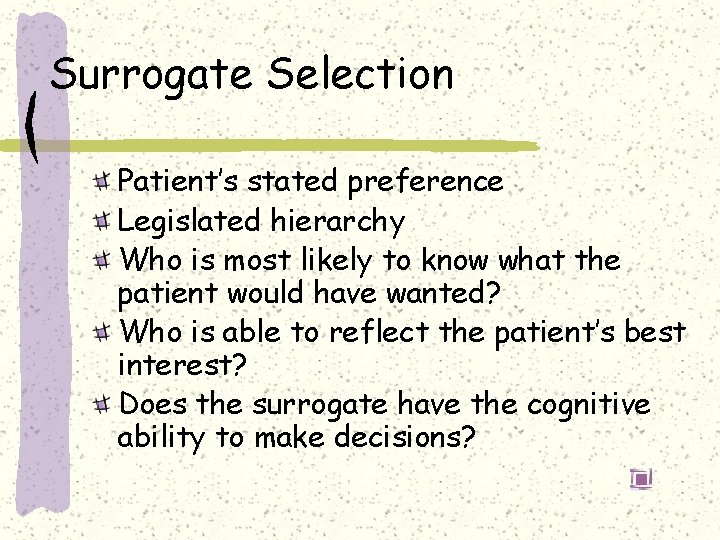
Surrogate Selection Patient’s stated preference Legislated hierarchy Who is most likely to know what the patient would have wanted? Who is able to reflect the patient’s best interest? Does the surrogate have the cognitive ability to make decisions?
Interpersonal Factors Mistrust Grief Guilt Family dynamics Secondary gain
Mistrust Patients give subtle clues Last doctor made a mistake Previous hospital gave poor care Address situation gently Explore the dimensions of mistrust Rebuild trust Offer a 2 nd opinion Promise truth
Grief Natural human response to loss May be anticipatory Help the family distinguish between what they want and what the patient would want Social work Spiritual work Nursing input
Guilt Relationship with dying patient… ”You must do everything. . you can’t let him die. ” Often associated with shame Not discussed with medical team Solution = whole patient assessment
Family Dynamics
Secondary Gain Implications of a patient’s death $$$$$$ Social status Place of residence The decision maker gains from the patient’s death May need legal or ethics consult
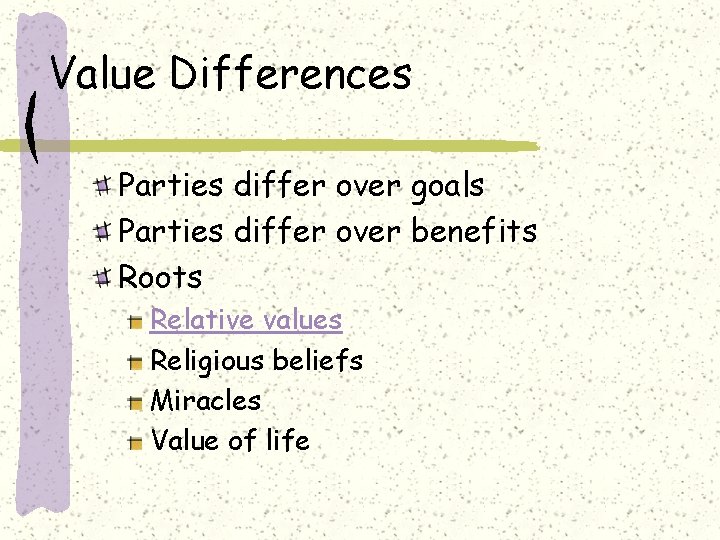
Value Differences Parties differ over goals Parties differ over benefits Roots Relative values Religious beliefs Miracles Value of life
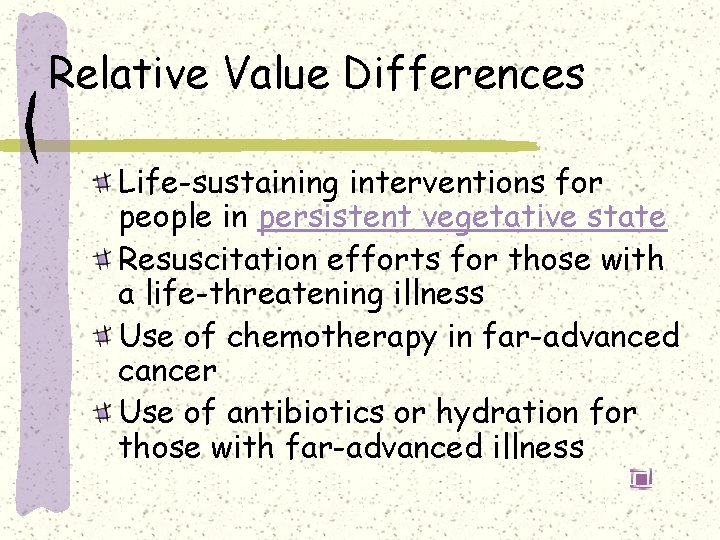
Relative Value Differences Life-sustaining interventions for people in persistent vegetative state Resuscitation efforts for those with a life-threatening illness Use of chemotherapy in far-advanced cancer Use of antibiotics or hydration for those with far-advanced illness
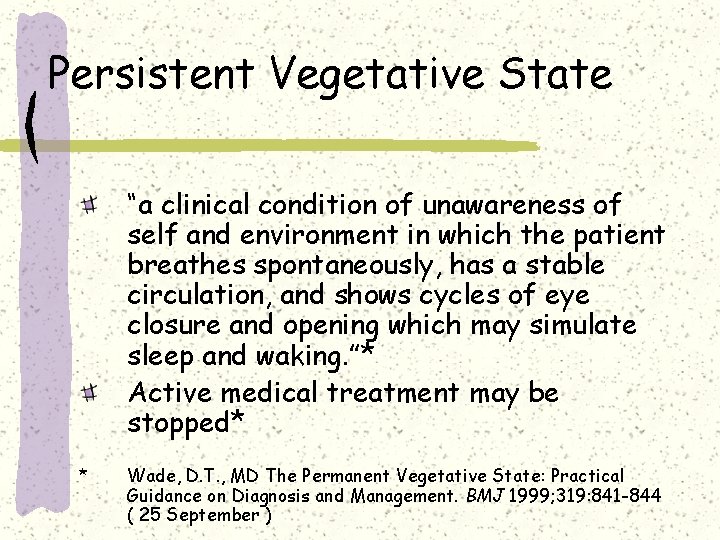
Persistent Vegetative State “a clinical condition of unawareness of self and environment in which the patient breathes spontaneously, has a stable circulation, and shows cycles of eye closure and opening which may simulate sleep and waking. ”* Active medical treatment may be stopped* * Wade, D. T. , MD The Permanent Vegetative State: Practical Guidance on Diagnosis and Management. BMJ 1999; 319: 841 -844 ( 25 September )
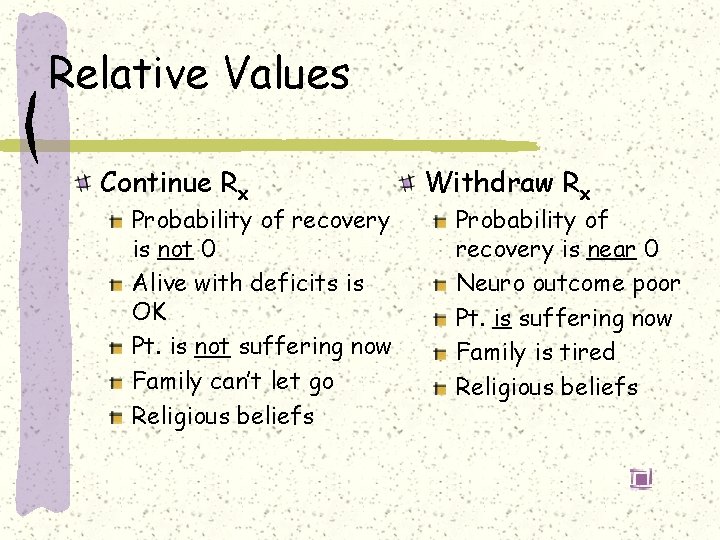
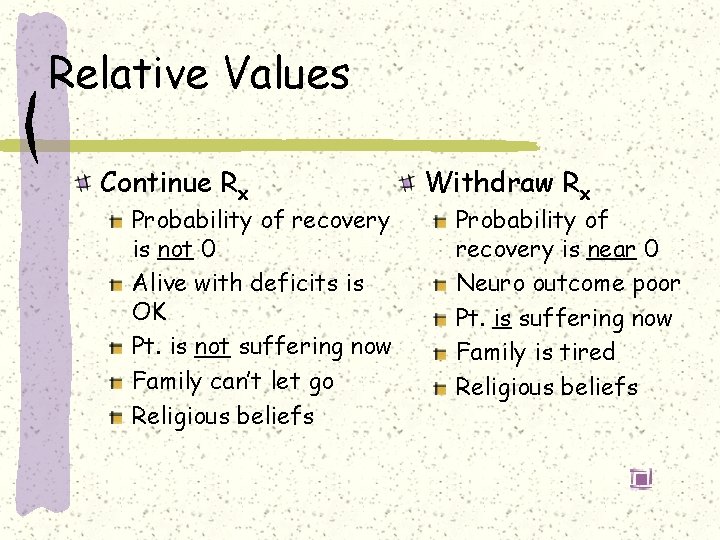
Relative Values Continue Rx Probability of recovery is not 0 Alive with deficits is OK Pt. is not suffering now Family can’t let go Religious beliefs Withdraw Rx Probability of recovery is near 0 Neuro outcome poor Pt. is suffering now Family is tired Religious beliefs
Religious Beliefs Patients may have a firm religious foundation for their decisions Clues, eg. : “It’s in the Lord’s hands. ” Exploration is important Overcome conventions to avoid religion Acknowledge importance to the patient Ask for help in understanding Work with a religious leader Know your own feelings
Miracles Ever-present hope Suggestions Embrace the patient’s hope Acknowledge human limits Plan for the worst Ask about “God’s plan” when appropriate
Value of Life “Worth preserving at all costs” “People shouldn’t play God” Suggestions Focus on advanced directives if available Parents can speculate what the child would wish Discuss “letting go”
Conflict Over Treatment Unresolved conflicts lead to misery most can be resolved Try to resolve differences Support the patient / family Base decisions on informed consent, advance care planning, goals of care
Finding a Resolution Attempt to negotiate an understanding of what would be considered futile care prior to the event – Example Joint decision making - communication Enlist institutional support – ethics committee Transfer of care
Anticipation G. E. is a 12 year-old girl with advancing spinal muscular atrophy type II. She can speak and move her right arm, but cannot cough. She has had increasingly frequent respiratory difficulties, any one of which may be fatal. Should she have a tracheostomy to better manage these episodes?
Role Reversal Medical person, team, or institution wishes to implement a treatment the patient feels is futile Adults Children
Role Reversal - Adult An adult with capacity or his surrogate makes the decision Medical person must accept +/- transfer Rarely, ongoing conflicts arise when the decision is believed to be illegal Medical person need not change his own viewpoint nor do anything he cannot Acceptance of other viewpoint helpful
Role Reversal - Child A child whose guardian makes the decision Medical team must decide if it is “reasonable” or if it constitutes neglect Neglect pursued through authorities “Reasonable” must be accepted +/transfer
Caregiver Survival Accept your feelings & find your role Professional – family – both Accept imperfection in nature Accept imperfection in yourself Adopt reasonable personal standards Learn from mistakes Admit your limits
Summary Futility situations have many angles Prevent problems before they occur Good communication is necessary Understand yourself Gary Allegretta, M. D. Phone: (207)-829 -3537 Medical Director Fax: (602)-294 -5066 The Jason Program E-mail: gallegr 1@maine. rr. com P. O. Box 336 Web: www. jasonprogram. org Cumberland, Maine 04021
Thank you very much