Medical Credentialing MELISSA JOHNSON CPMSM CPCS MEDICAL STAFF






- Slides: 25
Medical Credentialing MELISSA JOHNSON, CPMSM, CPCS MEDICAL STAFF & CREDENTIALING CONSULTANT IMPLEMENTATION/CLIENT SERVICES DIRECTOR – NEBRASKA CREDENTIALS VERIFICATION ORGANIZATION
Objectives: • Define primary source verification and sources for verifying information. • Discuss best practice standards for the credentialing of independent practitioners in medical facilities. • Review negligent credentialing. • Identify “red flags” in the credentialing process.
Credentialing • The process of obtaining, verifying and assessing the qualifications of practitioner to provide care or services in or for a health care organization. • Primary Source Verification: Obtain and verify a credential directly from the original issuing entity. • There are “designated equivalent sources” that are acceptable by the accrediting or regulatory bodies as an approved entity for primary source verification. • Example: Certifacts for board certification or AMA profile for training verification. • The verification MUST come directly from the source to the entity (not from the applicant). • Involves a series of activities designed to collect verify and evaluate data relevant to a practitioner’s clinical performance. • Serves as the foundation for objective, evidence-based decision regarding appointment, membership or privileges.
• Applicant completes application • Demographic information • Medical school and training facilities • Licenses, DEA, Controlled Substance certificates • Board certification • Malpractice history (current and past) • Professional references • Health status • Explanation of time gaps from medical school forward • CME attendance • Hospital or organizational affiliations/work history • Signs release of information, privilege delineation or various other facility specific forms
Education and Training: • Complete list of medical school, training programs (internship, residency and fellowship), Educational Commission Foreign Medical Graduates (ECFMG), and Fifth Pathway as well as dates of attendance and graduation. • Primary Source examples: • Directly from the school or training program • National Student Clearinghouse • AMA or AOA profile • ECFMG • Federation of State Medical Board
Professional & Controlled Substance Licensure: • Complete list of all professional and controlled substance licensure including the issuing state/agency, license type, license number, status and expiration date. • Primary Source examples: • State licensing board • Federation of State Medical Board • Drug Enforcement Agency (DEA) • National Technical Information Service (NTIS) • State controlled substance board/agency

Board Certification: • Complete list of board specialty certifications held including original date, recertification date and participation in Maintenance of Certification, if applicable. • Primary Source examples: • Directly from the issuing board • American Board of Medical Specialties • AMA or AOA profile • American Board of Physician Specialties **Acceptable boards are generally outlined in policy and procedures or Bylaws for the entity
Affiliation/Work History/Military/Time Gap: • • Chronological list of all facilities where the practitioner has worked or held clinical facilities including start date, status, and end date. • Explanation from the applicant for any time gaps over 30 days • Explanation from the applicant of any instances of discipline, suspension, probation or reprimand Primary Source examples: • Directly from the facility or current military duty station • DD 214 for military experience if discharged **Best practice is to get at least five years of affiliations/work history but will depend on policy & procedures or Bylaws for the facility.

Criminal Background Disclosure: • Background checks including conducting a county and national criminal search for the past seven years (this includes sex offender, vulnerable populations and terrorist activity). • Primary Source examples: • Facility approved background check vendor • National, state and country criminal databases
Sanctions: • Federal or state sanctions (or lack of sanctions). • Primary Source examples: • National Practitioner Data Bank (NPDB) • Office of the Inspector General (OIG) List of Excluded Individuals/Entities (LEIE) • System for Award Management (SAM)
National Practitioner Data Bank (NPDB): • NPDB provides healthcare specific reports on state and federal criminal convictions and civil judgements as well as malpractice history and hospital restrictions or reports. • Primary Source example: • National Practitioner Data Bank
Malpractice Insurance: • Complete list of insurance carriers including coverage dates as well as list of open, pending, settled, closed or dismissed malpractice cases. • Primary Source examples: • Current and past malpractice insurance carriers • National Practitioner Data Bank (NPDB) **Best practice is to verify the current carrier as well as the past five years carriers but will depend on an organization’s language in their policy and procedures or Bylaws.
Professional/Peer References: • Professional/peer references who can attest to the applicant’s current competence to perform clinical care. • Primary Source examples: • Letter or questionnaire from the reference **Accreditation Council for Graduate Medical Education (ACGME) recommends this information includes the six best practice standards for assessing an applicant’s competencies: patient care, medical knowledge, practice based learning and improvement, systems based practice, professionalism and interpersonal skills and communication.
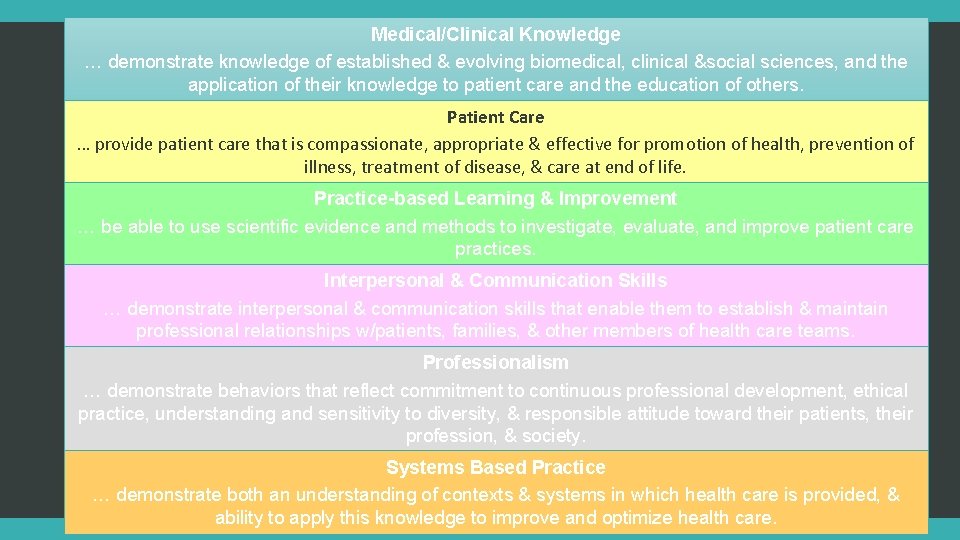
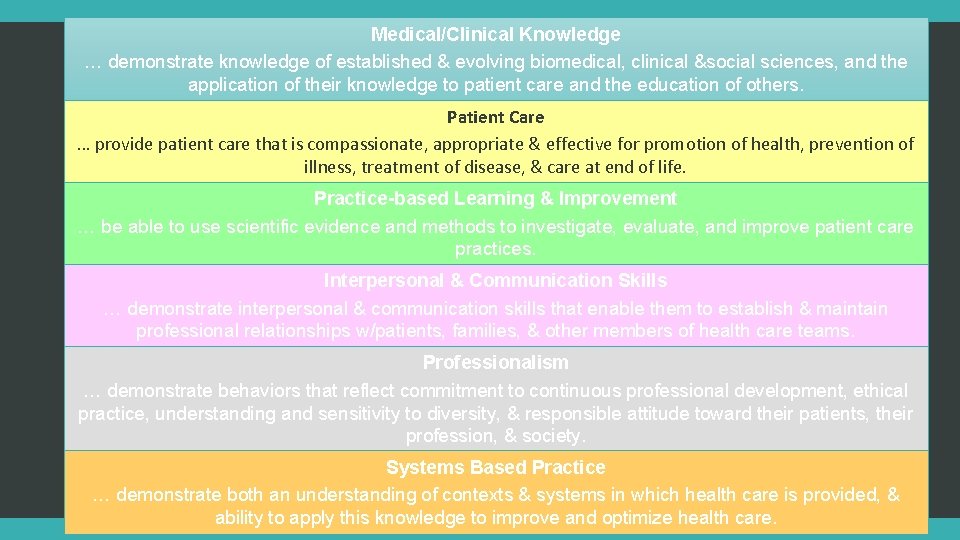
Medical/Clinical Knowledge … demonstrate knowledge of established & evolving biomedical, clinical &social sciences, and the application of their knowledge to patient care and the education of others. Patient Care … provide patient care that is compassionate, appropriate & effective for promotion of health, prevention of illness, treatment of disease, & care at end of life. Practice-based Learning & Improvement … be able to use scientific evidence and methods to investigate, evaluate, and improve patient care practices. Interpersonal & Communication Skills … demonstrate interpersonal & communication skills that enable them to establish & maintain professional relationships w/patients, families, & other members of health care teams. Professionalism … demonstrate behaviors that reflect commitment to continuous professional development, ethical practice, understanding and sensitivity to diversity, & responsible attitude toward their patients, their profession, & society. Systems Based Practice … demonstrate both an understanding of contexts & systems in which health care is provided, & ability to apply this knowledge to improve and optimize health care.

Approval process • Through the whole process, the burden is on the applicant to provide sufficient documentation to support their request • • Credentials Committee, if applicable, and Medical Executive Committee (MEC) • • If more information is needed, the applicant is responsible for providing it. Makes a recommendation to the Board of Directors or their designee Board of Directors • Approves or denies membership or privilege requests **Varies based on policy and procedures or Bylaws of the facility.
Reappointment • Privileges/membership are granted for a period not to exceed two years. • Process is very similar to the initial application process except concentrates on the previous two year period • Includes facility specific data on the provider such as ongoing professional practice evaluation information.
Why do we Credential? • To protect patients • Ensure high quality patient care by protecting the public from incompetent practitioners • Protect the practitioner and hospitals • from liability and legal risk when done correctly • Required by The Joint Commission, CMS and other regulatory agencies Too much risk involved to NOT credential practitioners correctly.
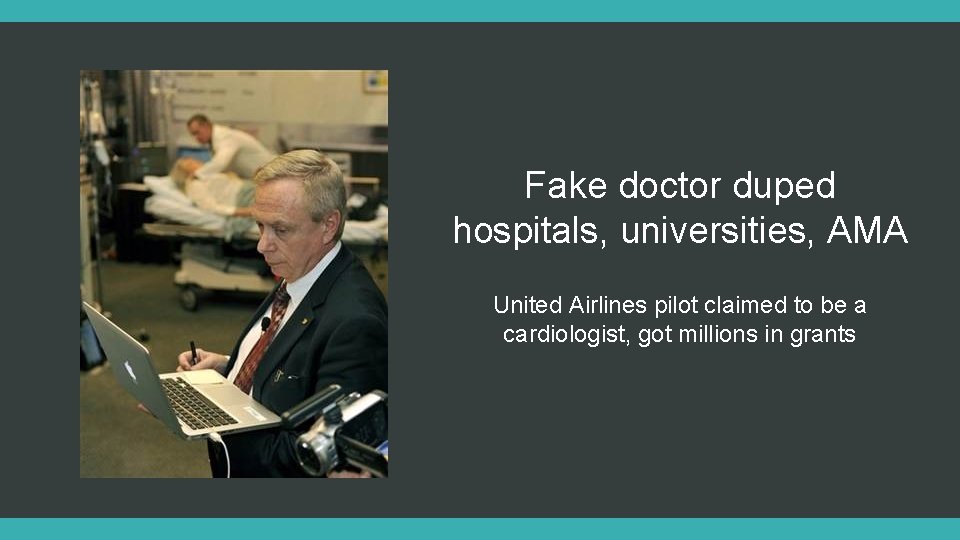
Fake doctor duped hospitals, universities, AMA United Airlines pilot claimed to be a cardiologist, got millions in grants

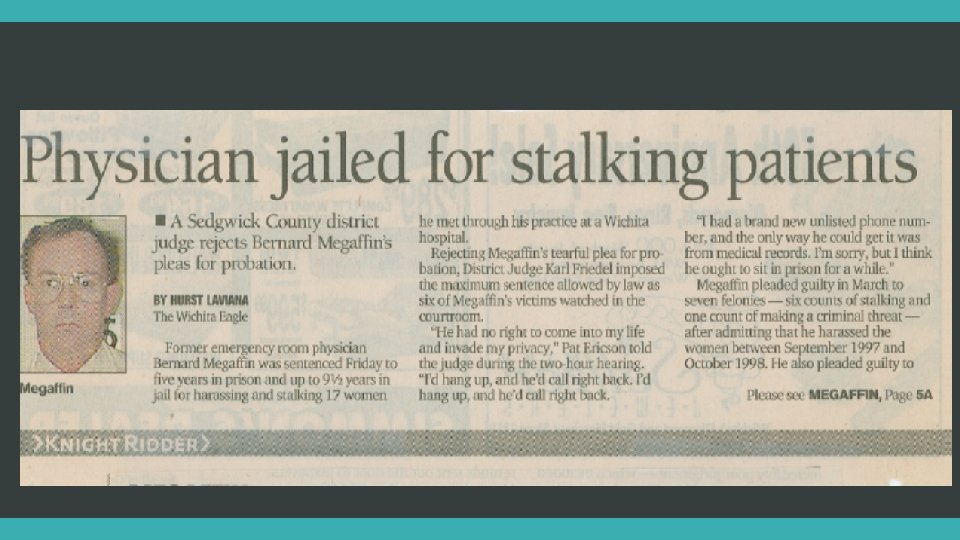
The Kadlec Case • It involved an impaired anesthesiologist who did serious harm to a patient. • When the last hospital which privileged the practitioner queried a previous employer they received a glowing reference – which turned out to be a lie. • The querying hospital also received generic references about the practitioner and didn’t dig deeper for more detailed information. Cost this patient, her family, the references and facilities greatly.
“Red Flags” 1) Less than excellent references 2) Time gaps since medical school 3) Moves from one area to another that lack a logical career progression 4) Disciplinary actions or investigations by medical staff organizations, hospitals, state medical boards, or professional societies 5) Resignation from a medical staff or practice 6) Pattern of jury verdicts or settlement for professional liability/malpractice claims. Litigation that is excessive for specialty and number of years in practice **Red flags do not automatically preclude a provider from being credentialed – they just need to be investigated.
“Determining the competency of practitioners to provide high quality, safe patient care is one of the most important and difficult decisions an organization must make. ” (The Joint Commission)

Questions & Discussion: • Questions ? • Recent survey experience ?

Thank you. Melissa Johnson, CPMSM, CPCS medstaffmelissa@cox. net Melissa@omahamedical. com
 Cpmsm
Cpmsm Melissa johnson
Melissa johnson Johnson and johnson credo
Johnson and johnson credo Jjeds jnj directory
Jjeds jnj directory Johnson and johnson swot analysis
Johnson and johnson swot analysis Johnson and johnson organizational structure
Johnson and johnson organizational structure Johnson and johnson three c's of classroom management
Johnson and johnson three c's of classroom management Johnson and johnson bcg matrix
Johnson and johnson bcg matrix Johnson and johnson botnet infections
Johnson and johnson botnet infections Johnson and johnson md&d
Johnson and johnson md&d Brad and laurie johnson
Brad and laurie johnson Johnson and johnson swot analysis
Johnson and johnson swot analysis Cms credentialing requirements
Cms credentialing requirements Qualification certification and credentialing personnel
Qualification certification and credentialing personnel Rcem acp curriculum
Rcem acp curriculum 607 meaning
607 meaning Mtm ride
Mtm ride Nacp credentialing
Nacp credentialing Namss certification
Namss certification Ucsf
Ucsf Florida association of medical staff services
Florida association of medical staff services Cpcs validator
Cpcs validator Cpcs table
Cpcs table Cpcs 222
Cpcs 222 Cpcs 202
Cpcs 202 Cpcs 202
Cpcs 202