Medicaid SpendDown in New York Evelyn Frank Legal

- Slides: 53
Medicaid Spend-Down in New York Evelyn Frank Legal Resources Program New York Legal Assistance Group EFLRP@nylag. org (212) 613 -7310 December 6, 2013 updated 10/20/2017
2 What is Spend-Down? • Carol’s income is $1200/month – above the Medicaid limit ($825 - 2017). But she may qualify for Medicaid by incurring medical bills in an amount that equals the monthly spenddown, also known as “surplus income. ” • Spend-down is like an insurance “deductible, ” but a deductible must usually be met only once a year. The spend-down must be met each month to have Medicaid ongoing.
3 Who Can Benefit from Medicaid Spend-down? • Pathway to Home Care – Carol, age 75, needs Medicaid home care, but her income is $1200/month, over the Medicaid level. • Subsidizing Medicare –Medicaid may help pay Medicare coinsurance like the Part A hospital deductible and Skilled Nursing Facility coinsurance. WARNING: Limited benefit! Does not always apply – see later re inpatient hospital care, Part B coinsurance. • Supplementing Medicare – Long term home care and other long term services are covered by Medicaid, not Medicare • Pathway to “Extra Help” for Part D – Meeting the spend-down for just ONE MONTH can get you EXTRA HELP for the remainder of the calendar year and ALL of the next year. • Especially important for those under 65 so are not eligible for EPIC. Example to follow.
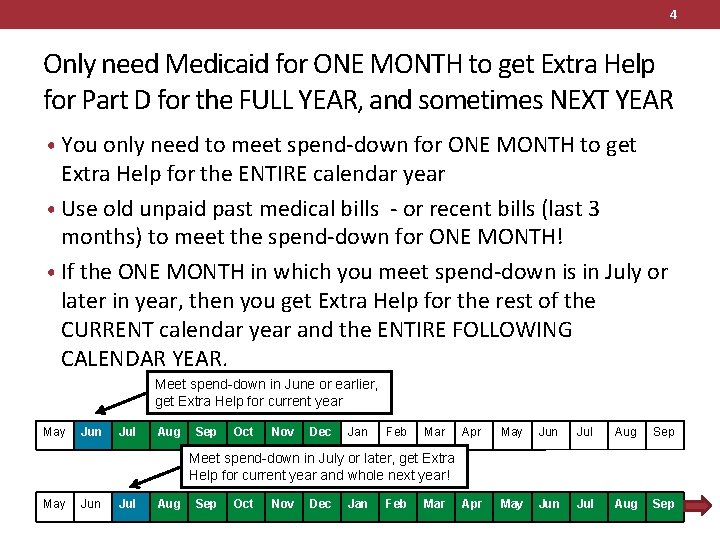
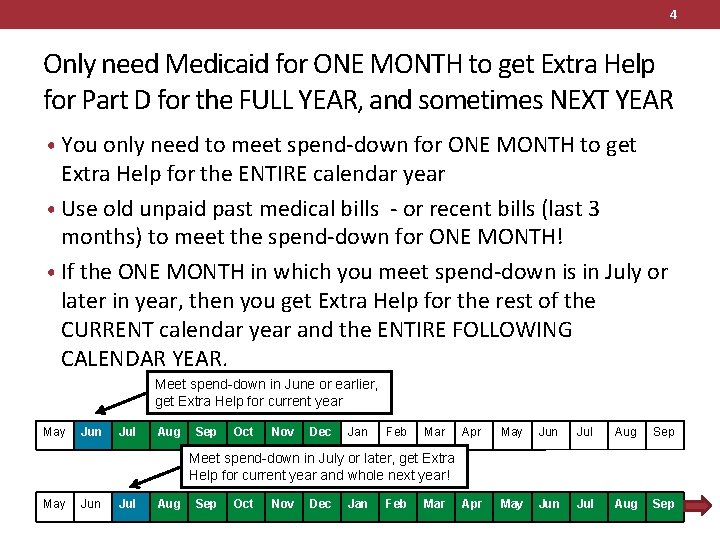
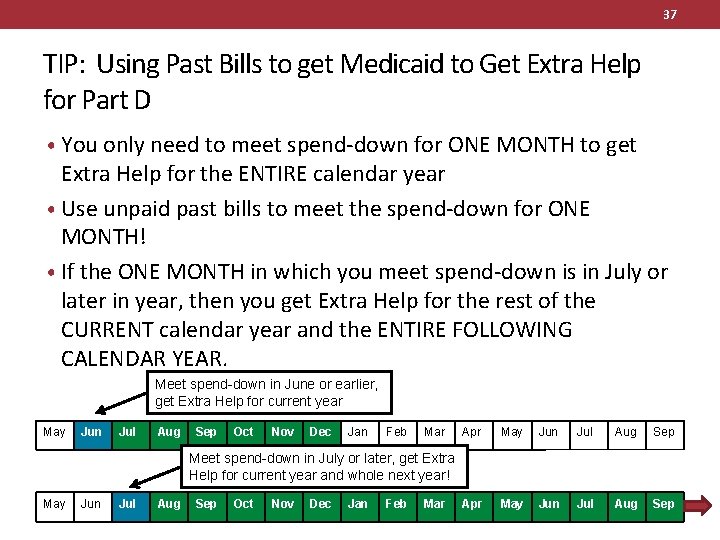
4 Only need Medicaid for ONE MONTH to get Extra Help for Part D for the FULL YEAR, and sometimes NEXT YEAR • You only need to meet spend-down for ONE MONTH to get Extra Help for the ENTIRE calendar year • Use old unpaid past medical bills - or recent bills (last 3 months) to meet the spend-down for ONE MONTH! • If the ONE MONTH in which you meet spend-down is in July or later in year, then you get Extra Help for the rest of the CURRENT calendar year and the ENTIRE FOLLOWING CALENDAR YEAR. Meet spend-down in June or earlier, get Extra Help for current year May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Apr May Jun Jul Aug Sep Meet spend-down in July or later, get Extra Help for current year and whole next year! May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar
5 Example: Helping Joyce in the Doughnut Hole with Past Bills • Joyce’s income is $1600/month, which is over $1357, the limit for both QI-1 Medicare Savings Program and Full Extra Help, and the $1507 limit for Partial Extra Help (2017). She is 58 so not eligible for EPIC. • She enrolled in an enhanced Part D plan (costing $45/month) and hit the doughnut hole by September. • She can’t work so can’t be MBI-WPD. She comes to you in October 2017. • Her Medicaid spend-down is $1600 - $845 = $755. Other than when she’s in the doughnut hole, her medical bills don’t meet her spend-down.
6 Spend-Down and Part D (cont’d) • You ask Joyce if she has any: • UNPAID medical bills from any time in the last 6 years, or • PAID medical bills from the past 3 calendar months • SHE SAYS YES – you go through them and see she has $1500 of unpaid bills, including bills from her Part D plan for mail order drugs she ordered before she realized she was in the doughnut hole.
7 Spend-Down and Part D (cont’d) • With the bills, she can meet the spend-down for the Application Month (November), December, and part of Jan. Explained more later. • TIP: Don’t forget to ask Joyce if she works even one hour per month. If she does, she might be eligible for MBI-WPD. Then, she would not have a spend down because the income limit for MBI-WPD is $2513/month.
8 Spend-Down and Part D (cont’d) • Even if the bills only meet ONE month’s spend-down: • If she had Medicaid for just one month after July, even if her Medicaid later stops, she gets Extra Help for the rest of the year and ALL of the following year. • Once she receives a Medicaid card or acceptance letter it is “Best Available Evidence”* for the Part D plan to bill the Full Extra Help copays to pay for her drugs now. If she’s not yet in a Part D plan, pharmacist bills Linet** (run by Humana) • Before Medicaid is accepted, while the application is pending, sweettalk her pharmacist to fill her prescriptions free. • If she isn’t yet in a Part D plan, pharmacist can back-bill LI-NET once Medicaid is approved. • If she was already on Part D, the “Extra Help” will be retroactive - up to 3 months before the application was filed -- and pharmacist can back-bill the Part D plan. She’d pay only Extra Help copays. *https: //www. cms. gov/medicare/prescription-drug-coverage/prescriptiondrugcovcontra/ best_available_evidence_policy. html ** Low income NET Program – see https: //www. cms. gov/Medicare/Eligibility-and. Enrollment/Low. Inc. Sub. Medicare. Pres. Cov/Medicare. Limited. Income. NET. html
9 Checklist – Add to Intake Questions • Ask Clients who have Excess Income or Resources: • Do you (or spouse) have any UNPAID medical bills from the past, even as long as 6 years ago? (Bill showing net amount due after Medicare paid). • Do you (or spouse) have any PAID medical bills from services received in the 3 calendar months before the current month? • Have you (or spouse) used EPIC or ADAP in the 3 calendar months before the current month, or in the current month?
10 BASICS OF SPEND-DOWN • Who can use Spend-down • How to Calculate the Spend-down • Which Bills Count • Using Past Medical Bills – or bills paid by EPIC - to meet Spend-down • Spend-down logistics – submit bills or pay-in • Hospital Inpatient rule
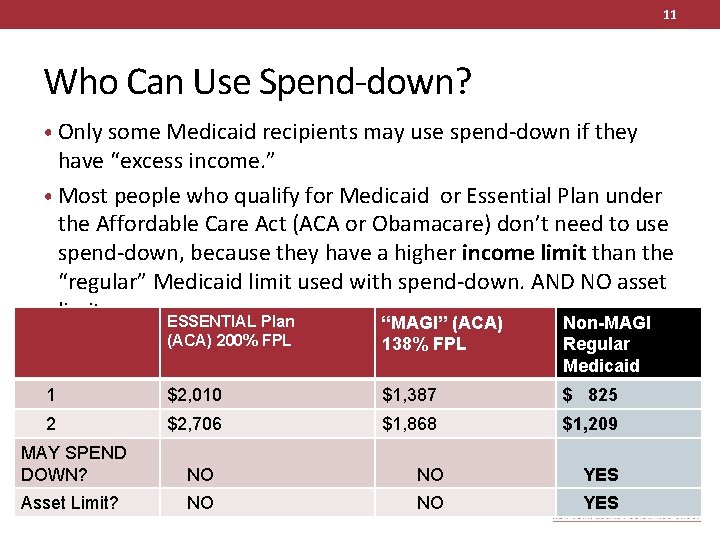
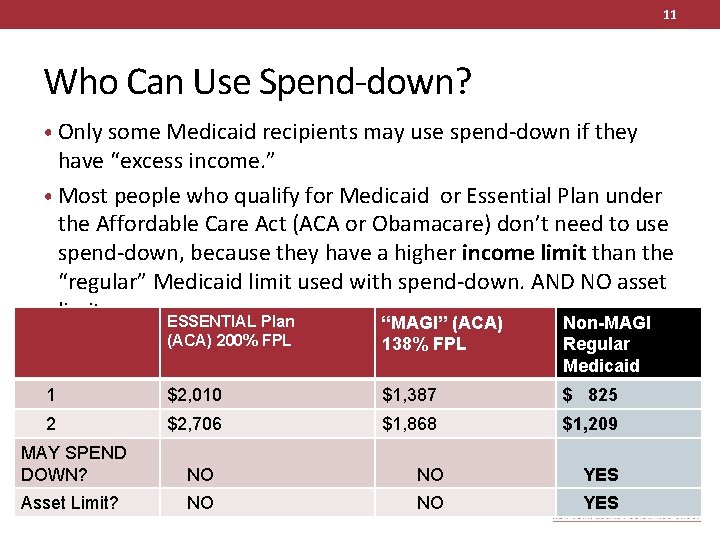
11 Who Can Use Spend-down? • Only some Medicaid recipients may use spend-down if they have “excess income. ” • Most people who qualify for Medicaid or Essential Plan under the Affordable Care Act (ACA or Obamacare) don’t need to use spend-down, because they have a higher income limit than the “regular” Medicaid limit used with spend-down. AND NO asset limit. ESSENTIAL Plan “MAGI” (ACA) Non-MAGI (ACA) 200% FPL 138% FPL Regular Medicaid 1 $2, 010 $1, 387 $ 825 2 $2, 706 $1, 868 $1, 209 MAY SPEND DOWN? NO NO YES Asset Limit? NO NO YES
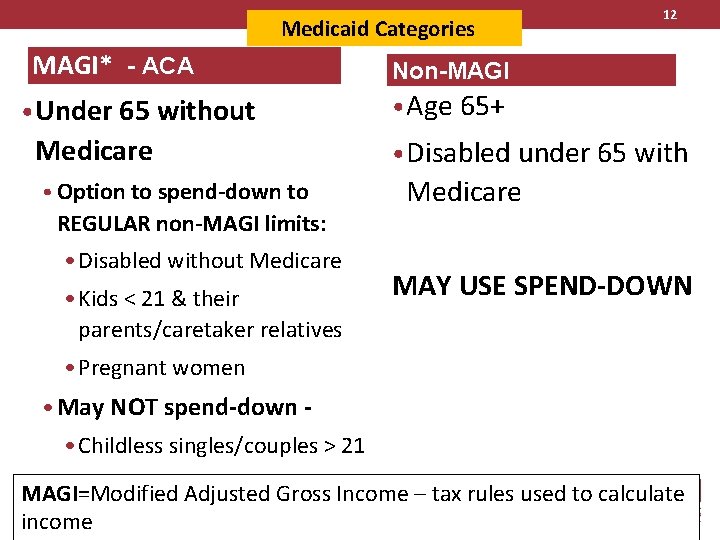
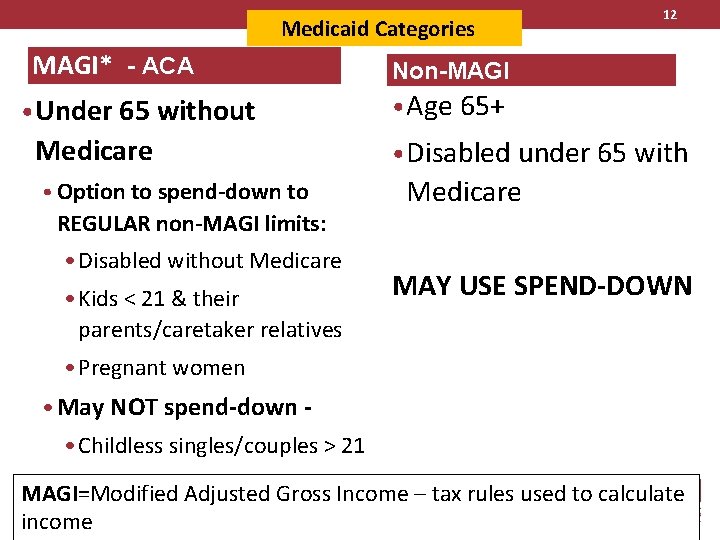
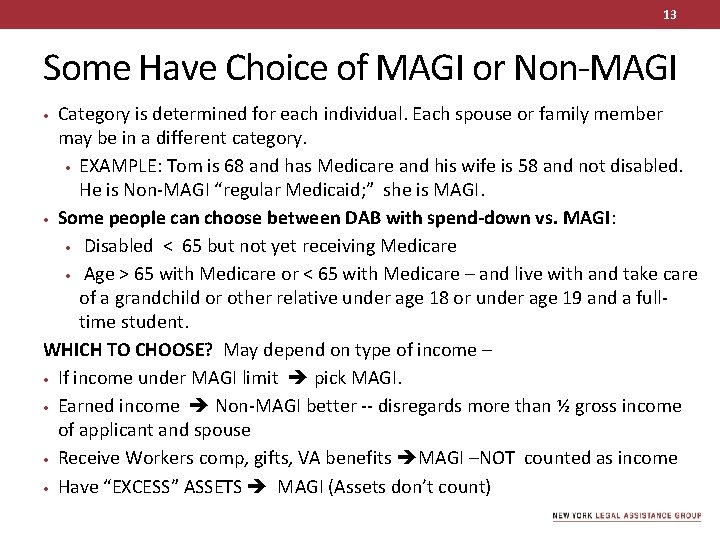
Medicaid Categories MAGI* - ACA • Under 65 without Medicare • Option to spend-down to REGULAR non-MAGI limits: • Disabled without Medicare • Kids < 21 & their parents/caretaker relatives 12 Non-MAGI • Age 65+ • Disabled under 65 with Medicare MAY USE SPEND-DOWN • Pregnant women • May NOT spend-down - • Childless singles/couples > 21 MAGI=Modified Adjusted Gross Income – tax rules used to calculate income
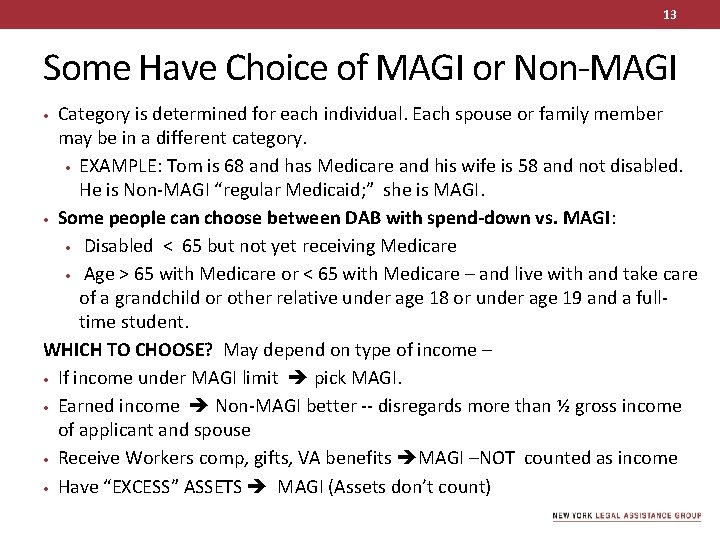
13 Some Have Choice of MAGI or Non-MAGI Category is determined for each individual. Each spouse or family member may be in a different category. • EXAMPLE: Tom is 68 and has Medicare and his wife is 58 and not disabled. He is Non-MAGI “regular Medicaid; ” she is MAGI. • Some people can choose between DAB with spend-down vs. MAGI: • Disabled < 65 but not yet receiving Medicare • Age > 65 with Medicare or < 65 with Medicare – and live with and take care of a grandchild or other relative under age 18 or under age 19 and a fulltime student. WHICH TO CHOOSE? May depend on type of income – • If income under MAGI limit pick MAGI. • Earned income Non-MAGI better -- disregards more than ½ gross income of applicant and spouse • Receive Workers comp, gifts, VA benefits MAGI –NOT counted as income • Have “EXCESS” ASSETS MAGI (Assets don’t count) •
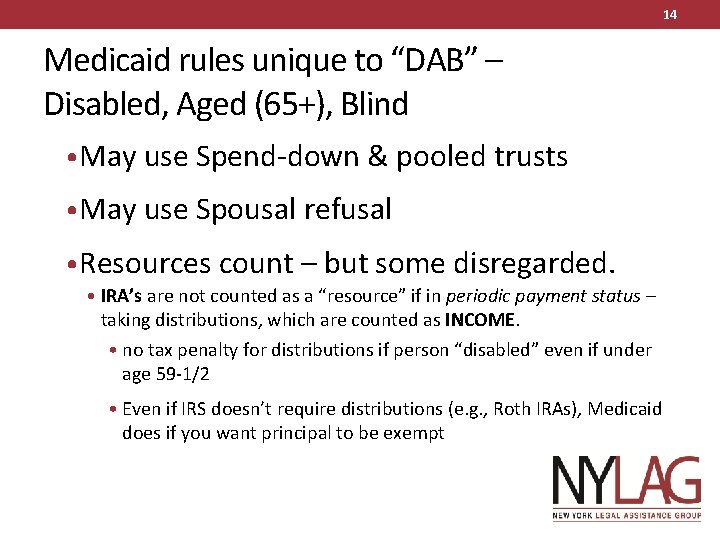
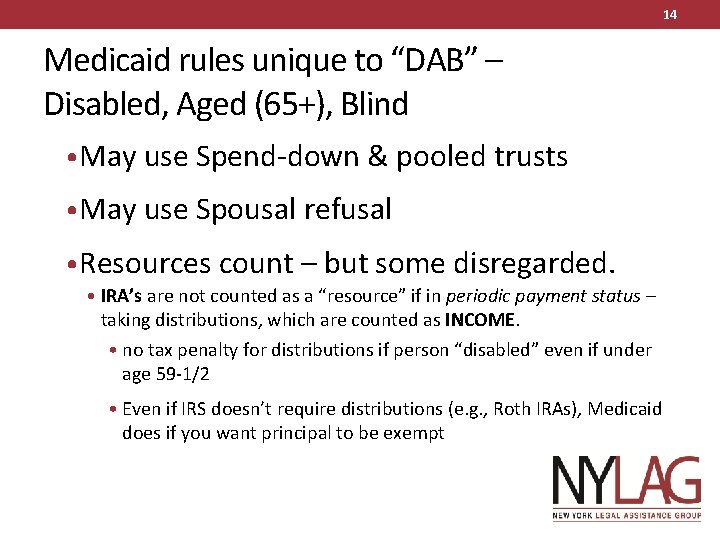
14 Medicaid rules unique to “DAB” – Disabled, Aged (65+), Blind • May use Spend-down & pooled trusts • May use Spousal refusal • Resources count – but some disregarded. • IRA’s are not counted as a “resource” if in periodic payment status – taking distributions, which are counted as INCOME. • no tax penalty for distributions if person “disabled” even if under age 59 -1/2 • Even if IRS doesn’t require distributions (e. g. , Roth IRAs), Medicaid does if you want principal to be exempt
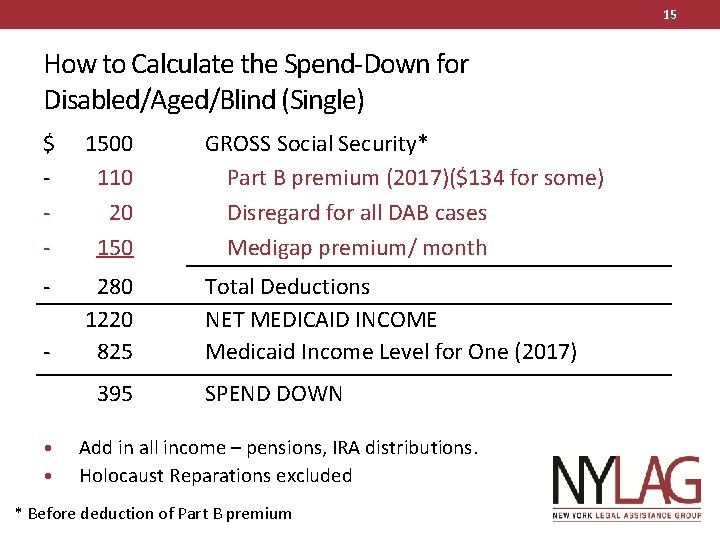
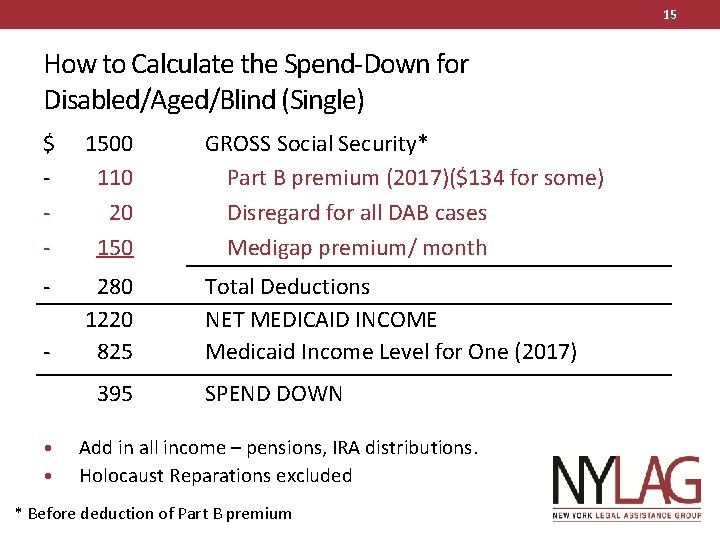
15 How to Calculate the Spend-Down for Disabled/Aged/Blind (Single) $ - 1500 110 20 150 GROSS Social Security* Part B premium (2017)($134 for some) Disregard for all DAB cases Medigap premium/ month - 280 1220 825 Total Deductions NET MEDICAID INCOME Medicaid Income Level for One (2017) - 395 • • SPEND DOWN Add in all income – pensions, IRA distributions. Holocaust Reparations excluded * Before deduction of Part B premium
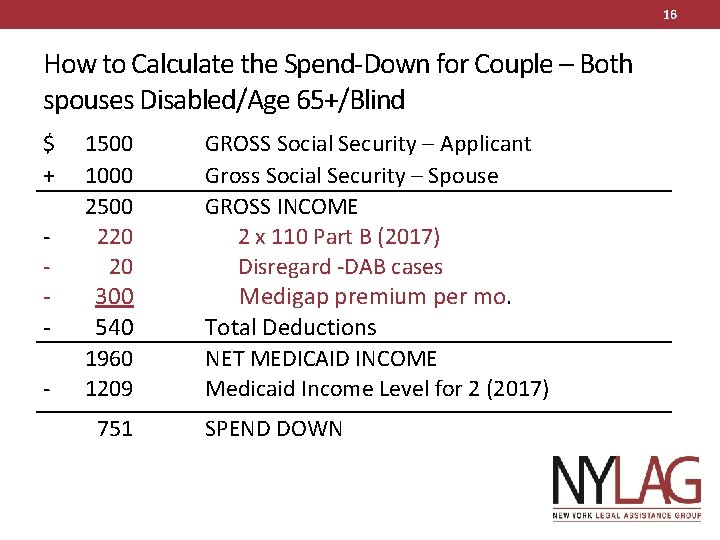
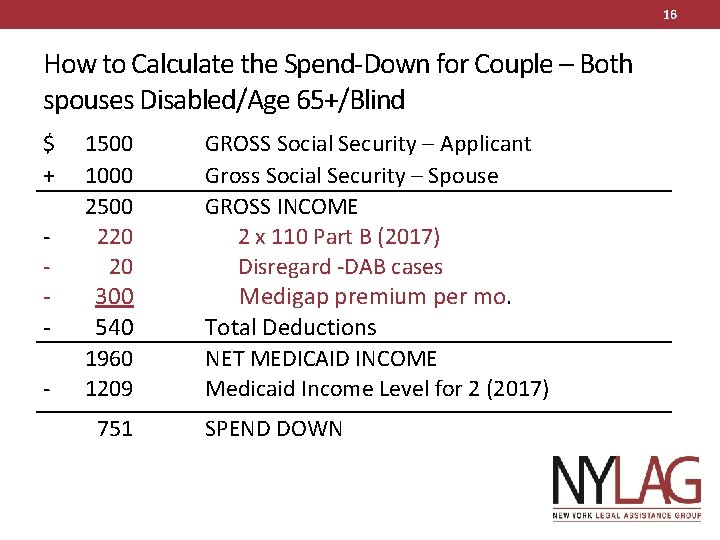
16 How to Calculate the Spend-Down for Couple – Both spouses Disabled/Age 65+/Blind $ + - 1500 1000 2500 220 20 300 540 1960 1209 751 GROSS Social Security – Applicant Gross Social Security – Spouse GROSS INCOME 2 x 110 Part B (2017) Disregard -DAB cases Medigap premium per mo. Total Deductions NET MEDICAID INCOME Medicaid Income Level for 2 (2017) SPEND DOWN
17 Spousal Refusal • If spouse does not need or qualify for Medicaid, client may apply alone if spouse “refuses” to make income/resources available for medical care. • With Spousal Refusal, budget is the same as the Single Budget Example – Spend down is $395 (Slide 8) instead of $752 (slide 9) • County has right to sue “refusing” spouse for support. Each county/NYC has different policy on who they sue. • NYC won’t sue if assets under $74, 820, income under $3, 022/mo. • NYC form can be used as a model – posted at http: //wnylc. com/health/download/66/
18 These basic budgets get more complicated if: • Client or spouse works – $65 + 1/2 of remainder of gross monthly earned income is deducted – so spend down is lower • “Mixed” Couple – The couple budget on slide 9 is used only if client AND spouse are BOTH Disabled, Aged 65+, or Blind (DAB category). • If non-applying spouse is MAGI, then different. • If client lives with and takes care of a child under 21 who is related to client, such as a grandchild, budget could be different
19 Special Situations Can Eliminate Spend-down 1. Under age 65, disabled, and able to work, even a minimal amount? Dog walker, child care, filing, even for a friend or neighbor – Medicaid Buy-In for Working People with Disabilities – MBI-WPD. Income limit $2, 513 (2017). See http: //www. wnylc. com/health/entry/59/ 2. Was client in a nursing home or adult home for more than 30 days, Medicaid paid for part of stay, and returning home in MLTC plan? May get Special Income Standard for Housing Expenses – can increase income limit up to $1, 285/month. Amount varies by region. See http: //www. wnylc. com/health/entry/212/. 3. Married MLTC member – if spouse not on Medicaid – spousal impoverishment protections may eliminate spenddown. See http: //www. wnylc. com/health/entry/165/
How to Meet the Spend-Down 20
21 Does a bill have to be paid to count toward the spend-down? NO • A bill only needs to be incurred to count toward the spend- down. An expense is incurred on the date of the medical service, not the date of the bill. 18 NYCRR 360 -4. 8(c), NYS DOH MRG 241 http: //www. health. ny. gov/health_care/medicaid/reference/mrg/
22 Whose bills can meet the spend-down? • The Medicaid recipient’s bills AND • The spouse’s bills, even if spouse is not applying for Medicaid. But if the spouse does a “spousal refusal, ” then you may not use his or her bills. • Bills for any dependent child under 21.
23 What bills can be used to meet spend-down? • Any medical bills not covered by insurance – such as deductibles and coinsurance for Medicare, Part D, or other private health insurance, and Medicaid copayments. • Services not covered by Medicaid that are medically necessary: • Chiropractors, podiatrists, drugs a Part D plan won’t cover, bills of doctors who don’t take Medicaid • Over the Counter Items – (vitamins, lotions) with a doctor’s note explaining medical necessity & receipts • PAST paid or unpaid medical bills – more later • EPIC or ADAP expenses – more later
24 How old can bills be for meeting the spenddown? • A new applicant may use past medical bills to meet their spend-down when applying for Medicaid. • How old the bills may be depends on whether the bills are PAID or UNPAID. • Once a new applicant’s past bills have been “used up, ” s/he may only use bills incurred in the current month to meet the spend-down for that month.
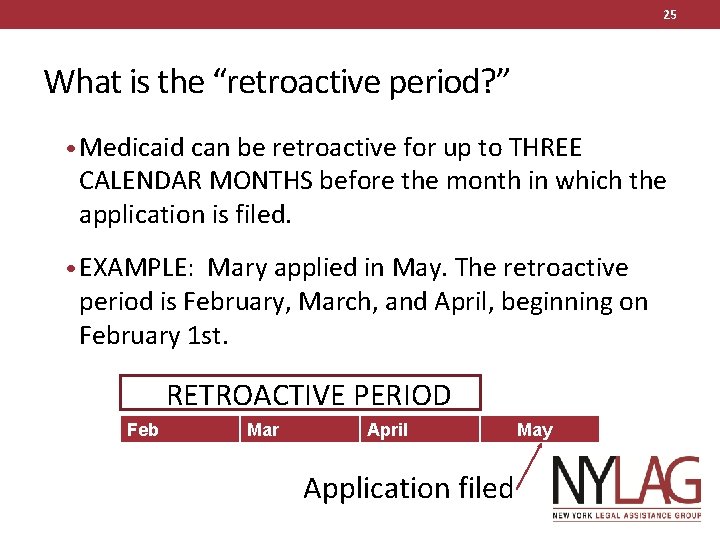
25 What is the “retroactive period? ” • Medicaid can be retroactive for up to THREE CALENDAR MONTHS before the month in which the application is filed. • EXAMPLE: Mary applied in May. The retroactive period is February, March, and April, beginning on February 1 st. Re RETROACTIVE PERIOD Feb Mar April Application filed May
26 Medical bills in 3 -month retroactive period – what will Medicaid do? • For medical services received during the retroactive period, if the bill is: • PAID – Medicaid can EITHER: • Reimburse the client or whoever paid the bill, IF the client was eligible for Medicaid during the retroactive period (assets within limits). • Credit the bill against the Spend-down. See below re which month the credit is used for • UNPAID – Medicaid can PAY the bill directly to the provider, if the provider accepts Medicaid
27 Using Past Paid vs. Unpaid Medical Bills for Spenddown • PAID bills can be used to meet the spend-down only if the services were provided and paid for in the retroactive period – the 3 calendar months before the month of application or during the application. • UNPAID bills can be used even if they are many years old as long as they are viable, meaning provider may still sue to collect them (rule of thumb is six years old)
28 PAID BILL Example • Marvin paid $3500 for dental surgery in October Year 1. He comes to you in December Year 1 wanting to apply for Medicaid (or needing Extra Help). He has a $500 spenddown. • HRA/DSS must receive his application by Jan. 31 st of Year 2 if he wants to use that paid bill to meet the spend-down or if he wants it reimbursed. • Don’t forget - he must either be over age 65, blind or disabled, or have a child/grandchild living with him to use spend-down
29 PAID bills can meet spend-down for up to SIX months • Marvin’s $3500 of bills would cover 7 months of his spend- down @ $500/month. However, a PAID bill may only cover up to six consecutive months of spend-down. • Marvin’s Jan. 18 application should be approved for six months of Medicaid through June 2018. He may not carry the balance of $500 of the dental bill forward to meet spenddown for July 2018. • See more spend-down materials at http: //wnylc. com/health/entry/46/
30 Recent past bills • Bills incurred in the retroactive period – the 3 calendar months before the month of application – may be paid or reimbursed OR be used to meet the current spend-down. It is client’s choice. • Client may want to mix it up – use some bills for spend-down credit, and get some bills paid or reimbursed. This is client’s choice. It gets complicated. • For more info see 96 -ADM-15* and more info on spend-down at http: //wnylc. com/health/entry/46/ *Posted at http: //www. health. state. ny. us/health_care/medicaid/publications/pub 1996 adm. htm
31 Bills PAID by EPIC or ADAP may meet spenddown • Bills paid by EPIC or ADAP in the 3 months before the month client applied for Medicaid, plus during the time the Medicaid application is processed, can be used to meet the spend-down for the first month of Medicaid and for up to the 1 st 6 months of Medicaid. • The amount EPIC or ADAP pays, not just client’s co-payment, counts toward the spend-down. 91 ADM-11, 18 NYCRR § 360 -4. 8(c)(1), MRG p. 239
32 EPIC How-To & Example • Sandy applied for Medicaid in April. • You wrote to EPIC asking for a printout of expenses paid by EPIC and the amount of his co-pays since January of the same year– the 3 -month period before the application, plus up date • WRITE TO: EPIC, POB 15018 Albany, NY 12212 or call 1 -800 - 332 -3742 • Include a HIPAA release with your letter. HIPPA release at http: //wnylc. com/health/download/267/ • Alternately, sometimes the pharmacy can give you a printout showing EPIC’s payments.
33 EPIC Example (cont’d) • EPIC’s printout shows total payments were $2000, including client EPIC copayments of $600. Spend-down is $600/mo. • Since EPIC bills are PAID, they can be used to meet the spend- down for up to 6 months. The $2000 in bills meet the spenddown for 3+ months. He has additional bills to meet the spenddown for the 4 th month. You request to start the 4 -month period in the month of application. • What if the EPIC paid bills total $5000? $600 x 6 = $3600 would be used to meet the spend-down for 6 months. $1400 of remaining bills cannot be carried over to later months.
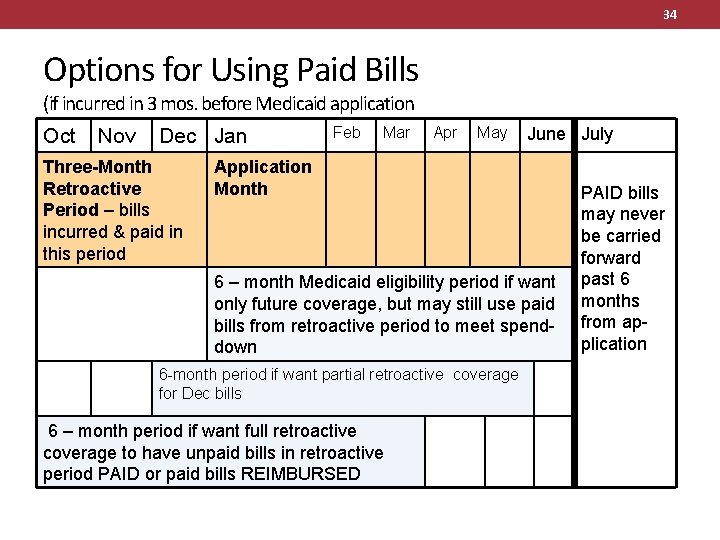
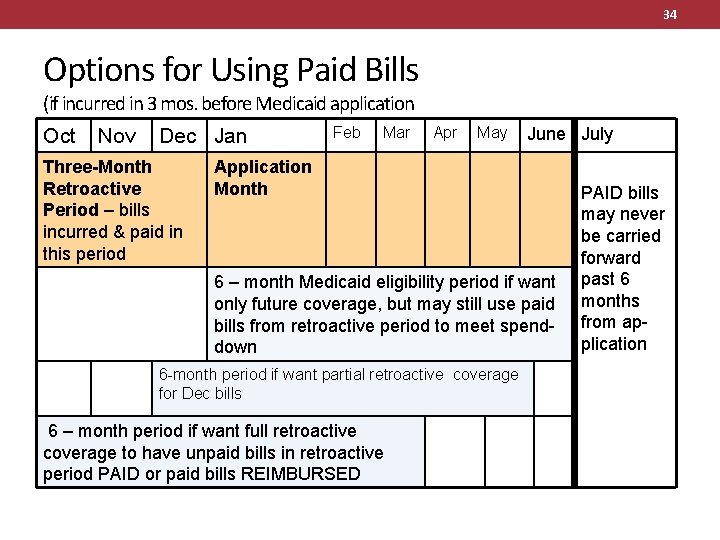
34 Options for Using Paid Bills (if incurred in 3 mos. before Medicaid application Oct Nov Dec Jan Three-Month Retroactive Period – bills incurred & paid in this period Feb Mar Apr May June July Application Month 6 – month Medicaid eligibility period if want only future coverage, but may still use paid bills from retroactive period to meet spenddown 6 -month period if want partial retroactive coverage for Dec bills 6 – month period if want full retroactive coverage to have unpaid bills in retroactive period PAID or paid bills REIMBURSED PAID bills may never be carried forward past 6 months from application
35 Using Unpaid Bills to Meet the Spend-Down • UNPAID bills are better for meeting the Spend-Down than PAID bills • Unpaid bills incurred years earlier can be used to meet the spend-down, as long as they are “viable, ” meaning the provider is still trying to collect them. A current collection letter or bill is enough to show this. Rule of thumb is SIX YEARS. • The unpaid bills can be carried forward indefinitely, past 6 months. Marvin could have used the $3500 in dental and other bills to meet his $500 spend-down for 7 months if they were unpaid.
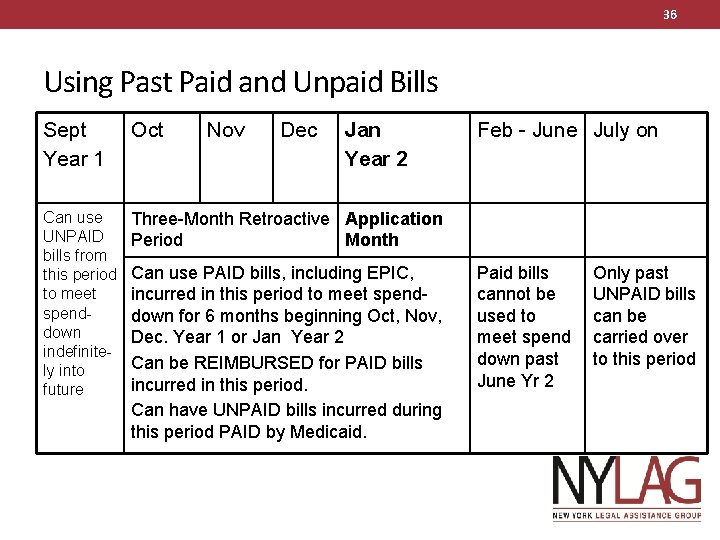
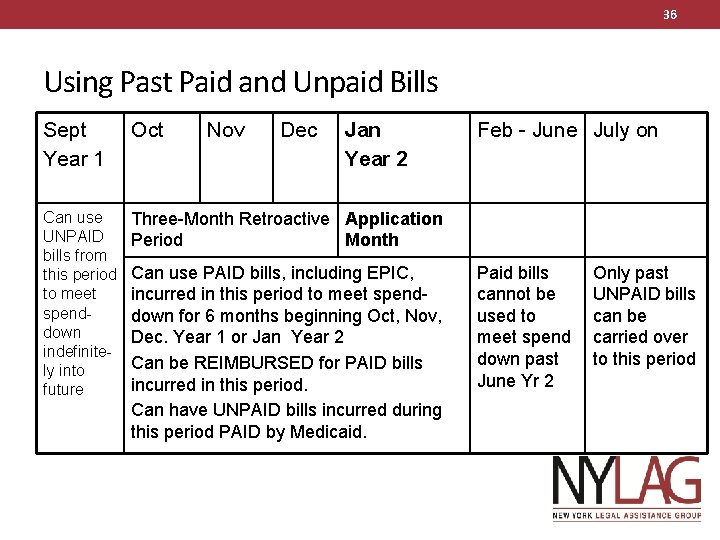
36 Using Past Paid and Unpaid Bills Sept Year 1 Oct Nov Dec Jan Year 2 Can use UNPAID bills from this period to meet spenddown indefinitely into future Three-Month Retroactive Application Period Month Can use PAID bills, including EPIC, incurred in this period to meet spenddown for 6 months beginning Oct, Nov, Dec. Year 1 or Jan Year 2 Can be REIMBURSED for PAID bills incurred in this period. Can have UNPAID bills incurred during this period PAID by Medicaid. Feb - June July on Paid bills cannot be used to meet spend down past June Yr 2 Only past UNPAID bills can be carried over to this period
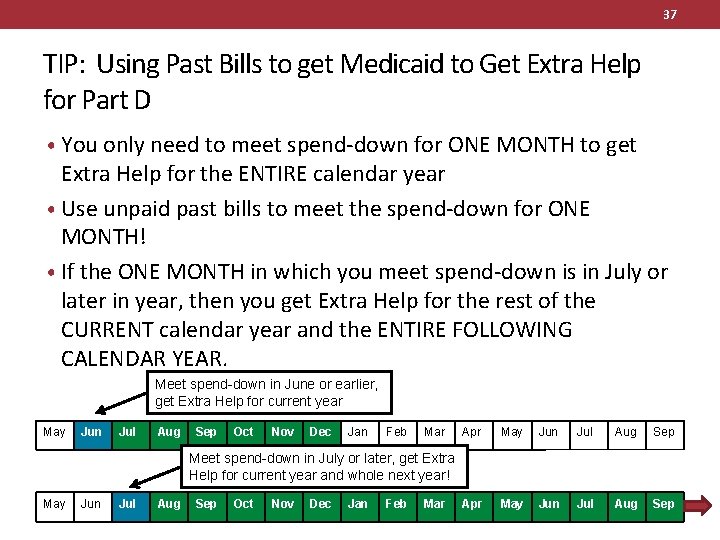
37 TIP: Using Past Bills to get Medicaid to Get Extra Help for Part D • You only need to meet spend-down for ONE MONTH to get Extra Help for the ENTIRE calendar year • Use unpaid past bills to meet the spend-down for ONE MONTH! • If the ONE MONTH in which you meet spend-down is in July or later in year, then you get Extra Help for the rest of the CURRENT calendar year and the ENTIRE FOLLOWING CALENDAR YEAR. Meet spend-down in June or earlier, get Extra Help for current year May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Apr May Jun Jul Aug Sep Meet spend-down in July or later, get Extra Help for current year and whole next year! May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar
38 Special Hospital Inpatient Stay Rule • Medicaid requires a higher spend-down for inpatient hospital stays. Even if just hospitalized for one night, client is charged SIX times the monthly spend-down before Medicaid pays. • EXAMPLE: The Medicare hospital deductible will be $1, 316 (2017). Client does not have Medigap to pay this. Spend-down is $100/month. • Medicaid will pay only $716 of the $1316 bill, client is charged 6 x $100 = $600. If client needs Medicaid in the community for those 6 months, the spend-down is already met with this bill.
39 Logistics of Spend-Down • Submitting Bills • Pay-In
40 Submitting Bills Month-to-Month • Bringing in past paid or unpaid bills at the application will get Medicaid activated for as much as 6 months at a time, if there are enough past bills. • After the past bills are used up, Medicaid recipients must bring or fax proof of medical bills incurred during the current month, equal to the spend-down amount, to the local Medicaid office each month. The Medicaid office then activates Medicaid for that month only. This must be repeated monthly. • NYC - BILLS MAY BE FAXED to 917 -639 -0645. Use fax cover form at http: //wnylc. com/health/entry/55/.
41 Submitting Bills Month-to-Month • If applicant does not show enough bills to meet their spend- down initially, they are only provisionally eligible until they bring medical bills that meet the spend-down, and Medicaid is activated. If Medicaid is not activated within 3 -4 months, they must re-apply. • SOME PROVIDERS HELP – Some Certified Home Health agencies and other providers help clients keep Medicaid activated by sending bills directly to the Medicaid office that meet the spend-down. • All PCA, MLTC, dialysis and waiver clients in NYC have Medicaid activated automatically.

42 Pay-In Program • The Pay-In Program allows clients to pre-pay their spend-down to Medicaid for a period of One to Six months. Once paid, their Medicaid is activated for this period. They even get their money back if they end up not using Medicaid services equal to the spend-down. • The Pay-In Program is best for people with a low spend-down so that they can afford to pay 3 -6 months at a time – it’s too much trouble to bring in medical bills, or use Pay-In, every month; or • To enroll in Pay-In with HRA/DSS. NYC forms see http: //www. wnylc. com/health/download/175/ and http: //www. wnylc. com/health/download/174/ MRG p. 248 (See last slide for link)
43 RESOURCE SPEND-DOWB
44 Spending Down Excess Resources • Spend-down is not only for excess Income. It can also be used if one’s Resources are over the Medicaid limit. • EXAMPLE • Jerry is age 65 has $20, 080 in the bank. He also has a $1500 burial fund and pre-paid funeral agreement. His resources are $4, 000 over the $14, 580 resource limit (2013). He has an income spend-down of $500/mo. • Jerry is hospitalized. Medicaid will pay his hospital bill above $ 7000: $4000 excess resources + 6 x $500 excess income. • Past unpaid or paid medical bills can be applied to offset the resource spend-down, just like excess income.
45 More about Resource Spend-Down • Only Age 65+, Disabled, Blind or children < 21 & their caregiver relatives may use Resource Spend-down, just like Income Spend -down. If Jerry was not 65+ or disabled, and has no child/other relative under 21 living with him, he could not spend-down. If was < 65 he could be MAGI with no resource test. • If Medicaid is not needed until the following month, it is better to do Medicaid planning, i. e. transfer assets (with legal advice), spend resources on other needs. This is because with Resource Spend-down, you may only spend-down on Medical Care, not pay rent or buy other things. • EX: Jerry applies in May with $2000 excess resources. Even though he owes $2000 in back rent, he can’t spend-down the excess savings on the rent bill. Only on medical bills.
46 ANOTHER CASE EXAMPLE EPIC and past medical bills meet Spend-down
47 Helping Carol – age 75 • Carol is 75, with income of $1800/mo. She needs Medicaid for home care & “Extra Help. ” Family has been private paying home care $1500/mo. and would like to be reimbursed if possible. She comes to you in May 2013. • You ask if she has Medigap – Her AARP premium $250/mo. brings her spend-down to $ 625.
48 Helping Carol – age 75 • Does she have EPIC or other medical bills to meet the spend-down? • She has EPIC – you write for a printout that says EPIC payments plus her copays total $1000 since 2/1/13. • She has another $500 in paid medical bills since 2/1/13 – coinsurance, etc. • Application is filed in May, is approved and she starts receiving Medicaid home care in July 2013.
49 More Carol – Using EPIC bills for spend-down • The $1500 in EPIC/medical bills can be used to meet Carol’s spend-down for 2 months EITHER beginning: • With month she applied for Medicaid, in May 2013 OR • Back to February, March or April 2013, if her resources were within the limits. Family could be reimbursed for private paid home care in these months, after deducting spenddown. The past EPIC bills would meet the spenddown for 2 of the months. • For more information on reimbursement see http: //wnylc. com/health/entry/18/
50 Helping Carol – going forward • Going forward, you recommend that Carol enrolls in a pooled trust to eliminate her spend-down. See fact sheet at http: //wnylc. com/health/entry/44/ • You counsel her on whether she needs to keep the Medigap policy, since Medicaid is now like a Medigap. By joining the trust, she may no longer need the Medigap as a deduction – she can simply increase her deposit to the trust. But she may want to keep it because her doctors don’t accept Medicaid. • FOR MORE info on trusts see http: //wnylc. com/health/14/
51 Checklist • Ask Clients who have Excess Income or Resources: • Do you (or spouse) have any UNPAID medical bills from the past, even as long as 6 years ago? (Bill showing amount due after Medicare paid counts). • Do you (or spouse) have any PAID medical bills from services received in the 3 calendar months before the current month? • Have you (or spouse) used EPIC or ADAP in the 3 calendar months before the current month, or in the current month?
52 Advocacy resources/bookmarks • NYS DOH Medicaid Reference Guide (MRG) • http: //www. health. ny. gov/health_care/medicaid/reference/mrg/ • Spend-down is at INCOME section pp. 239 -249 • NYS DOH Administrative Directives, etc. • http: //www. health. ny. gov/health_care/medicaid/publications/ • Key Spend-down Directive is 96 -ADM-15 • Directives before 1996 are on http: //onlineresources. wnylc. net/pb/default. asp • EPIC spend-down directive is 91 -ADM-11 http: //onlineresources. wnylc. net/pb/docs/91_adm-11. pdf
53 Advocacy resources/bookmarks • Medicaid income/resource charts updated and posted at • http: //www. nyc. gov/html/hra/downloads/pdf/income_level. pdf • http: //www. health. state. ny. us/health_care/medicaid/ • NY Health Access – http: //nyhealthaccess. org • Pathways to Extra Help http: //wnylc. com/health/entry/46/ • Pooled Trusts http: //wnylc. com/health/14/ • Spenddown & Medicaid Financial rules: http: //wnylc. com/health/12/ • Medicaid Buy-In for Working People with Disabilities – MBI-WPD http: //www. wnylc. com/health/entry/59/ • Special Income Standard for Housing Expenses if discharged from nursing home/adult home and enroll in MLTC http: //www. wnylc. com/health/entry/212/. • Spousal impoverishment protections where 1 spouse in MLTC or “Immediate Need” home care and other not on Medicaid or not in MLTC See http: //www. wnylc. com/health/entry/165/