Mechanical Ventilation I Presenter Michael Burton PAC Content
Mechanical Ventilation I Presenter: Michael Burton, PA-C Content Developer: John Heisler, PA-C
Objectives • Indications for Intubation • NIPPV vs Intubation • Vent Modes
Case Study ● 65 -year-old with an exacerbation of COPD ●Using accessory muscles and wheezing after 2 bronchodilator treatments ●HR 110, BP 160/110, RR 30, T 99°F(37. 2°C) ●ABG on 3 L/min O 2: p. H 7. 24 Pa. CO 2 60 mm. Hg Pa. O 2 65 mm. Hg
What type of respiratory support should be initiated? NC @ 3 L/min? NRB 15 L/min? Intubation? NIPPV/BIPAP?
Non-Invasive Ventilation • Positive Pressure ventilation without endotracheal tube • IPAP: Inspiratory Positive Airway pressure • EPAP: Expiratory Positive Airway pressure • “Bridge Therapy”
Good Candidates • COPD Exacerbation • Asthma • Pulmonary Edema Volume Overload ●Heart Failure • Obstructive Sleep Apnea/Obesity Hypoventilation Syndrome • Respiratory condition expected to improve in the next 24 – 48 hours • Cooperative Use for respiratory failure requires ICU in most centers
Bad Candidates • Unable • Facial to protect airway trauma • Vomiting/Aspiration • Hemodynamic • GI instability Bleeding • Unable to cooperate/agitated
What are advantages of using noninvasive positive pressure ventilation in OUR patient? ●Avoid complications of intubation ●Preserve airway reflexes ●Improve patient comfort ●Less need for sedation ●Shorter hospital/ICU stay ●Improved survival
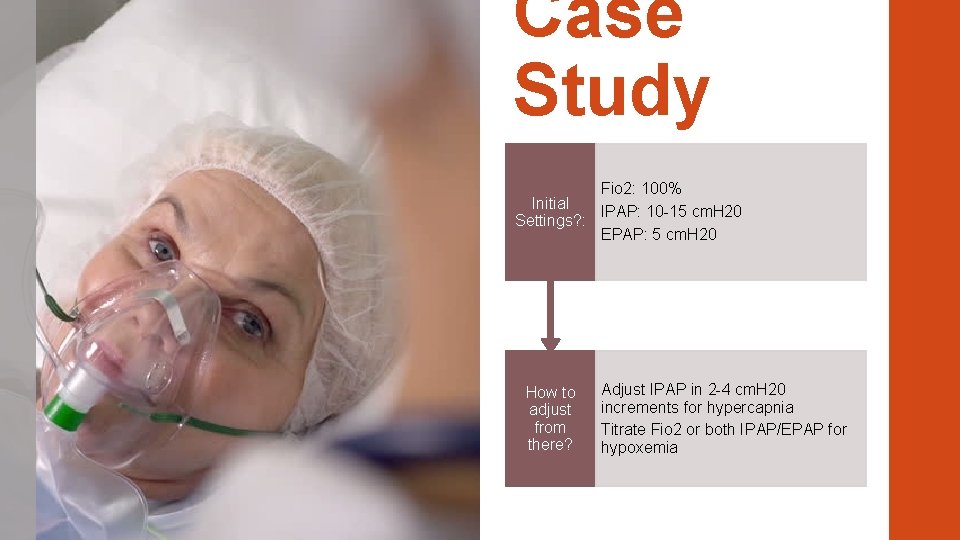
Case Study Fio 2: 100% Initial IPAP: 10 -15 cm. H 20 Settings? : EPAP: 5 cm. H 20 How to adjust from there? Adjust IPAP in 2 -4 cm. H 20 increments for hypercapnia Titrate Fio 2 or both IPAP/EPAP for hypoxemia
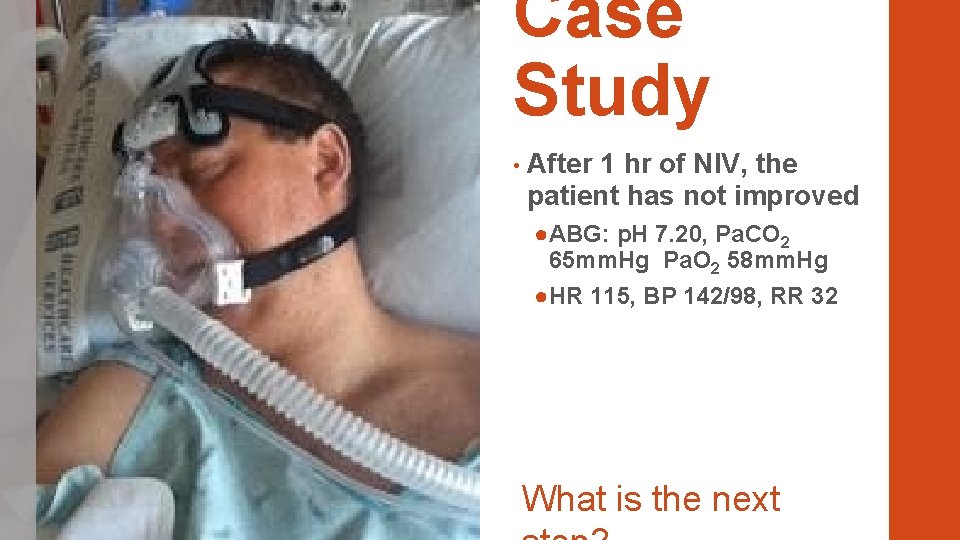
Case Study • After 1 hr of NIV, the patient has not improved ●ABG: p. H 7. 20, Pa. CO 2 65 mm. Hg Pa. O 2 58 mm. Hg ●HR 115, BP 142/98, RR 32 What is the next
1955: POLIO EPIDEMIC
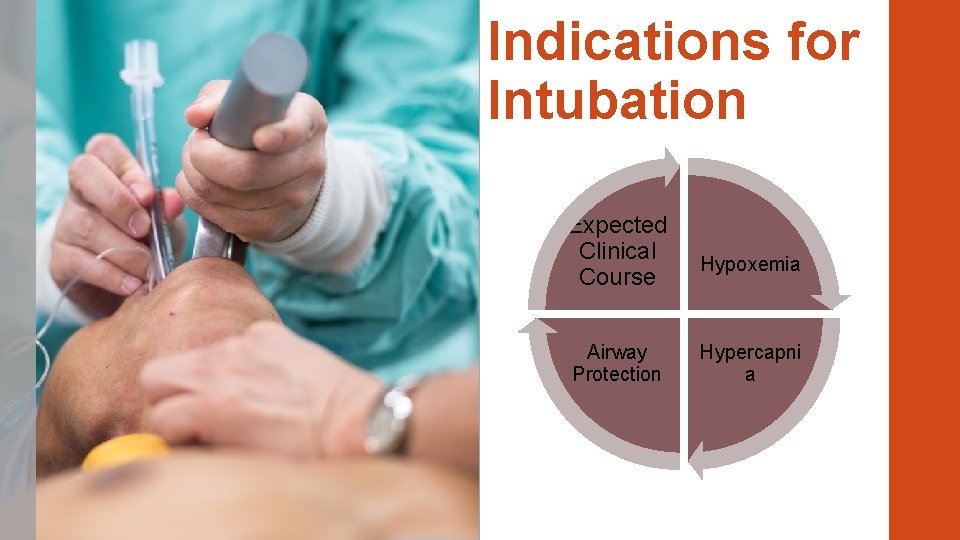
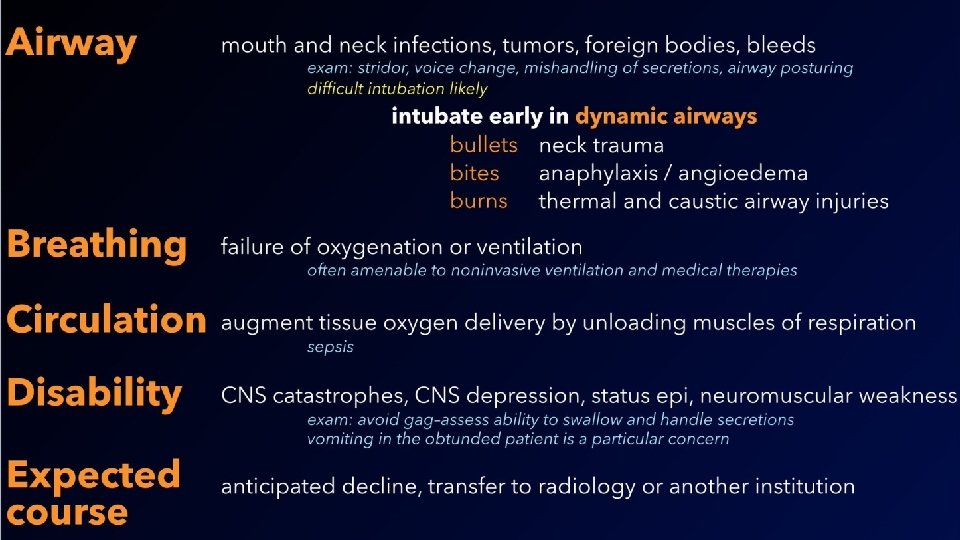
Indications for Intubation Expected Clinical Course Airway Protection Hypoxemia Hypercapni a
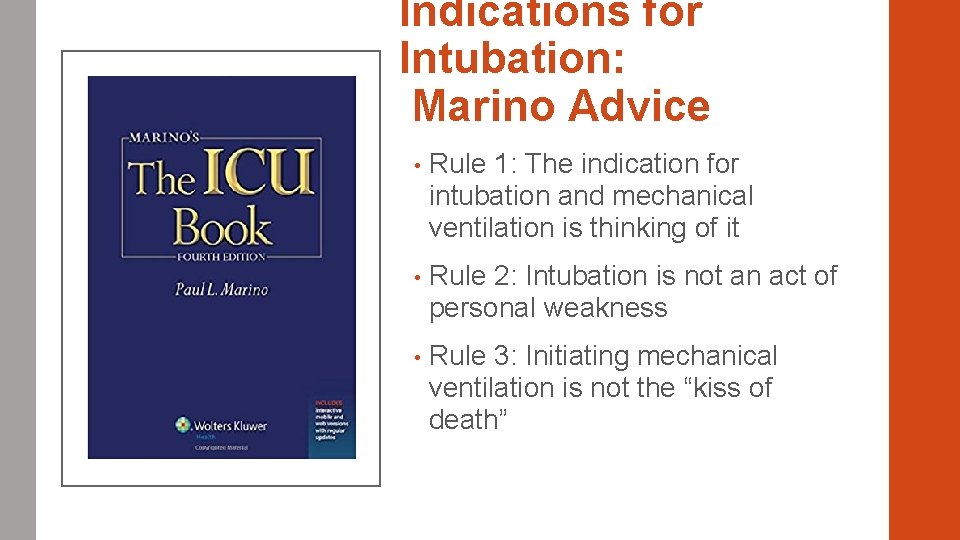
Indications for Intubation: Marino Advice • Rule 1: The indication for intubation and mechanical ventilation is thinking of it • Rule 2: Intubation is not an act of personal weakness • Rule 3: Initiating mechanical ventilation is not the “kiss of death”
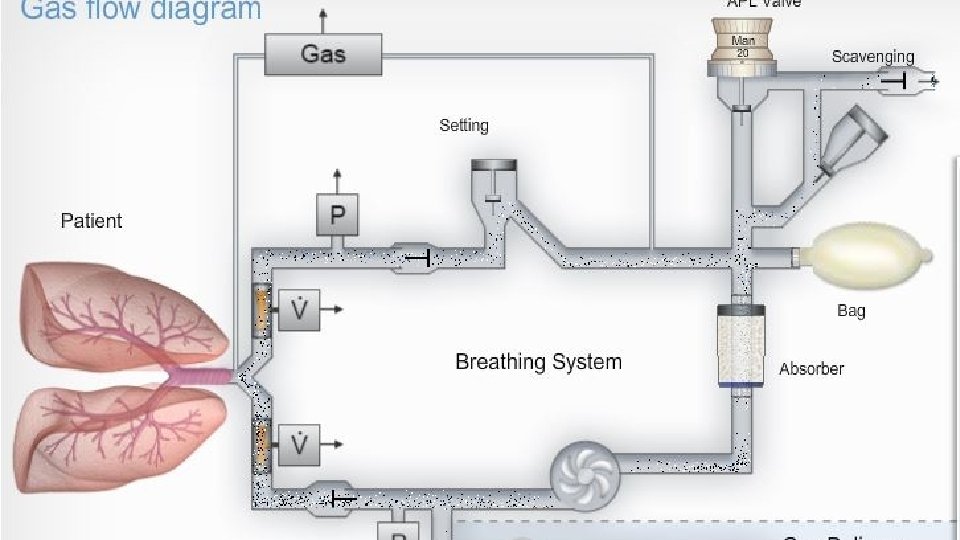
Vent Basics Vents are complicated……
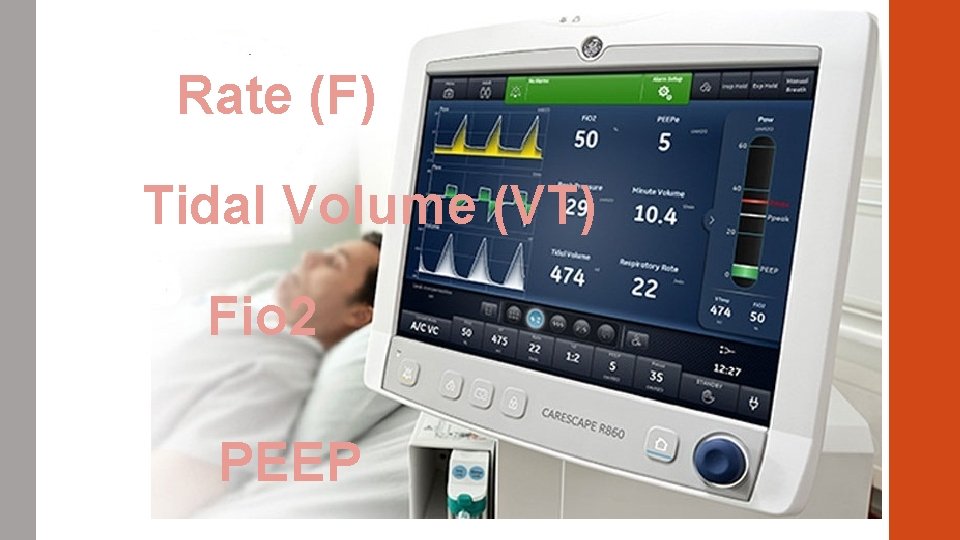
Rate (F) Tidal Volume (VT) Fio 2 PEEP
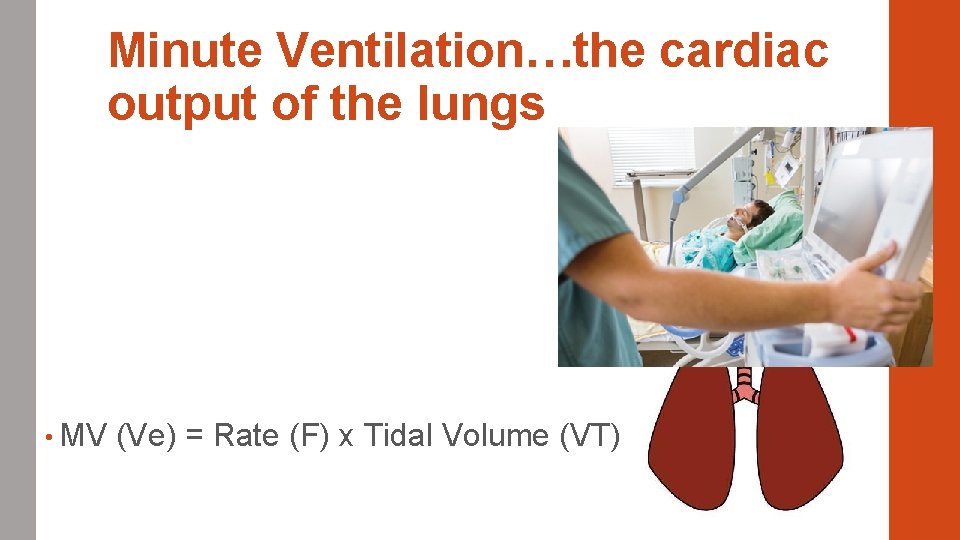
Minute Ventilation…the cardiac output of the lungs • MV (Ve) = Rate (F) x Tidal Volume (VT)
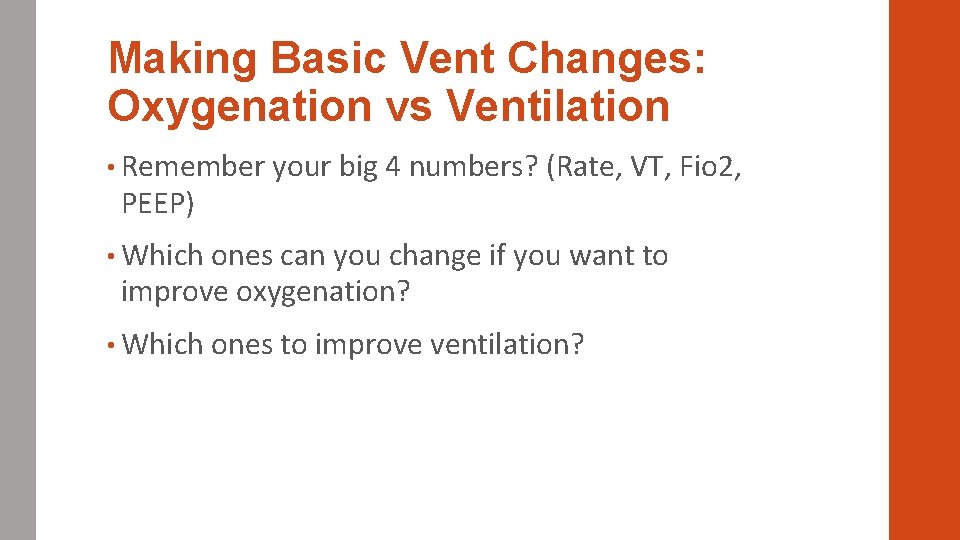
Making Basic Vent Changes: Oxygenation vs Ventilation • Remember your big 4 numbers? (Rate, VT, Fio 2, PEEP) • Which ones can you change if you want to improve oxygenation? • Which ones to improve ventilation?
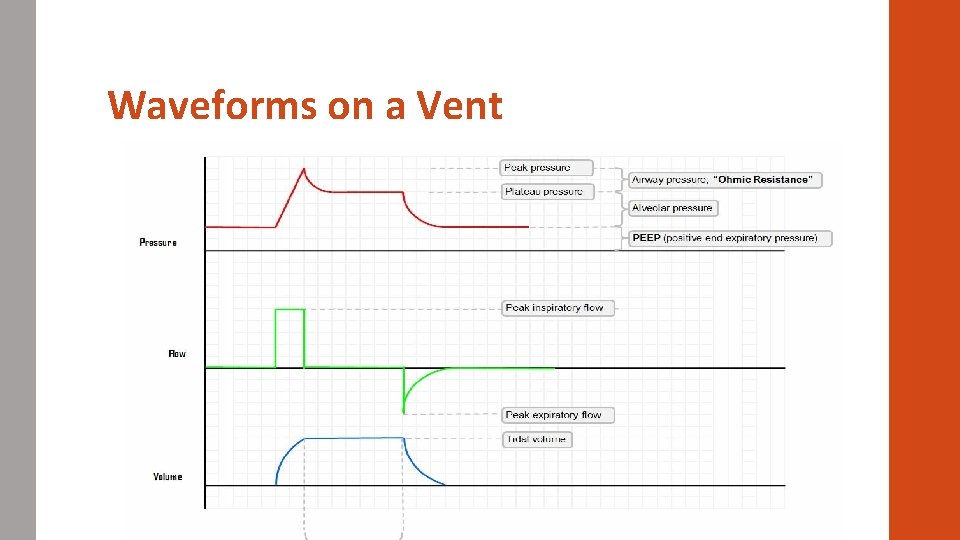
Waveforms on a Vent
Vent Modes • Volume Control ●Independent Variable: Volume ●Dependent Variable: Pressure • Pressure Control: ●Independent Variable: Pressure ●Dependent Variable: Volume
Understanding Modes: Assist Control (ACVC) • Preset Tidal Volume • Preset Rate • What happens when patient initiates a breath? • How is this different than other modes? • What are the advantages and disadvantages?
Modes: Pressure Control (PCV+) • Preset Pressure (Pinsp) • Present Rate • What happens when the patient initiates a breath? • “Time cycled” • What are the advantages and disadvantages?
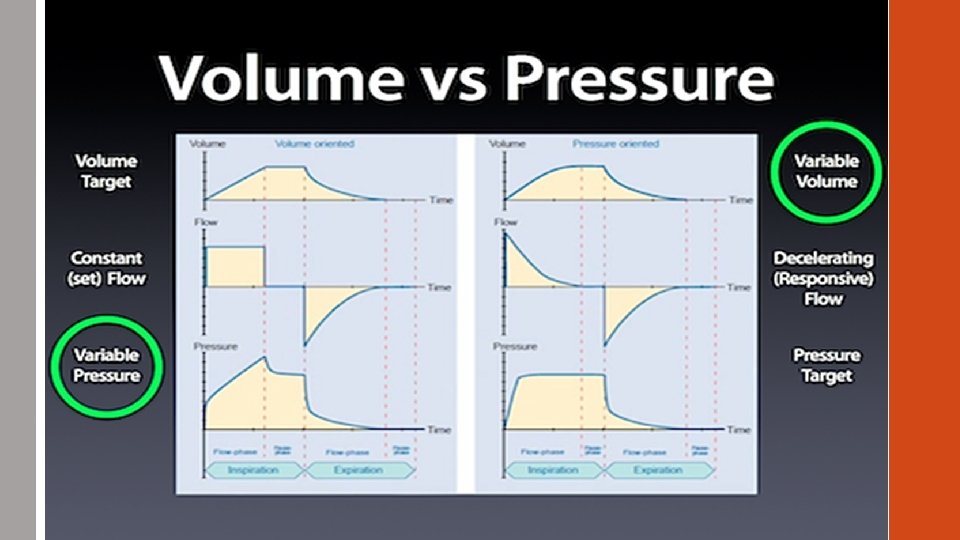
Volume vs Pressure • Which is better? • Why do we use volume? • Shouldn’t pressure be better since causes less barotrauma? • Why do some groups use one and others a different mode?
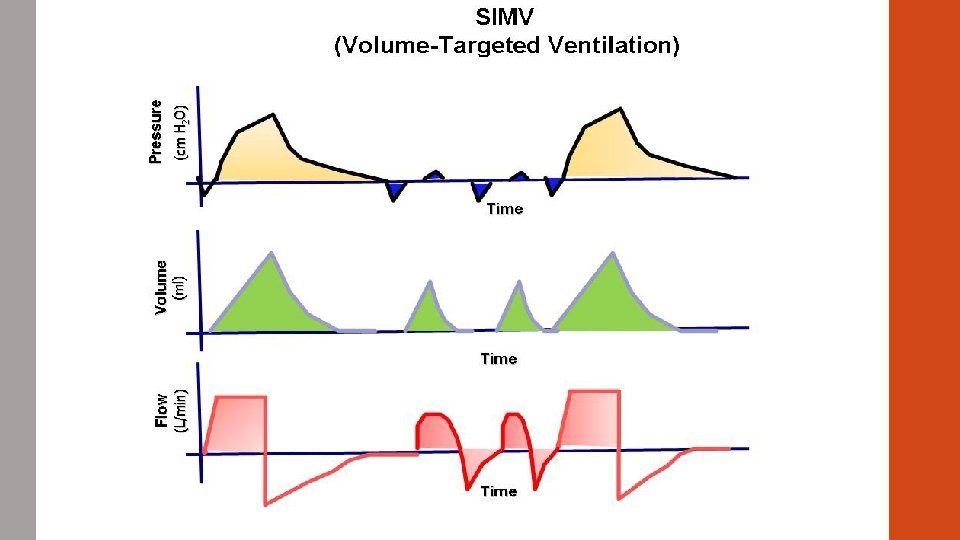
SIMV: Synchronized Intermittent Mandatory Ventilation • Volume or Pressure Driven (SIMV-VC) • What happens when the patient triggers breaths? ●Patient determines the volume ●Pressure Support can be added to these breaths • Why? • When to use?
Pressure Support (PS) • Spontaneously breathing patients • Pressure given to “overcome the circuit” • Why would we use it? ●Weaning mode
Next time • ARDS • Making ventilator changes • When to extubate? ● SBT’s • PAD
- Slides: 30