Medical Decision Making Capacity AZ DHS BEMS Education
Medical Decision Making Capacity AZ DHS BEMS Education Committee Updated November 2020
Objectives • • • Background for education development Define decision making capacity Review actual patches/cases Interrupt Learn
Informed consent “Every human of adult years with a sound mind has the right to determine what should be done with his own body” 1 1) Schloendoff v Society of New York Hospital, 211 NY 125 (NY 1914)
Refusal • A competent adult has the constitutionally protected right to refuse medical care 1 • Providers who honor a competent (adult) decision to refuse treatment will not be subject to liability for any resulting bad outcome 2, 3 1) Cruzan v Director, Missouri Department of Health, 497 UA 261, 279 (1990) 2) Rodriguez v Pino, 634 So 2 d 681 (Fla Ct App 1994) 3) Wons v Public Health Trust, 500 So 2 d 679, 686 (Fla Dist Ct App 1987)
Risks of Failure to Consent • False Imprisonment “Providers can be sued for treating patients over • Battery ” 1 their objections • Negligence 1) Moore v Wyoming Medical Center 825 F. Supp. 1531 (1993)
BUT “Delaying treatment in an emergency …. is a much more serious and common medicolegal problem than failure to obtain …. consent” Rosen’s Emergency Medicine; concepts and clinical practice 6 th ed
Refusals “Every human of adult years with a sound mind has the right to determine what should be done with his own body” 1 Every adult (others require special considerations) … who is competent … can refuse medical care Schloendoff v Society of New York Hospital, 211 NY 125 (NY 1914)
Adult • Age 18 or above • Emancipated minors -Married minors -Minors in the military • Age ≥ 12 and Homeless -Under special circumstances only
Minor can consent (Arizona) • Emancipated, married or homeless -Care relates to: • STD/STI • Drug and Alcohol treatment • HIV • Pregnancy and family planning • Not emancipated minors age ≥ 12 and: -Care relates to rape/sexual assault -Care related to substance abuse http: //www. peds. arizona. edu/residency/documents/Consent. Confidentiality. pdf
Capacity versus Competency • Capacity • Clinical determination • What we determine • Based on a series of questions • Patients with capacity can make their own decisions • NOT simply A & O x 4 Competency • Legal standard • Determined by the judicial system, ie. a judge • Whether an individual is able to make their own decisions • Presumed for most adults • Irrelevant in the prehospital setting!
Take Home Point • If you only remember one thing from this lecture, it is that A & O x 4 ≠ Capacity
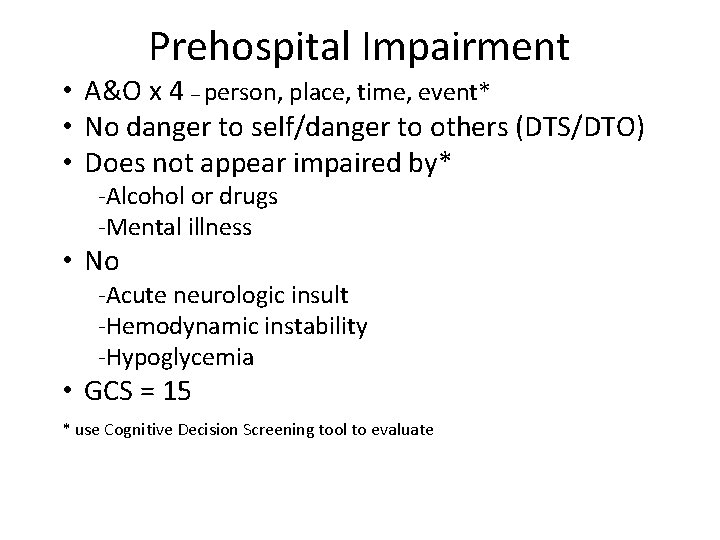
Prehospital Impairment • A&O x 4 – person, place, time, event* • No danger to self/danger to others (DTS/DTO) • Does not appear impaired by* -Alcohol or drugs -Mental illness • No -Acute neurologic insult -Hemodynamic instability -Hypoglycemia • GCS = 15 * use Cognitive Decision Screening tool to evaluate
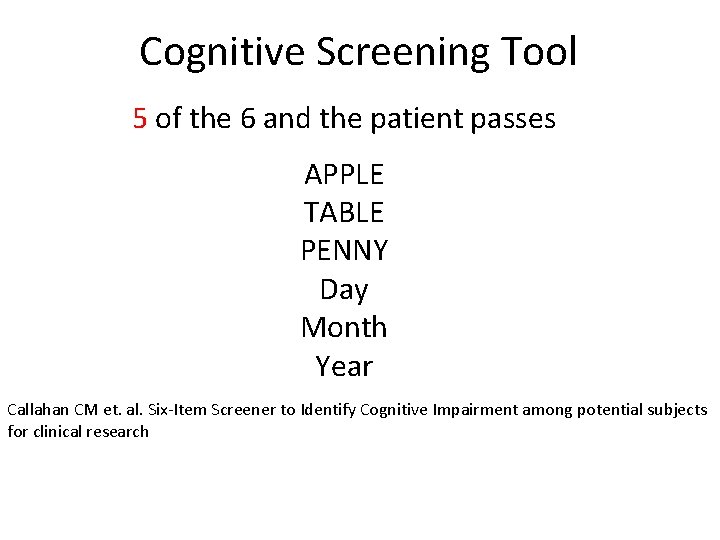
Cognitive Screening Tool 5 of the 6 and the patient passes APPLE TABLE PENNY Day Month Year Callahan CM et. al. Six-Item Screener to Identify Cognitive Impairment among potential subjects for clinical research

Its never that easy • Not an adult • Not competent – Adults with legal guardians – Adults in custody – Adults with DTO/DTS – Impaired adults
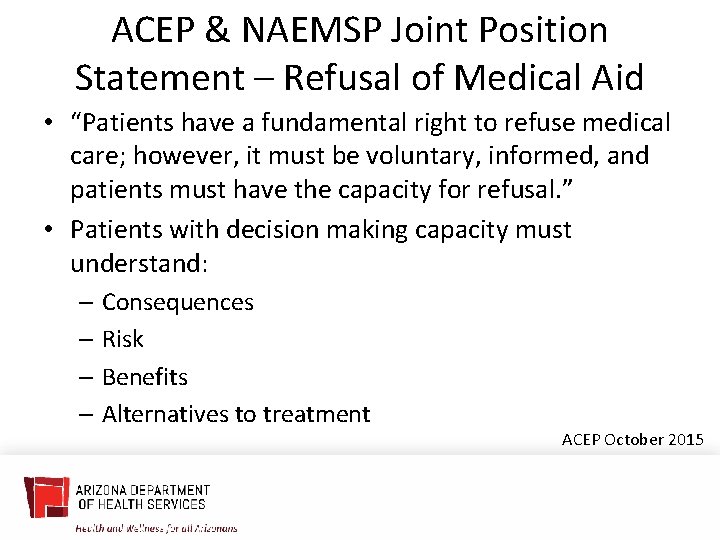
ACEP & NAEMSP Joint Position Statement – Refusal of Medical Aid • “Patients have a fundamental right to refuse medical care; however, it must be voluntary, informed, and patients must have the capacity for refusal. ” • Patients with decision making capacity must understand: – Consequences – Risk – Benefits – Alternatives to treatment ACEP October 2015
Autonomy • The right of “self-determination” • The patient has the right to refuse or choose treatment • This means they can make a “bad decision” that could result in harm • However, we must determine that they have decision making capacity to make this decision
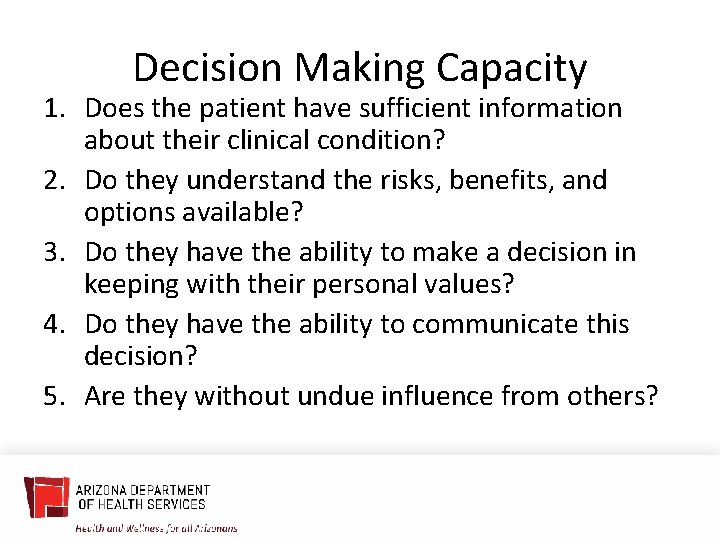
Decision Making Capacity 1. Does the patient have sufficient information about their clinical condition? 2. Do they understand the risks, benefits, and options available? 3. Do they have the ability to make a decision in keeping with their personal values? 4. Do they have the ability to communicate this decision? 5. Are they without undue influence from others?
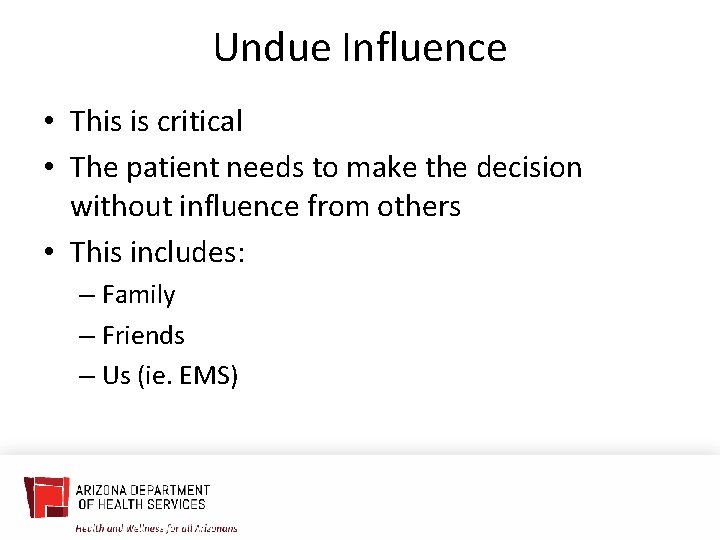
Undue Influence • This is critical • The patient needs to make the decision without influence from others • This includes: – Family – Friends – Us (ie. EMS)
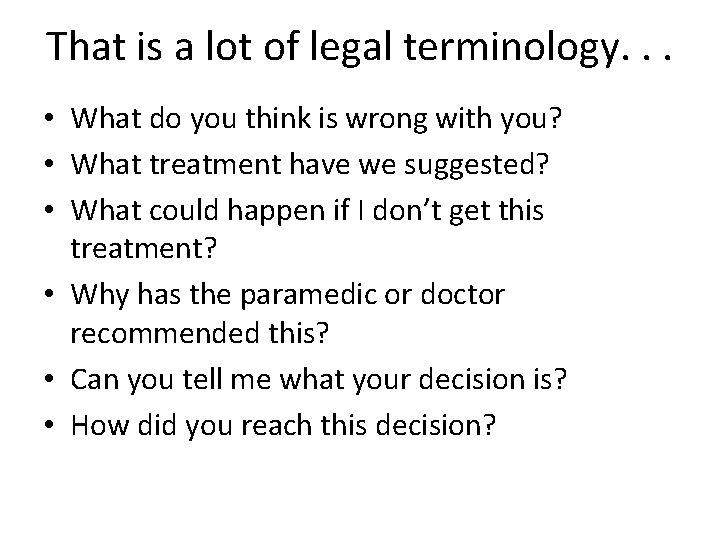
That is a lot of legal terminology. . . • What do you think is wrong with you? • What treatment have we suggested? • What could happen if I don’t get this treatment? • Why has the paramedic or doctor recommended this? • Can you tell me what your decision is? • How did you reach this decision?
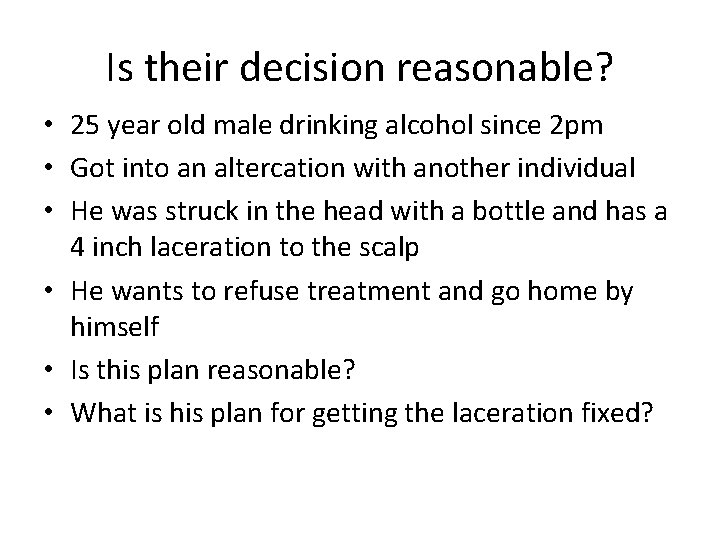
Is their decision reasonable? • 25 year old male drinking alcohol since 2 pm • Got into an altercation with another individual • He was struck in the head with a bottle and has a 4 inch laceration to the scalp • He wants to refuse treatment and go home by himself • Is this plan reasonable? • What is his plan for getting the laceration fixed?
Is their decision reasonable? • 75 year old patient with terminal lung cancer • Family got nervous and called 911 • The patient’s pulse oximetry is 85% and he is working hard to breathe • He tells you that he is on hospice, and his oncologist has told him that he has no further treatment options • He states, “I am going to die, I understand this, and have come to terms with this. My family is scared, but we have discussed this and made the appropriate arrangements. ” • Reasonable decision?
Can someone who is drinking or using drugs have capacity? • Yes! • The key is to ask the right questions to determine if they have medical decision making capacity! • They must be able to communicate clearly
Case Scenario • Family called 911 after finding their 23 year old daughter unresponsive • Patient has history of heroin use • Family gives dose of intranasal naloxone at same time as calling 911 • Upon arrival of EMS crew, patient is awake, alert, and oriented times four • She now wants to refuse transport to the ED
Case Scenario • Crew patches for ALS refusal • Physician speaks to patient on patch phone • When asked why she doesn’t want transport the patient states, “this happened before, all you do at the hospital is watch me for a few hours then I go home” • When asked if she understands that she may lose consciousness and stop breathing when the naloxone wears off she states, “I know, but my parents have another dose of narcan” • Does she have capacity? • Yes
Case scenario • Crew dispatched to home with pertinent patient information stating assault • Upon arrival crew finds adult male patient talking to PD outside of residence • Crew briefly talks to patient and officer, and offers patient evaluation, which he declines • Crew goes back in service
Case scenario • 2 days later the Fire and Police Chiefs receive an email of concern from the patient’s wife • Her email includes the following statements: – “He was intoxicated as well as emotionally a mess” – “His clothing was quite bloody (from scrapes on his arms from the fall), and he had a scrape on his forehead. ” – “That the next morning, my husband woke up in the motel with a severe headache and couldn’t see properly out of one eye; he walked himself to an urgent care near the motel, where he was diagnosed with a concussion. ” – “There was a lot of blood visible on his clothing, and small pools of it on the walkway in front of the house. ” – “Big knot under his cap in addition to the scrape on his forehead. ”
Case scenario • The closing statements from her email stated, “as a lawyer, I am not sure he was in the right frame of mind to refuse treatment” • e. PCR from the crew included the following: – HPI: Assault. Called out for an assault. Cancelled on scene by PD. No pt contact. • Is this enough documentation to paint the picture? • Crew states that it was dark outside and they did not appreciate blood on the patient • They did not inquire about alcohol or drug use
Any red flags? • When called out to a domestic violence incident are alcohol and drugs often involved? • Police requested your assistance, are they concerned about an injury? • What does “no patient contact mean? ” • Is simply saying “do you want us to check you out” sufficient?
Alcohol • Alcohol intoxication itself may not render a patient incompetent 1 • Must determine in each situation if …. incapacitated by alcohol (and) … can not understand the risks and benefits (of)…. treatment …. . • Alcohol level should not be used to determine competance 2, 3 1) Miller v Rhode Island Hospital, 625 A 2 d 778 (RI 1993) 2) Siegel DM: Consent and refusal of treatment. Emerg Med Clini North Am 11: 833, 1993 3) Ethering JM: Emergency management of acute alcohol problems. Can Fam Physician 42: 2423, 1996
Alcohol & Refusals • In the ED we allow patients to sign out AMA or we discharge them with alcohol levels well above the legal limit • We typically “metabolize to freedom” • Key is to allow patient to sober up enough to go home safely • How does this related to EMS?
“Roosevelt Rule” • Attending at Maricopa taught us that in order for us to discharge or sign out AMA someone who had been drinking, they had to pass the “Roosevelt Rule” • This meant they could cross Roosevelt Road (4 lanes) at night in the dark, without getting hit by a car • What does this demonstrate?
What about dementia patients? • Patients can have a diagnosis of dementia and still have decision making capacity • However, this should prompt you to ask more specific questions to determine if the patient has capacity
Dementia • Prehospital – Cognitive screen – Simple yes or no • Spectrum of capacity 1 – Ability to make a treatment choice – Ability to appreciate the decision & consequences – Ability to rationally manipulate the information – Ability to understand treatment options
Case Scenario 73 y. o. male in altercation a home with his son PD called EMS to evaluate the patient VS = 202/108, 84, 98%, Accucheck 120 Patient has history of HTN & reports taking Rx Patient has dementia, but per the crew he is “A & O x 4” • Wife reports she is his POA and would like the patient transported • • •
Case Scenario • Patient states he wants to stay home with his family • Physician talks to patient on the patch phone • Patient able to explain why EMS & PD were called to the house • When asked about his HTN, he states “it is normal for my BP to be high” • He can give the name of his med, “Losartan. HCT”
Case Scenario • Patient correctly provides the year, month, city, and state • When asked what could happen if his BP stays elevated, he responds with “it will destroy my organs, but I don’t want that to happen” • He then states, ‘if my son and I stop having altercations my BP won’t be high” • Does he have decision making capacity? • Yes!
Capacity • Capacity isn’t a blanket term • It applies to this point in time • For more complex decisions, patients may not have decision making capacity • This needs to be reassessed with each decision
Case Scenario • Dispatched to group home, pertinent patient information is patient with fever, chills, and history of HTN • e. PCR documented as patient refusal with minimal information, including no VS or patient assessment • Different crew dispatched two days later, patient transported at that time • Diagnosed with acute renal failure and acute vision loss
Family Complaint • Mother contacts Fire Department admin to inquire why her son was not transported after 911 was called on his behalf the first time • Per complaint, “he is a resident of a group home, diagnosed with special needs, requires adult supervision and decision making oversight. ” • Mother states he does not have capacity and she maintains guardianship with all documentation on file at the group home
Case Discussion • Crew brought in to discuss case • They recall that patient had “special needs” and was lying in bed with the blanked pulled over his head • He refused to speak to the crew • Staff provided the crew with “some medical records” but reported that he could make his own decisions • Is this enough information to allow refusal?
Case Discussion • Adult patients residing in group home often lack medical decision making capacity • Many of these individuals have guardians, either family or court appointment that make their decisions • Ask staff to specifically provide any demographic paperwork or documentation on guardianship • When in doubt, contact online medical control
Special Considerations • Is the patient an adult without a guardian? • Does the patient live in a group home? – If so, are they their own guardian? – Who makes medical decisions for them? • Can a patient communicate their decision to you? – If a patient refuses to cooperate with an evaluation and won’t communicate with you, these patients are deemed to lack decision making capacity "Evaluating Patient's Decision Making Capacity. " EMS World. T Dunn. May 2015
High Risk Evaluations • Be cautious with patients with possible head injury or other disease processes that affect their cognition – This includes CVA, hypoglycemia, seizure/postictal pts – Has the patient regained normal cognition and understanding of the risks associated with refusing care?
Recent case in the ED • 45 y. o. male with acute expressive aphasia • CT found acute frontal lobe stroke • Patient waiting on in-patient bed and becomes very agitated, trying to leave • Nursing staff ask if they should “just sign him out AMA? ” • Does this patient have decision making capacity?
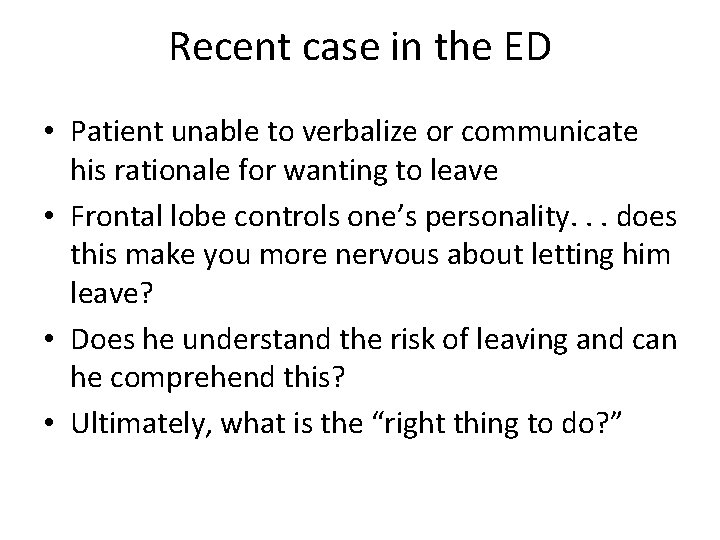
Recent case in the ED • Patient unable to verbalize or communicate his rationale for wanting to leave • Frontal lobe controls one’s personality. . . does this make you more nervous about letting him leave? • Does he understand the risk of leaving and can he comprehend this? • Ultimately, what is the “right thing to do? ”
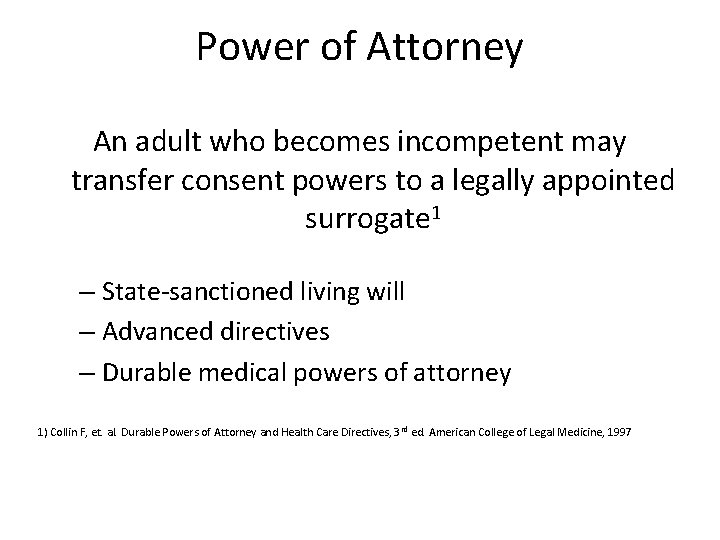
Power of Attorney An adult who becomes incompetent may transfer consent powers to a legally appointed surrogate 1 – State-sanctioned living will – Advanced directives – Durable medical powers of attorney 1) Collin F, et. al. Durable Powers of Attorney and Health Care Directives, 3 rd ed. American College of Legal Medicine, 1997
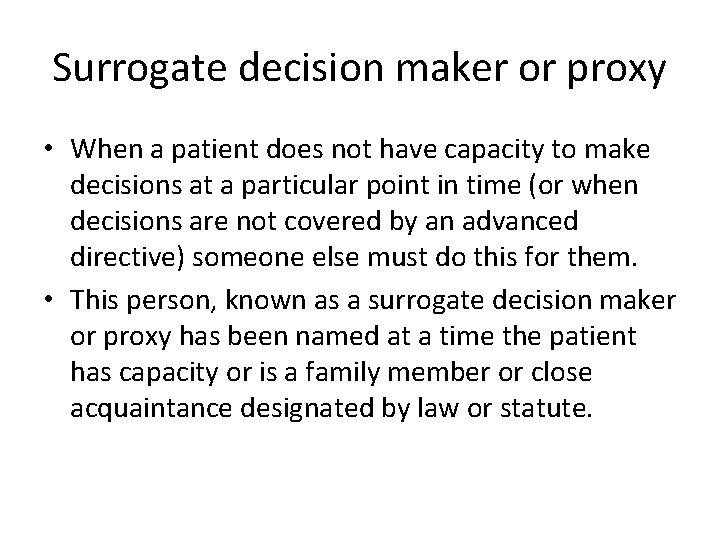
Surrogate decision maker or proxy • When a patient does not have capacity to make decisions at a particular point in time (or when decisions are not covered by an advanced directive) someone else must do this for them. • This person, known as a surrogate decision maker or proxy has been named at a time the patient has capacity or is a family member or close acquaintance designated by law or statute.
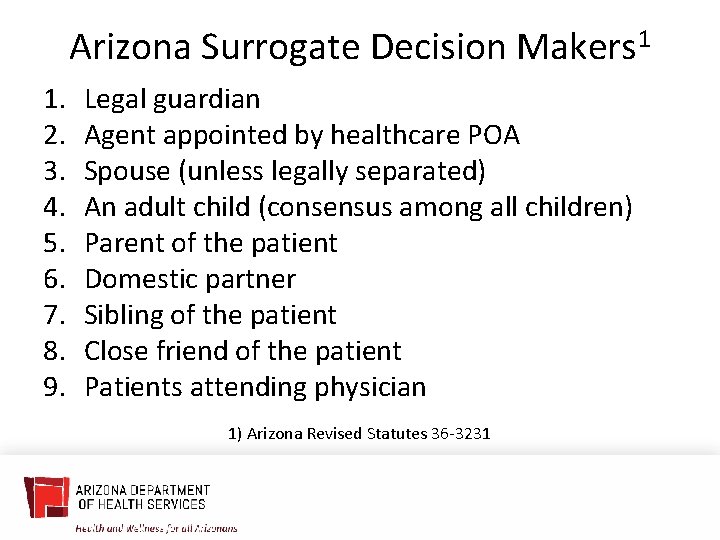
Arizona Surrogate Decision Makers 1 1. 2. 3. 4. 5. 6. 7. 8. 9. Legal guardian Agent appointed by healthcare POA Spouse (unless legally separated) An adult child (consensus among all children) Parent of the patient Domestic partner Sibling of the patient Close friend of the patient Patients attending physician 1) Arizona Revised Statutes 36 -3231
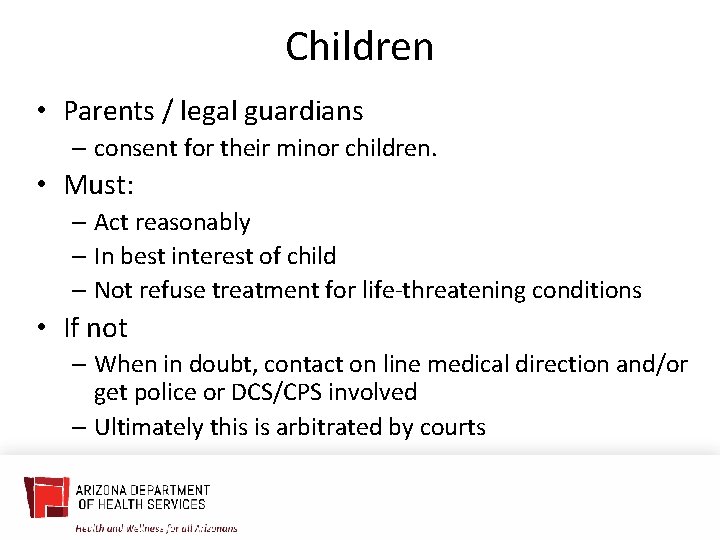
Children • Parents / legal guardians – consent for their minor children. • Must: – Act reasonably – In best interest of child – Not refuse treatment for life-threatening conditions • If not – When in doubt, contact on line medical direction and/or get police or DCS/CPS involved – Ultimately this is arbitrated by courts
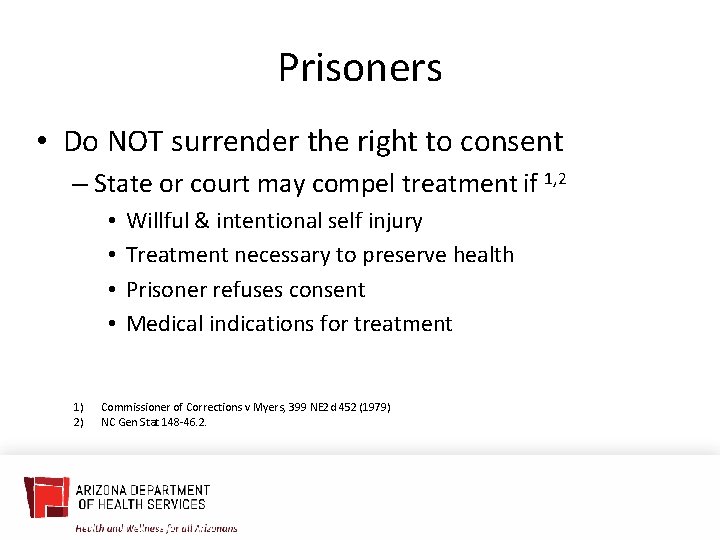
Prisoners • Do NOT surrender the right to consent – State or court may compel treatment if 1, 2 • • 1) 2) Willful & intentional self injury Treatment necessary to preserve health Prisoner refuses consent Medical indications for treatment Commissioner of Corrections v Myers, 399 NE 2 d 452 (1979) NC Gen Stat 148 -46. 2.
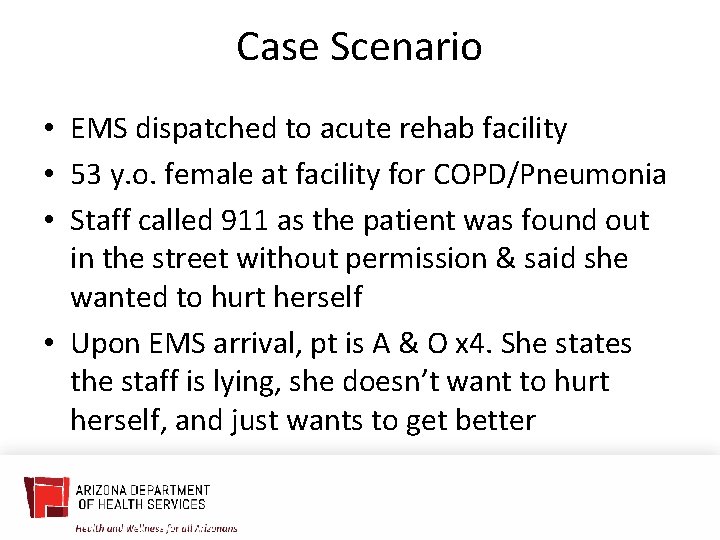
Case Scenario • EMS dispatched to acute rehab facility • 53 y. o. female at facility for COPD/Pneumonia • Staff called 911 as the patient was found out in the street without permission & said she wanted to hurt herself • Upon EMS arrival, pt is A & O x 4. She states the staff is lying, she doesn’t want to hurt herself, and just wants to get better
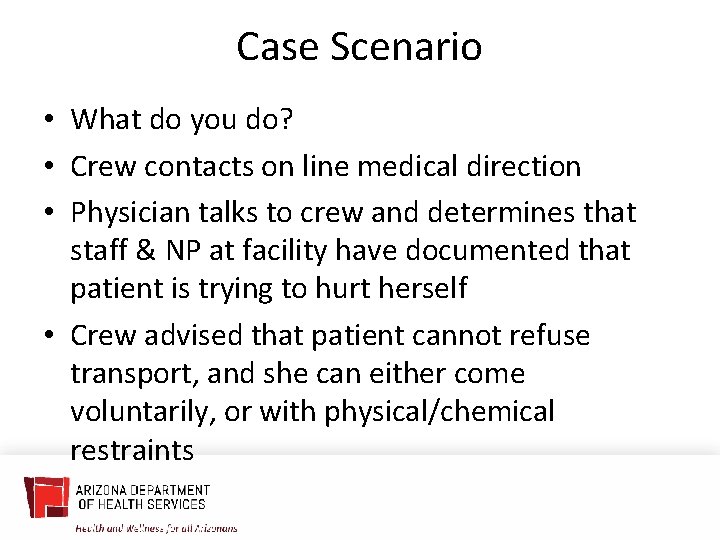
Case Scenario • What do you do? • Crew contacts on line medical direction • Physician talks to crew and determines that staff & NP at facility have documented that patient is trying to hurt herself • Crew advised that patient cannot refuse transport, and she can either come voluntarily, or with physical/chemical restraints
Case Scenario • Upon arrival in ED, provider reviews documentation from facility • Facility documents “patient found in bed at 0754 crying and stated I am just going to leave and run in front of traffic and end it all. ” • Patient petitioned and transferred to inpatient psychiatric facility
SI/HI “A person acting under a reasonable belief that another person is about to commit suicide or to inflict serious physical injury upon himself may use physical force upon that person to the extent reasonably necessary to thwart the result. ” ARS § 13 -403
“When in Doubt Rule” Emergency Care providers should “do what they believe to be in the patient’s best interest and worry about the legal consequences later”

THANK YOU Gail Bradley|Medical Director azhealth. gov @azdhs facebook. com/azdhs
- Slides: 57