Medical Documentation What is it n Broadly speaking
Medical Documentation
What is it? n Broadly speaking Preparation and maintenance of records that describe a pt’s care n Gathered in a clear, concise, and organized manner n Verifying and justifying a Respiratory Therapist’s actions n May include pt history, current condition, assessment, treatment, procedure, care plan, etc n
Purposes of Documentation n Evidence of the quality of pt care n Used by various groups to evaluate and enhance pt care n Track pt progress n Pt’s chart is admissible in court as a legal document and can guard against liability n To serve as an educational tool
Types of Medical Records n n n n A complex record containing many different forms Initial assessment Pt history Daily assessment flow sheets Problem list Diagnosis lists Care plan Etc.
SOAP Written as narrative progress notes n. S = Subjective n. O = Objective n. A = Assessment n. P = Plan
SOAP n Subjective – Information the patient or family members tell you, such as the chief complaint and other impressions n Objective – Factual, measurable data you gather during the assessment, such as observed signs and symptoms, vital signs, and lab test values
SOAP cont. n Assessment – Conclusions based on the collected subjective and objective data and formulated as pt problems (dynamic and ongoing process) n Plan – Strategy for relieving the pt’s problem (Includes both Immediate or short-term actions and long-term measures)
PIE n n n Developed to simplify the documentation process. Problem-orientated approach. Problem – Use collected data from initial assessment to list problems and diagnosis Intervention – Document each intervention for each problem Evaluation – Document-related effects for each problem
PIP n Problem n Intervention n Plan
Charting By Exception (CBE) n Only deviations from standards need to be documented n Developed to overcome lengthy and repetitive notes, poorly organized information, and difficult-to-retrieve data n Basic standards of care clear and concise; they are outlined and considered routine care, and therefore are eliminated n One drawback is that the standards are sometimes inaccessible to staff
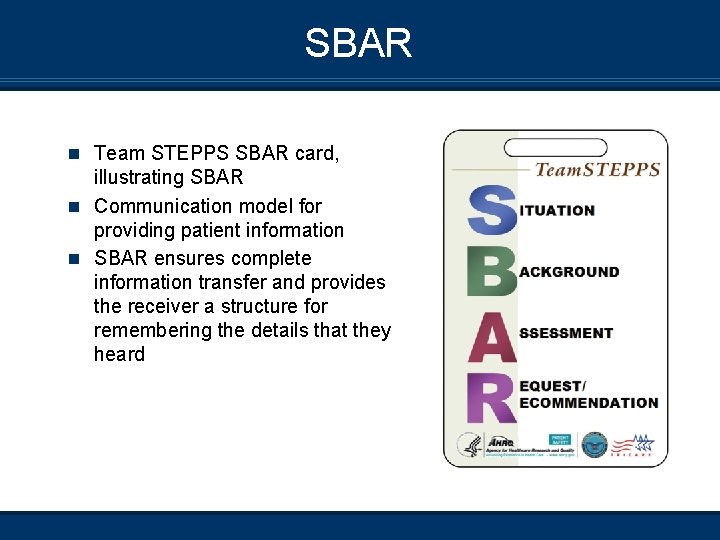
SBAR n Team STEPPS SBAR card, illustrating SBAR n Communication model for providing patient information n SBAR ensures complete information transfer and provides the receiver a structure for remembering the details that they heard
SBAR cont. n What is it? The SBAR (Situation-Background-Assessment-Recommendation) technique provides a framework for communication between members of the health care team about a patient’s condition n Why use it? The SBAR tool ensures completeness of info and reduces the likelihood of missed data It allows for an easy and focused way to set expectations for what will be communicated and how it will be communicated n Standardizes communication between healthcare providers, doctor-RT, nurse-nurse, nurse-Dr n How do I do it? • S– Situation – What’s going on (5– 10 seconds) • B– background – Brief pertinent history, relevant context • A– Assessment – What I think, conclusion • R– Recommendation – What I need and in what time frame
SBAR (What it looks like) S Situation – Identify self: The unit I am calling about <patient name and location> The problem I am calling about is __ / I have just assessed the patient personally and these are the changes in the patient’s status: B Background A Assessment n This is what I think the problem is: _______/The problem seems to be < cardiac infection neurologic respiratory / I am not sure what the problem is but the patient is deteriorating / The patient seems to be unstable and may get worse; we need to do something
SBAR – In Practice R Recommendation n I request that you <say what you would like to see done> n Transfer the patient to critical care / Come to see the patient at this time / Talk to the patient or family about code status / Ask the on-call family practice resident to see the patient now / Ask for a consult to see the patient now n Are any tests needed? n Do you need any tests like CXR, ABG, EKG, CBC, or BMP? n If a change in treatment is ordered then ask n How often do you want vital signs? How long do you expect this problem will last? / If the patient does not get better when would you want us to call again? n Confirm n I understand that the treatment plan is: <intervention and time frame for anticipated outcomes> n What should I do before you get here to assess the patient?
Elements of Sound Documentation n Logical approach to problem-solving n Systematic n Accurate and thorough n Well-written (Correct spelling, grammar, and abbreviations)
Sound Documentation cont. n Neat and legible n Write in black ink only n Demonstrate professionalism and diligence n Timely Three C’s: Clarity, Consciousness, and Consistency
Legal & Ethical Implications of Documentation n RTs are ethically and legally accountable to all of their patients n The scope of your professional responsibility is set out by CARTA
Legal & Ethical Implications cont. n Your documentation demonstrates that the patient care you provide meets the needs of the patient at a specific point in time and meets accepted standards of RT practice mandated by your profession n Assures every effort has been made to guarantee pt well -being

Legal & Ethical Implications cont. “If it isn’t documented, it wasn’t done. ” n Information contained in the chart belongs to the patient, who has the right to obtain a copy of the materials
Legal Relevance n Think of the medical record first and foremost as a clinical communication that you documented carefully n Example: When the pt’s condition deteriorates or changes in therapy are clearly indicated, you must not only chart this information but contact the physician as soon as possible and chart the fact that you contacted the physician
Errors or Omissions n Can severely undermine your credibility in court n If you failed to chart something and need to enter a late entry, date and time it the day you entered it and also indicate what period of time the documentation refers to
Corrections and Alterations n Corrections to the medical record should be made only by drawing a line through the initial charting, then signing and dating it n Then proceed to supply the proper entry n NEVER erase, obliterate, white-out, or otherwise alter a record n Never throw out a pt’s medical record
When & What to Document n Each health care facility and specific areas within the facility will establish policies about frequency of pt assessment n Besides documenting simply according to policy, be sure to record specific and descriptive narrative notes whenever you observe any of the following:
When & What Cont. A. B. Change in pt condition (progression, regression, or new problems). E. g. “The pt can walk 300 feet on 2 lpm oxygen via nasal cannula on flat ground with no assistance. ” Pt’s response to a treatment or meds. E. g. “The patient states that SOB is relieved 10 minutes after receiving 1 mg Ventolin via SSN. Some accessory muscle usage still noted… RR… HR… O 2… etc. ”
When and What Cont. C. D. Lack of improvement in the patient’s condition. E. g. “No change in pt colour, RR, HR, accessory muscle usage, SOB, or Pa. O 2 after oxygen increased from 6 lpm NC to 15 lpm NRM. ” Pt or family members’ response to teaching. E. g. “The patient performed MDI use proficiently x 2 after instruction and stated she should repeat 2 puffs morning and night. ”
What Else? n Date and time… every time E. g. May 2, 2005 1305 Pt found on the floor…………………………. . . n Draw a line through any blank spaces to discourage others from adding to your notes
What Else cont… n If you don’t have enough room to sign your name at the end of the last entry, draw a line in the next space from the left margin toward the right margin, leaving room to sign your name on the far right side 1/5/03 1200 Will continue plan and request Mucomyst for thick secretions. n If you are recording a lot of information and think you might run out of room on the page, leave space at the bottom of the page to write “continue on next page”
Verbal Dr’s Orders n Ask for protocol at each site n RTs can write verbal orders from physicians in the appropriate place on the order sheet, as long as the order pertains to scope of practice relating to RT practice
What to do for Your Clinical Experience as a Student n Watch and learn from your preceptors n Try to recognize good and bad habits n Each site has their own way of doing things; follow hospital protocol and use good judgment
Summary n Documentation of pt assessments serves a variety of purposes n A variety of documentation formats are available, each with its own advantages n Regardless of method chosen, high-quality documentation after each pt encounter promotes improved communication within the health care organization and promotes improved pt outcome
References n Clinical Assessment in Respiratory Care. 5 th Edition, 2005 n Complete Guide to Documentation. Lippincott, Williams, & Wilkins, 2003
- Slides: 31