Measuring CVP Central venous pressure CVP Is the
- Slides: 14
Measuring CVP
Central venous pressure (CVP): Is the pressure of blood within the right atrium of the heart, which measures the ability of the right side of the heart to deal with the systemic fluid load. CVP changes reflect the patient’s overall fluid volume status.
Purpose of measuring CVP: 1. To assess patient intravascular volume status and right ventricular preload 2. To evaluate right sided heart hemodynamics. 3. To evaluate patient response to therapy
N. B: § A low CVP is an indicator of hypovolemia generally calling for an increase in IV fluids. § A high CVP can be caused by Hypervolemia or by poor cardiac function. This is usually treated by diuresing the patient. § CVP value can be obtained by using a fluid manometer system or a hemodynamic monitoring system.
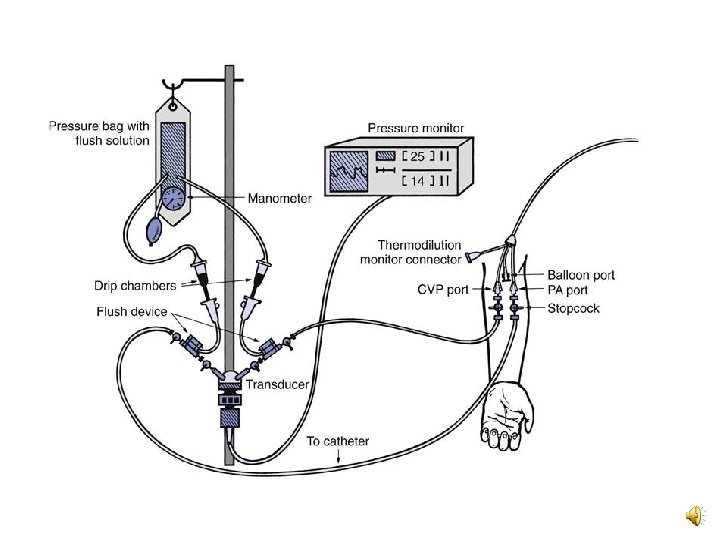
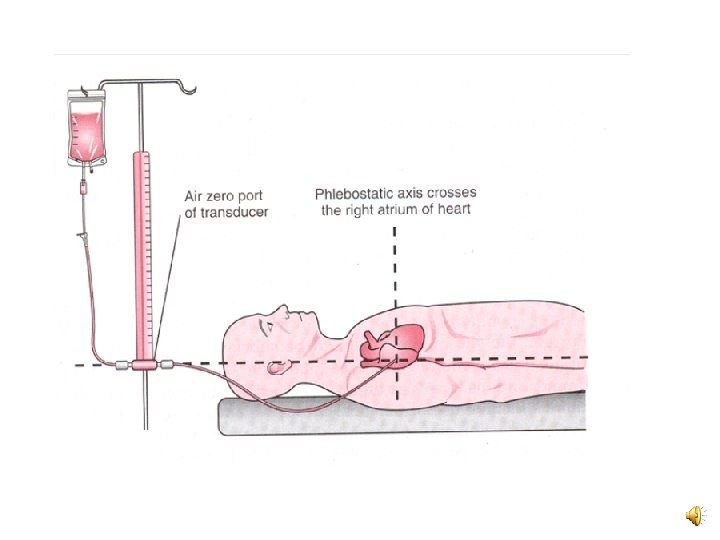
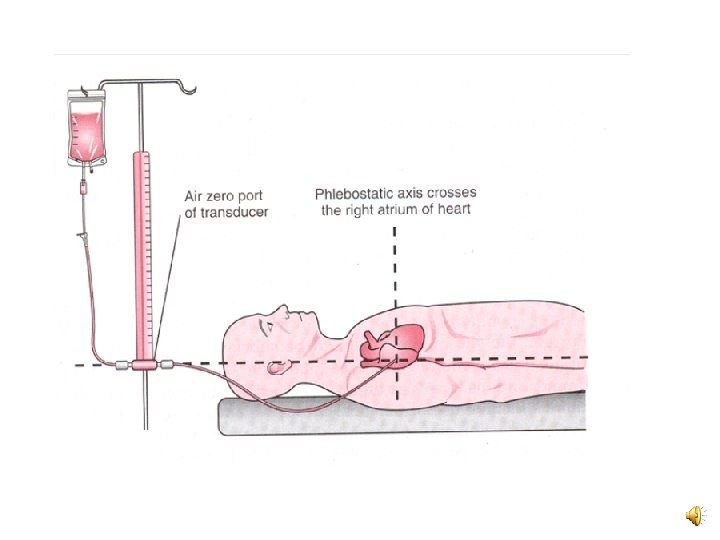
CVP can be measured using: 1. Hemodynamic monitoring system. • CVP is commonly measured using a pressure transducer attached to a bedside monitor. The transducer must be leveled at the phlebostatic axis as well. • Advantages: - it reduces the risk of air embolus while measuring the CVP. • Normal CVP value =2 to 6 mm. Hg =5 to 10 cm H 2 o
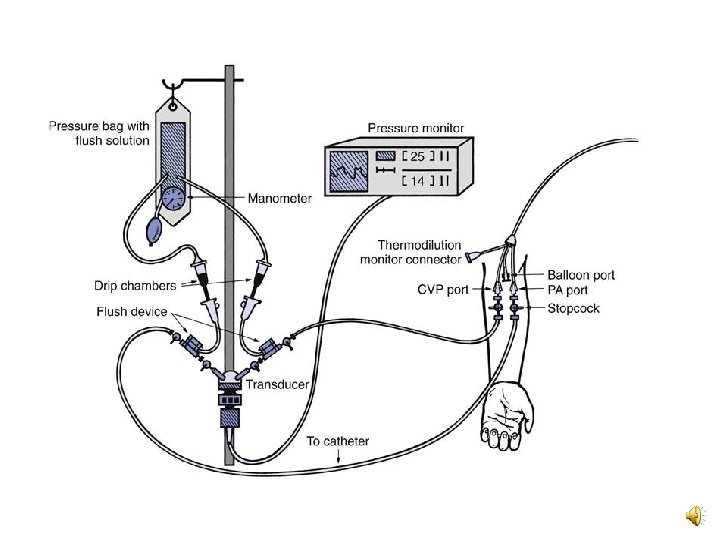
2. Water manometer system • CVP can be measured using a fluid manometer attached the intravenous fluid line. • Disadvantages: - It exposes the patient to complications of infection and air embolism.
Causes of increased CVP • Elevated intravascular volume • Depressed right-sided cardiac function (RV infarct, RV failure)
• Cardiac temponade • Constrictive pericarditis • Pulmonary hypertension • Positive pressure ventilation
Causes of decreased CVP: • Blood loss • Fluid loss • Venous dilation. (drug induced)
Equipment • IV Solution (normal saline) • IV infusion set • Water manometer • Non sterile gloves • Three way stopcock, if not included in manometer set
Procedure
Patient care and Monitoring: