Mechanics of Breathing Pulmonary Ventilation Completely mechanical process
Mechanics of Breathing (Pulmonary Ventilation) • Completely mechanical process that depends on volume changes in the thoracic cavity • Volume changes lead to pressure changes, which lead to the flow of gases to equalize pressure
Mechanics of Breathing (Pulmonary Ventilation) • Two phases • Inspiration = inhalation • Flow of air into lungs • Expiration = exhalation • Air leaving lungs
Mechanics of Breathing (Pulmonary Ventilation) • Inspiration • Diaphragm and external intercostal muscles contract • The size of the thoracic cavity increases • External air is pulled into the lungs as a result of: • Increase in intrapulmonary volume • Decrease in gas pressure • Air is sucked into the lungs

Figure 13. 7 a Rib cage and diaphragm positions during breathing. Changes in anterior-posterior and superior-inferior dimensions Ribs elevated as external intercostals contract External intercostal muscles Changes in lateral dimensions Full inspiration (External intercostals contract) Diaphragm moves inferiorly during contraction (a) Inspiration: Air (gases) flows into the lungs

Pressure relative to atmospheric pressure Figure 13. 8 Changes in intrapulmonary pressure and air flow during inspiration and expiration. +2 +1 Inspiration Expiration Intrapulmonary pressure 0 − 1 − 2 (a) Volume of breath Volume (L) 0. 5 0 − 0. 5 (b)
Mechanics of Breathing (Pulmonary Ventilation) • Expiration • Largely a passive process that depends on natural lung elasticity • As muscles relax, air is pushed out of the lungs as a result of: • Decrease in intrapulmonary volume • Increase in gas pressure • Forced expiration can occur mostly by contraction of internal intercostal muscles to depress the rib cage
Mechanics of Breathing (Pulmonary Ventilation) • Normal pressure within the pleural space is always negative (intrapleural pressure) • Differences in lung and pleural space pressures keep lungs from collapsing • Atelectasis is collapsed lung • Pneumothorax is the presence of air in the intrapleural space
Respiratory Volumes and Capacities • Normal breathing moves about 500 ml of air with each breath • This respiratory volume is tidal volume (TV) • Many factors affect respiratory capacity • • A person’s size Sex Age Physical condition

Respiratory Volumes and Capacities • Inspiratory reserve volume (IRV) • Amount of air that can be taken in forcibly over the tidal volume • Usually around 3, 100 ml • Expiratory reserve volume (ERV) • Amount of air that can be forcibly exhaled after a tidal expiration • Approximately 1, 200 ml
Respiratory Volumes and Capacities • Residual volume • Air remaining in lung after expiration • Allows gas exchange to go on continuously, even between breaths, and helps keep alveoli open (inflated) • About 1, 200 ml
Respiratory Volumes and Capacities • Vital capacity • The total amount of exchangeable air • Vital capacity = TV + IRV + ERV • 4, 800 ml in men; 3, 100 ml in women • Dead space volume • Air that remains in conducting zone and never reaches alveoli • About 150 ml
Respiratory Volumes and Capacities • Functional volume • Air that actually reaches the respiratory zone • Usually about 350 ml • Respiratory capacities are measured with a spirometer
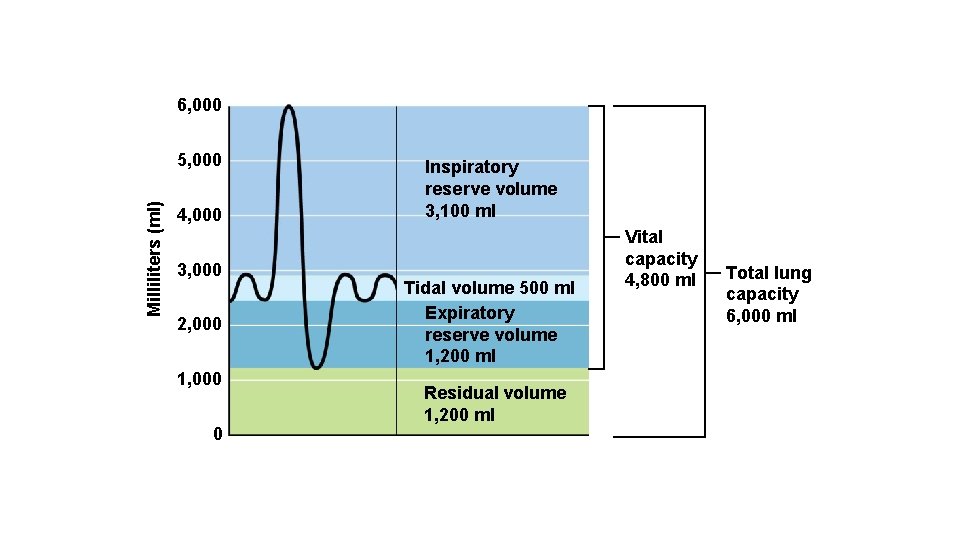
6, 000 Milliliters (ml) 5, 000 4, 000 3, 000 2, 000 1, 000 0 Inspiratory reserve volume 3, 100 ml Tidal volume 500 ml Expiratory reserve volume 1, 200 ml Residual volume 1, 200 ml Vital capacity 4, 800 ml Total lung capacity 6, 000 ml

Nonrespiratory Air (Gas) Movements • Can be caused by reflexes or voluntary actions • Examples: • • • Cough and sneeze—clears lungs of debris Crying—emotionally induced mechanism Laughing—similar to crying Hiccup—sudden inspirations Yawn—very deep inspiration https: //www. youtube. com/watch? v=h 53 Q 0 tsl. R 9 Y
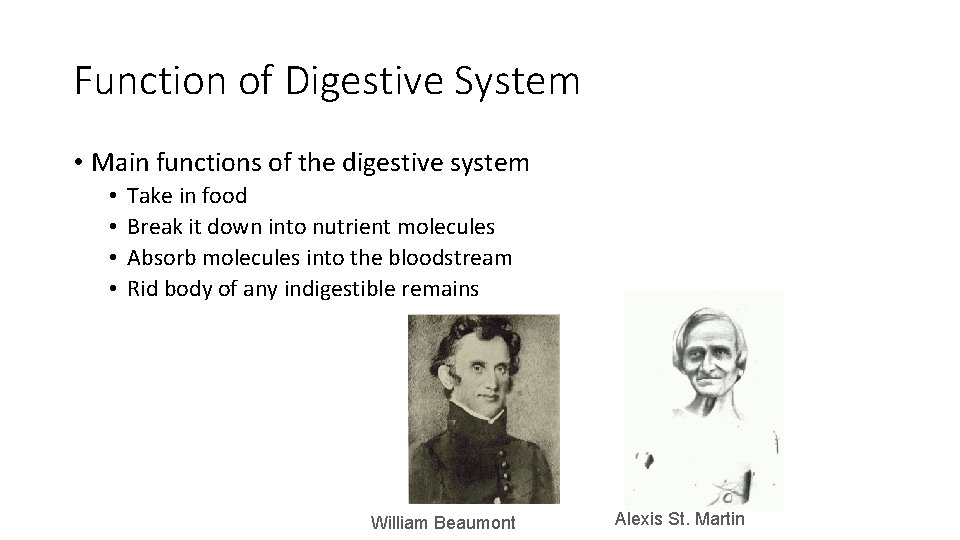
Function of Digestive System • Main functions of the digestive system • • Take in food Break it down into nutrient molecules Absorb molecules into the bloodstream Rid body of any indigestible remains William Beaumont Alexis St. Martin
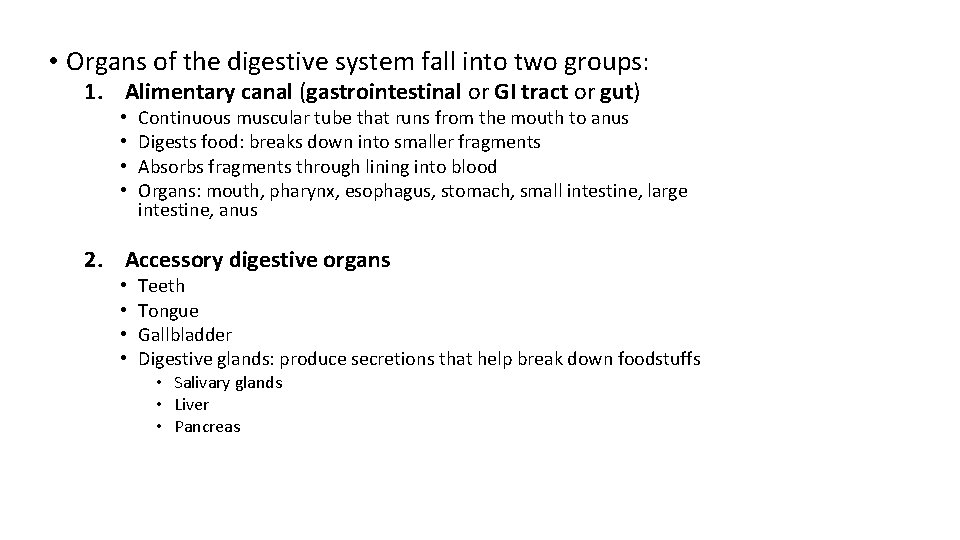
• Organs of the digestive system fall into two groups: 1. Alimentary canal (gastrointestinal or GI tract or gut) • • Continuous muscular tube that runs from the mouth to anus Digests food: breaks down into smaller fragments Absorbs fragments through lining into blood Organs: mouth, pharynx, esophagus, stomach, small intestine, large intestine, anus 2. Accessory digestive organs • • Teeth Tongue Gallbladder Digestive glands: produce secretions that help break down foodstuffs • Salivary glands • Liver • Pancreas
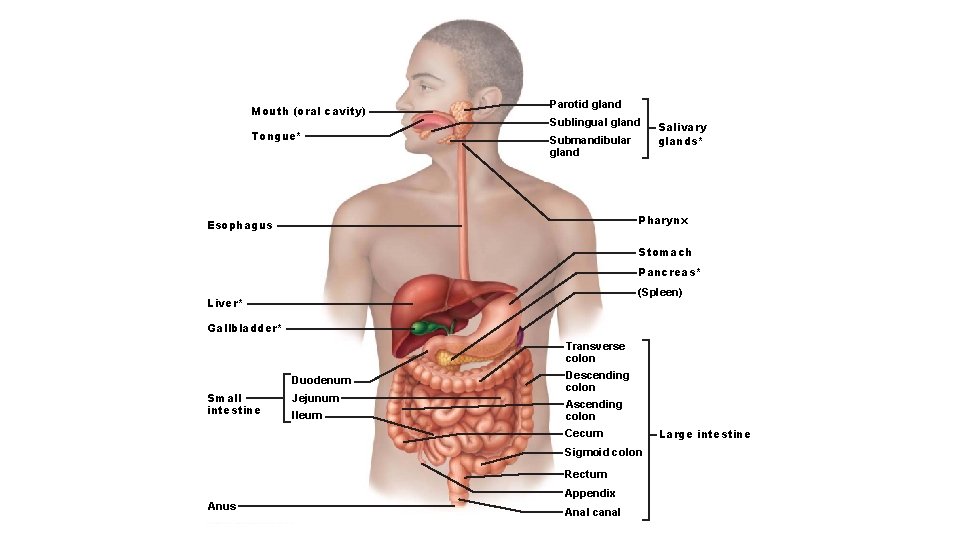
Mouth (oral cavity) Tongue* Parotid gland Sublingual gland Submandibular gland Salivary glands* Pharynx Esophagus Stomach Pancreas* (Spleen) Liver* Gallbladder* Transverse colon Duodenum Small intestine Jejunum Ileum Descending colon Ascending colon Cecum Sigmoid colon Rectum Appendix Anus Anal canal Large intestine
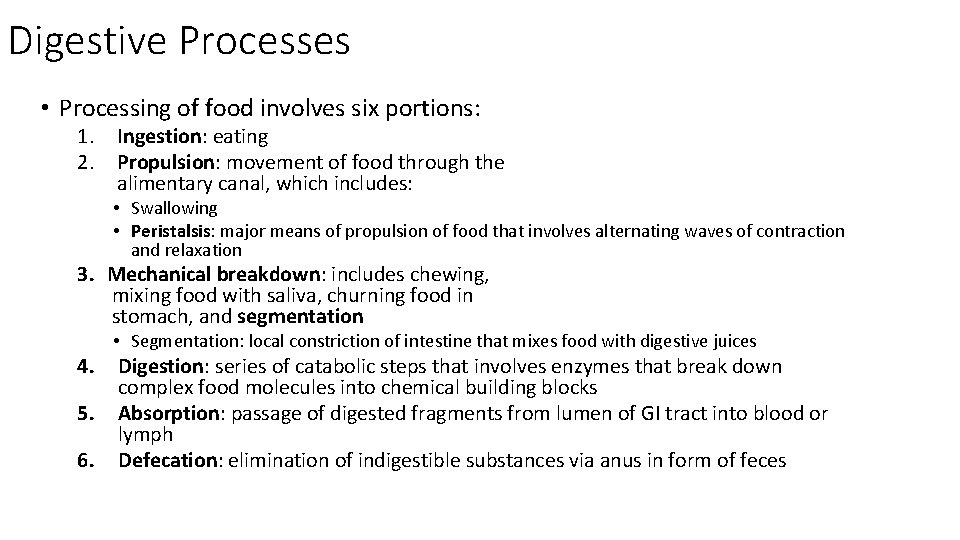
Digestive Processes • Processing of food involves six portions: 1. 2. Ingestion: eating Propulsion: movement of food through the alimentary canal, which includes: • Swallowing • Peristalsis: major means of propulsion of food that involves alternating waves of contraction and relaxation 3. Mechanical breakdown: includes chewing, mixing food with saliva, churning food in stomach, and segmentation 4. 5. 6. • Segmentation: local constriction of intestine that mixes food with digestive juices Digestion: series of catabolic steps that involves enzymes that break down complex food molecules into chemical building blocks Absorption: passage of digested fragments from lumen of GI tract into blood or lymph Defecation: elimination of indigestible substances via anus in form of feces
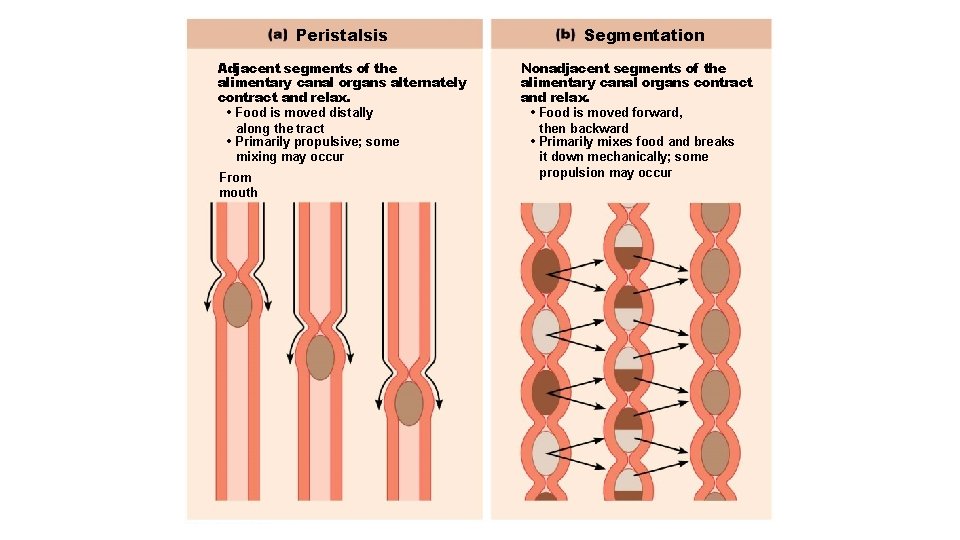
Peristalsis Adjacent segments of the alimentary canal organs alternately contract and relax. • Food is moved distally along the tract • Primarily propulsive; some mixing may occur From mouth Segmentation Nonadjacent segments of the alimentary canal organs contract and relax. • Food is moved forward, then backward • Primarily mixes food and breaks it down mechanically; some propulsion may occur
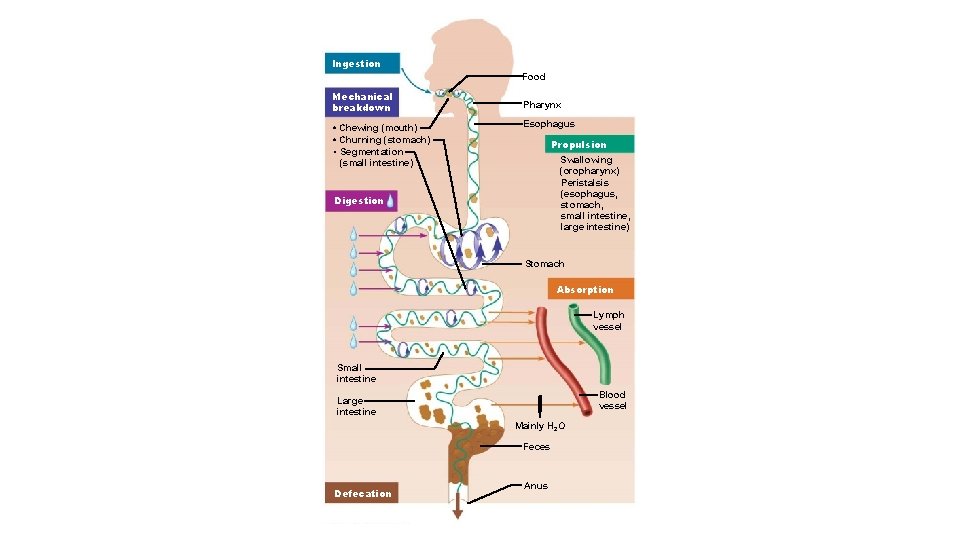
Ingestion Food Mechanical breakdown • Chewing (mouth) • Churning (stomach) • Segmentation (small intestine) Pharynx Esophagus Propulsion Swallowing (oropharynx) Peristalsis (esophagus, stomach, small intestine, large intestine) Digestion Stomach Absorption Lymph vessel Small intestine Blood vessel Large intestine Mainly H 2 O Feces Defecation Anus
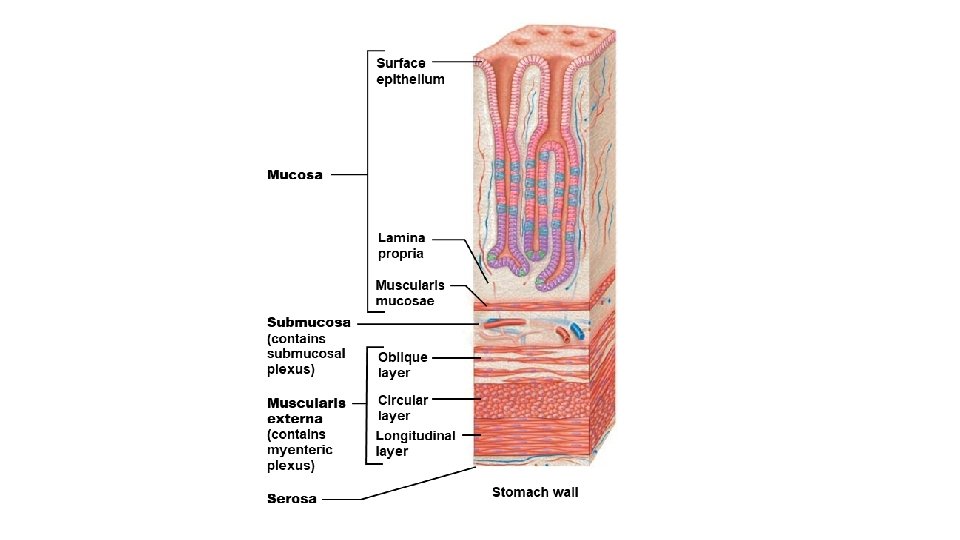
Histology of the Alimentary Canal • All digestive organs have the same four basic layers, or tunics 1. 2. 3. 4. Mucosa Submucosa Muscularis externa Serosa
1. Mucosa • Tunic layer that lines lumen • Functions: • Secretes mucus, digestive enzymes, and hormones • Absorbs end products of digestion • Protects against infectious disease 2. Submucosa • Consists of areolar connective tissue • Contains blood and lymphatic vessels, lymphoid follicles, and submucosal nerve plexus that supply surrounding GI tract tissues • Has abundant amount of elastic tissues that help organs to regain shape after storing large meal
3. Muscularis externa • Muscle layer responsible for segmentation and peristalsis • Contains inner circular muscle layer and outer longitudinal layers • Circular layer thickens in some areas to form sphincters 4. Serosa • Outermost layer, which is made up of the visceral peritoneum
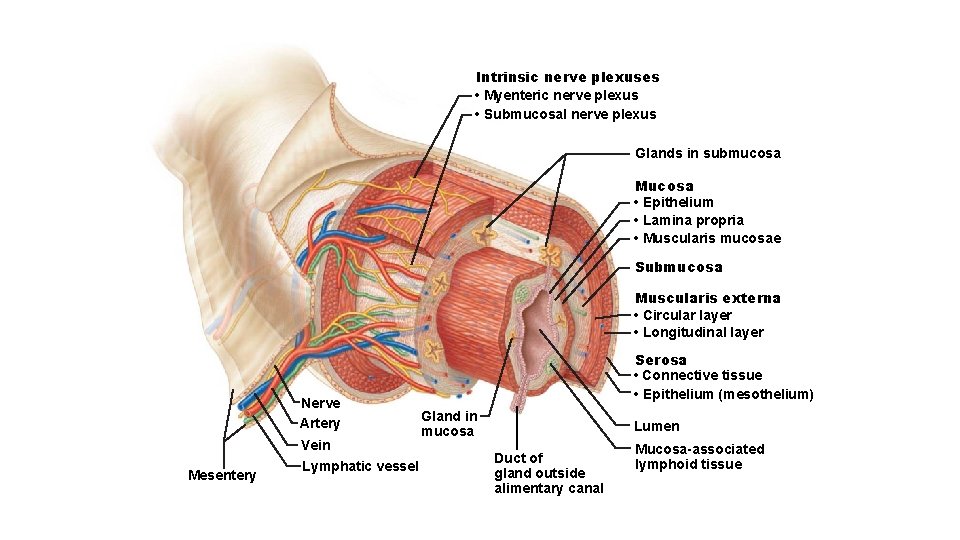
Intrinsic nerve plexuses • Myenteric nerve plexus • Submucosal nerve plexus Glands in submucosa Mucosa • Epithelium • Lamina propria • Muscularis mucosae Submucosa Muscularis externa • Circular layer • Longitudinal layer Nerve Artery Vein Mesentery Lymphatic vessel Serosa • Connective tissue • Epithelium (mesothelium) Gland in mucosa Lumen Duct of gland outside alimentary canal Mucosa-associated lymphoid tissue
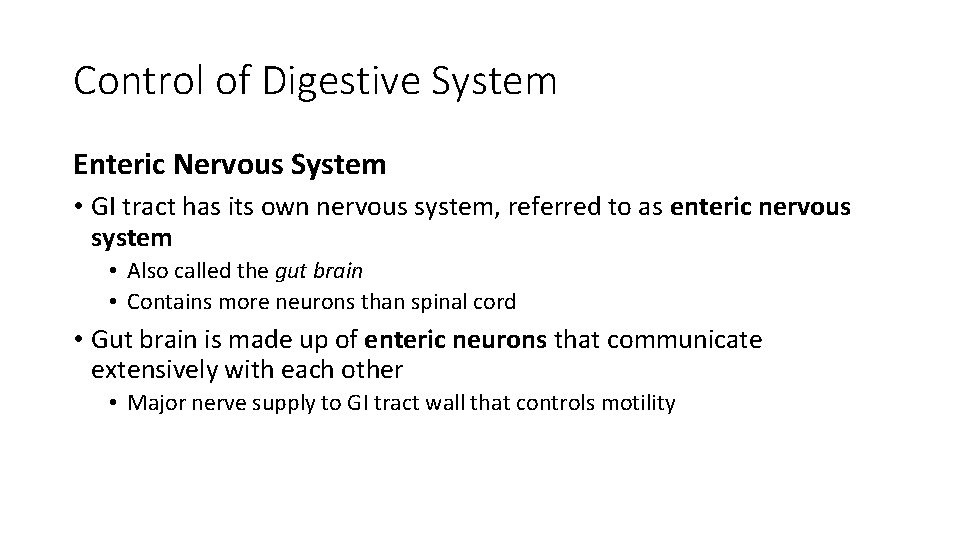
Control of Digestive System Enteric Nervous System • GI tract has its own nervous system, referred to as enteric nervous system • Also called the gut brain • Contains more neurons than spinal cord • Gut brain is made up of enteric neurons that communicate extensively with each other • Major nerve supply to GI tract wall that controls motility
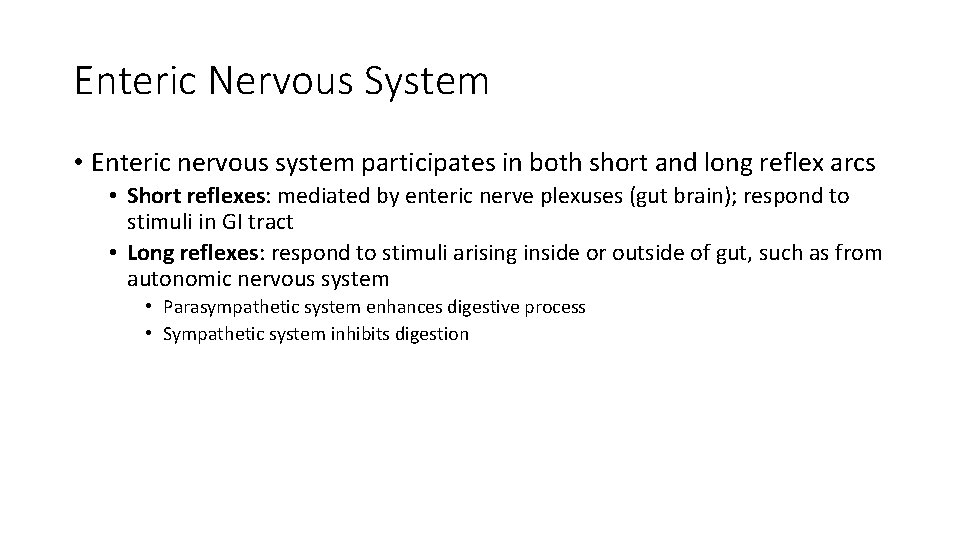
Enteric Nervous System • Enteric nervous system participates in both short and long reflex arcs • Short reflexes: mediated by enteric nerve plexuses (gut brain); respond to stimuli in GI tract • Long reflexes: respond to stimuli arising inside or outside of gut, such as from autonomic nervous system • Parasympathetic system enhances digestive process • Sympathetic system inhibits digestion
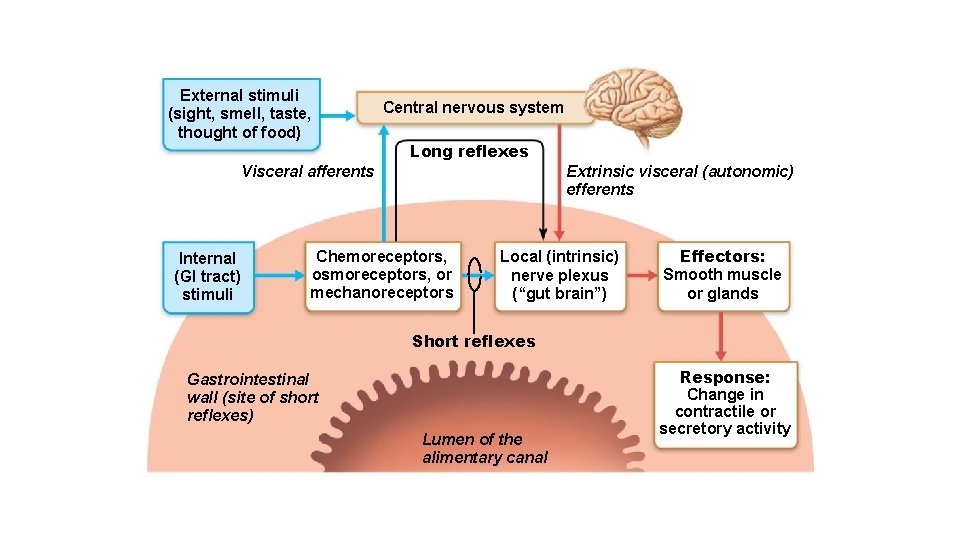
External stimuli (sight, smell, taste, thought of food) Central nervous system Long reflexes Visceral afferents Internal (GI tract) stimuli Extrinsic visceral (autonomic) efferents Chemoreceptors, osmoreceptors, or mechanoreceptors Local (intrinsic) nerve plexus (“gut brain”) Effectors: Smooth muscle or glands Short reflexes Gastrointestinal wall (site of short reflexes) Lumen of the alimentary canal Response: Change in contractile or secretory activity
Basic Regulation of Digestive Activity Digestive activity is provoked by a range of mechanical and chemical stimuli • Receptors located in walls of GI tract organs • Respond to stretch, changes in osmolarity and p. H, and presence of substrate and end products of digestion 2. Effectors of digestive activity are smooth muscle and glands • When stimulated, receptors initiate reflexes that stimulate smooth muscle to mix and move lumen contents • Reflexes can also activate or inhibit digestive glands that secrete digestive juices or hormones 3. Neurons (intrinsic and extrinsic) and hormones control digestive activity • Nervous system control • Intrinsic controls: involve short reflexes (enteric nervous system) • Extrinsic controls: involve long reflexes (autonomic nervous system) • Hormonal controls • Hormones from cells in stomach and small intestine stimulate target cells in same or different organs to secrete or contract
Mouth etc. • Mouth is where food is chewed and mixed with enzymecontaining saliva that begins process of digestion, and swallowing process is initiated • Associated organs include: • • Mouth Tongue Salivary glands Teeth
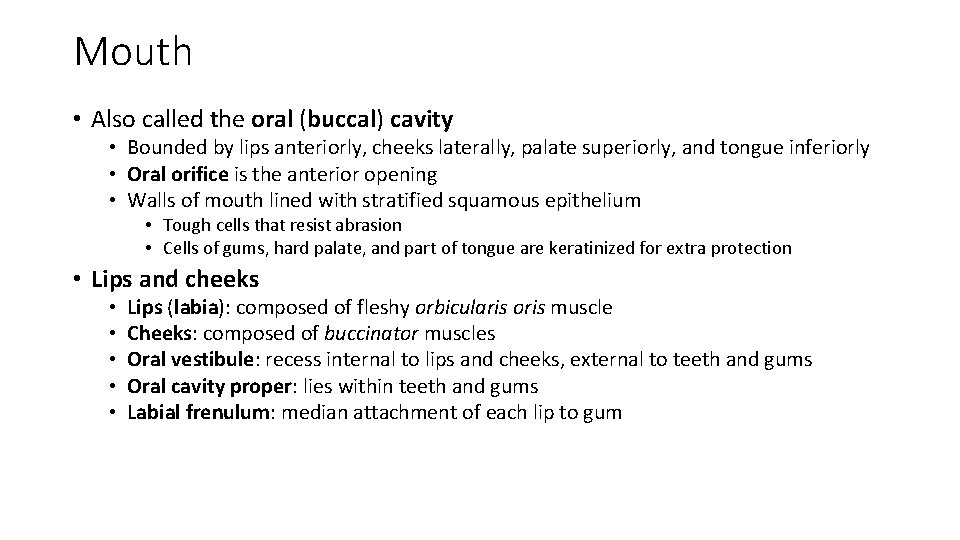
Mouth • Also called the oral (buccal) cavity • Bounded by lips anteriorly, cheeks laterally, palate superiorly, and tongue inferiorly • Oral orifice is the anterior opening • Walls of mouth lined with stratified squamous epithelium • Tough cells that resist abrasion • Cells of gums, hard palate, and part of tongue are keratinized for extra protection • Lips and cheeks • • • Lips (labia): composed of fleshy orbicularis oris muscle Cheeks: composed of buccinator muscles Oral vestibule: recess internal to lips and cheeks, external to teeth and gums Oral cavity proper: lies within teeth and gums Labial frenulum: median attachment of each lip to gum
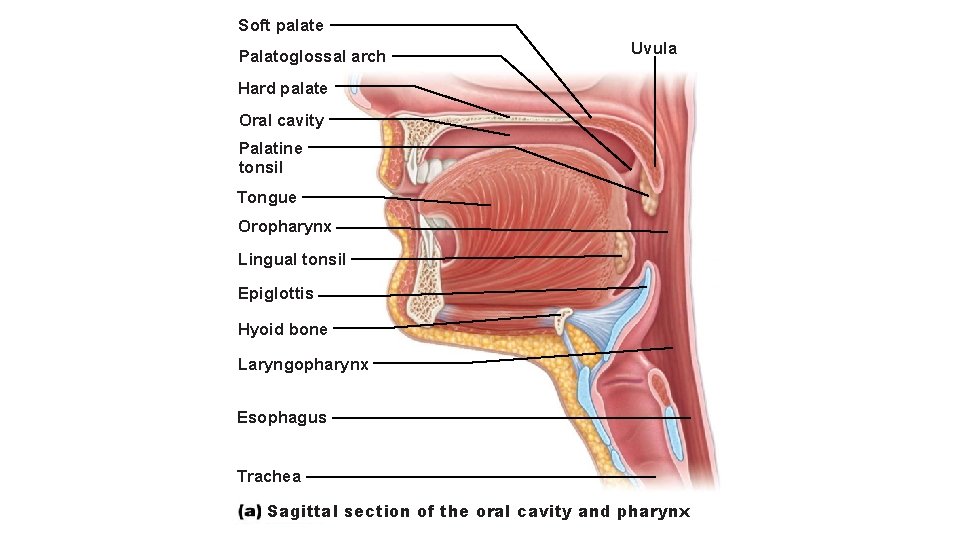
Soft palate Palatoglossal arch Uvula Hard palate Oral cavity Palatine tonsil Tongue Oropharynx Lingual tonsil Epiglottis Hyoid bone Laryngopharynx Esophagus Trachea Sagittal section of the oral cavity and pharynx
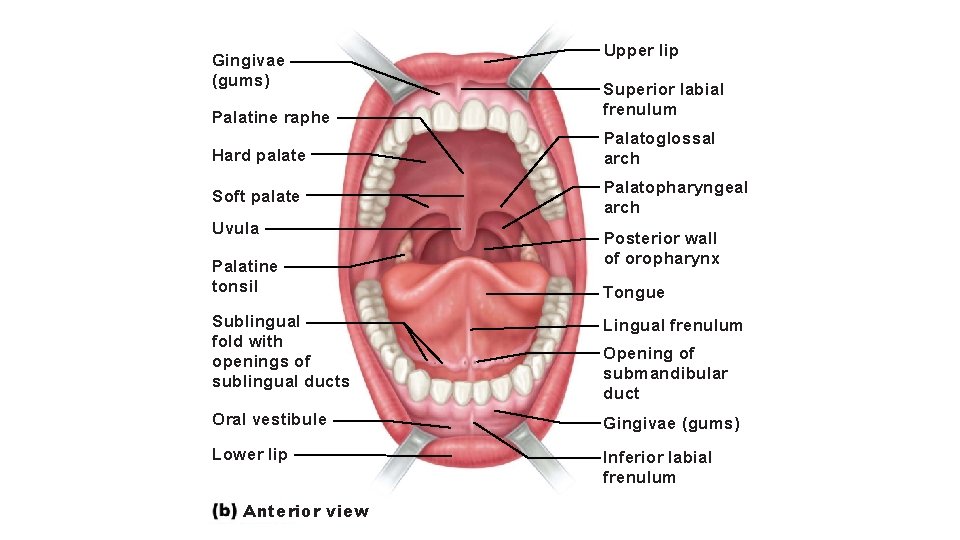
Gingivae (gums) Upper lip Palatine raphe Superior labial frenulum Hard palate Palatoglossal arch Soft palate Palatopharyngeal arch Uvula Palatine tonsil Sublingual fold with openings of sublingual ducts Posterior wall of oropharynx Tongue Lingual frenulum Opening of submandibular duct Oral vestibule Gingivae (gums) Lower lip Inferior labial frenulum Anterior view
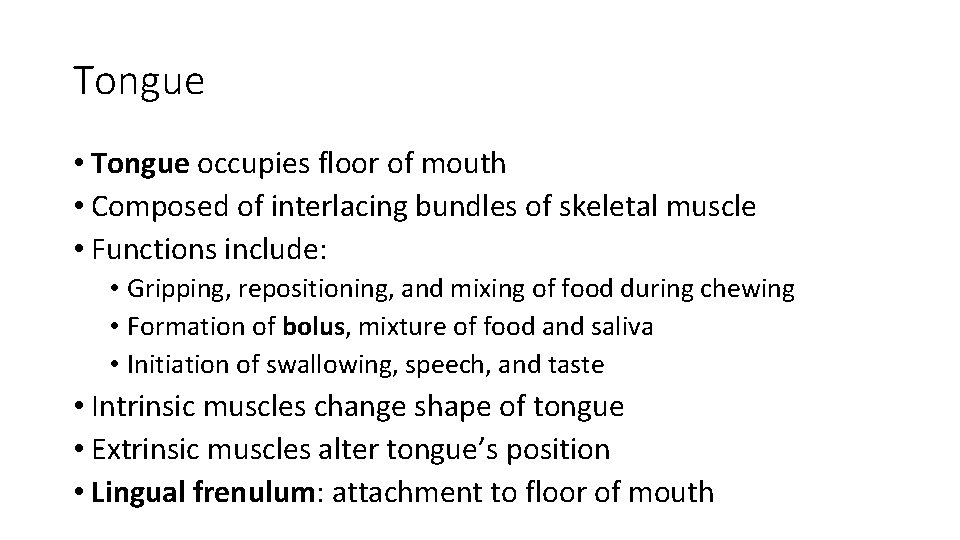
Tongue • Tongue occupies floor of mouth • Composed of interlacing bundles of skeletal muscle • Functions include: • Gripping, repositioning, and mixing of food during chewing • Formation of bolus, mixture of food and saliva • Initiation of swallowing, speech, and taste • Intrinsic muscles change shape of tongue • Extrinsic muscles alter tongue’s position • Lingual frenulum: attachment to floor of mouth
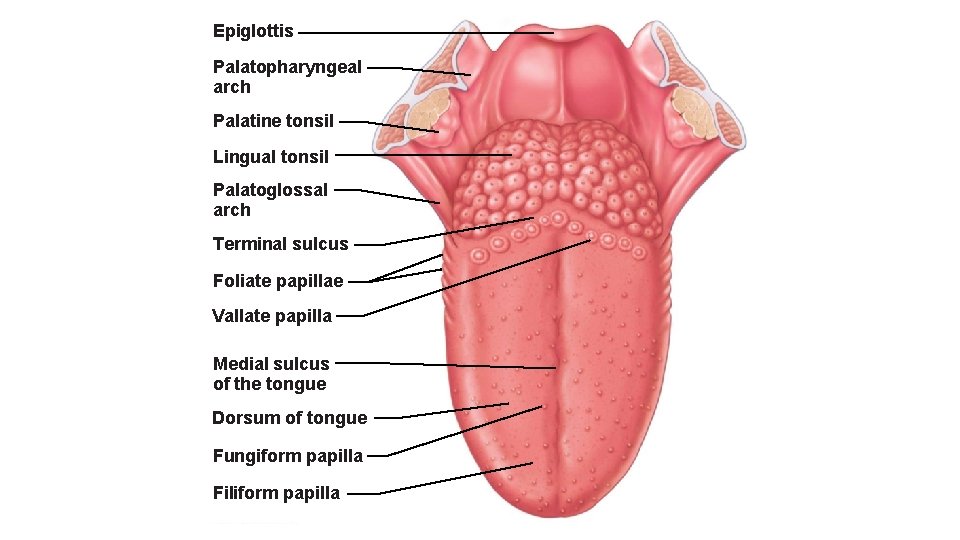
Epiglottis Palatopharyngeal arch Palatine tonsil Lingual tonsil Palatoglossal arch Terminal sulcus Foliate papillae Vallate papilla Medial sulcus of the tongue Dorsum of tongue Fungiform papilla Filiform papilla
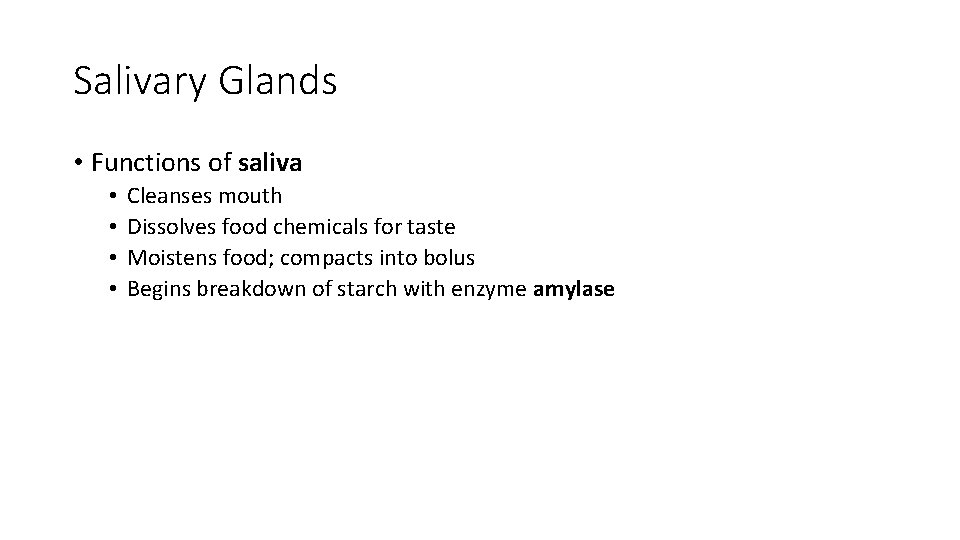
Salivary Glands • Functions of saliva • • Cleanses mouth Dissolves food chemicals for taste Moistens food; compacts into bolus Begins breakdown of starch with enzyme amylase
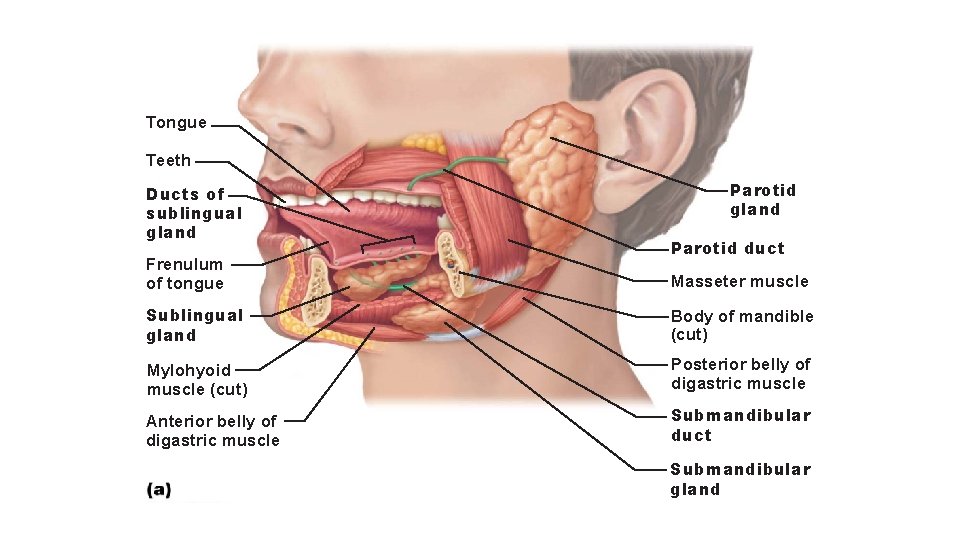
Tongue Teeth Ducts of sublingual gland Frenulum of tongue Parotid gland Parotid duct Masseter muscle Sublingual gland Body of mandible (cut) Mylohyoid muscle (cut) Posterior belly of digastric muscle Anterior belly of digastric muscle Submandibular duct Submandibular gland
Problem • Mumps: inflammation of parotid glands caused by the mumps virus (myxovirus) • Can spread from person to person via saliva • Symptoms: pain upon trying to open mouth or chew, fever, and pain when swallowing acidic foods • Mumps in adult males carries a 25% risk of infecting testes too, which could lead to sterility
The Teeth • Teeth lie in sockets in gum-covered margins of mandible and maxilla • Primary dentition consists of 20 deciduous teeth, or milk or baby teeth, that erupt between 6 and 24 months of age • 32 deep-lying permanent teeth enlarge and develop while roots of milk teeth are resorbed from below, causing them to loosen and fall out
The Teeth • Dentition and the dental formula • All but 3 rd molars (wisdom teeth) are in by end of adolescence • Teeth are classified according to shape: • Incisors: chisel shaped for cutting • Canines: fanglike teeth that tear or pierce • Premolars (bicuspids): broad crowns with rounded cusps used to grind or crush • Molars: broad crowns, rounded cusps: best grinders
Tooth and Gum Disease • Gingivitis • • Plaque calcifies to form calculus (tartar) Calculus disrupts seal between gingivae and teeth Anaerobic bacteria infect gums Infection is reversible if calculus removed • Periodontitis (periodontal disease) • Neglected gingivitis can escalate to disease • Immune cells attack not only bacterial intruders, but also body tissues • May increase heart disease and stroke • Risk factors: smoking, diabetes mellitus, oral piercings
Pharynx and Esophagus The Pharynx • Food passes from mouth into oropharynx and then into laryngopharynx • Allows passage of food, fluids, and air • Stratified squamous epithelium lining with mucus-producing glands • External muscle layers consists of two skeletal muscle layers
The Esophagus • Flat muscular tube that runs from laryngopharynx to stomach • Is collapsed when not involved in food propulsion • Joins stomach at cardial orifice • Gastroesophageal (cardiac) sphincter surrounds cardial orifice • Keeps orifice closed when food is not being swallowed • Mucus cells on both sides of sphincter help protect esophagus from acid reflux
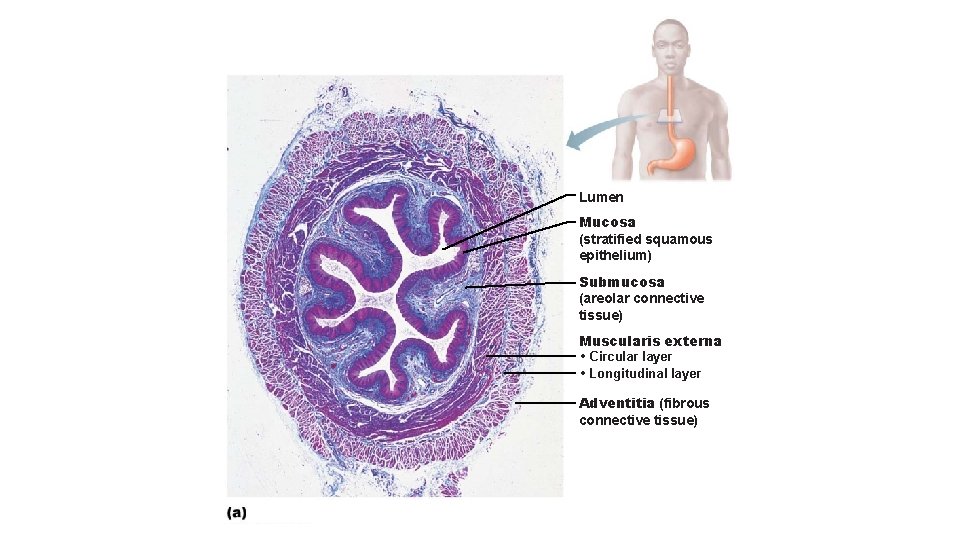
Lumen Mucosa (stratified squamous epithelium) Submucosa (areolar connective tissue) Muscularis externa • Circular layer • Longitudinal layer Adventitia (fibrous connective tissue)
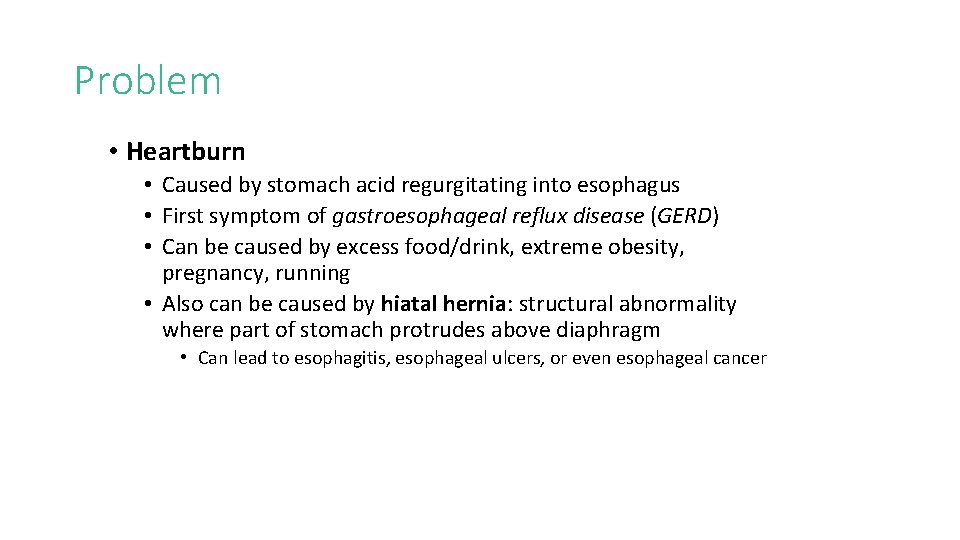
Problem • Heartburn • Caused by stomach acid regurgitating into esophagus • First symptom of gastroesophageal reflux disease (GERD) • Can be caused by excess food/drink, extreme obesity, pregnancy, running • Also can be caused by hiatal hernia: structural abnormality where part of stomach protrudes above diaphragm • Can lead to esophagitis, esophageal ulcers, or even esophageal cancer
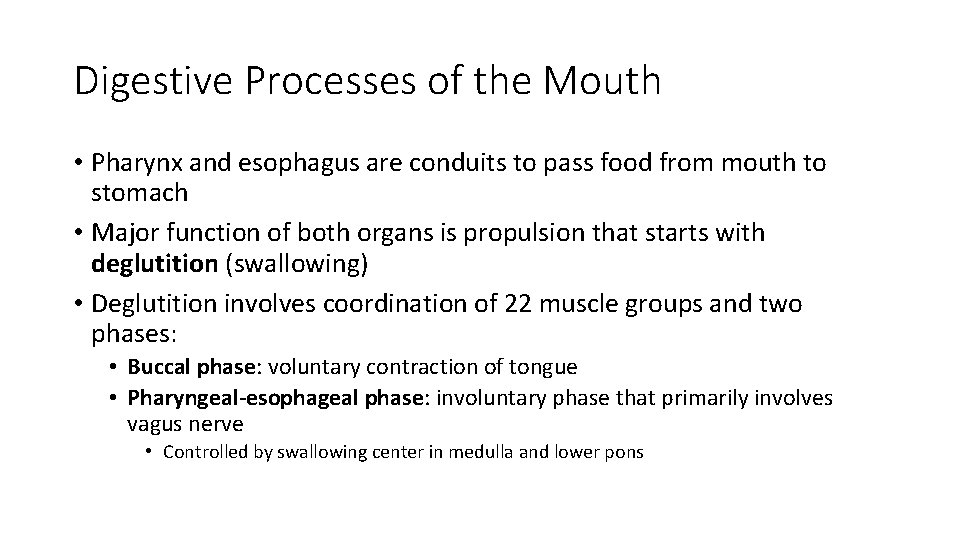
Digestive Processes of the Mouth • Pharynx and esophagus are conduits to pass food from mouth to stomach • Major function of both organs is propulsion that starts with deglutition (swallowing) • Deglutition involves coordination of 22 muscle groups and two phases: • Buccal phase: voluntary contraction of tongue • Pharyngeal-esophageal phase: involuntary phase that primarily involves vagus nerve • Controlled by swallowing center in medulla and lower pons
The Stomach Gross Anatomy of the Stomach • Stomach is a temporary storage tank that starts chemical breakdown of protein digestion • Converts bolus of food to paste-like chyme • Empty stomach has ~50 ml volume but can expand to 4 L
Gross Anatomy of the Stomach • Major regions of the stomach • • Cardial part (cardia): surrounds cardial orifice Fundus: dome-shaped region beneath diaphragm Body: midportion Pyloric part: wider and more superior portion of pyloric region, antrum, narrows into pyloric canal that terminates in pylorus • Pylorus is continuous with duodenum through pyloric valve (sphincter controlling stomach emptying)
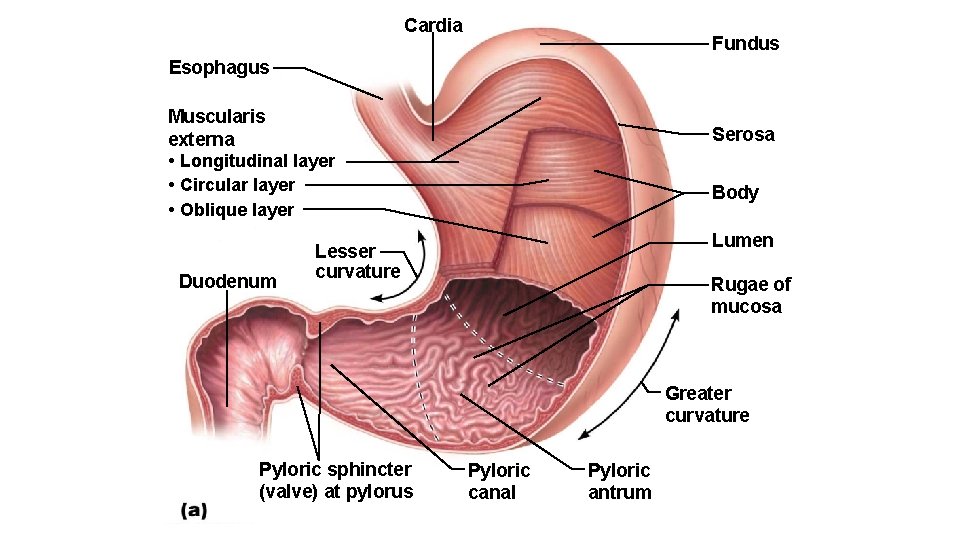
Cardia Fundus Esophagus Muscularis externa • Longitudinal layer • Circular layer • Oblique layer Duodenum Serosa Body Lumen Lesser curvature Rugae of mucosa Greater curvature Pyloric sphincter (valve) at pylorus Pyloric canal Pyloric antrum
Anatomy of the Stomach • Autonomic nervous system supplies stomach • Sympathetic fibers from thoracic splanchnic nerves are relayed through celiac plexus • Parasympathetic fibers are supplied by vagus nerve • Stomach wall contains regular four tunics; however, muscularis and mucosa are modified • Muscularis externa has circular and longitudinal smooth muscle layers, but also has extra third layer • Inner oblique layer allows stomach not only to churn, mix, and move chyme, but also to pummel it, which increases physical breakdown
Anatomy of the Stomach • Mucosa layer is also modified • Consists of simple columnar epithelium entirely composed of mucous cells • Secrete two-layer coat of alkaline mucus • Surface layer traps bicarbonate-rich fluid layer that is beneath it • Dotted with gastric pits, which lead into gastric glands • Gastric glands produce gastric juice
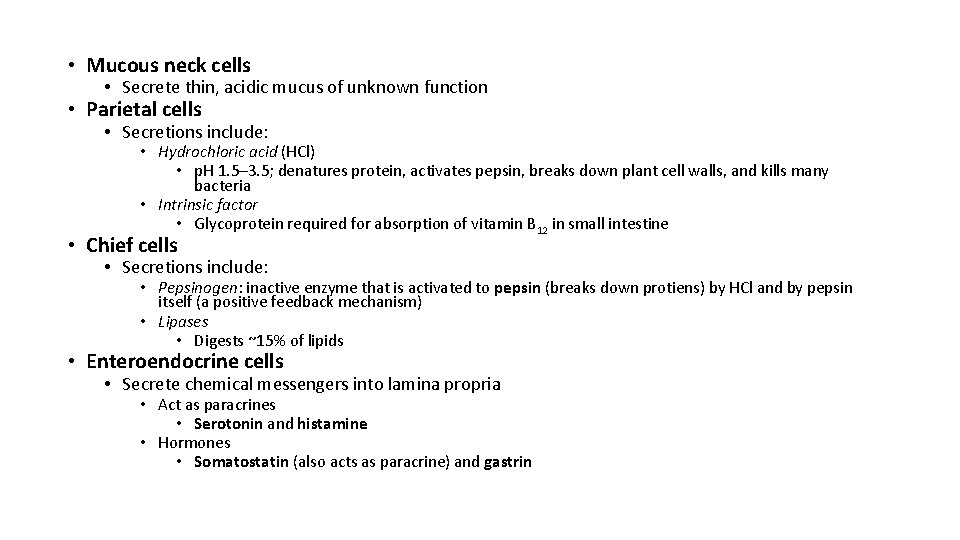
• Mucous neck cells • Secrete thin, acidic mucus of unknown function • Parietal cells • Secretions include: • Hydrochloric acid (HCl) • p. H 1. 5– 3. 5; denatures protein, activates pepsin, breaks down plant cell walls, and kills many bacteria • Intrinsic factor • Glycoprotein required for absorption of vitamin B 12 in small intestine • Chief cells • Secretions include: • Pepsinogen: inactive enzyme that is activated to pepsin (breaks down protiens) by HCl and by pepsin itself (a positive feedback mechanism) • Lipases • Digests ~15% of lipids • Enteroendocrine cells • Secrete chemical messengers into lamina propria • Act as paracrines • Serotonin and histamine • Hormones • Somatostatin (also acts as paracrine) and gastrin
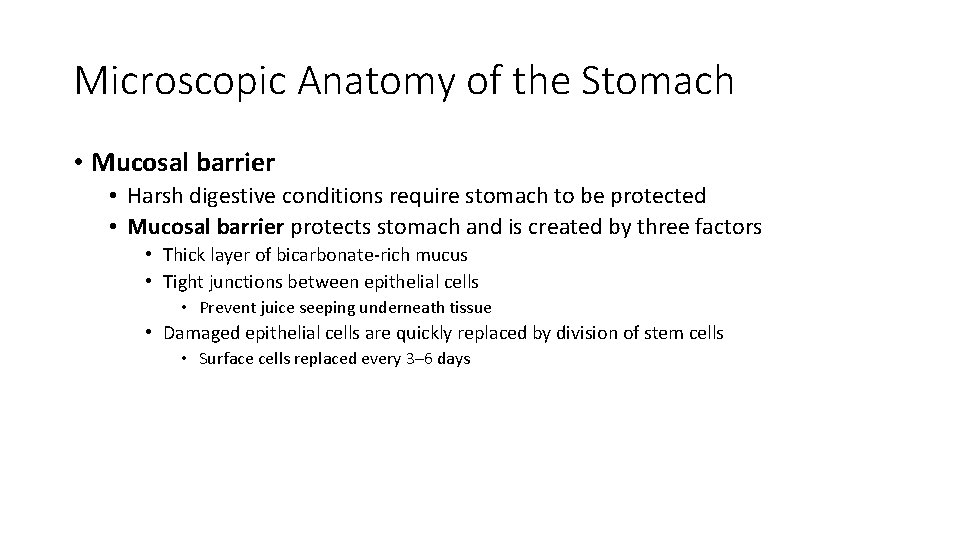
Microscopic Anatomy of the Stomach • Mucosal barrier • Harsh digestive conditions require stomach to be protected • Mucosal barrier protects stomach and is created by three factors • Thick layer of bicarbonate-rich mucus • Tight junctions between epithelial cells • Prevent juice seeping underneath tissue • Damaged epithelial cells are quickly replaced by division of stem cells • Surface cells replaced every 3– 6 days
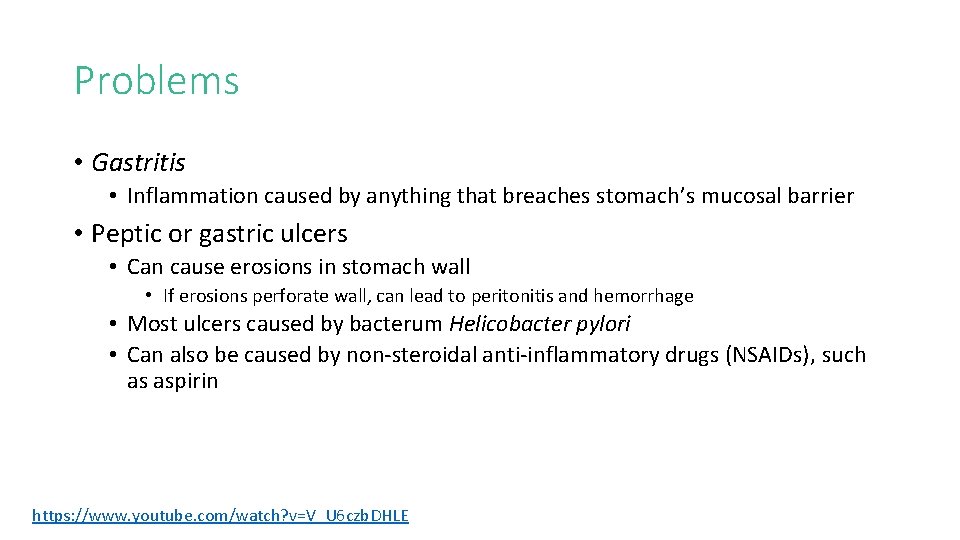
Problems • Gastritis • Inflammation caused by anything that breaches stomach’s mucosal barrier • Peptic or gastric ulcers • Can cause erosions in stomach wall • If erosions perforate wall, can lead to peritonitis and hemorrhage • Most ulcers caused by bacterum Helicobacter pylori • Can also be caused by non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin https: //www. youtube. com/watch? v=V_U 6 czb. DHLE
Barry Marshall and Robin Warren
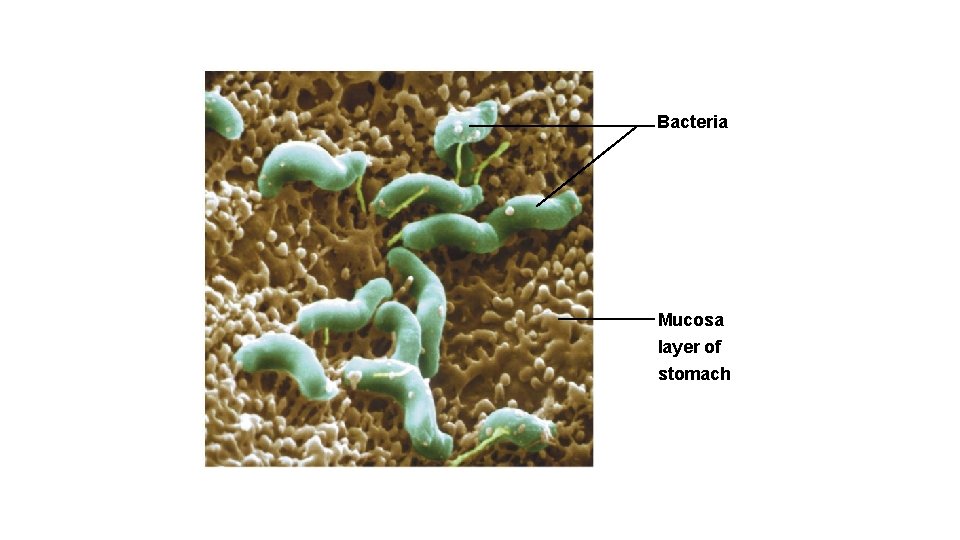
Bacteria Mucosa layer of stomach
- Slides: 58