Medical Concerns After Spinal Cord Injury Frazier Rehab
Medical Concerns After Spinal Cord Injury Frazier Rehab Institute Spinal Cord Medicine Program
Possible Medical Concerns • • Skin Issues/Pressure Ulcers Autonomic Dysreflexia Orthostatic Hypotension Spasticity Pain Heterotopic Ossification Deep Vein Thrombosis
Skin Issues • Largest organ of the human body • Functions: – Prevents harmful bacteria from entering body – Helps prevent fluid loss – Helps regulate body temperature – Organ of sensation • Pain, touch, pressure, hot, cold • Skin after spinal cord injury – Nerve cells may be damaged resulting in decreased or loss of sensation below the level of injury = decreased awareness
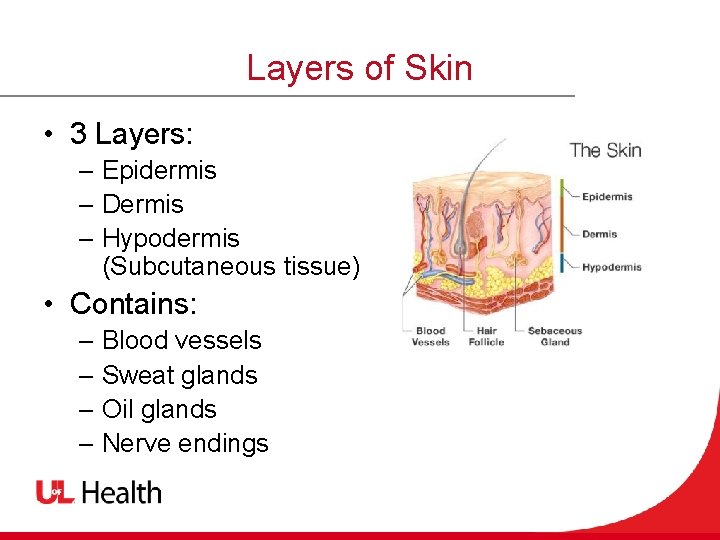
Layers of Skin • 3 Layers: – Epidermis – Dermis – Hypodermis (Subcutaneous tissue) • Contains: – Blood vessels – Sweat glands – Oil glands – Nerve endings
Pressure Ulcers • Decubitus ulcer, skin sores, bedsores • Wound or injury usually caused by unrelieved pressure resulting in damage to the skin and underlying tissue • Most common cause of re-hospitalization

Common Sites for Pressure Ulcers
Stages of Pressure Ulcers • 6 Stages • Does not always start on top of your skin where it can be seen • It can take up to 5 days to see damage to your skin from unrelieved pressure
Stages of Pressure Ulcers Stage I • Damage to top 2 layers • Non-blanching redness Stage II • Damage extends into 3 rd layer • Skin is open –May appear as an abrasion or blister • May have clear or bloody drainage
Stages of Pressure Ulcers Stage III • Damage through all layers of skin and into muscle tissue • May appear as deep crater • May have clear or bloody drainage Stage IV • Damage through all layers, into bone and possibly tendons and joints • Possible clear or bloody drainage • Very difficult to heal
Stages of Pressure Ulcers Un-stageable • Unable to be staged because the depth of the wound cannot be seen due to necrotic tissue or slough Deep Tissue Injury • Area of discolored (bruise-like) skin or blood -filled blister due to damage of underlying tissue
Treatment • Can be treated easily if detected in early stages • Will need to be followed by wound care for appropriate treatment • Debridement –removal of dead or infected tissue • Topical medications or surgical • Surgery
Pressure Relief • • • Prevention is key Every 2 hours when in bed Use pillows, foam wedge, heel protectors DO NOT use “donut rings” Every 15 minutes for 15 seconds when in manual wheelchair • Every 30 minutes for 30 seconds when in power wheelchair

Pressure Relief
Other Prevention Strategies • • Check skin Keep skin clean, dry and moisturized Check equipment regularly Wear appropriate clothing Maintain appropriate weight Well balanced diet with plenty of fluids Be careful about heat
Thermo-regulation • Abnormal regulation of body temperature due to decreased ability to respond to changes in the environment • Abnormal sweating response • Lost ability to shiver • Poikiolothermia • Takes on the temperature of the environment
Thermo-regulation • Provide good environmental control • Dress appropriately
Autonomic Dysreflexia (AD) • A true medical emergency • Over-reaction of your central nervous system due to the spinal cord injury • Caused by a painful stimulus below the level of injury • Dangerous rise in blood pressure • Usually mid thoracic level (Thoracic 6)
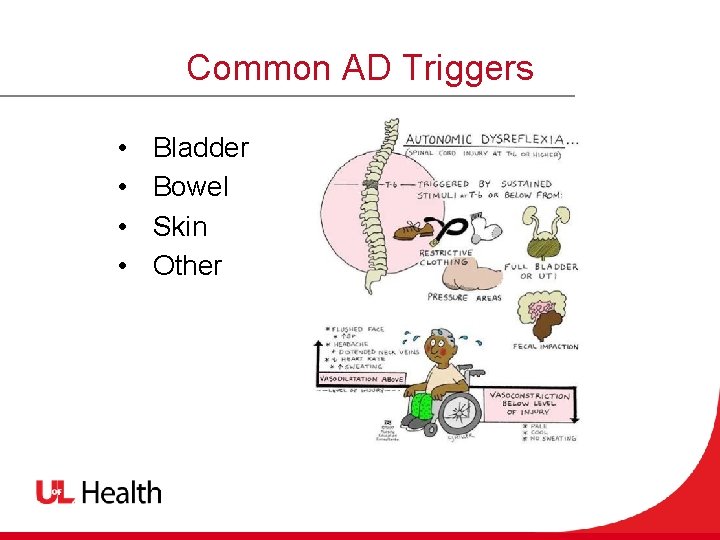
Common AD Triggers • • Bladder Bowel Skin Other

AD Bladder Triggers • Overfull, overstretched, distended bladder • Kinked or clogged catheter or full drainage device • Intermittent Catheterization (IC) • UTI
AD Bowel Triggers • Full or distended bowel • Constipation, obstipation, impaction or obstruction • Insertion of suppository • Digital stimulation • Hemorrhoids
AD Skin Triggers • • • Pressure ulcers Prolonged pressure Ingrown toenails Constrictive clothing Sunburn
AD Other Triggers • • Sexual activity / Ejaculation Menstruation Pregnancy / Labor & delivery Medical procedures Urodynamics, etc. Medical Issues Fractures, DVT, HO, etc.
AD Signs & Symptoms • Sudden increase in blood pressure • • • 20 mm. Hg above baseline blood pressure Low heart rate with increased blood pressure Sudden pounding headache Goose bumps above/below level of injury Flushing of the skin above level of injury Sweating above/below level of injury Nasal congestion Blurred vision Feeling anxious, nervous or confused Sometimes there are NO symptoms
AD Intervention • • • ACT QUICKLY to lower blood pressure Sit upright Loosen restrictive clothing Empty bladder, bowel and check skin Nitro paste (talk to your provider before using) Call 911 if you are unable to lower blood pressure • Go to the nearest emergency room
Preventing AD • Maintain a consistent bladder and bowel program • Use Lidocaine or Dibucaineto • Protect your skin and perform daily skin checks • Pressure relief • Always let your provider know if you have symptoms of AD
Orthostatic Hypotension • Orthostatic hypotension is a decrease in blood pressure usually from positional changes • • SBP – 20 mm. Hg DBP – 10 mm. Hg • Commonly seen in spinal cord injuries at or above thoracic 6
Signs & Symptoms • • • Lightheadedness Dizziness Feeling fuzzy Blurred vision Syncope • passing out
OH Interventions • • • Drink plenty of fluids Avoid caffeine, alcohol, diuretics Slow positional changes Abdominal binder Compression socks Medications • Midodrine
Spasticity • Involuntary activation of muscles • Common with spinal cord injury • Spasms • Sudden, involuntary muscle contraction • Clonus • Rhythmic pattern of muscle contraction
Complications of Spasticity • • • Pain Fatigue Functional impairment Skin breakdown Joint restriction Contractures

Spasticity Management • • Stretching Splints and casts Modalities Medications • • Baclofen Tizanidine Dantrolene Diazepam • Botox • Baclofen pump

Pain • Most people with a spinal cord injury will have pain • Ongoing pain may have an enormous emotional, physical and social impact on a person’s daily life

Musculoskeletal Pain • Dull, aching pain usually in muscles, tendons, ligaments, bones • Related to posture, activity, movement • Shoulder pain – 50% with spinal cord injuries • Back pain from lack of truck muscles and sitting in wheelchair • Management • • • Proper body alignment Joint protection Stretching Massage Modalities – heat, ice Anti-inflammatory
Neuropathic Pain • Caused by damage to the sensory nerves: – – – – – Hot Burning Tingling Prickling Pins & needles Sharp Shooting Squeezing Electric shock-like • • Management Exercise Relaxation Medications – – Gabapentin (Neurontin) Pregabalin(Lyrica) Amitriptyline (Elavil) Venlafaxine (Effexor) • Steroid injection • Electrical stimulation
Heterotopic Ossification (HO) • Formation of bone in soft tissue of joints below the level of injury • Most commonly around hips followed by knees, elbow, shoulders • Complications: – Interferes with function – Difficulty sitting or standing – Difficulty with transfers
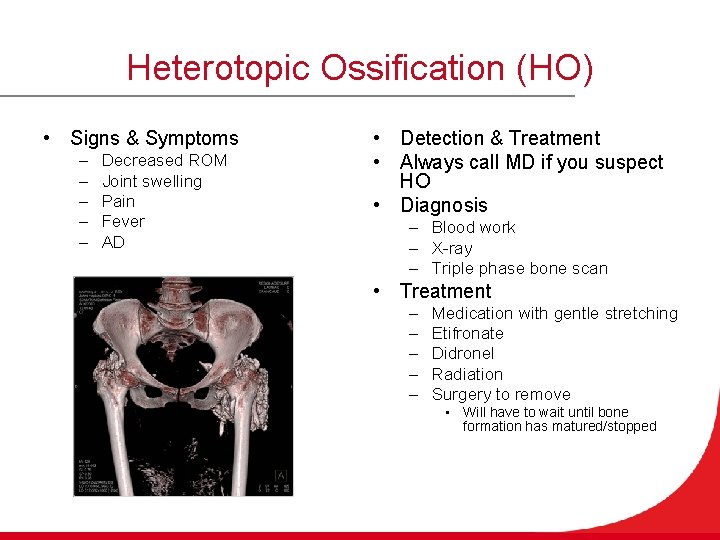
Heterotopic Ossification (HO) • Signs & Symptoms – – – Decreased ROM Joint swelling Pain Fever AD • Detection & Treatment • Always call MD if you suspect HO • Diagnosis – Blood work – X-ray – Triple phase bone scan • Treatment – – – Medication with gentle stretching Etifronate Didronel Radiation Surgery to remove • Will have to wait until bone formation has matured/stopped
Deep Vein Thrombosis (DVT) • Development of a blood clot • Most commonly develops in legs – Can break off and travel to lungs, heart, brain (serious complication) • Can cause circulation problems and pain • Risk factors – – Decreased mobility Prolonged bed rest Trauma Surgery

DVT Signs & Symptoms • • • Swelling in affected area Warmth Pain or tenderness Skin color changes Fever AD
DVT Diagnosis & Treatment • Diagnosis – – Call MD or go to the ER Elevate affected extremity DO NOT rub or massage affected extremity Ultrasound • Treatment – Anticoagulation – Compression hose – ROM exercises
References • Facing Disability. (2019, February 15). Retrieved from Bedsores: http: //www. facingdisability. com • Kirshblum, S. , & Lin, V. W. (2018). Spinal Cord Medicine. Demos Medical; 3 edition. • Paralyzed Veterans of America. (2019, February). Retrieved from https: //www. pva. org
- Slides: 40