Mechanical Ventilation 1 Objectives Discuss indications and techniques
Mechanical Ventilation 1
Objectives Discuss indications and techniques for noninvasive positive pressure ventilation (NPPV) Describe types of breaths and modes of mechanical ventilation Outline settings and monitoring for initiation of mechanical ventilation Copyright 2008 Society of Critical Care Medicine 2
Case Study 65 -year-old with an exacerbation of COPD Using accessory muscles and wheezing after 2 bronchodilator treatments HR 110 beats/min, BP 160/110 mm Hg, RR 30 breaths/min, T 99 F(37. 2 C) ABG on 3 L/min O 2: p. H 7. 24, PCO 2 60 mm Hg (8 k. Pa), PO 2 65 mm Hg (8. 7 k. Pa) What type of respiratory support should be initiated? Copyright 2008 Society of Critical Care Medicine 3
Candidates for NPPV Respiratory condition expected to improve in 48 -72 hours Alert, cooperative Hemodynamically stable Able to control airway secretions Able to coordinate with ventilator No contraindications Copyright 2008 Society of Critical Care Medicine 4
Case Study What are advantages of using noninvasive positive pressure ventilation in this patient? Avoids complications of intubation Preserves airway reflexes Improved patient comfort Less need for sedation Shorter hospital/ICU stay Improved survival Copyright 2008 Society of Critical Care Medicine 5
Case Study ABG on 3 L/min O 2: p. H 7. 24, Pa. CO 2 60 mm Hg (8 k. Pa), Pa. O 2 65 mm Hg (8. 7 k. Pa) HR 110 beats/min, BP 160/110 mm Hg, RR 30 breaths/min What are the goals for respiratory support? What settings should be selected for NPPV? How should the patient be monitored? Copyright 2008 Society of Critical Care Medicine 6
Case Study After 1 hr of NPPV, the patient has not improved Arterial blood gas on 40% O 2: p. H 7. 20, Pa. CO 2 65 mm Hg (8. 7 k. Pa), Pa. O 2 58 mm Hg (7. 8 k. Pa) HR 115 beats/min, BP 142/98 mm Hg, RR 32 breaths/min What is the next step? Copyright 2008 Society of Critical Care Medicine 7
Case Study Orotracheal intubation is performed What ventilator mode should be selected? What tidal volume is optimum? What rate of ventilation should be set? Copyright 2008 Society of Critical Care Medicine 8
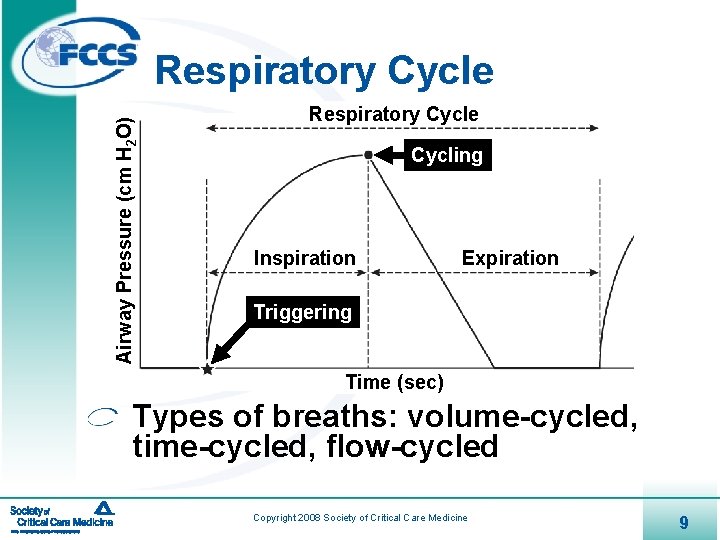
Airway Pressure (cm H 2 O) Respiratory Cycle Cycling Inspiration Expiration Triggering Time (sec) Types of breaths: volume-cycled, time-cycled, flow-cycled Copyright 2008 Society of Critical Care Medicine 9
Modes of Mechanical Ventilation Interface of breath types with patient Assist-control (AC) Pressure support (PSV) Synchronized intermittent mandatory (SIMV) Continuous positive pressure airway pressure (CPAP)—not a mode of ventilation Copyright 2008 Society of Critical Care Medicine 10
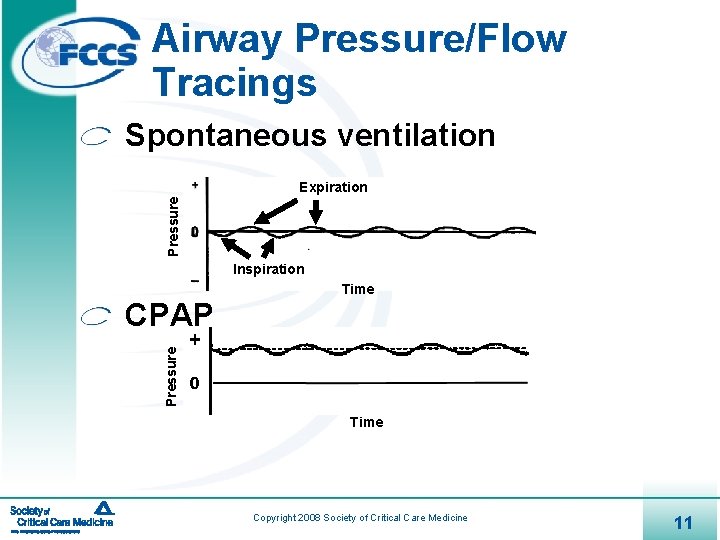
Airway Pressure/Flow Tracings Spontaneous ventilation Pressure Expiration Inspiration Time Pressure CPAP Time Copyright 2008 Society of Critical Care Medicine 11

Modes of Mechanical Ventilation Assist-control ventilation - Volume or time-cycled breaths Inspiration Expiration Volume assist-control Pressure support ventilation - Flow-cycled breaths Copyright 2008 Society of Critical Care Medicine 12
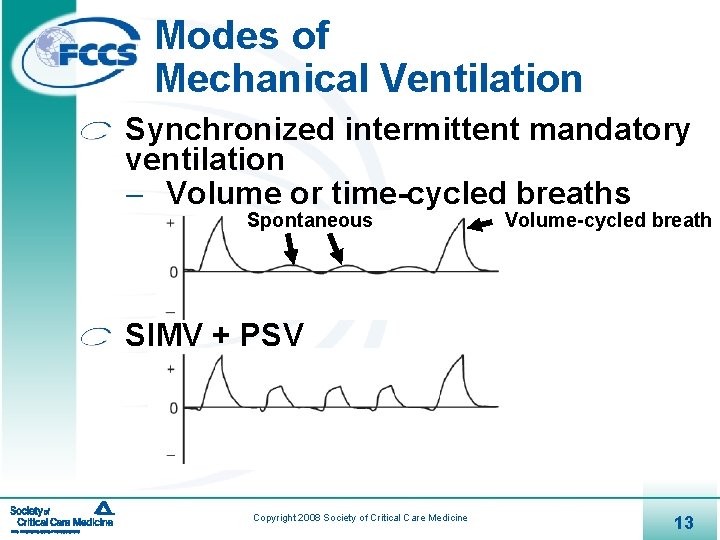
Modes of Mechanical Ventilation Synchronized intermittent mandatory ventilation - Volume or time-cycled breaths Spontaneous Volume-cycled breath SIMV + PSV Copyright 2008 Society of Critical Care Medicine 13
Case Study Patient with COPD exacerbation who failed NPPV What ventilator mode should be selected? What tidal volume is optimum? What rate of ventilation should be set? What FIO 2 should be delivered? Copyright 2008 Society of Critical Care Medicine 14
Initiation of Mechanical Ventilation Familiar ventilation mode Initial FIO 2 = 1. 0; decrease to maintain Sp. O 2 >92% to 94% Initial tidal volume = 8 -10 m. L/kg Rate and minute ventilation appropriate for clinical needs PEEP to support oxygenation Call critical care consultant for help Copyright 2008 Society of Critical Care Medicine 15 ®
Case Study What monitoring and assessment is needed after initiation of mechanical ventilation? Chest radiograph Vital signs Sp. O 2 Patient-ventilator synchrony Arterial blood gas Inspiratory pressures Inspiratory: expiratory ratio Auto-PEEP Ventilator alarms Copyright 2008 Society of Critical Care Medicine 16
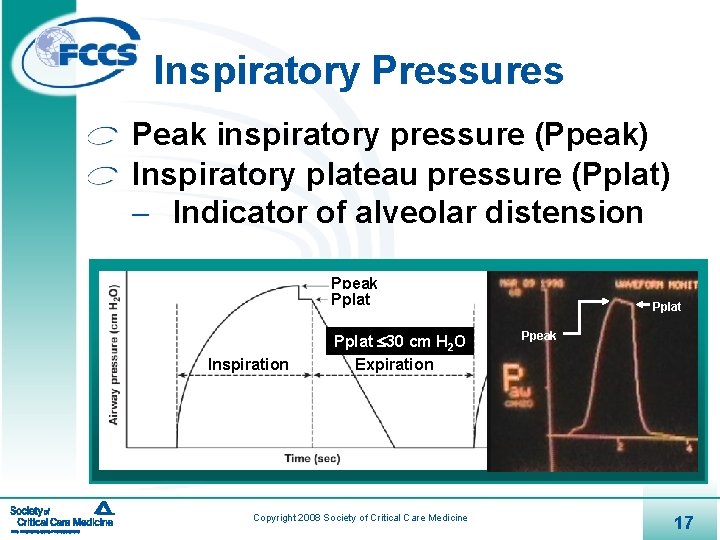
Inspiratory Pressures Peak inspiratory pressure (Ppeak) Inspiratory plateau pressure (Pplat) - Indicator of alveolar distension Ppeak Pplat Inspiration Pplat 30 cm H 2 O Expiration Copyright 2008 Society of Critical Care Medicine Pplat Ppeak 17
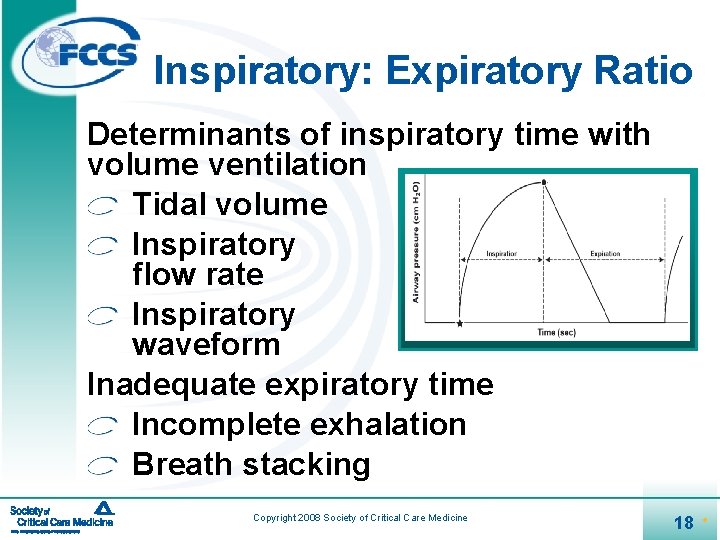
Inspiratory: Expiratory Ratio Determinants of inspiratory time with volume ventilation Tidal volume Inspiratory flow rate Inspiratory waveform Inadequate expiratory time Incomplete exhalation Breath stacking Copyright 2008 Society of Critical Care Medicine 18 ®
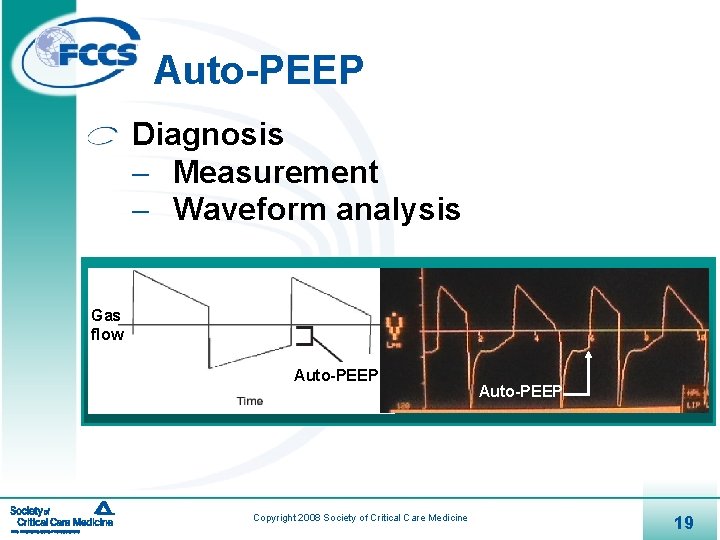
Auto-PEEP Diagnosis - Measurement - Waveform analysis Gas flow Auto-PEEP Copyright 2008 Society of Critical Care Medicine Auto-PEEP 19
Auto-PEEP Consequences - Inspiratory pressures - Hypotension - Worsened oxygenation Interventions to decrease auto-PEEP - Respiratory rate - Tidal volume - Gas flow rate Copyright 2008 Society of Critical Care Medicine 20 ®
Questions Copyright 2008 Society of Critical Care Medicine 21
Key Points Goals of NPPV and mechanical ventilation are support of oxygenation and ventilation and reduction in work of breathing NPPV is best used in the alert, cooperative patient whose condition will improve in 48 -72 hours Consider the advantages/disadvantages of different modes when selecting ventilatory support Use guidelines when initiating mechanical ventilation and adjust based on monitoring Copyright 2008 Society of Critical Care Medicine 22
- Slides: 22