Mechanical Ventilation A Primer How to save a


- Slides: 69
Mechanical Ventilation: A Primer (How to save a life when I’m alone in the middle of the night) Nick Mohr, MD Assistant Professor Department of Emergency Medicine Division of Critical Care, Department of Anesthesia University of Iowa Carver College of Medicine
Objectives • To review basic mechanical ventilation theory and terminology • To define an algorithmic approach to mechanical ventilation in the emergency department • To explore algorithms for troubleshooting ventilation and oxygenation problems • To discuss specific clinical scenarios requiring specialized ventilation strategies
Conflicts of Interest • This speaker has no financial relationships to disclose. • Topics discussed in this lecture a component of the University of Iowa Visiting Professor Program Conference Series. • The content of this lecture was developed following an extensive literature search and contains up-todate, evidence-based information.
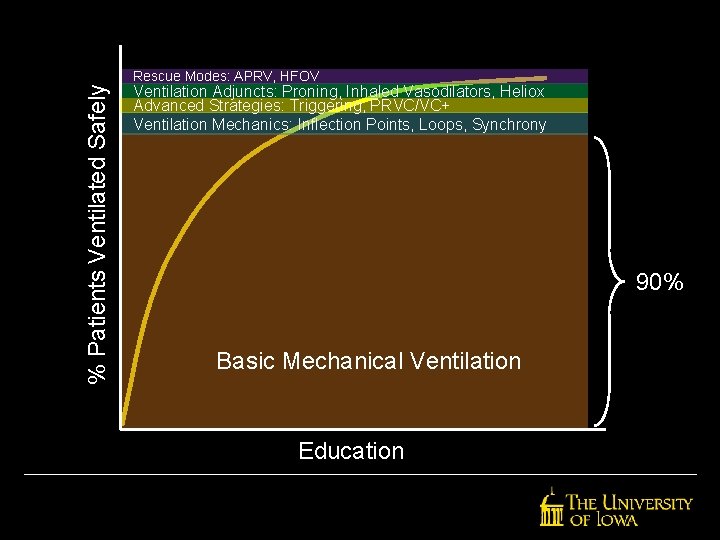
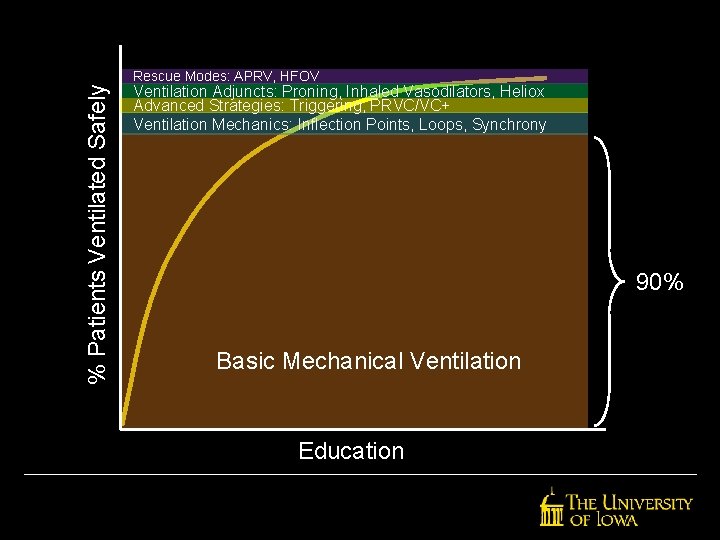
% Patients Ventilated Safely Rescue Modes: APRV, HFOV Ventilation Adjuncts: Proning, Inhaled Vasodilators, Heliox Advanced Strategies: Triggering, PRVC/VC+ Ventilation Mechanics: Inflection Points, Loops, Synchrony 90% Basic Mechanical Ventilation Education
What is the goal of mechanical ventilation?

Definitions
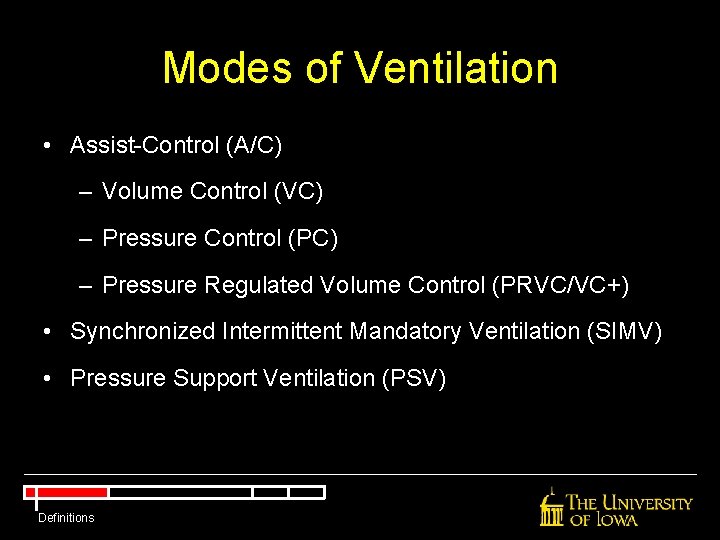
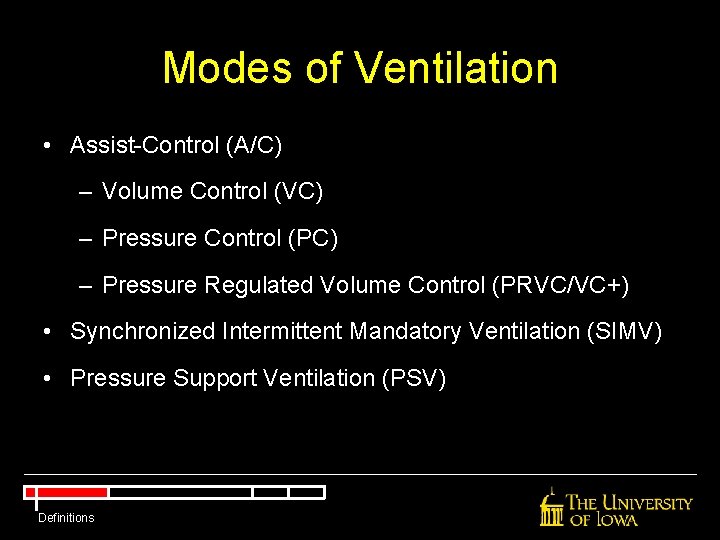
Modes of Ventilation • Assist-Control (A/C) – Volume Control (VC) – Pressure Control (PC) – Pressure Regulated Volume Control (PRVC/VC+) • Synchronized Intermittent Mandatory Ventilation (SIMV) • Pressure Support Ventilation (PSV) Definitions
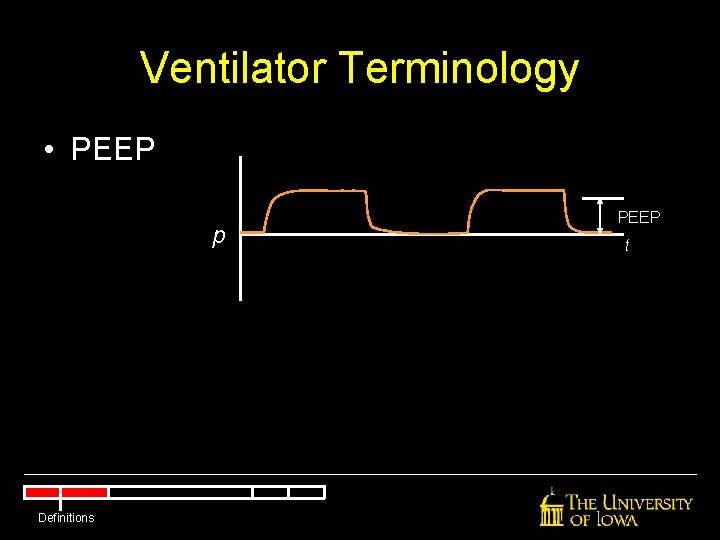
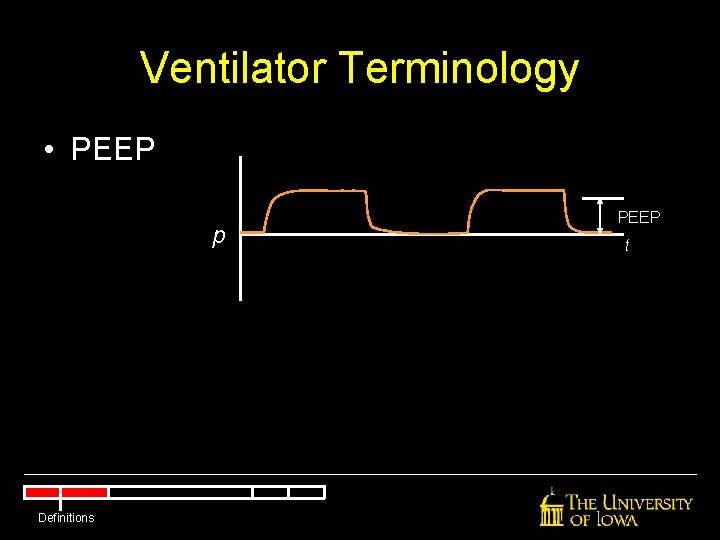
Ventilator Terminology • PEEP p Definitions PEEP t
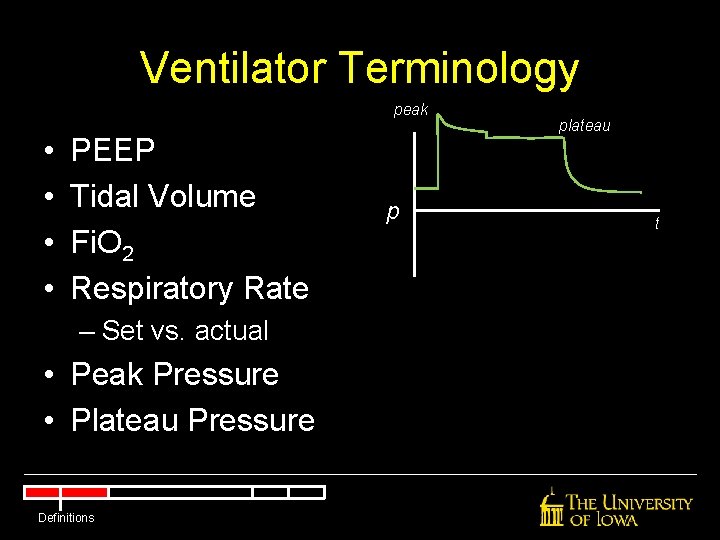
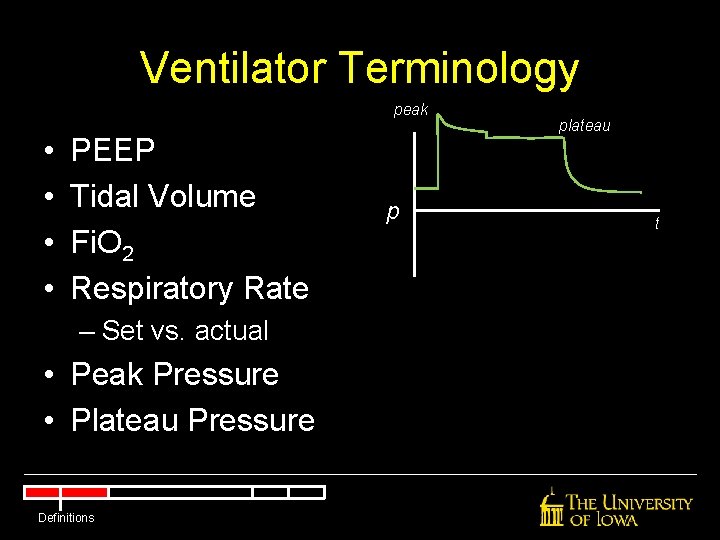
Ventilator Terminology peak • • PEEP Tidal Volume Fi. O 2 Respiratory Rate – Set vs. actual • Peak Pressure • Plateau Pressure Definitions p plateau t
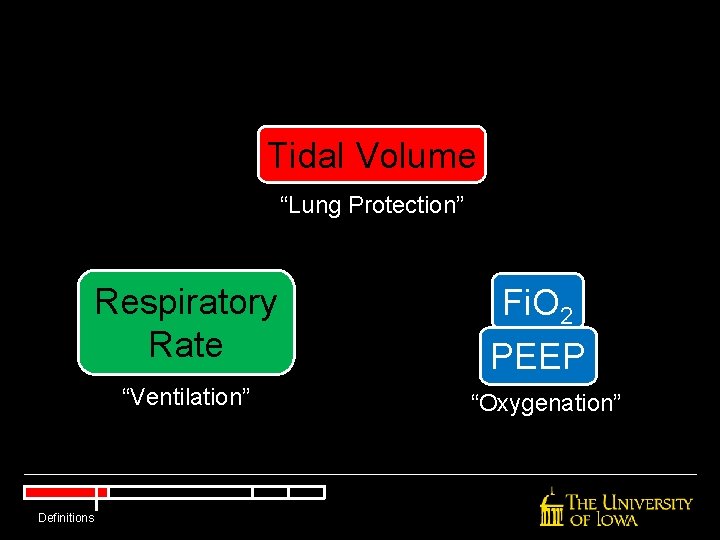
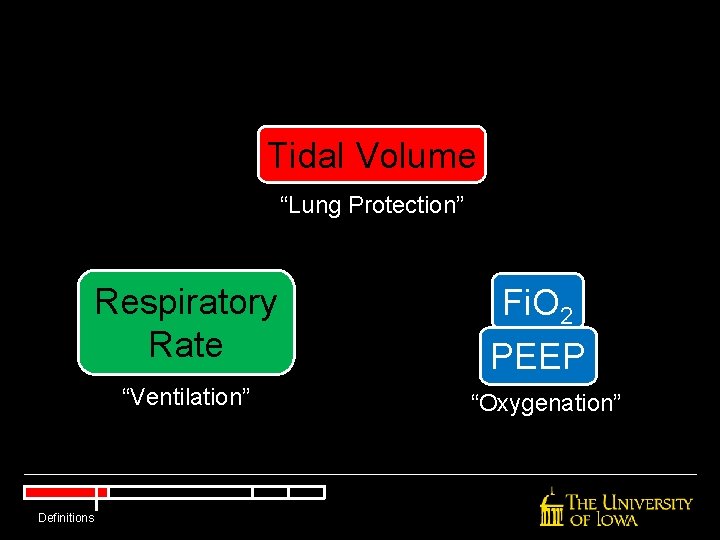
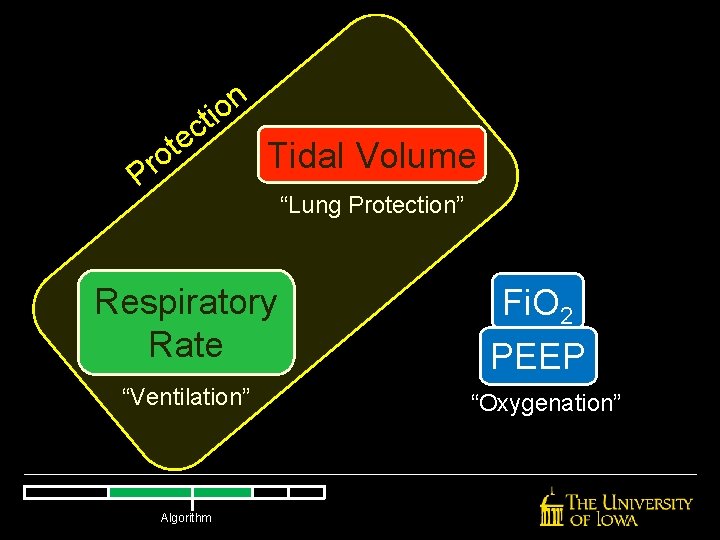
Tidal Volume “Lung Protection” Respiratory Rate “Ventilation” Definitions Fi. O 2 PEEP “Oxygenation”
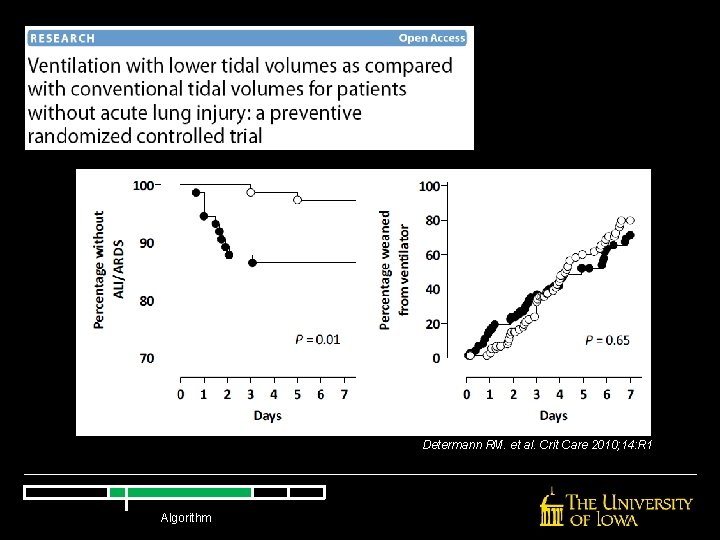
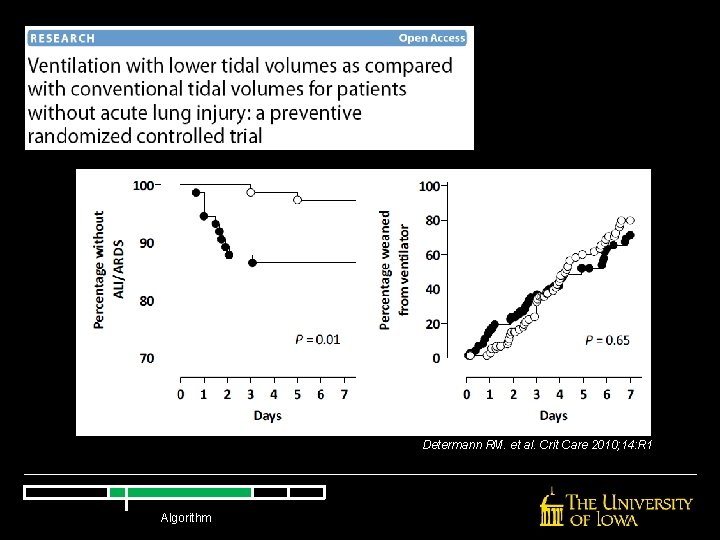
Determann RM. et al. Crit Care 2010; 14: R 1 Algorithm
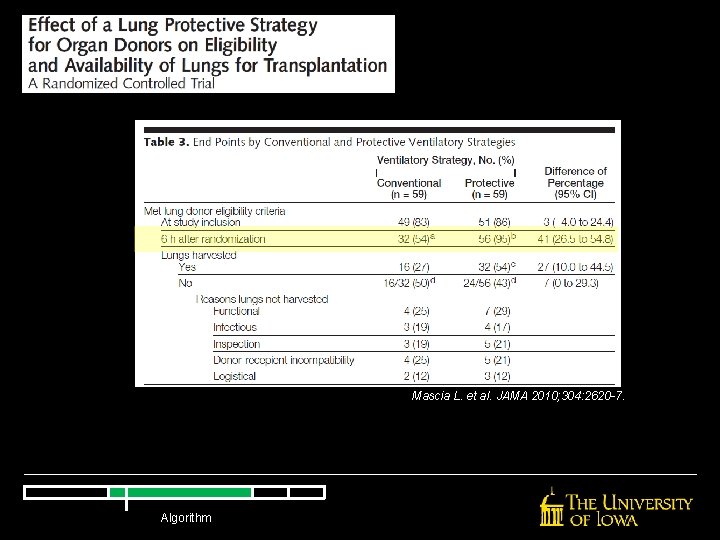
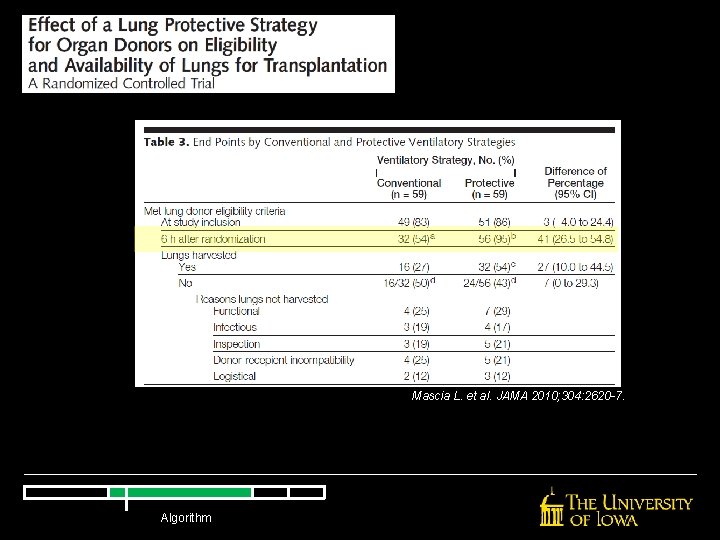
Mascia L. et al. JAMA 2010; 304: 2620 -7. Algorithm
Ventilation Algorithm Courtesy Scott Weingart, MD Algorithm
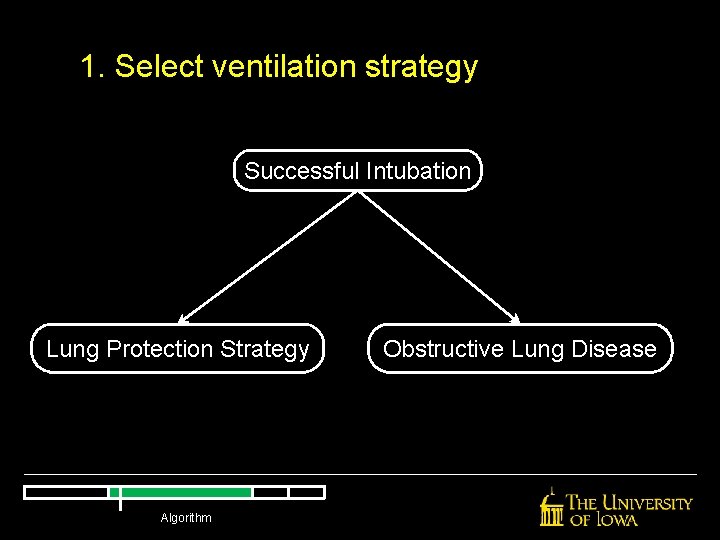
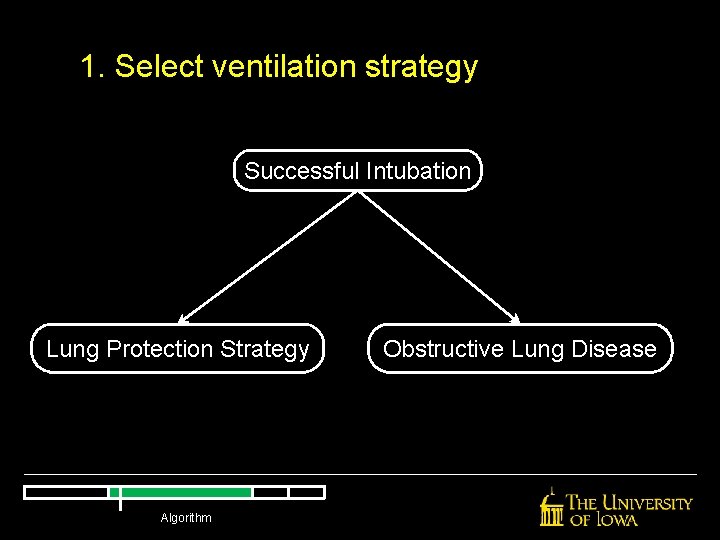
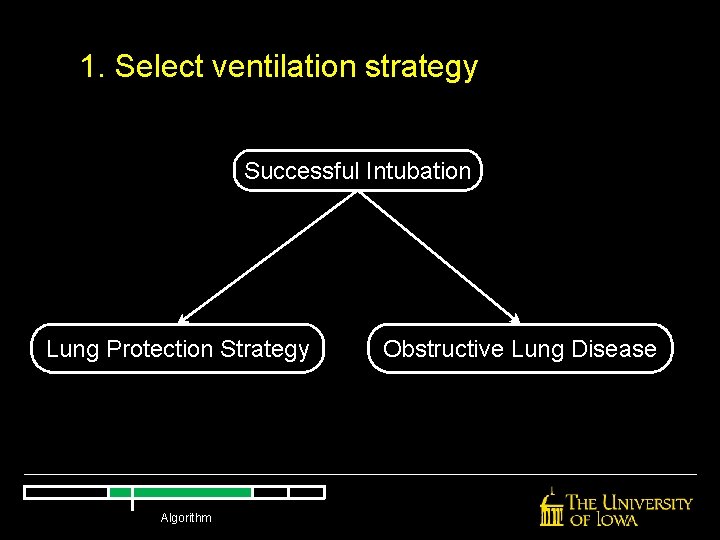
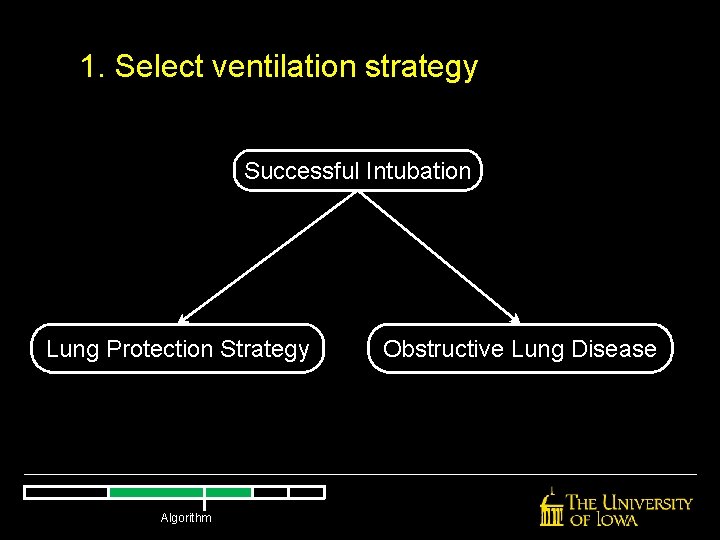
1. Select ventilation strategy Successful Intubation Lung Protection Strategy Algorithm Obstructive Lung Disease
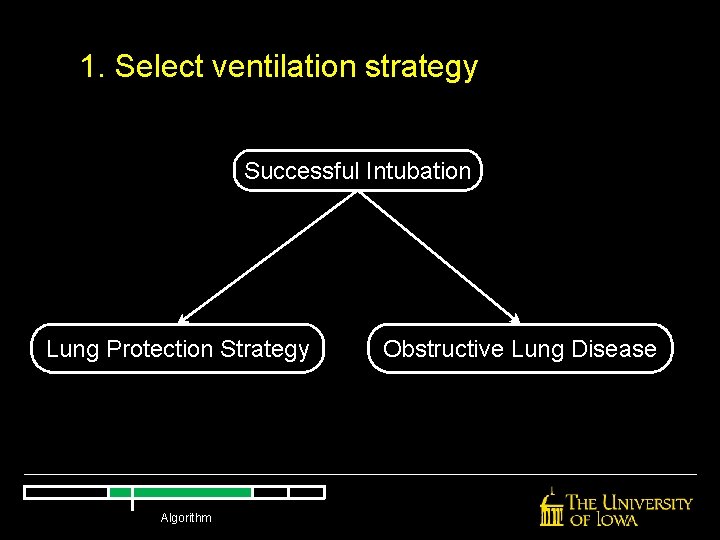
1. Select ventilation strategy Successful Intubation Lung Protection Strategy Algorithm Obstructive Lung Disease
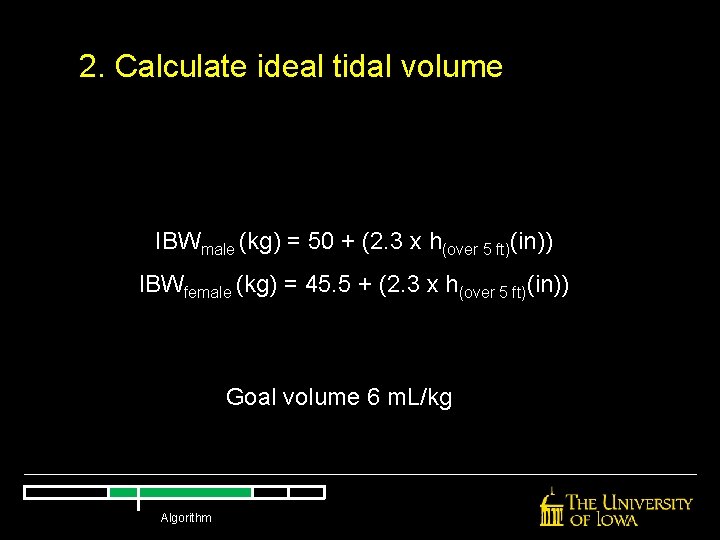
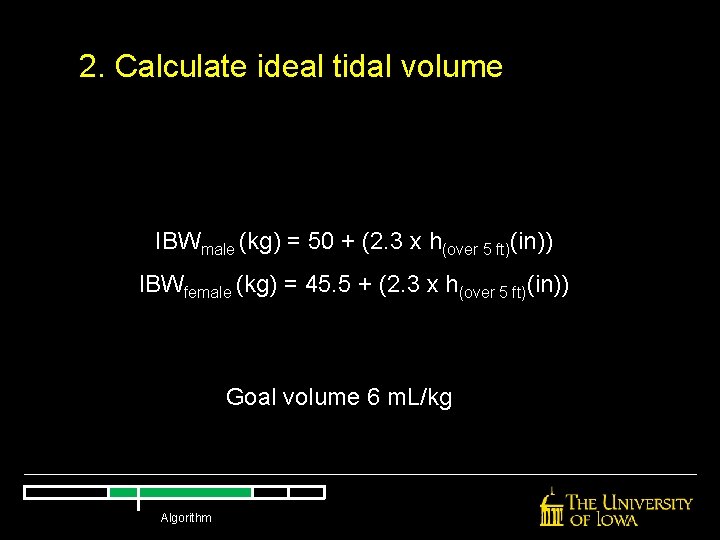
2. Calculate ideal tidal volume IBWmale (kg) = 50 + (2. 3 x h(over 5 ft)(in)) IBWfemale (kg) = 45. 5 + (2. 3 x h(over 5 ft)(in)) Goal volume 6 m. L/kg Algorithm
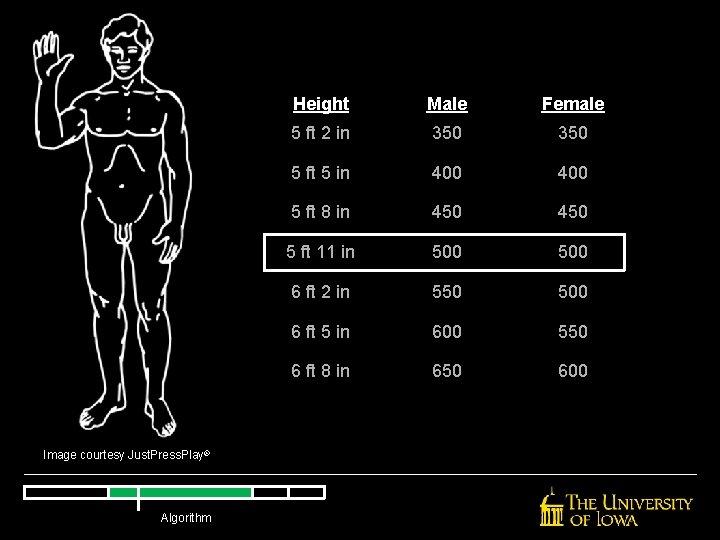
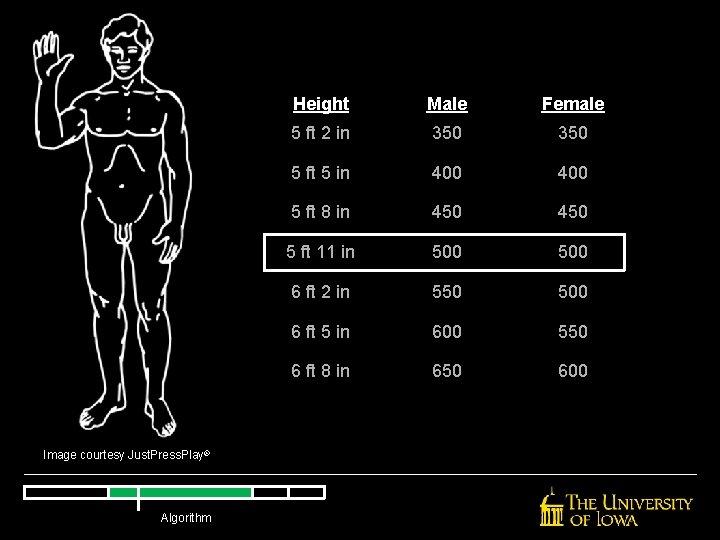
Image courtesy Just. Press. Play® Algorithm Height Male Female 5 ft 2 in 350 5 ft 5 in 400 5 ft 8 in 450 5 ft 11 in 500 6 ft 2 in 550 500 6 ft 5 in 600 550 6 ft 8 in 650 600
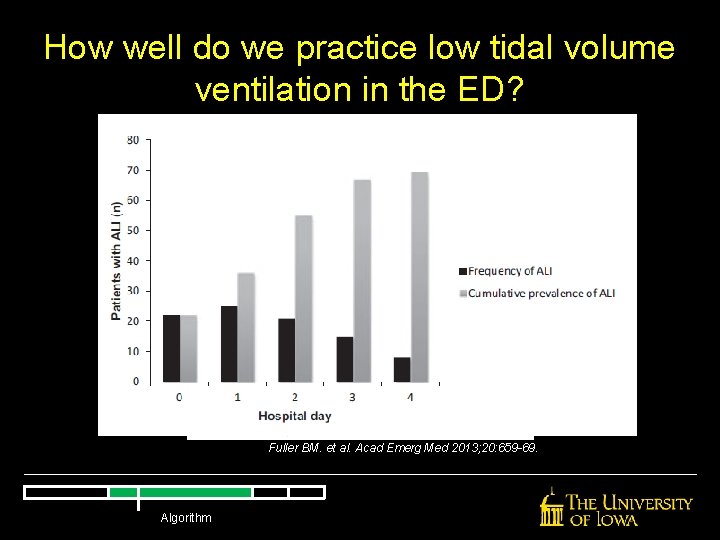
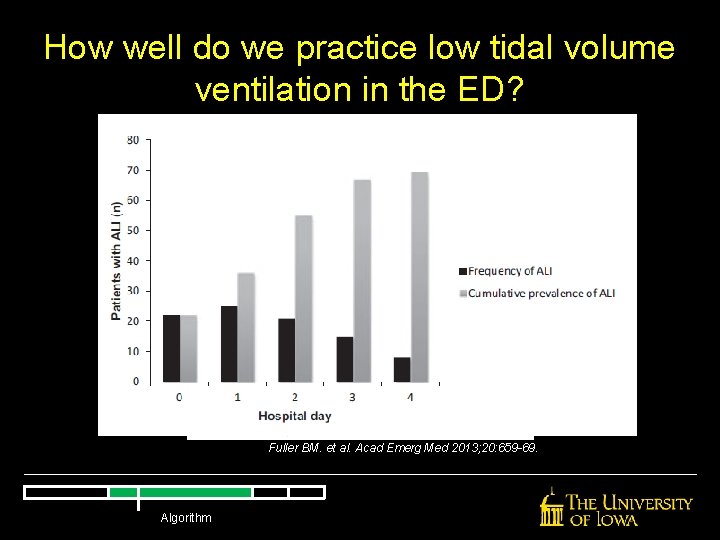
How well do we practice low tidal volume ventilation in the ED? Fuller BM. et al. Acad Emerg Med 2013; 20: 659 -69. Algorithm
3. Select respiratory rate Try to match required minute ventilation Usually start at 14 -18 breaths/minute Check a blood gas Algorithm
4. Select oxygenation parameters Start all ventilated patients at Fi. O 2 = 100% Wean aggressively Algorithm
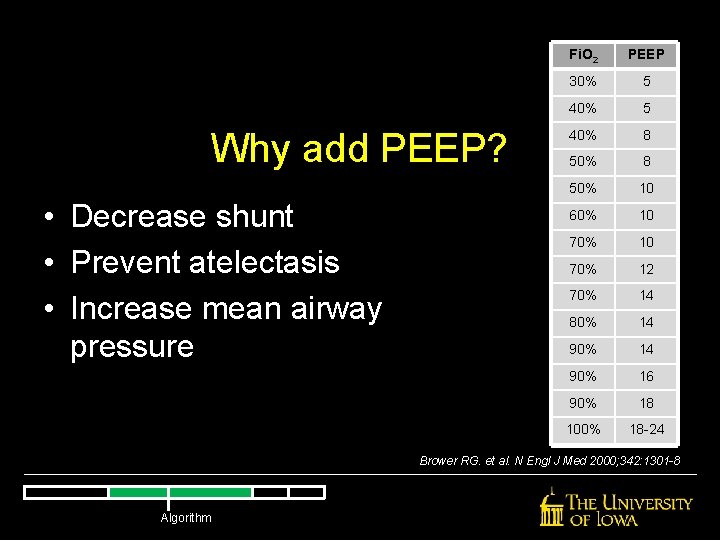
Why add PEEP? Algorithm
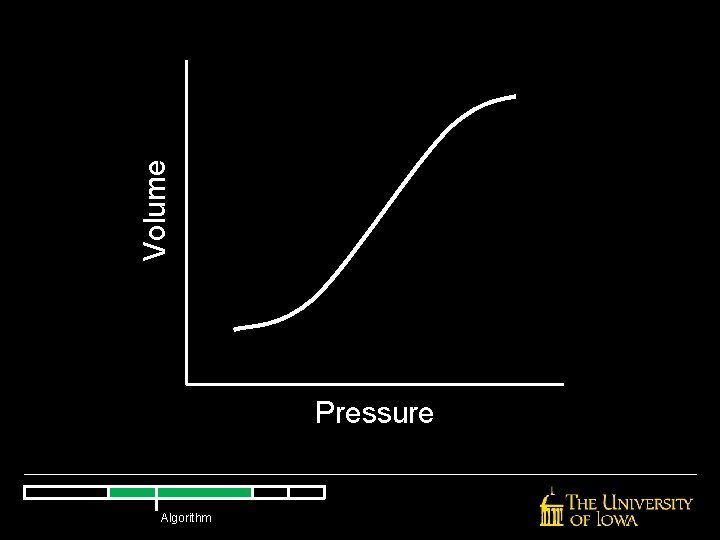
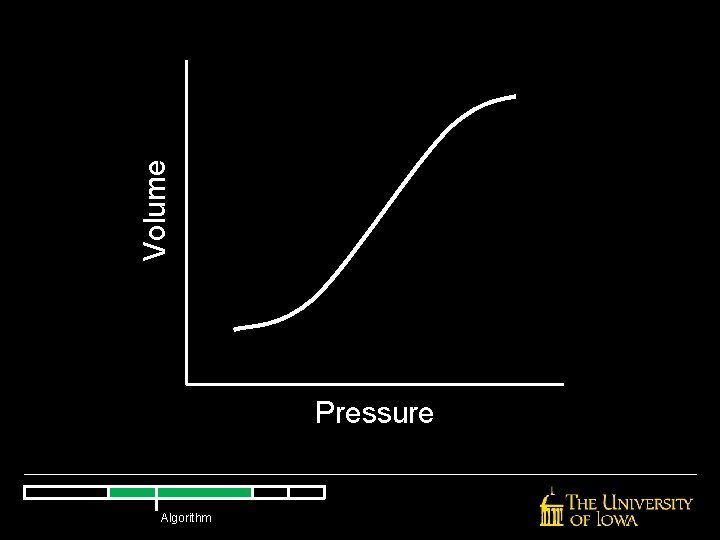
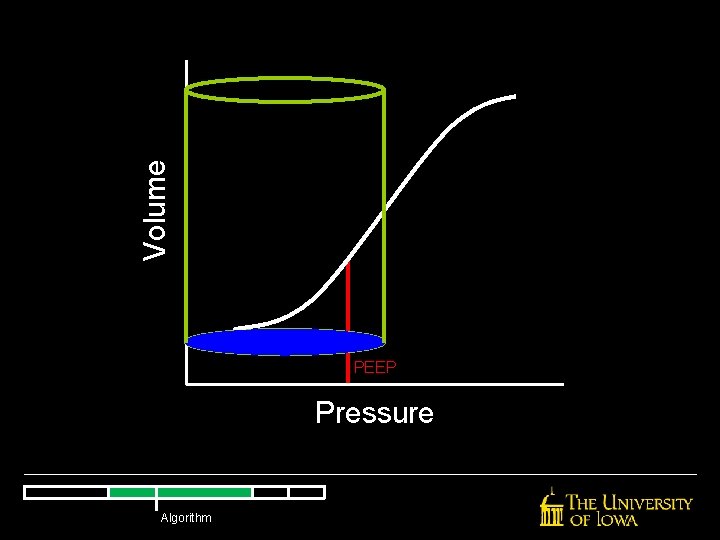
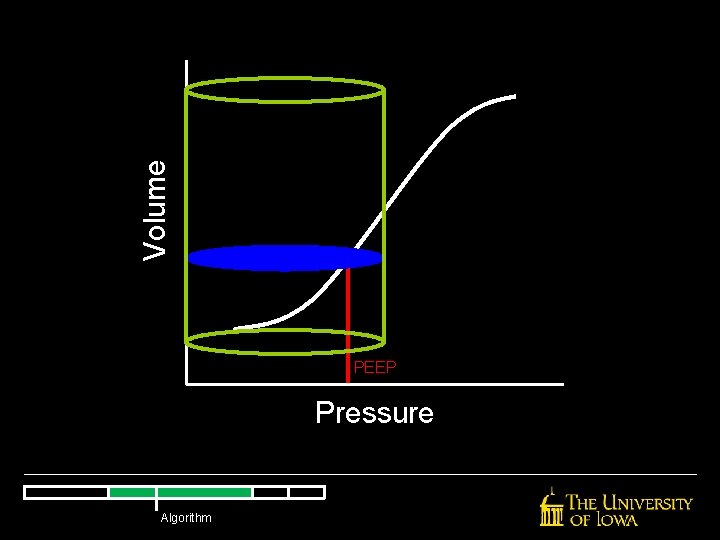
Volume Pressure Algorithm
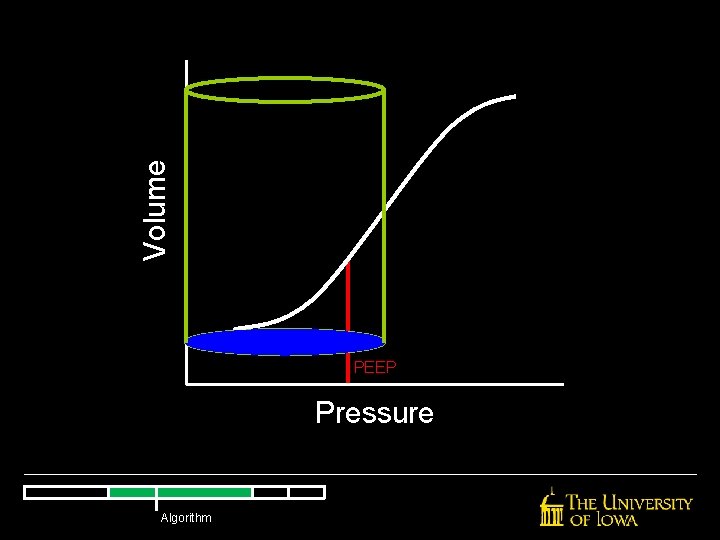
Volume PEEP Pressure Algorithm
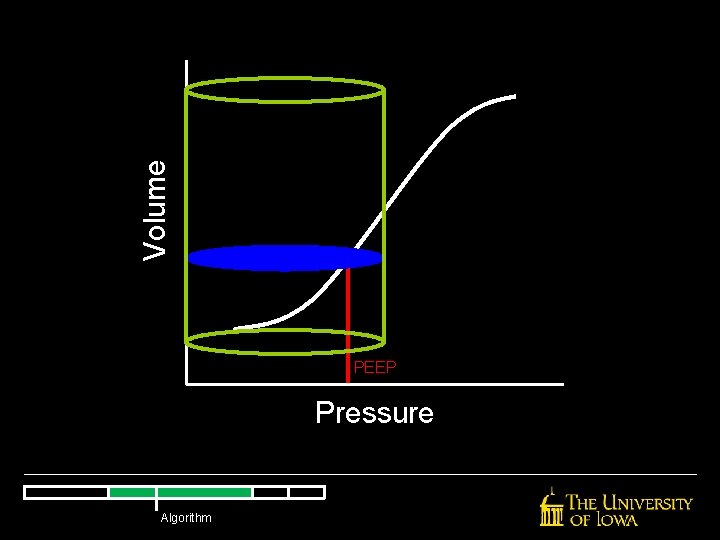
Volume PEEP Pressure Algorithm
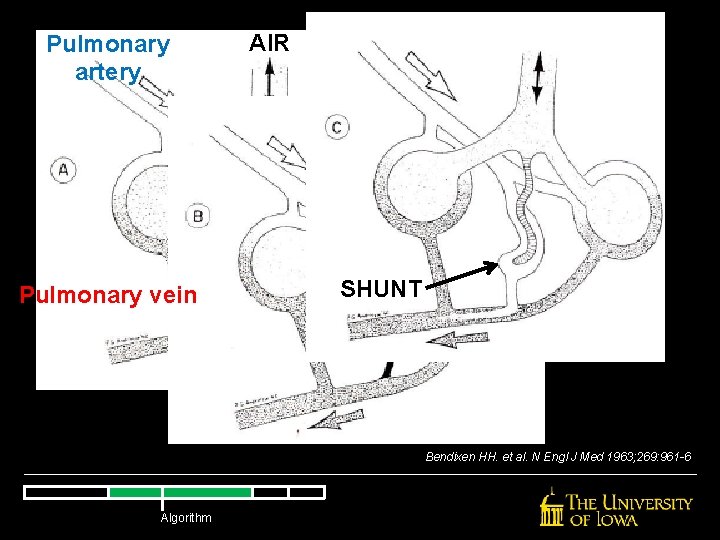
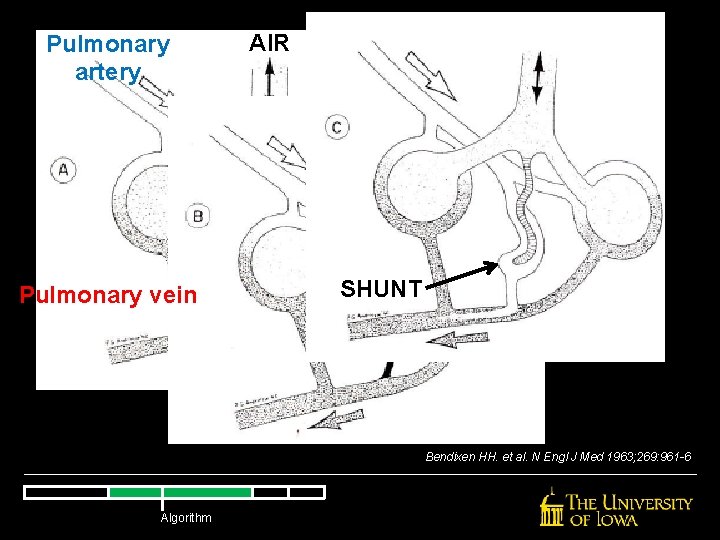
Pulmonary artery Pulmonary vein AIR SHUNT Bendixen HH. et al. N Engl J Med 1963; 269: 961 -6 Algorithm
Slutsky AS. et al. NEJM 2006; 354: 1839 -41 Algorithm
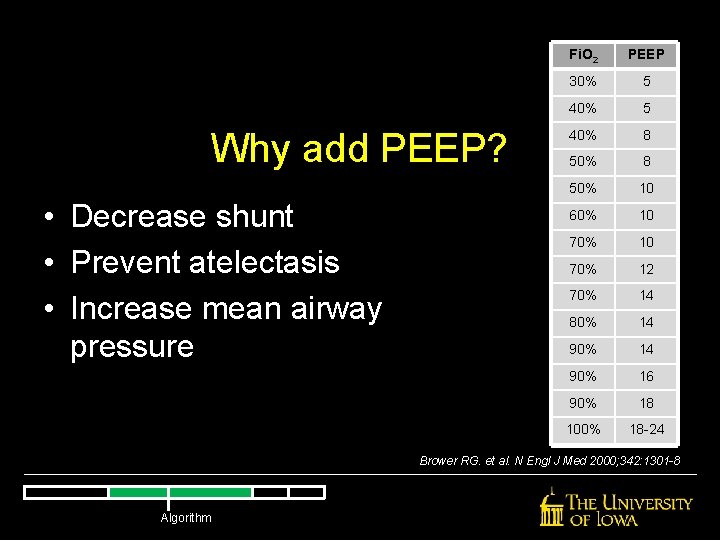
Why add PEEP? • Decrease shunt • Prevent atelectasis • Increase mean airway pressure Fi. O 2 PEEP 30% 5 40% 8 50% 10 60% 10 70% 12 70% 14 80% 14 90% 16 90% 18 100% 18 -24 Brower RG. et al. N Engl J Med 2000; 342: 1301 -8 Algorithm
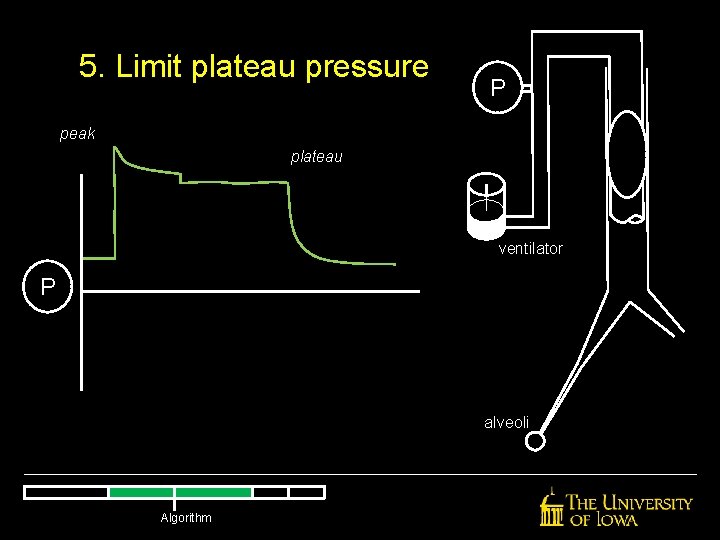
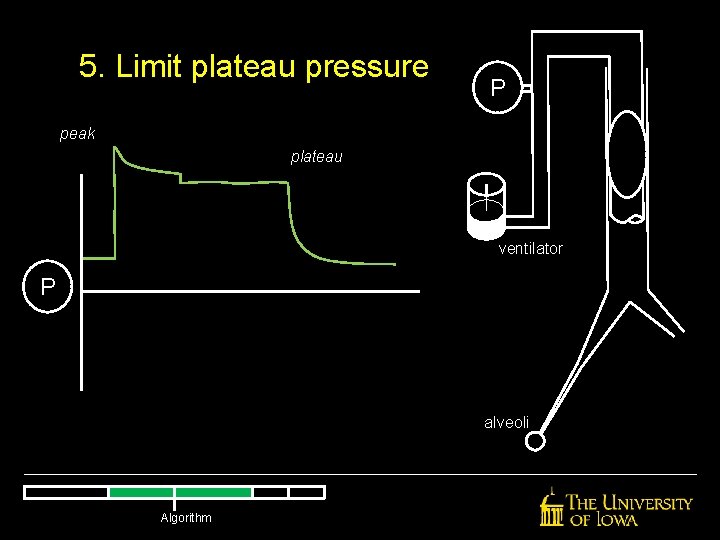
5. Limit plateau pressure P peak plateau ventilator P alveoli Algorithm
6. Check blood gas, reassess Check ABG/VBG at 15 -30 minutes Correlate with Et. CO 2 Algorithm
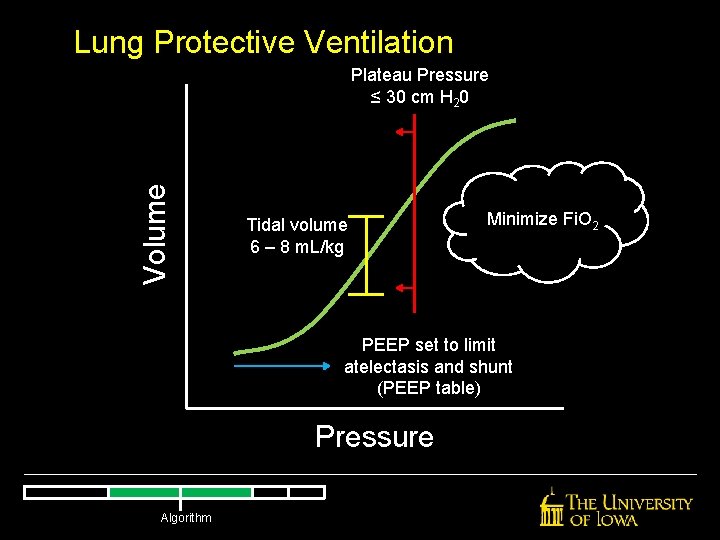
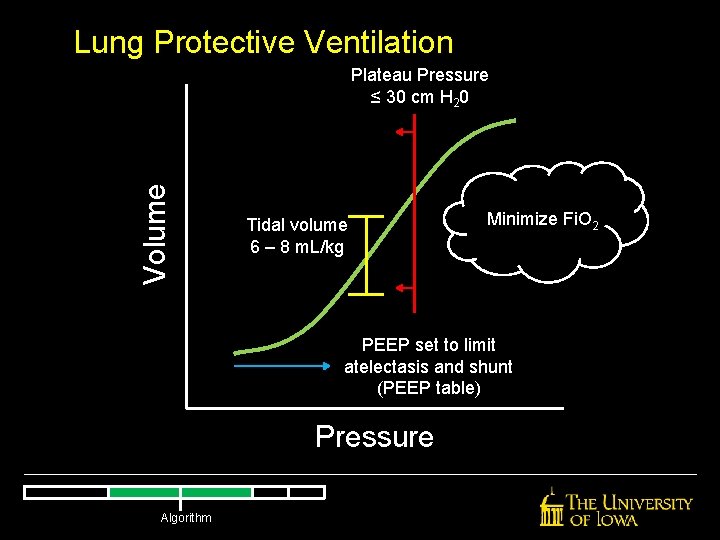
Lung Protective Ventilation Volume Plateau Pressure ≤ 30 cm H 20 Tidal volume 6 – 8 m. L/kg Minimize Fi. O 2 PEEP set to limit atelectasis and shunt (PEEP table) Pressure Algorithm
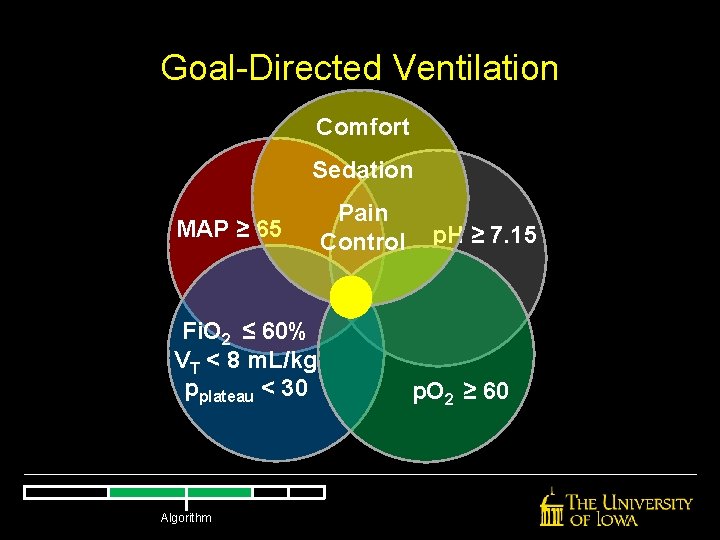
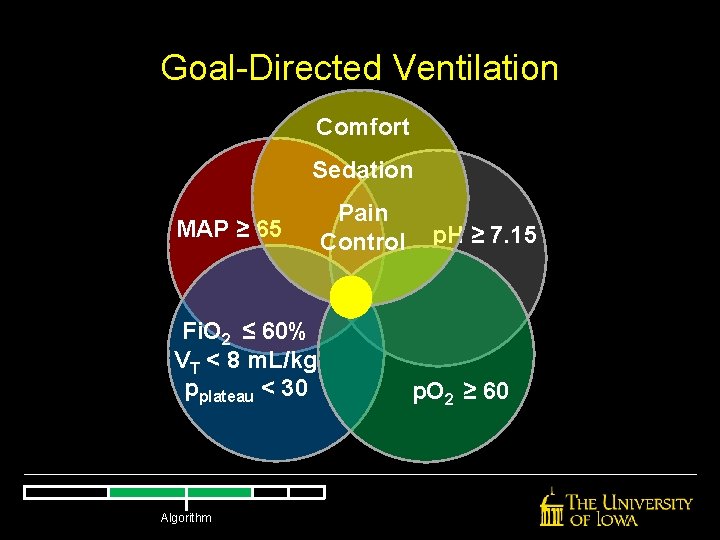
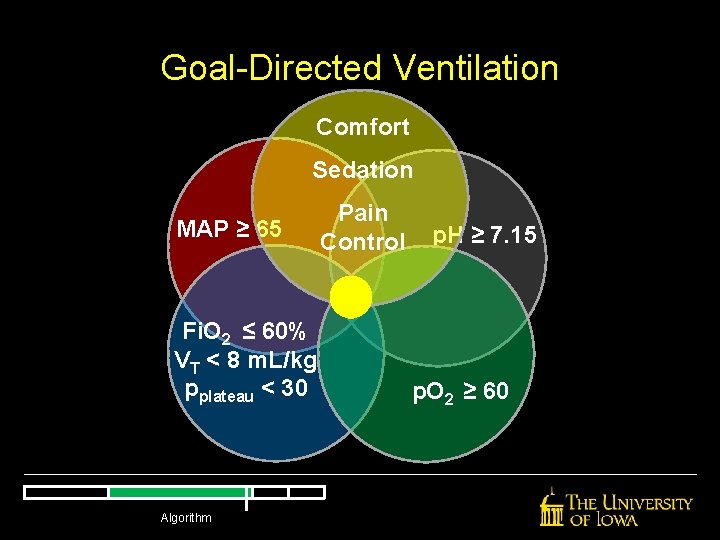
Goal-Directed Ventilation Comfort Sedation MAP ≥ 65 Fi. O 2 ≤ 60% VT < 8 m. L/kg pplateau < 30 Algorithm Pain Control p. H ≥ 7. 15 p. O 2 ≥ 60
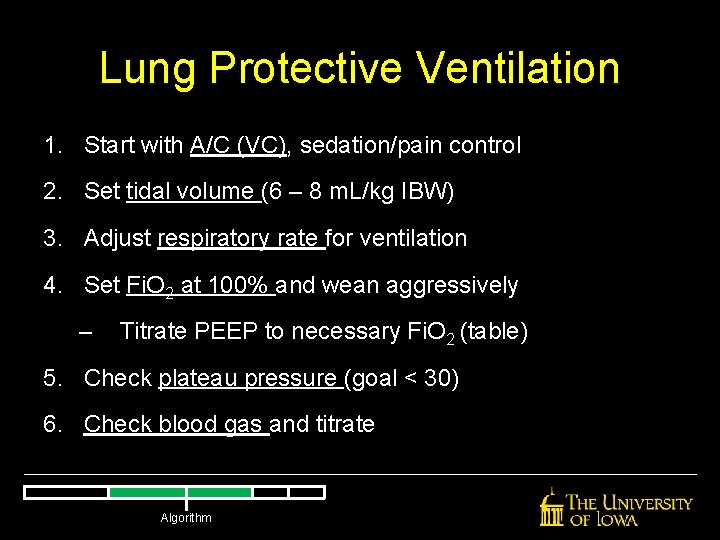
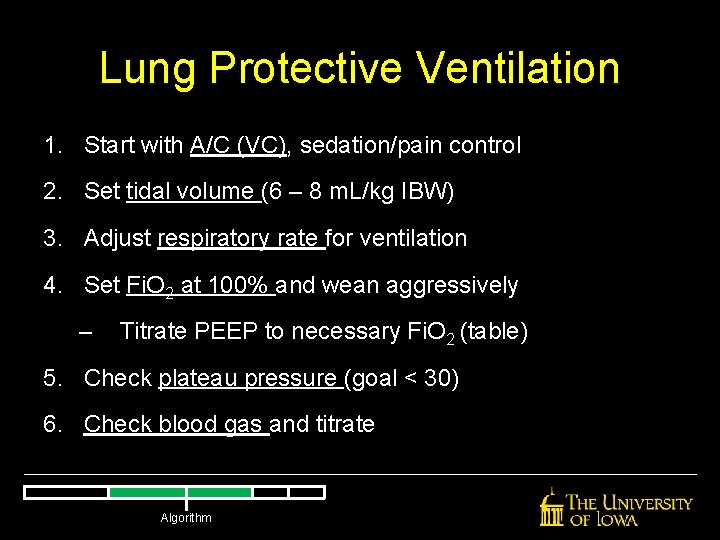
Lung Protective Ventilation 1. Start with A/C (VC), sedation/pain control 2. Set tidal volume (6 – 8 m. L/kg IBW) 3. Adjust respiratory rate for ventilation 4. Set Fi. O 2 at 100% and wean aggressively – Titrate PEEP to necessary Fi. O 2 (table) 5. Check plateau pressure (goal < 30) 6. Check blood gas and titrate Algorithm
How does ventilation differ in patients with obstructive lung disease? Algorithm
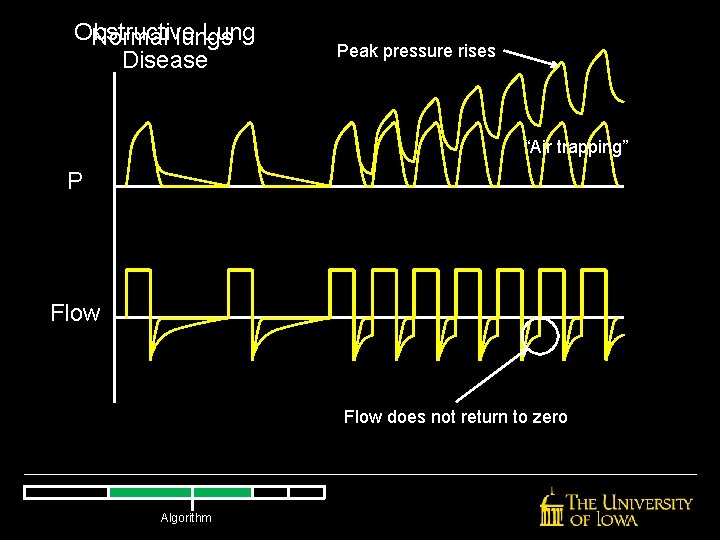
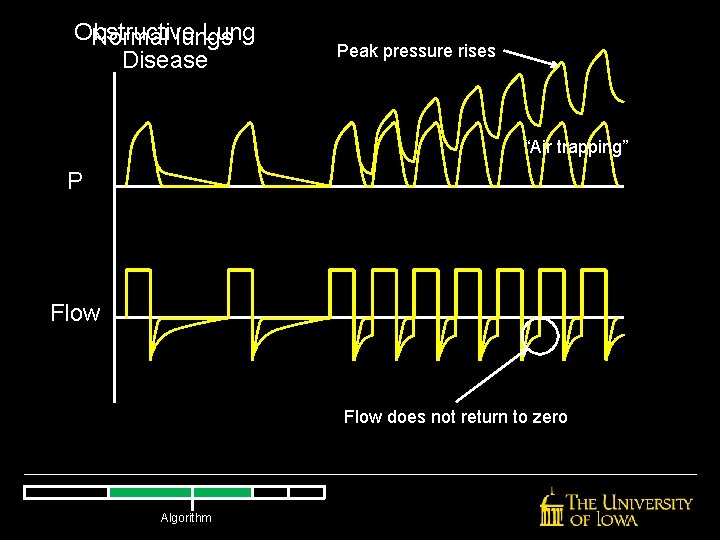
Obstructive Lung Normal lungs Disease Peak pressure rises “Air trapping” P Flow does not return to zero Algorithm
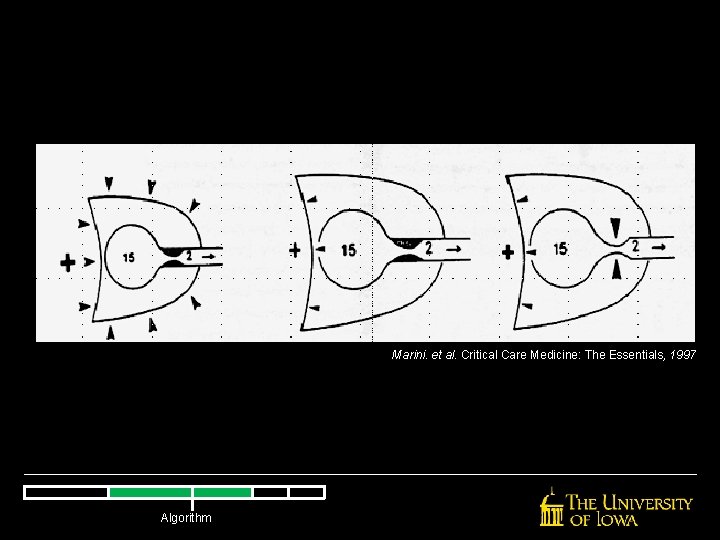
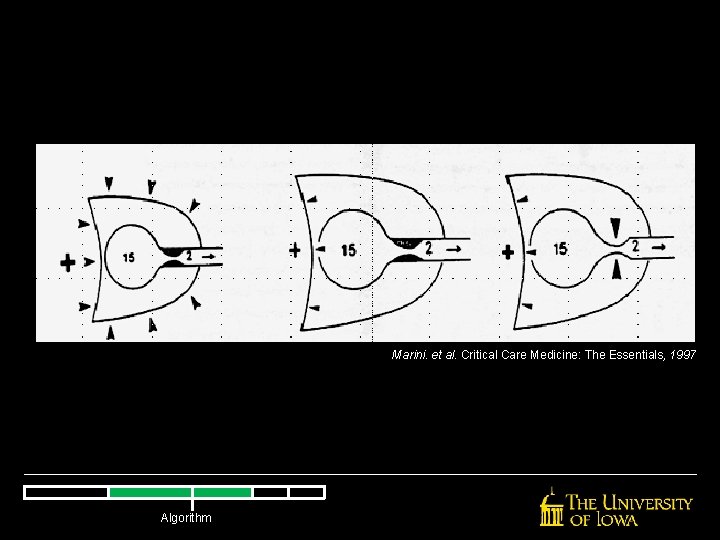
Marini. et al. Critical Care Medicine: The Essentials, 1997 Algorithm
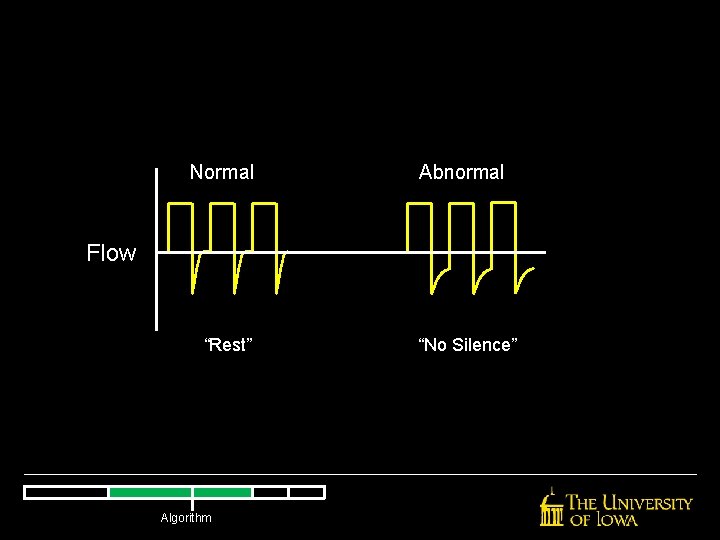
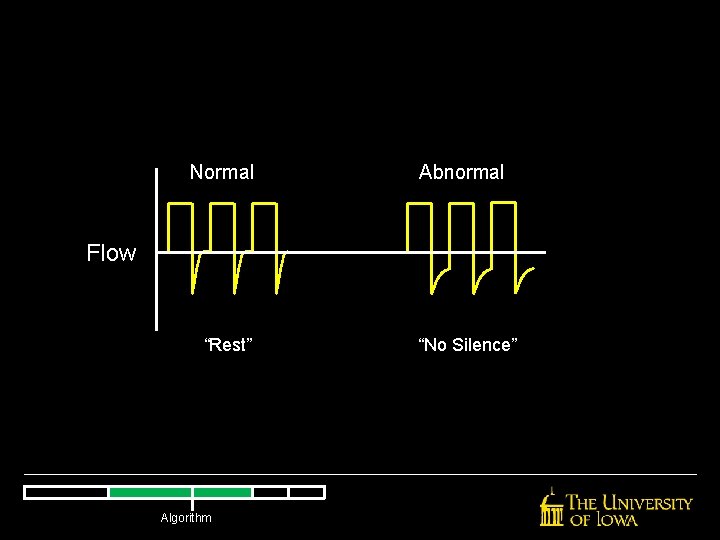
Normal Abnormal Flow “Rest” Algorithm “No Silence”
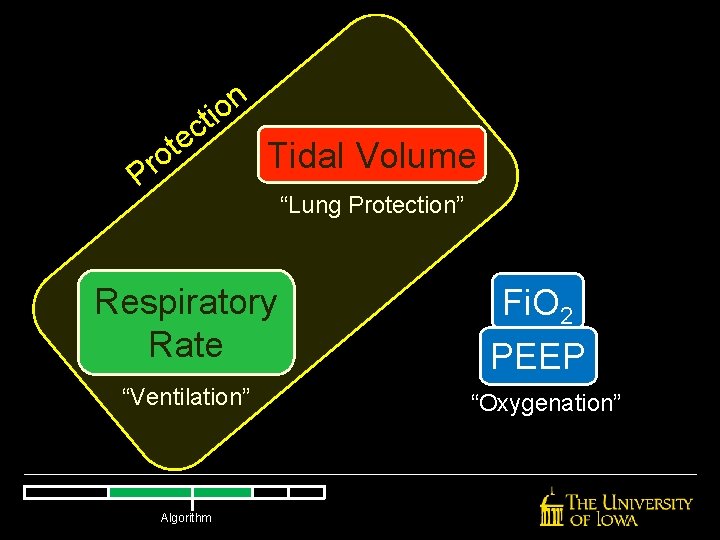
n o i t c e t o r P Tidal Volume Respiratory Rate “Ventilation” Algorithm “Lung Protection” Fi. O 2 PEEP “Oxygenation”
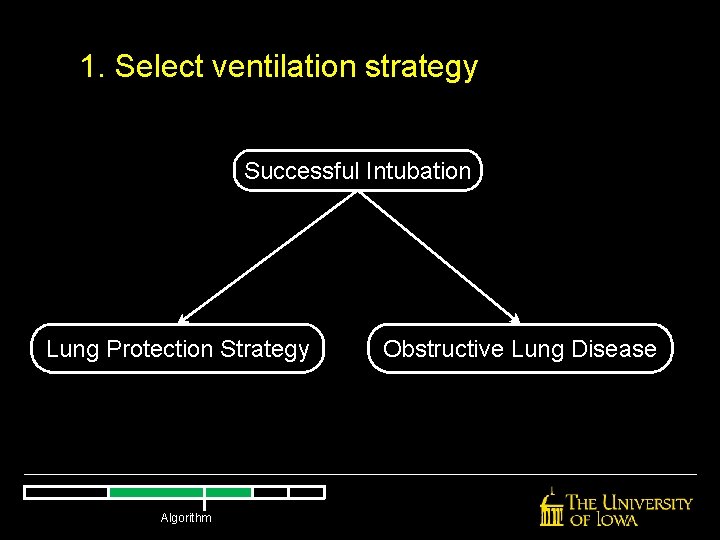
1. Select ventilation strategy Successful Intubation Lung Protection Strategy Algorithm Obstructive Lung Disease
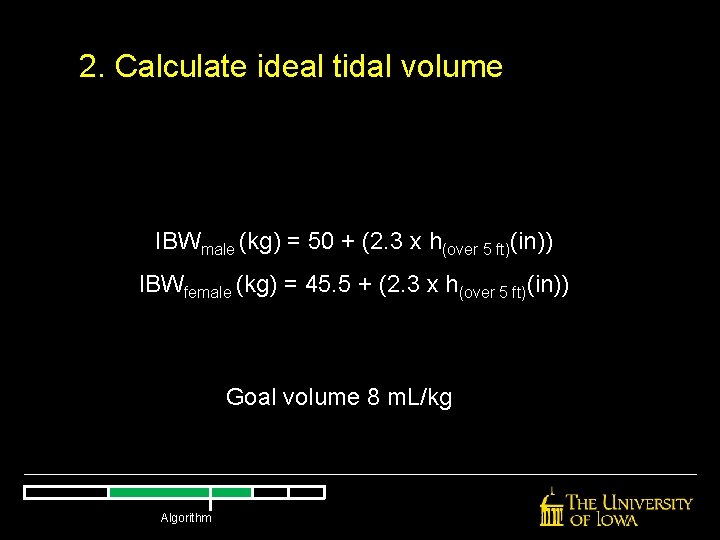
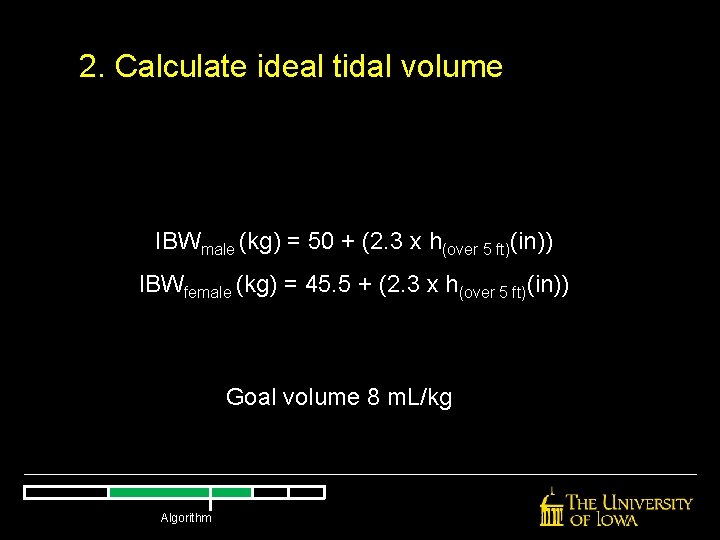
2. Calculate ideal tidal volume IBWmale (kg) = 50 + (2. 3 x h(over 5 ft)(in)) IBWfemale (kg) = 45. 5 + (2. 3 x h(over 5 ft)(in)) Goal volume 8 m. L/kg Algorithm
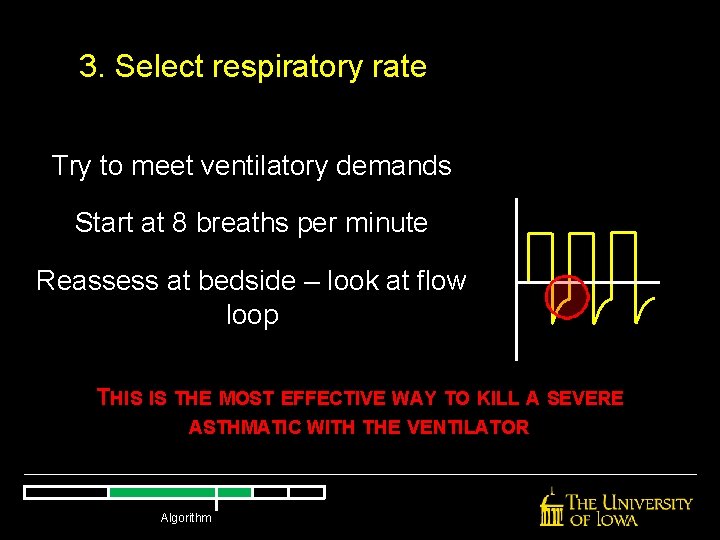
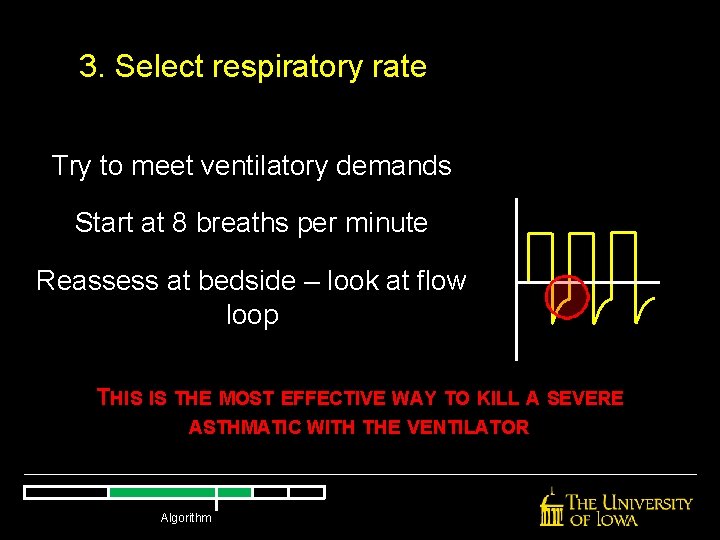
3. Select respiratory rate Try to meet ventilatory demands Start at 8 breaths per minute Reassess at bedside – look at flow loop THIS IS THE MOST EFFECTIVE WAY TO KILL A SEVERE ASTHMATIC WITH THE VENTILATOR Algorithm
4. Select oxygenation parameters Start all ventilated patients at Fi. O 2 = 100% Wean aggressively These patients probably will not require high Fi. O 2 levels Algorithm
5. Set PEEP Start low (PEEP 0 okay) Keep it low Algorithm
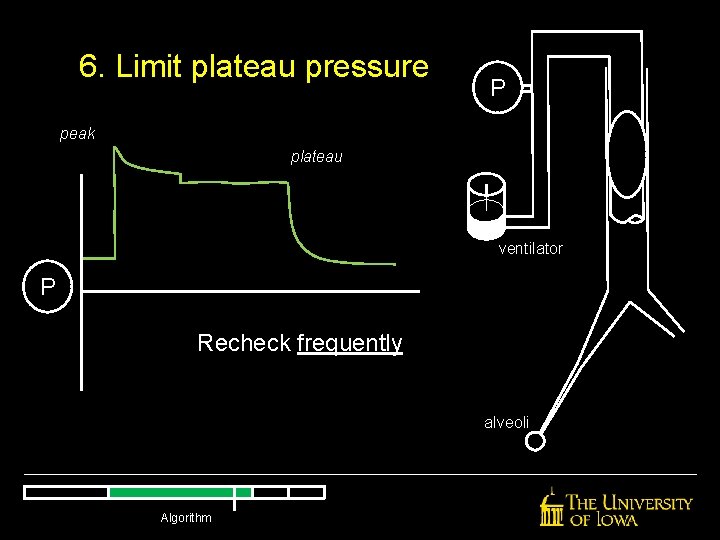
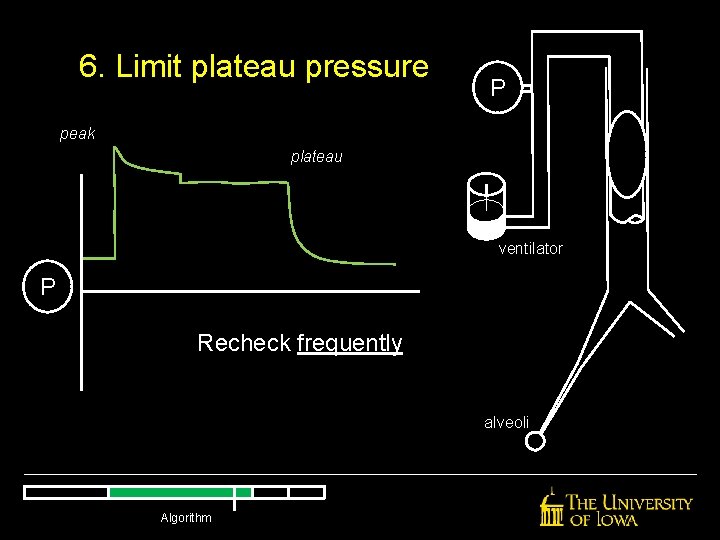
6. Limit plateau pressure P peak plateau ventilator P Recheck frequently alveoli Algorithm
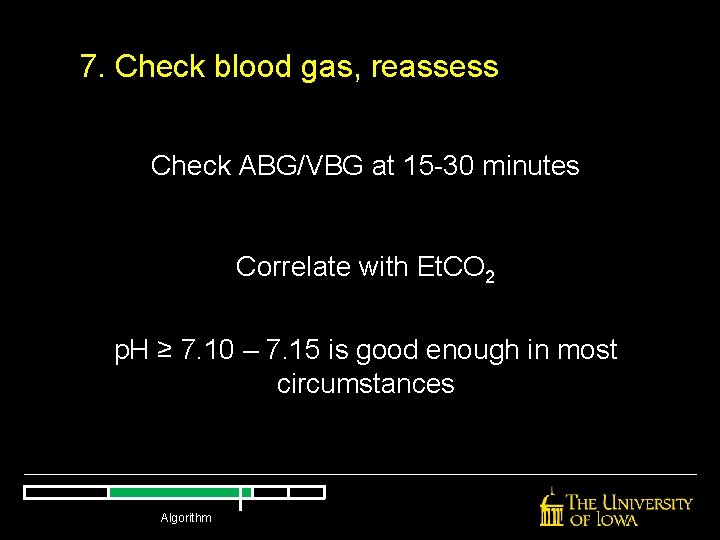
7. Check blood gas, reassess Check ABG/VBG at 15 -30 minutes Correlate with Et. CO 2 p. H ≥ 7. 10 – 7. 15 is good enough in most circumstances Algorithm
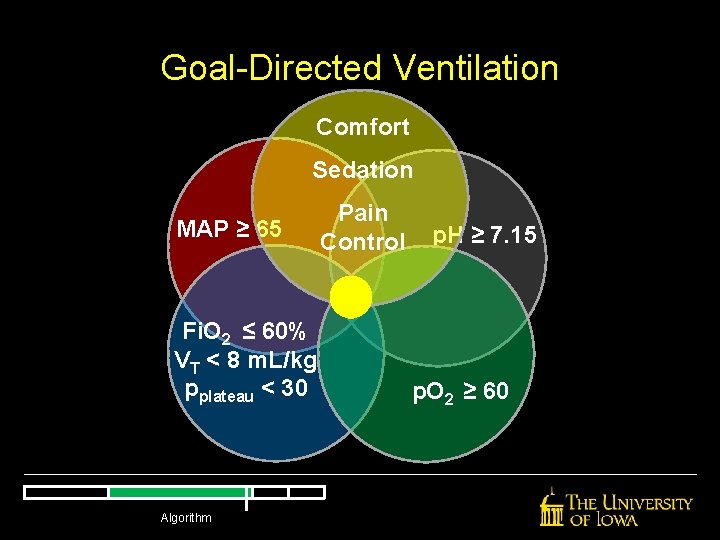
Goal-Directed Ventilation Comfort Sedation MAP ≥ 65 Fi. O 2 ≤ 60% VT < 8 m. L/kg pplateau < 30 Algorithm Pain Control p. H ≥ 7. 15 p. O 2 ≥ 60
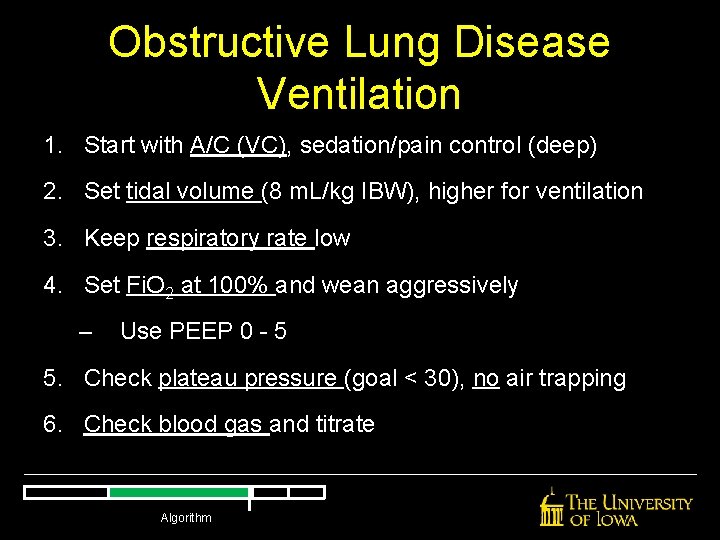
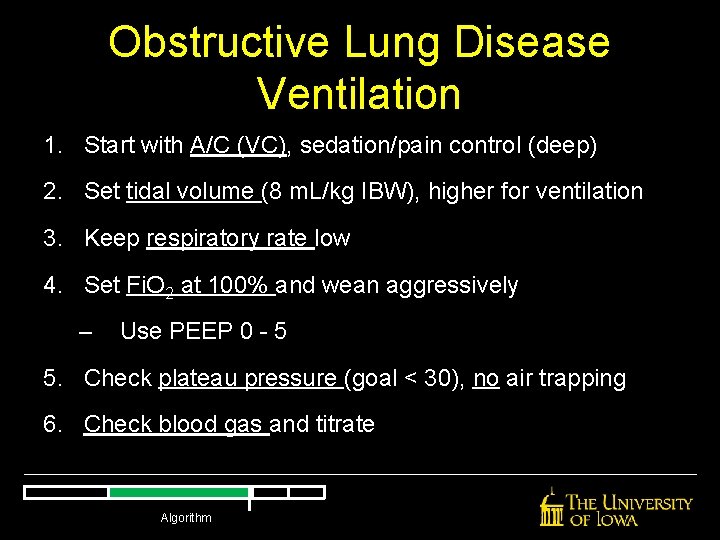
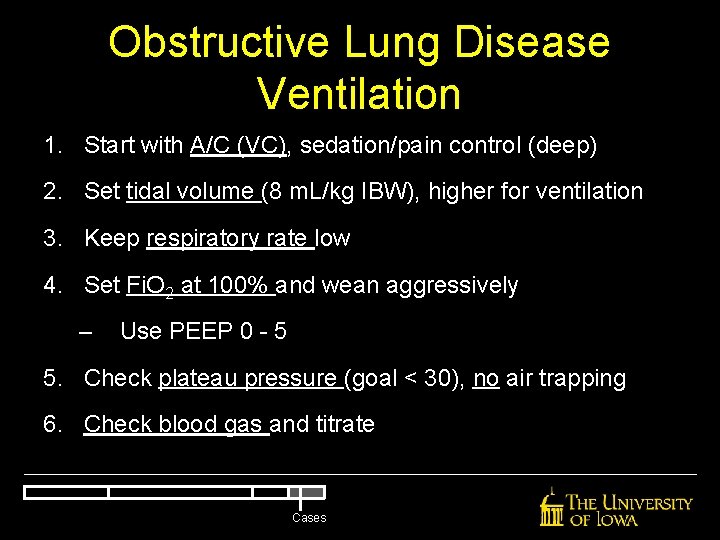
Obstructive Lung Disease Ventilation 1. Start with A/C (VC), sedation/pain control (deep) 2. Set tidal volume (8 m. L/kg IBW), higher for ventilation 3. Keep respiratory rate low 4. Set Fi. O 2 at 100% and wean aggressively – Use PEEP 0 - 5 5. Check plateau pressure (goal < 30), no air trapping 6. Check blood gas and titrate Algorithm
Troubleshooting the Ventilator Troubleshooting
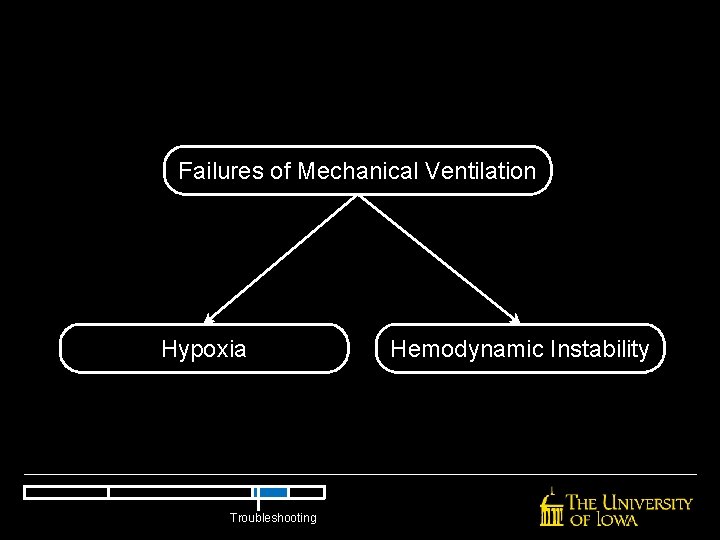
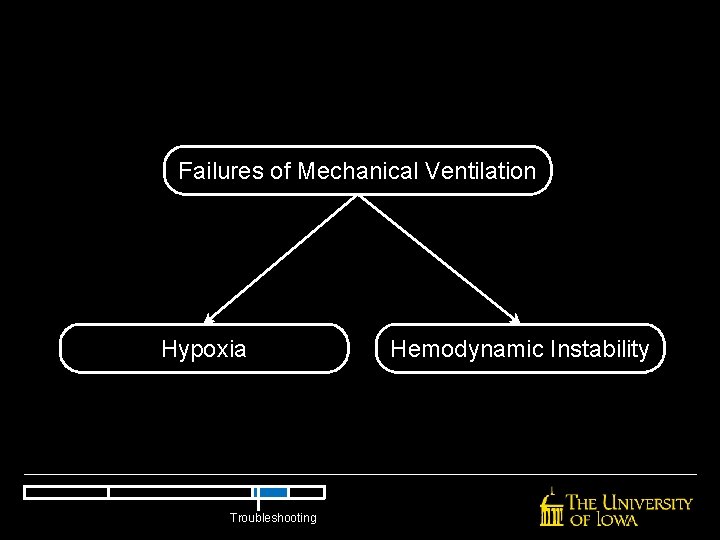
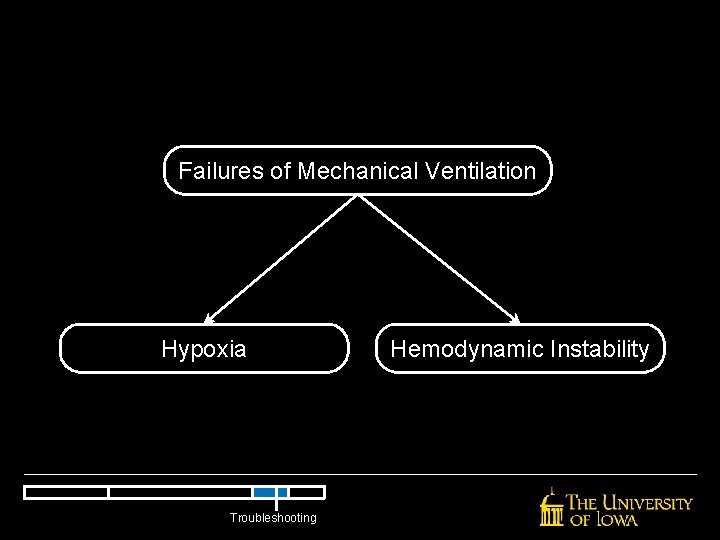
Failures of Mechanical Ventilation Hypoxia Troubleshooting Hemodynamic Instability
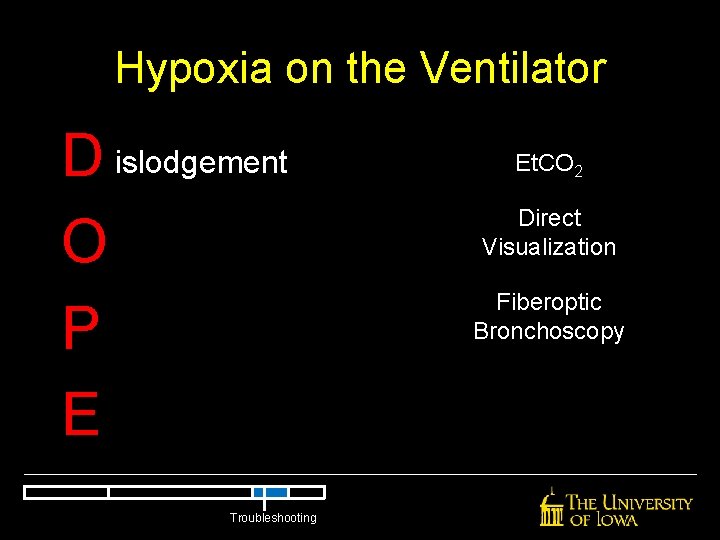
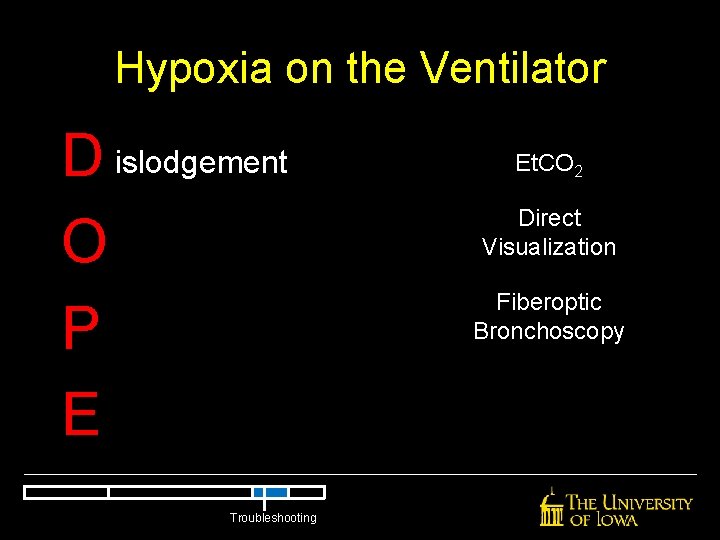
Hypoxia on the Ventilator D islodgement O P E Troubleshooting Et. CO 2 Direct Visualization Fiberoptic Bronchoscopy
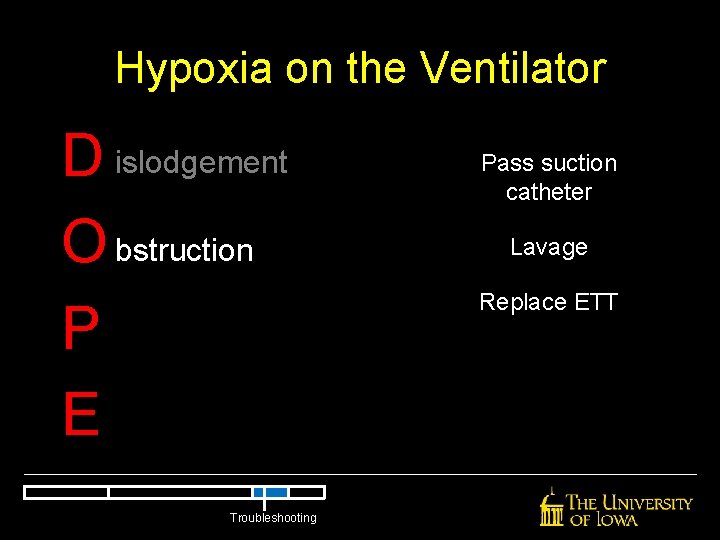
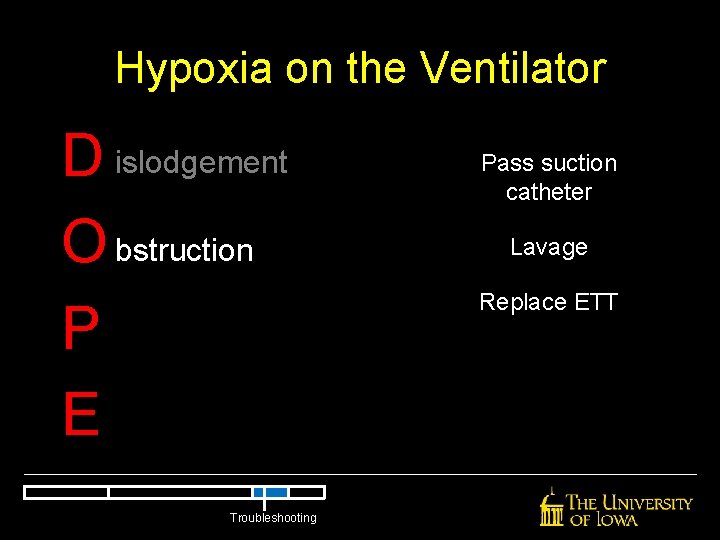
Hypoxia on the Ventilator D islodgement O bstruction P E Troubleshooting Pass suction catheter Lavage Replace ETT
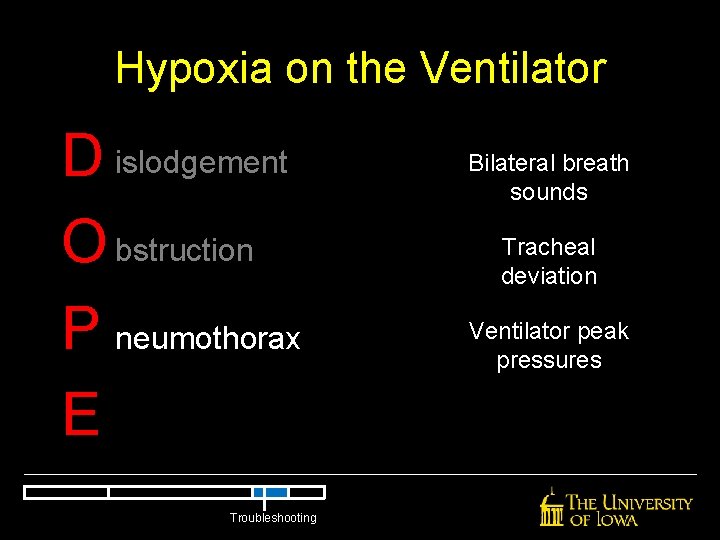
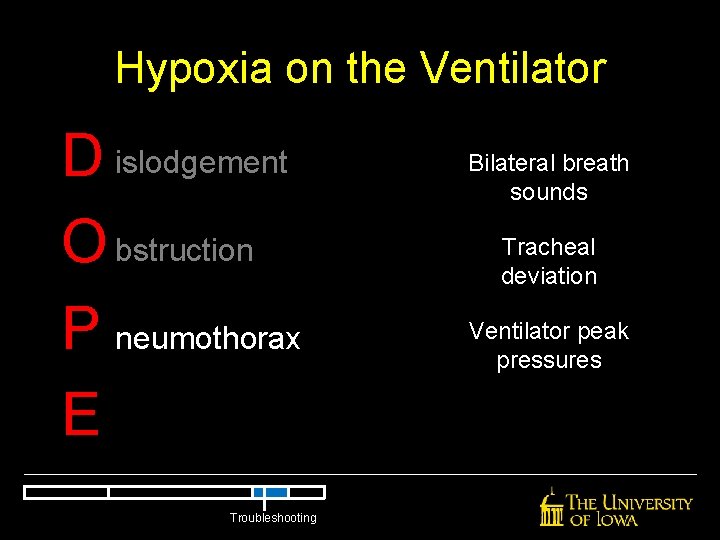
Hypoxia on the Ventilator D islodgement O bstruction P neumothorax E Troubleshooting Bilateral breath sounds Tracheal deviation Ventilator peak pressures
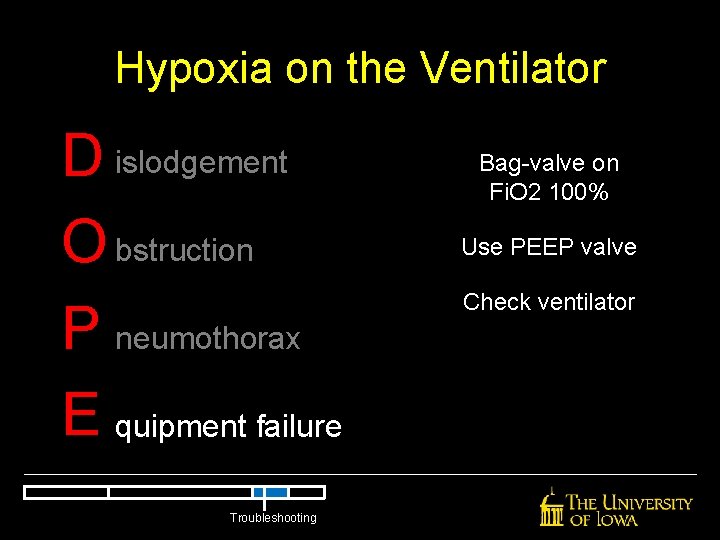
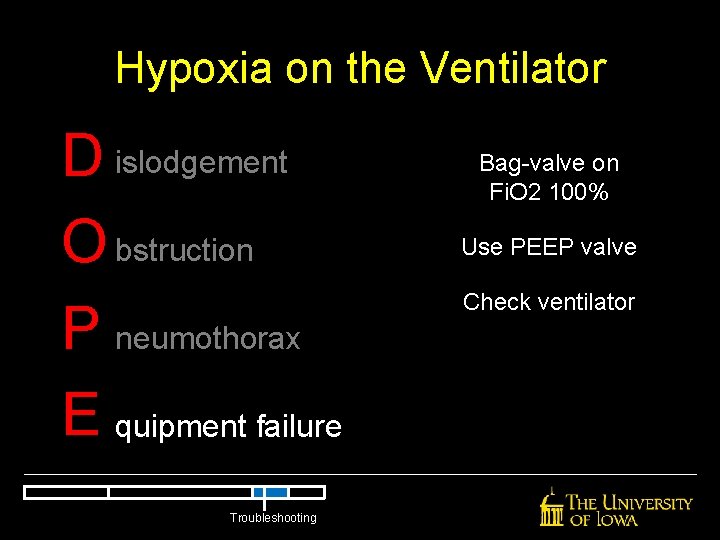
Hypoxia on the Ventilator D islodgement O bstruction P neumothorax E quipment failure Troubleshooting Bag-valve on Fi. O 2 100% Use PEEP valve Check ventilator

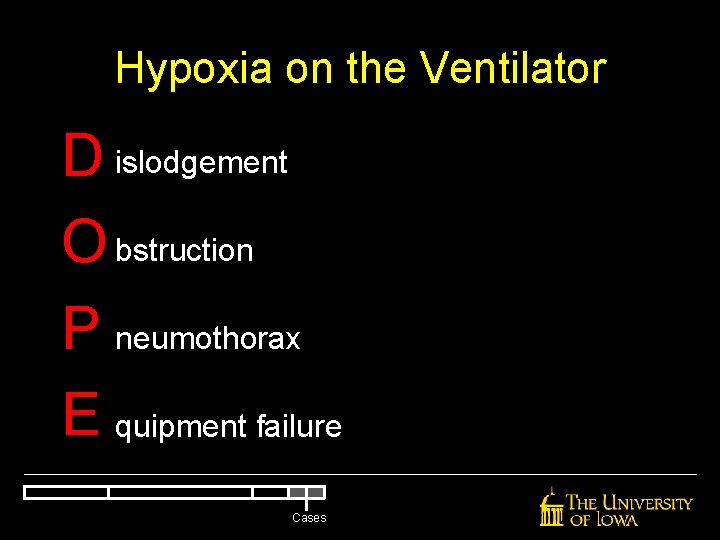
Hypoxia on the Ventilator D islodgement O bstruction P neumothorax E quipment failure Troubleshooting
Failures of Mechanical Ventilation Hypoxia Troubleshooting Hemodynamic Instability
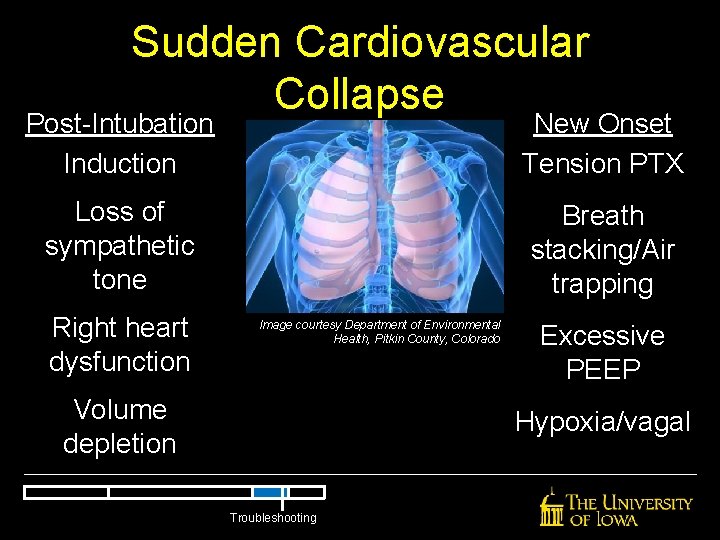
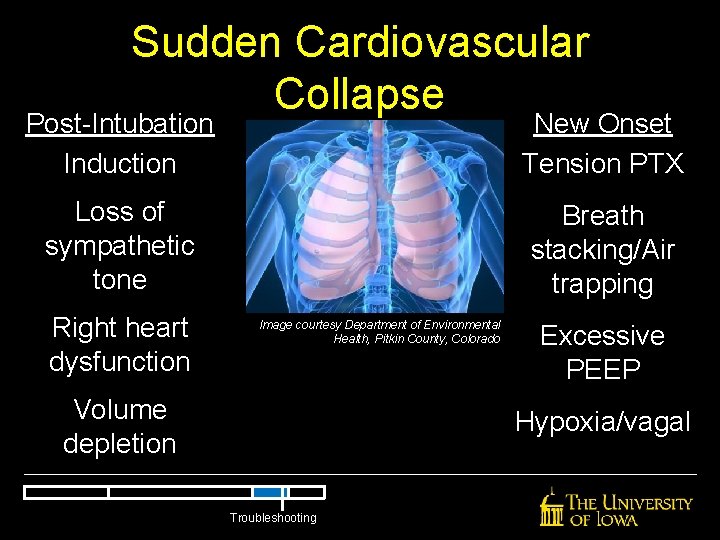
Sudden Cardiovascular Collapse Post-Intubation Induction New Onset Tension PTX Loss of sympathetic tone Breath stacking/Air trapping Right heart dysfunction Image courtesy Department of Environmental Health, Pitkin County, Colorado Volume depletion Excessive PEEP Hypoxia/vagal Troubleshooting
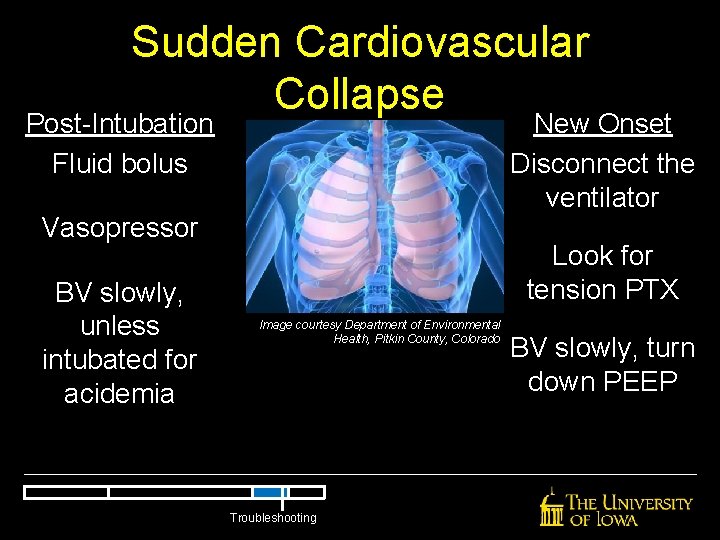
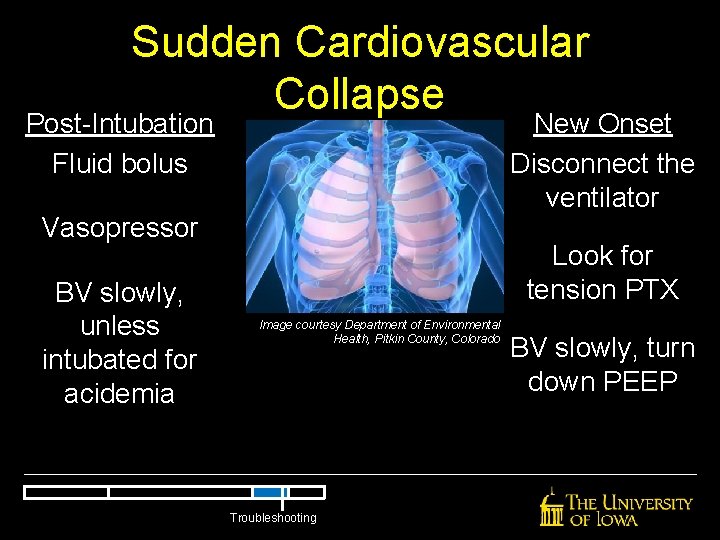
Sudden Cardiovascular Collapse New Onset Disconnect the ventilator Post-Intubation Fluid bolus Vasopressor BV slowly, unless intubated for acidemia Look for tension PTX Image courtesy Department of Environmental Health, Pitkin County, Colorado Troubleshooting BV slowly, turn down PEEP
Cases
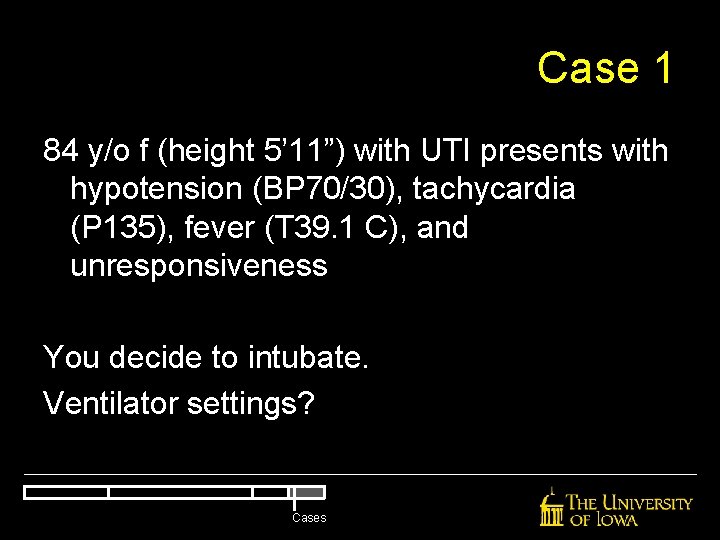
Case 1 84 y/o f (height 5’ 11”) with UTI presents with hypotension (BP 70/30), tachycardia (P 135), fever (T 39. 1 C), and unresponsiveness You decide to intubate. Ventilator settings? Cases
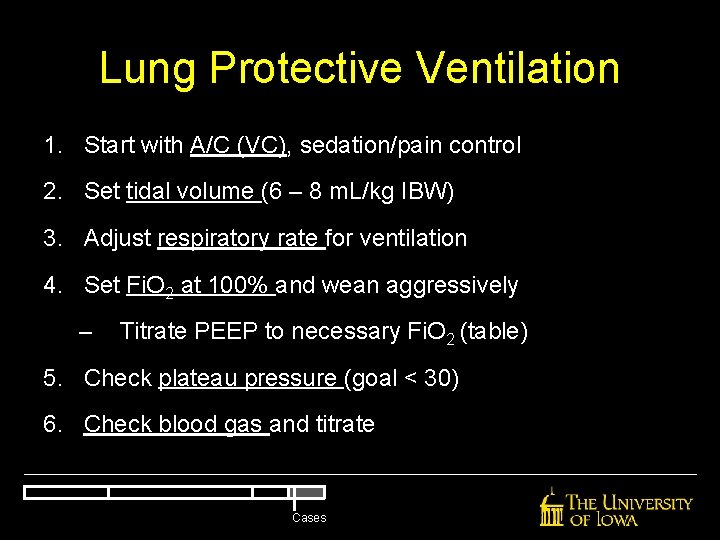
Lung Protective Ventilation 1. Start with A/C (VC), sedation/pain control 2. Set tidal volume (6 – 8 m. L/kg IBW) 3. Adjust respiratory rate for ventilation 4. Set Fi. O 2 at 100% and wean aggressively – Titrate PEEP to necessary Fi. O 2 (table) 5. Check plateau pressure (goal < 30) 6. Check blood gas and titrate Cases
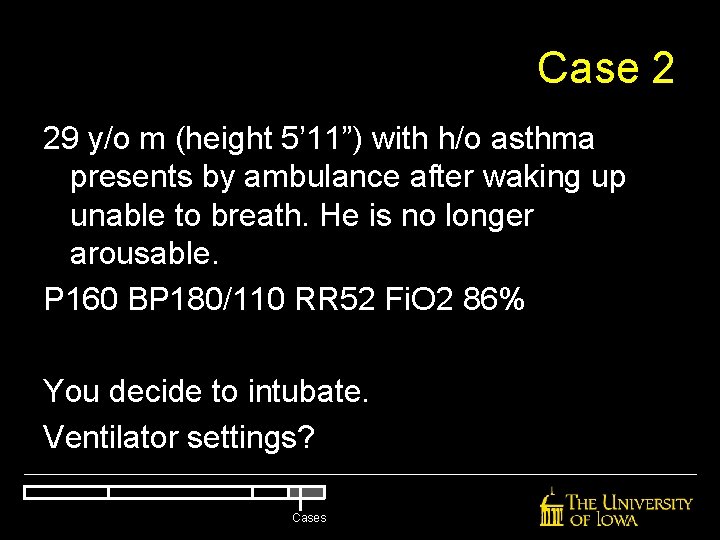
Case 2 29 y/o m (height 5’ 11”) with h/o asthma presents by ambulance after waking up unable to breath. He is no longer arousable. P 160 BP 180/110 RR 52 Fi. O 2 86% You decide to intubate. Ventilator settings? Cases
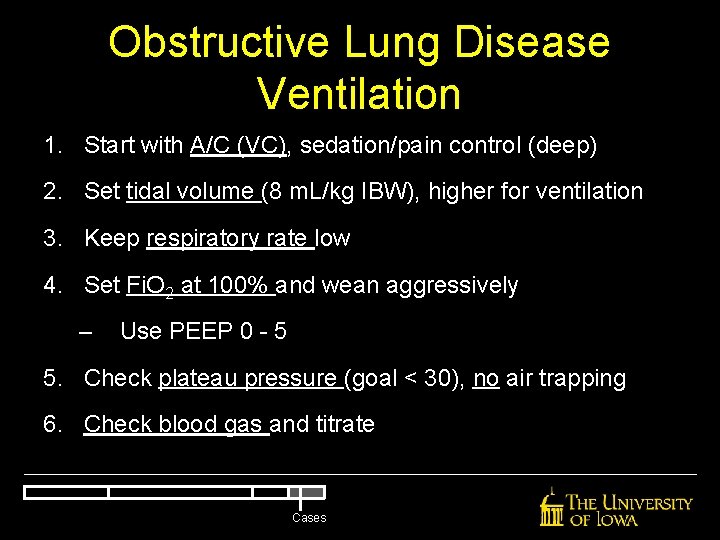
Obstructive Lung Disease Ventilation 1. Start with A/C (VC), sedation/pain control (deep) 2. Set tidal volume (8 m. L/kg IBW), higher for ventilation 3. Keep respiratory rate low 4. Set Fi. O 2 at 100% and wean aggressively – Use PEEP 0 - 5 5. Check plateau pressure (goal < 30), no air trapping 6. Check blood gas and titrate Cases
Case 3 68 y/o m with h/o COPD was involved in MVC and was intubated on arrival. While he is returning from CT 25 minutes later, he becomes hypoxic to 60% and bradycardic. What is your intervention? Cases
Hypoxia on the Ventilator D islodgement O bstruction P neumothorax E quipment failure Cases
Case 4 49 y/o f intubated for severe COPD at OSH is transferred for ICU care. As EMS arrives, they are starting chest compressions. What is your intervention? Cases
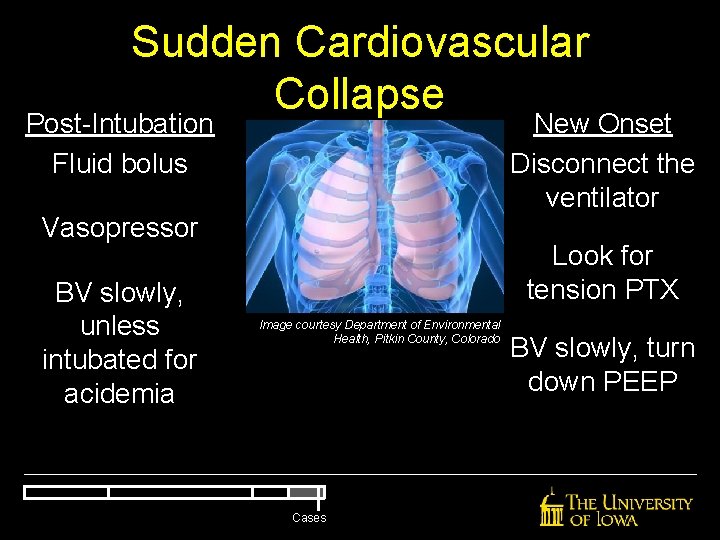
Sudden Cardiovascular Collapse New Onset Disconnect the ventilator Post-Intubation Fluid bolus Vasopressor BV slowly, unless intubated for acidemia Look for tension PTX Image courtesy Department of Environmental Health, Pitkin County, Colorado Cases BV slowly, turn down PEEP
Summary • Thou shalt not fear mechanical ventilation. Most problems in the ED can be resolved with sedation, respiratory rate, and Fi. O 2 • Thou shalt not use injurious ventilatory strategies (low tidal volume) • Thou shalt not code an asthmatic on the ventilator (low respiratory rate/air trapping) • Maintain an algorithmic approach to critically ill patients, then think about the physiology
Mechanical Ventilation: A Primer Nick Mohr, MD Assistant Professor Department of Emergency Medicine Division of Critical Care, Department of Anesthesia University of Iowa Carver College of Medicine