Mechanisms of Sports Trauma Tissue Response to Injury


- Slides: 34

Mechanisms of Sports Trauma & Tissue Response to Injury
Mechanical Injury Trauma is defined as physical injury or wound, produced by internal or external force Mechanical injury results from force or mechanical energy that changes state of rest or uniform motion of matter
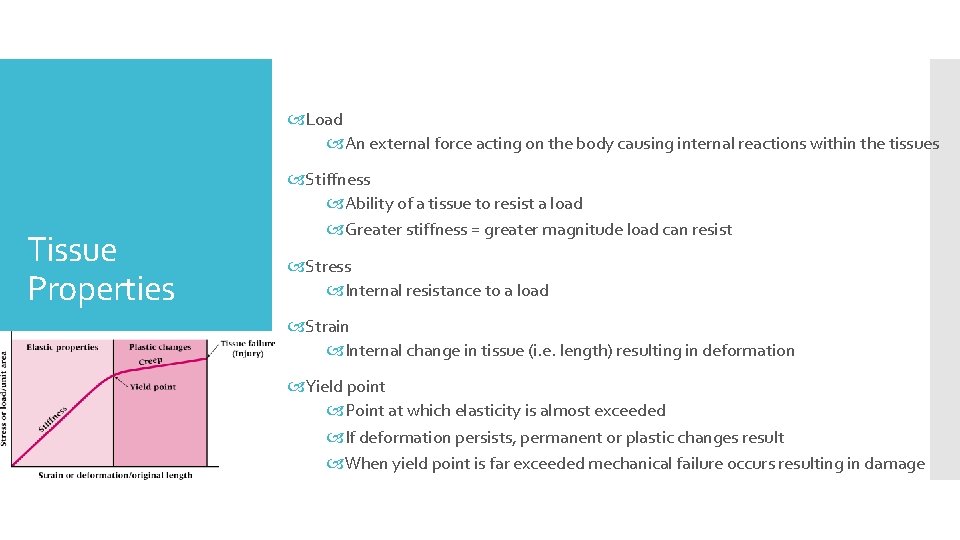
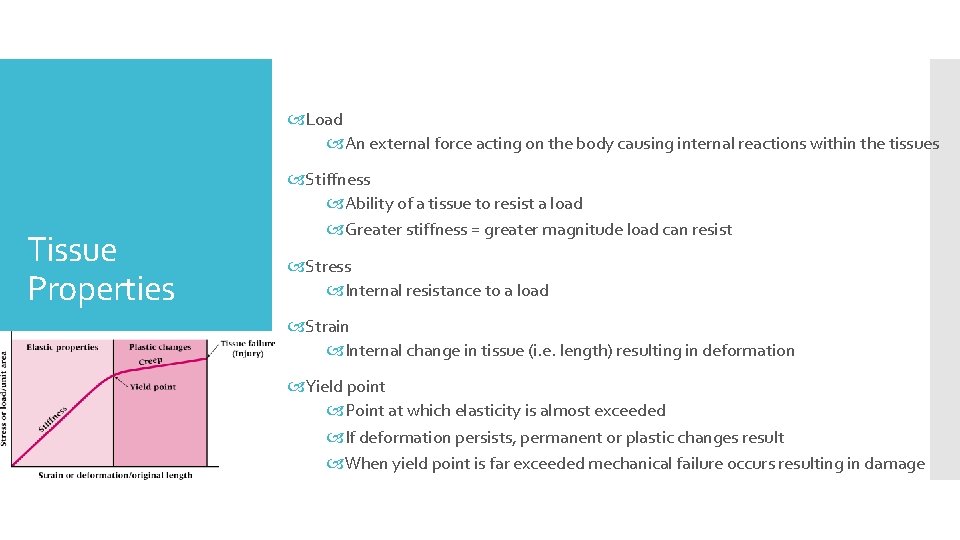
Load An external force acting on the body causing internal reactions within the tissues Tissue Properties Stiffness Ability of a tissue to resist a load Greater stiffness = greater magnitude load can resist Stress Internal resistance to a load Strain Internal change in tissue (i. e. length) resulting in deformation Yield point Point at which elasticity is almost exceeded If deformation persists, permanent or plastic changes result When yield point is far exceeded mechanical failure occurs resulting in damage
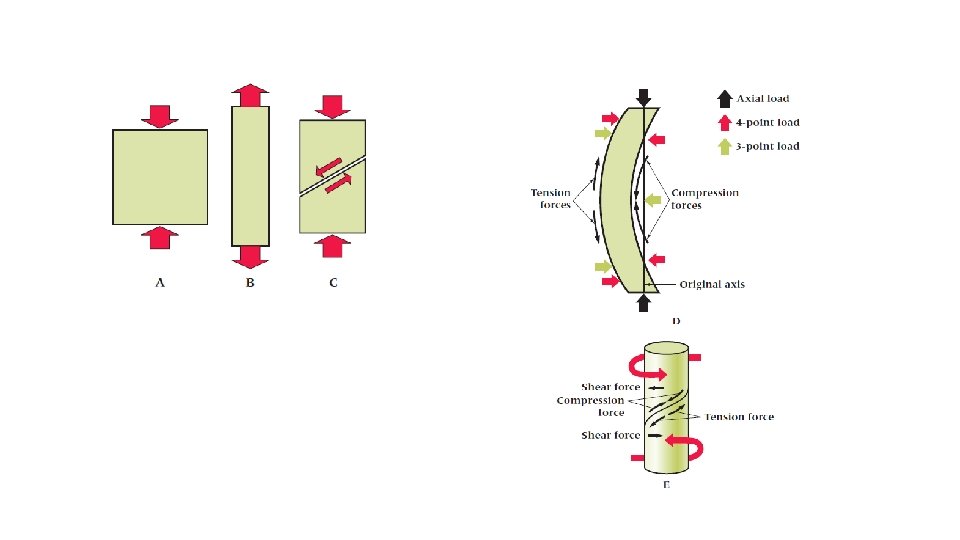
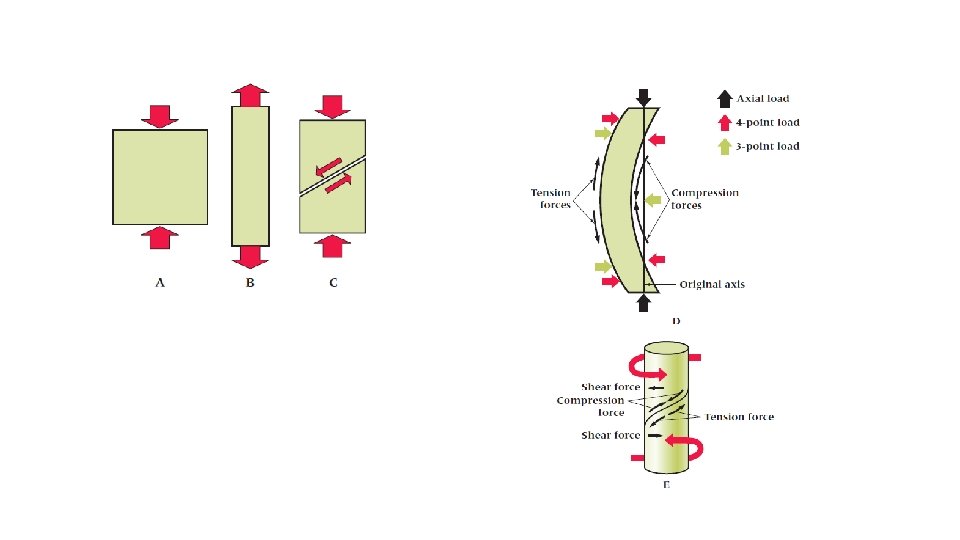
Tension Force that pulls and stretches tissue apart Compression Force that results in tissue being crushed – two forces applied towards one another Shearing Force that moves across the parallel organization of tissue Tissue Loading Bending Two force pairs act at opposite ends of a structure (4 points) Three forces cause bending (3 points) Already bowed structures encounter axial loading Torsion Loads caused by twisting in opposite directions from opposite ends Shear stress encountered will be perpendicular and parallel to the loads
When injury is acute – something has initiated the injury process Traumatic v. Overuse Injury becomes chronic when it doesn’t properly heal Could define relative to mechanism Traumatic (i. e. a direct blow) vs. Overuse (i. e. repetitive dynamic use over time)
Muscle Strains: Stretch, tear or rip to muscle or adjacent tissue May range from minute separation of connective tissue to complete tendinous avulsion or muscle rupture Muscle Strain Grades Musculotendinous Injuries Grade I - some fibers have been stretched or actually torn resulting in tenderness and pain on active ROM, movement painful but full range present Grade II - number of fibers have been torn and active contraction is painful, usually a depression or divot is palpable, some swelling and discoloration result Grade III- Complete rupture of muscle or musculotendinous junction, significant impairment, with initially a great deal of pain that diminishes due to nerve damage Time required for healing may be lengthy Often involves large, force-producing muscles Treatment and recovery may take 6 -8 weeks depending on severity Return to play too soon could result in re-injury
Muscle Cramps: Painful involuntary skeletal muscle contraction Muscle Guarding: Involuntary muscle contraction in response to pain following injury Following injury, muscles within an effected area contract to splint the area in an effort to minimize pain through limitation of motion Muscle Spasm: A reflex reaction caused by trauma Muscle Soreness: Overexertion in strenuous exercise resulting in muscular pain Musculotendinous Injuries Generally occurs following participation in activity that individual is unaccustomed AOMS/DOMS Tendon Injuries Wavy parallel collagenous fibers organized in bundles Tears generally occur in muscle and not tendon Repetitive stress on tendon will result in microtrauma and elongation Results in weakness
Tendinitis: Gradual onset, with diffuse tenderness due to repeated microtrauma and degenerative changes Without proper healing condition may begin to degenerate and be referred to as tendinosis Tenosynovitis: Inflammation of synovial sheath Myofascial Trigger Points: Discrete, hypersensitive nodule within tight band of muscle or fascia Musculotendinous Injuries Classified as latent or active Develop as the result of mechanical stress Latent trigger point Does not cause spontaneous pain Active trigger point Causes pain at rest Tender to palpation with referred pain Contusions: Result of sudden blow to body Atrophy: wasting away of muscle due to immobilization, inactivity, or loss of nerve functioning
Ligament Sprains: Result of traumatic joint twist that causes stretching or tearing of connective tissue Grade I - some pain, minimal loss of function, no abnormal motion, and mild point tenderness Grade II - pain, moderate loss of function, swelling, and instability with tearing and separation of ligament fibers Grade III - extremely painful, inevitable loss of function, severe instability and swelling, and may also represent subluxation Synovial Joint Injuries Subluxation: Partial dislocations causing incomplete separation of two bones Dislocation: Occurs when at least one bone in a joint is forced out of alignment and must be manually or surgically reduced Osteoarthritis: Wearing away of hyaline cartilage as a result of normal use Bursitis Bursa are fluid filled sacs that develop in areas of friction Sudden irritation cause acute bursitis, while overuse and constant external compression cause chronic bursitis
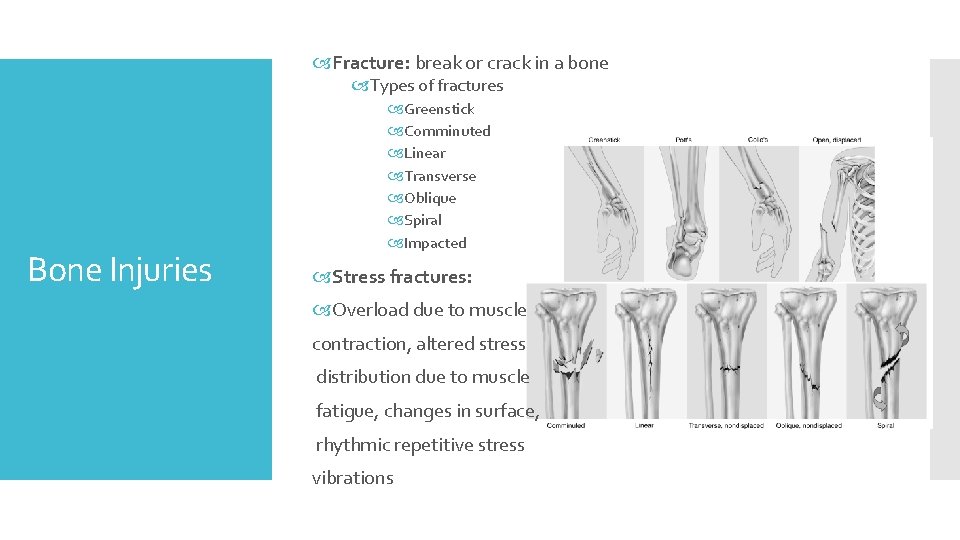
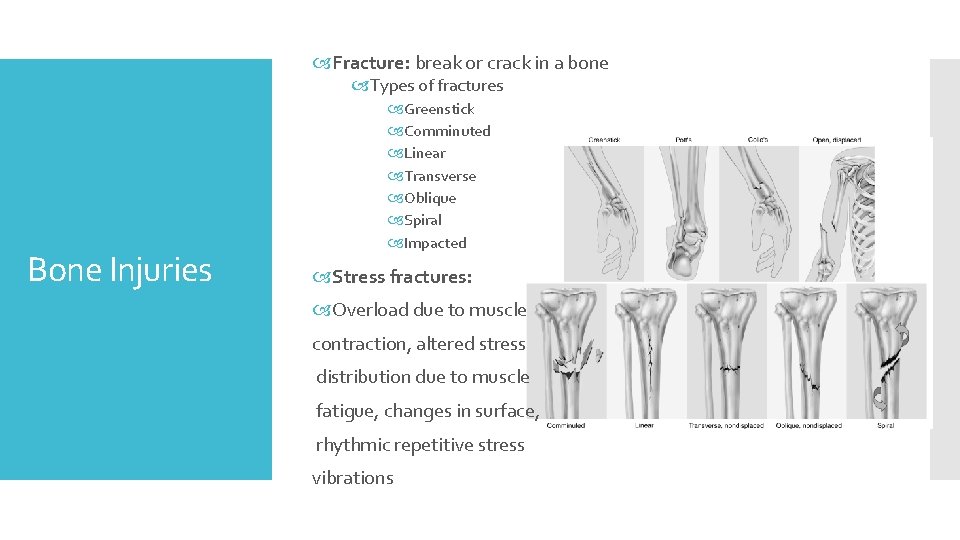
Fracture: break or crack in a bone Types of fractures Bone Injuries Greenstick Comminuted Linear Transverse Oblique Spiral Impacted Stress fractures: Overload due to muscle contraction, altered stress distribution due to muscle fatigue, changes in surface, rhythmic repetitive stress vibrations
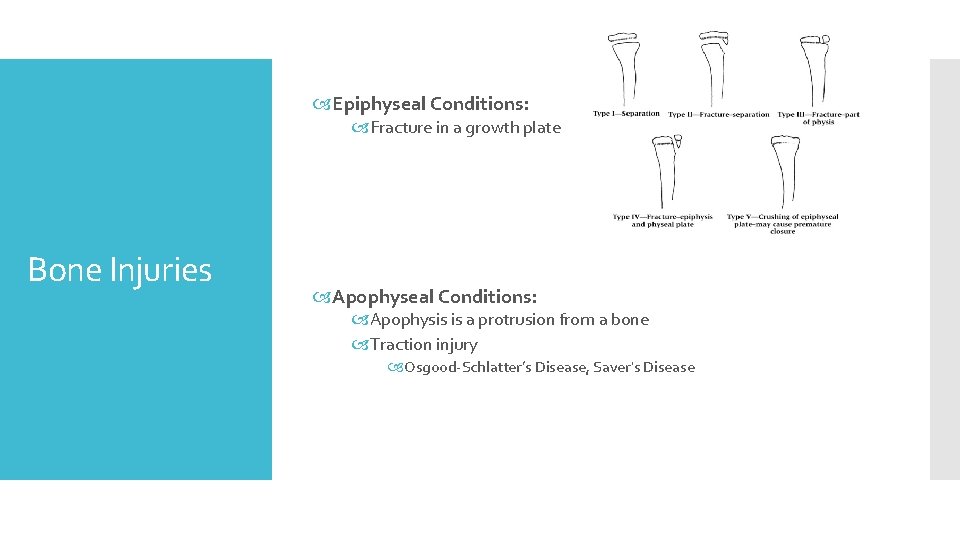
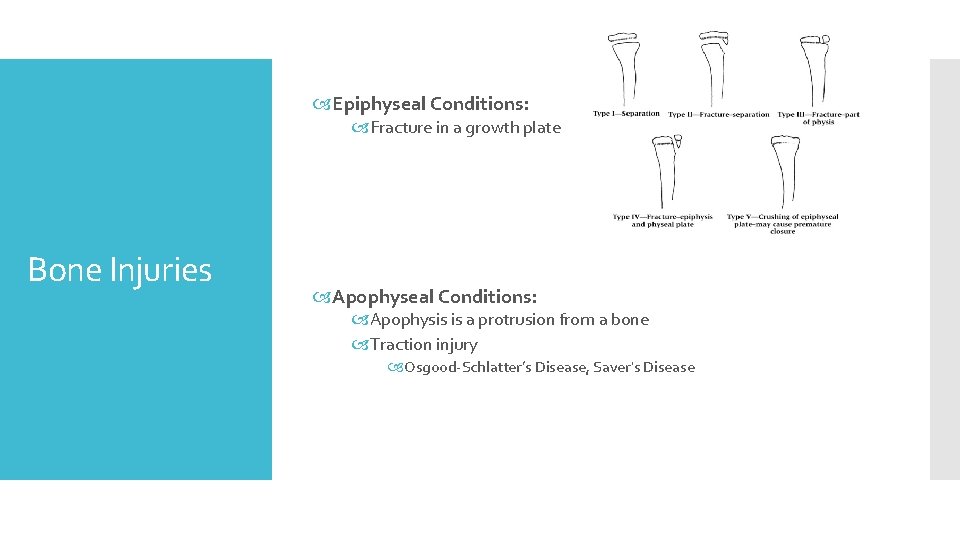
Epiphyseal Conditions: Fracture in a growth plate Bone Injuries Apophyseal Conditions: Apophysis is a protrusion from a bone Traction injury Osgood-Schlatter’s Disease, Saver's Disease
Compression and tension are primary mechanisms Neuropraxia: Interruption in conduction through nerve fiber Nerve Injuries Brought about via compression or blunt trauma Impact motor more than sensory function Temporary loss of function
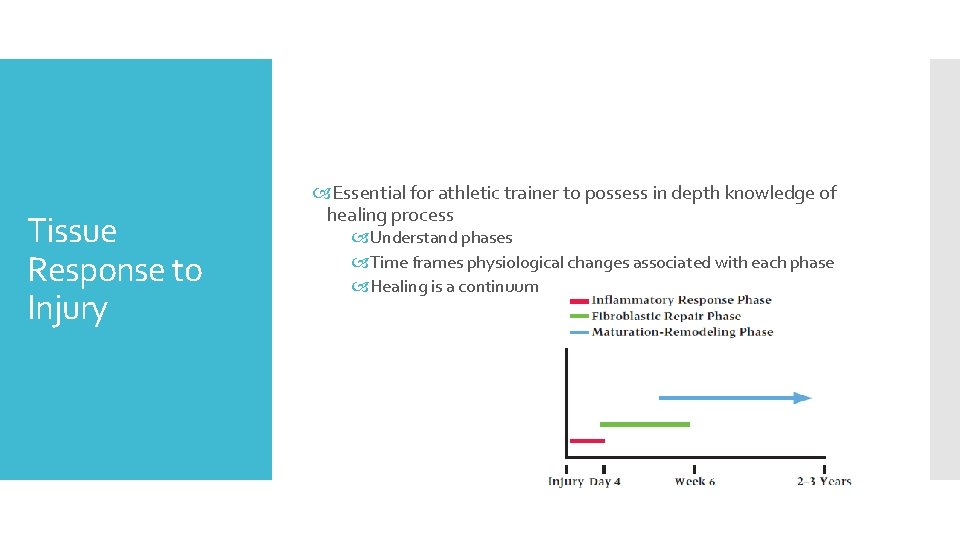
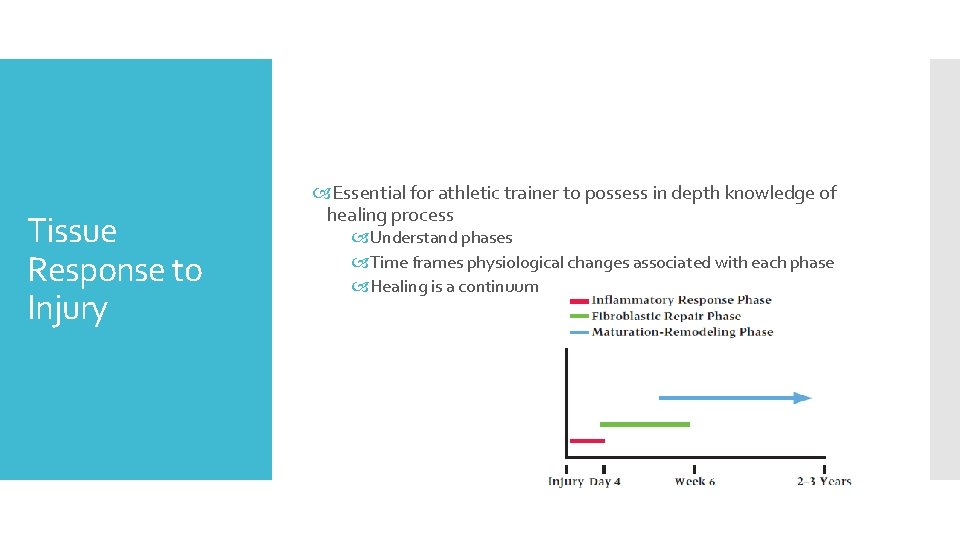
Tissue Response to Injury Essential for athletic trainer to possess in depth knowledge of healing process Understand phases Time frames physiological changes associated with each phase Healing is a continuum
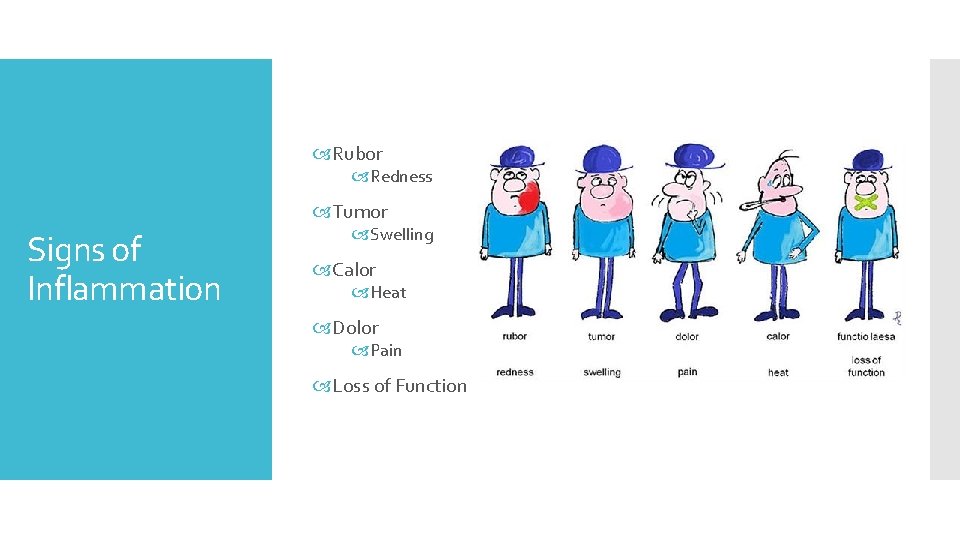
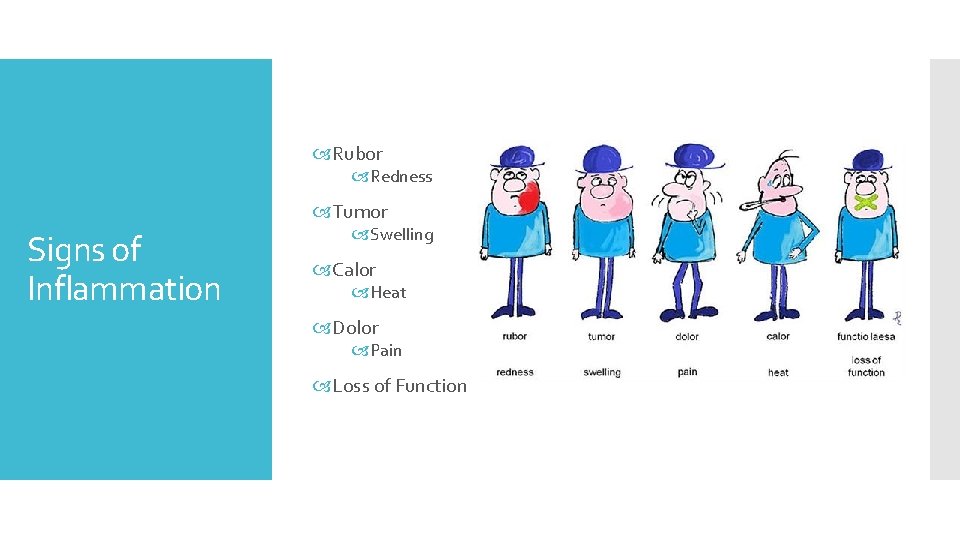
Rubor Redness Tumor Signs of Inflammation Swelling Calor Heat Dolor Pain Loss of Function
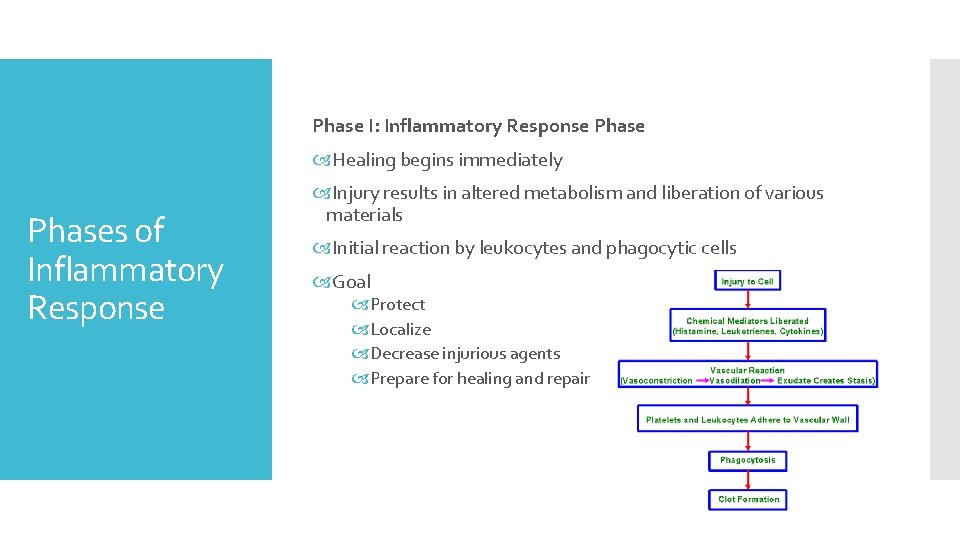
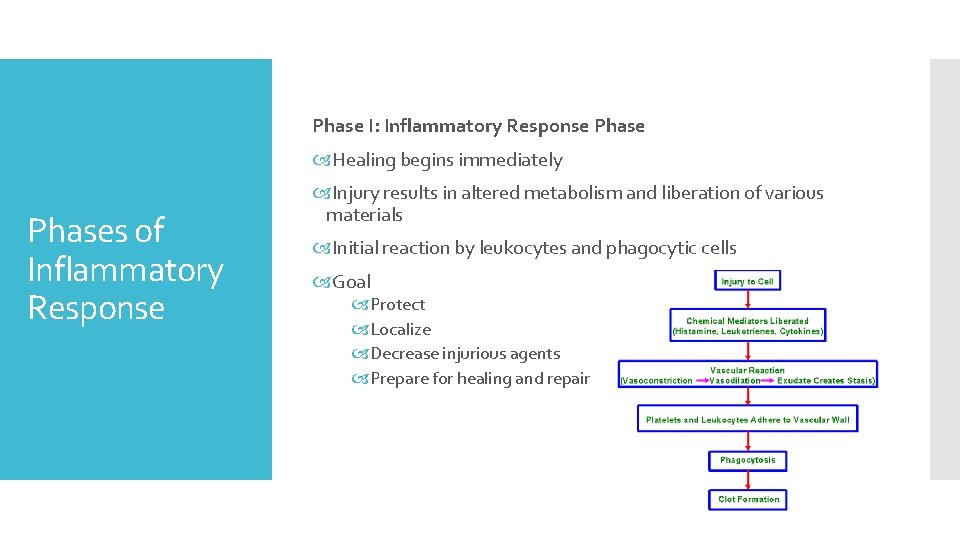
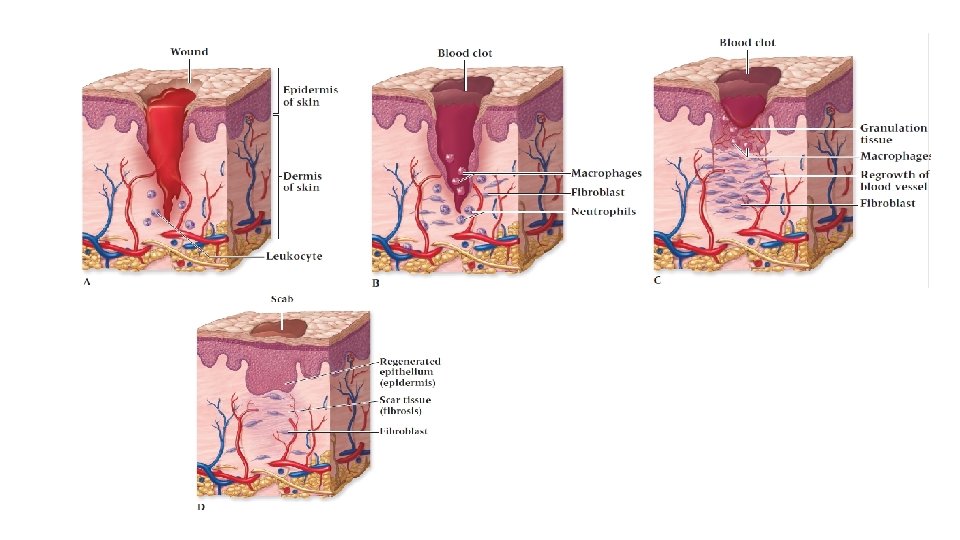
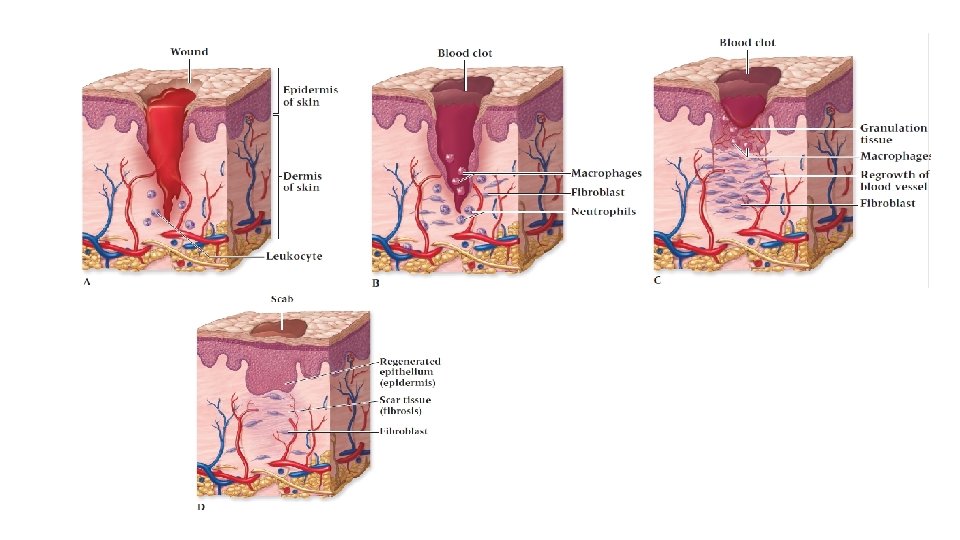
Phase I: Inflammatory Response Phase Healing begins immediately Phases of Inflammatory Response Injury results in altered metabolism and liberation of various materials Initial reaction by leukocytes and phagocytic cells Goal Protect Localize Decrease injurious agents Prepare for healing and repair
Clot Formation Platelets adhere to exposed collagen leading to formation of plug (clot) Clots obstruct lymphatic fluid drainage and aid in localizing injury Requires conversion of fibrinogen to fibrin Phase I: Inflammatory Response Initial stage: thromboplastin is formed Second stage: Prothrombin is converted to thrombin due to interaction with thromboplastin Third stage: thrombin changes from soluble fibrinogen to insoluble fibrin coagulating into a network localizing the injury Chronic Inflammation Occurs when acute inflammatory response does not eliminate injuring agent Tissue not restored to normal physiologic state Involves replacement of leukocytes with macrophages, lymphocytes and plasma cells As inflammation persists necrosis and fibrosis prolong healing process
Scar formation through 3 phases Resolution (little tissue damage and normal restoration) Restoration (if resolution is delayed) Regeneration (replacement of tissue by same tissue) Fibroplasia: formation of a scar Phase II: Fibroblastic Repair Complaints of pain and tenderness gradually subside during this period Scar Formation Capillary buds form Formation of delicate connective tissue (granulation tissue) Consists of fibroblasts, extracellular matrix, develop collagen, elastin, ground substance With proliferation of collagen scar tensile strength increases # of fibroblasts gradually diminishes Normal sequence = minimal scarring Persistent inflammation = extended fibroplasia
Long-term process Phase III: Maturation & Remodeling Realignment of collagen relative to applied tensile forces Continued breakdown and synthesis of collagen = increased strength Tissue will gradually assume normal appearance May require several years to complete

Factors That Impede Healing Extent of injury Corticosteroids Edema Keloids and Hypertrophic Scars Hemorrhage Infection Poor Vascular Supply Humidity, Climate, Oxygen Tension Separation of Tissue Muscle Spasm Atrophy Health, Age, and Nutrition
Limited capacity to heal Cartilage Healing Little or no direct blood supply If area involves subchondral bone (enhanced blood supply) granulation tissue is present and healing proceeds normally
Proper care will result in acute repair, and remodeling phases in same time required by other vascular tissues Repair phase will involve random laying down of collagen which, as scar forms, will mature and realign in reaction to joint stresses and strain Ligament Healing Full healing may require 12 months Surgically repaired ligaments tend to be stronger due to decreased scar formation Exercised ligaments are stronger Exercise vs. Immobilization Muscles must be strengthened to reinforce the joint Increased tension will increase joint stability
Initial bleeding followed by proliferation of ground substance and fibroblast Skeletal Muscle Healing Myoblastic cells form = regeneration of new myofibrils Collagen will mature and orient along lines of tension Healing could last 6 -8 weeks depending on muscle injured
Requires dense fibrous union of separated ends Abundance of collagen is required for good tensile strength Tendon Healing Too much = fibrosis – may interfere with gliding Initially injured tendon will adhere to surrounding tissues (week 2) Week 3 – tendon will gradually separate Tissue not strong enough until weeks 4 -5
Therapeutic Modalities Heat: facilitates acute inflammation Cold: slows inflammatory process Management of Injuries Ultrasound, electrical stimulation: treat inflammation Therapeutic Exercise Pain free movement, full strength, power, and tissue extensibility Immobilization, while sometimes necessary, can have a negative effect on injury healing Early mobilization may enhance healing
Acute fractures have 5 stages Hematoma formation Cellular proliferation Callus formation Ossification Remodeling Trauma to the periosteum and surrounding soft tissue occurs due to the initial bone trauma Bone Healing Hematoma occurs during first 48 hours Osteoblasts fill the internal and external calluses to immobilize the site Hard callus becomes more well-formed as osteoblasts lay down cancellous bone, replacing cartilage Ossification is complete when bone has been laid down and the excess callus has been resorbed by osteoclasts Time required is dependent on various factors Severity and site of fracture Age and extent of trauma
Poor Blood Supply Bone may die and union/healing will not occur (avascular necrosis) Head of femur, scaphoid, talus, base of 5 th metatarsal Problems with Bone Healing Poor Immobilization Poor casting allowing for motion between bone parts Patient not following immobilization recommendations May prevent proper union or result in bony deformity Infection Interferes with healing More common with compound fractures Soft tissue alterations could cause non-union
Cutaneous: sharp, bright, burning, fast and slow onset Deep Somatic: originates in tendons, muscles, joints, periosteum and blood vessels Visceral: begins in organs and is diffuse at first and may become localized Psychogenic: felt by individual, but is emotional rather than physical Types of Pain Fast vs Slow: Fast: localized and carried through A-delta fibers Slow: perceived as aching, throbbing or burning; through c-fibers Acute vs Chronic: Acute: less than 6 months duration Chronic: longer than 6 months duration Referred Pain: occurs away from actual site of injury/irritation A-alpha fibers are sensitive to pressure and can produce paresthesia Myofacial, scleromatic, and dermatomatic
Myofascial Pain: trigger points, acute or chronic Referred Pain Scleromatic: travels on C fibers; deep, aching, poorly localized pain; can cause depression, anxiety, fear, anger; autonomic changes (Bp, sweating) Dermotomic: irritation of A-delta fibers; sharp, localized
Gate Control Theory: at spinal cord level Pain Control Sensory information from receptors on cutaneous tissue enter A-beta fibers Pain simultaneously travels along A-delta and Cfibers Sensory information overrides the pain information, “closing the gate” Pain message isn’t received
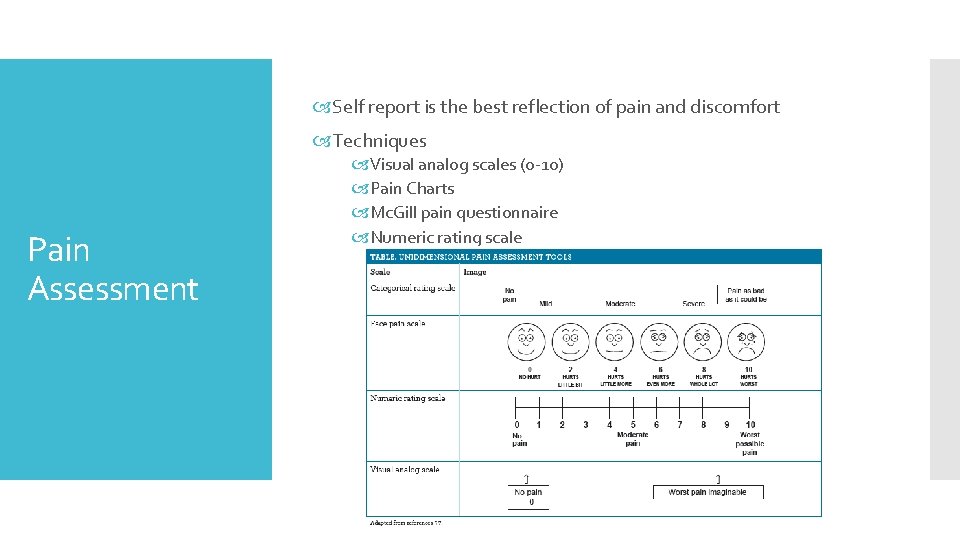
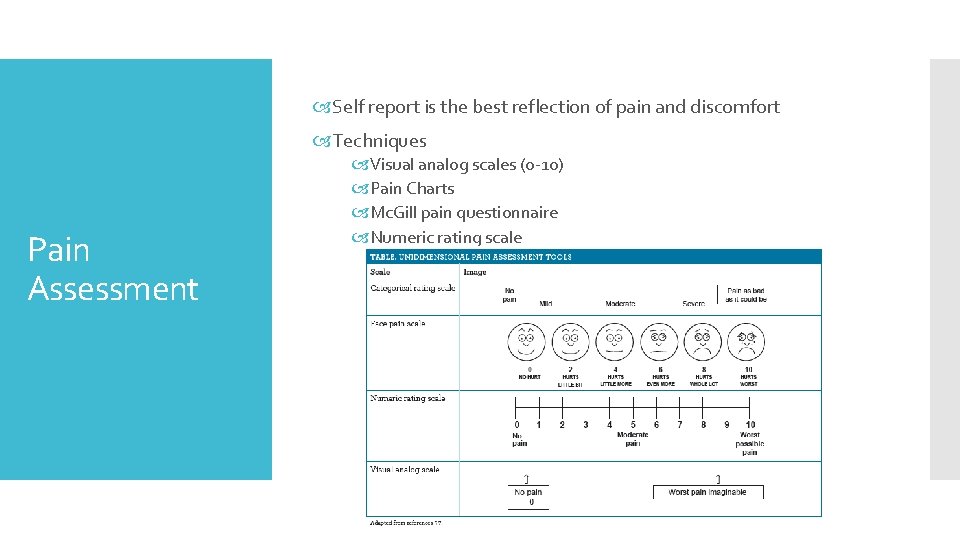
Self report is the best reflection of pain and discomfort Techniques Pain Assessment Visual analog scales (0 -10) Pain Charts Mc. Gill pain questionnaire Numeric rating scale
Pain Assessment
Modalities Used to relieve pain and control other s & sx of injury/surgery Use in conjunction with exercise Induced analgesia (pain reduction/removal) Treating Pain Thermal agents for pain control Electrical modalities to reduce pain control TENS, superficial heat/cold, massage used to target gate control theory Electrical stimulation, deep massage Pharmacological Agents Oral, injectable medications Analgesics and anti-inflammatories Referring physicians or pharmacists ATs are not allowed to dispense medications to minors