Maternity Update Agenda Antenatal VTE assessment Pregnancy for
- Slides: 21
Maternity Update
Agenda • Antenatal VTE assessment • Pregnancy for women with complex needs • Maternity service update
Antenatal VTE assessment Dr Lauren Ward – CCG clinical lead for preconception and antenatal care
Background – venous thromboembolism • VTE - DVT and PE which are confirmed by objective investigations including Doppler ultrasound and CTPA. Past VTE can be assumed if the woman gives a good history and received prolonged (6 -12 weeks) therapeutic anticoagulation • PE remains a leading cause of maternal death in the UK • Pregnancy is a risk factor for VTE and is associated with a 4 -6 -fold increase in risk compared to the non-pregnant state. The postpartum risk of VTE is increased further. • This guideline aims to summarise the RCOG guidance on thromboprophylaxis in pregnancy and the puerperium with relation to GP antenatal appointments.
Risk Assessment • All women will have a VTE risk assessment with the midwives at booking but given that the first trimester is a high risk time for women at high risk of VTE, a VTE assessment should be done by the GP at first presenation • This is to highlight those women who need antenatal LMWH, particularly in the first trimester. • For women at high risk of VTE (e. g. previous VTE and/or thrombophilia, multiple risk factors) pre-pregnancy counselling should be offered to formulate a maternity care plan in conjunction with the Haematology team
Risk Assessment • Based on the RCOG guidelines • If total score ≥ 4 antenatally, consider thromboprophylaxis from the first trimester. • If total score 3 antenatally, consider thromboprophylaxis from 28 weeks. • For patients with an identified bleeding risk, the balance of risks of bleeding and thrombosis should be discussed in consultation with a haematologist with expertise in thrombosis and bleeding in pregnancy
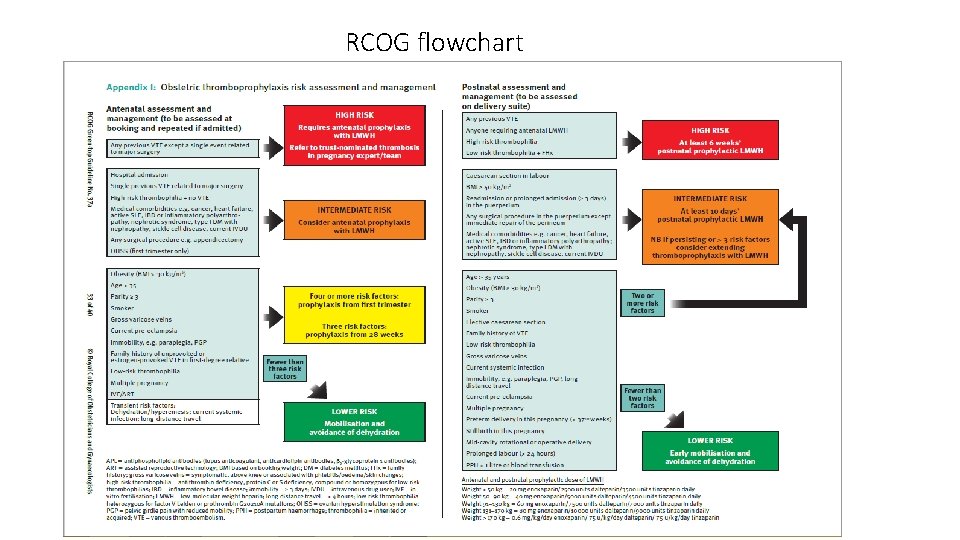
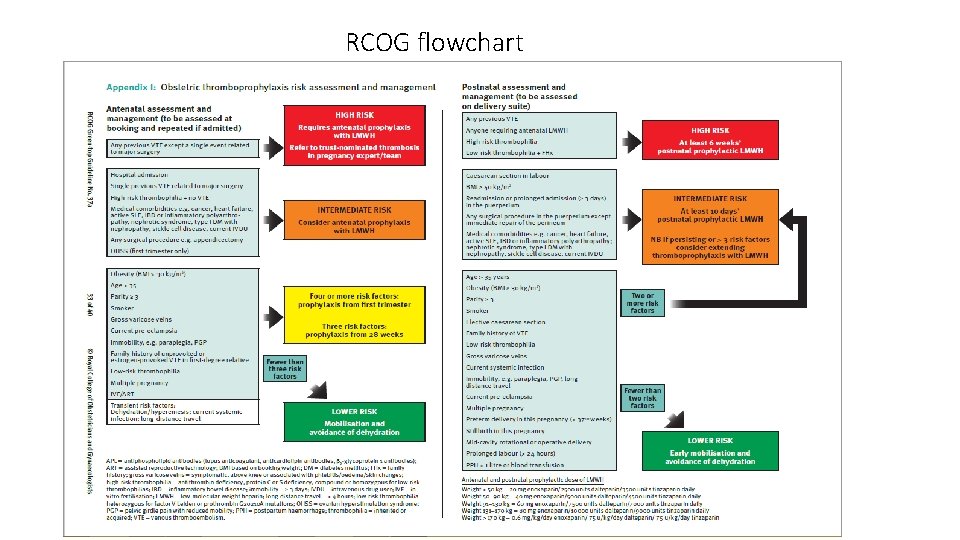
RCOG flowchart
Agents for thromboprophylaxis • LMWH has at least as good a safety profile as unfractionated heparin with the advantage of once daily dosing for prophylaxis so it is the most convenient and suitable agent for the majority of women. • LMWH does not cross the placenta in significant quantities and is safe in breastfeeding. • No monitoring is required • The recommended LMWH used at Homerton Hospital NHS Trust is Enoxaparin (Clexane). • Shared care guidelines are now available on the CCG website
Prescribing clexane • If a woman is deemed high risk at first presentation and needs clexane starting in the first trimester this should be actioned urgently by the GP. • The GP should initiate clexane that day after discussion with the oncall haematologist and obstetrician. • She should also be urgently referred to the obstetrician-led antenatal clinic by emailing the obstetric query line obstetricquery@homerton. nhs. uk. • If the GP does not feel happy to initiate clexane, they should email the obstetric query line to arrange an urgent antenatal clinic appointment within 1 week
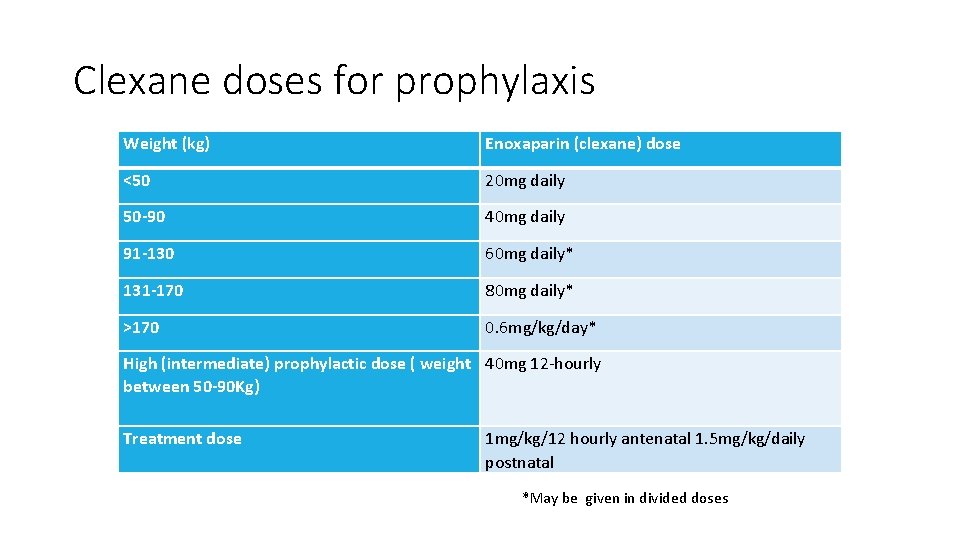
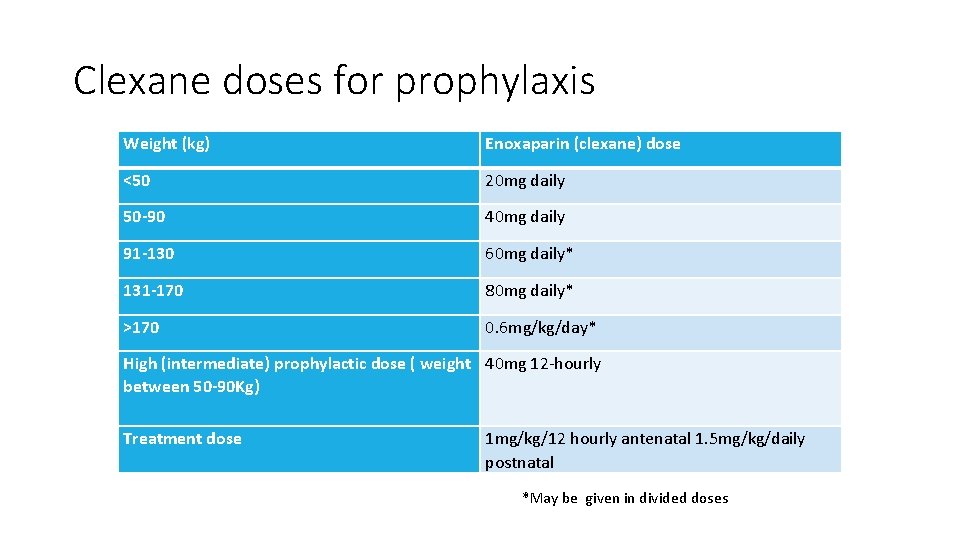
Clexane doses for prophylaxis Weight (kg) Enoxaparin (clexane) dose <50 20 mg daily 50 -90 40 mg daily 91 -130 60 mg daily* 131 -170 80 mg daily* >170 0. 6 mg/kg/day* High (intermediate) prophylactic dose ( weight 40 mg 12 -hourly between 50 -90 Kg) Treatment dose 1 mg/kg/12 hourly antenatal 1. 5 mg/kg/daily postnatal *May be given in divided doses
Thromboprophylaxis • Warfarin has significant teratogenic potential, crosses the placenta and is therefore reserved for very limited circumstances in the antenatal period – principally for women with mechanical prosthetic heart valves. • Warfarin is however a useful alternative to LMWH for prophylaxis in the postpartum period and is safe to use when breastfeeding. • Aspirin is not recommended for thromboprophylaxis in obstetric patients.
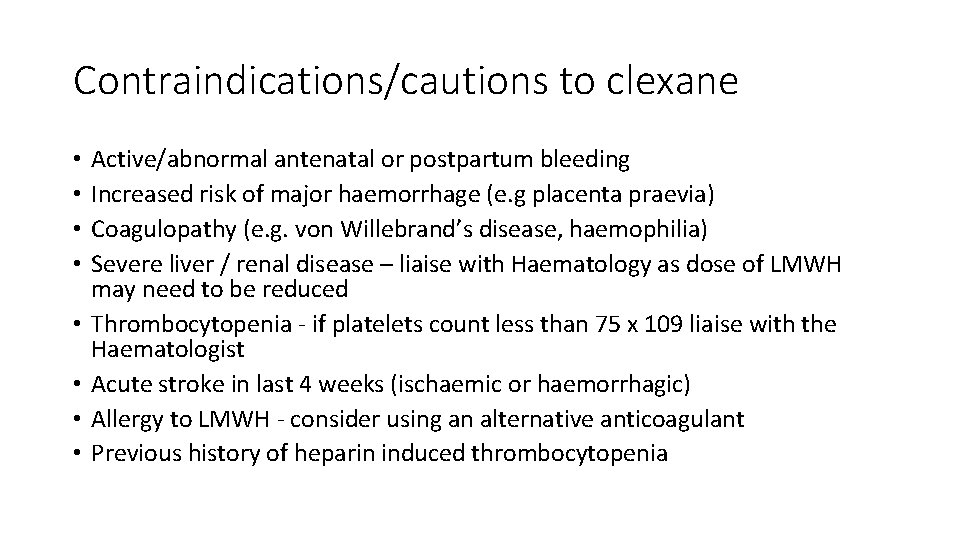
Contraindications/cautions to clexane • • Active/abnormal antenatal or postpartum bleeding Increased risk of major haemorrhage (e. g placenta praevia) Coagulopathy (e. g. von Willebrand’s disease, haemophilia) Severe liver / renal disease – liaise with Haematology as dose of LMWH may need to be reduced Thrombocytopenia - if platelets count less than 75 x 109 liaise with the Haematologist Acute stroke in last 4 weeks (ischaemic or haemorrhagic) Allergy to LMWH - consider using an alternative anticoagulant Previous history of heparin induced thrombocytopenia
Monitoring requirements • None for clexane • Thrombocytopenia is a rare complication and monitoring platelet counts in not routinely recommended when LMWH is used.
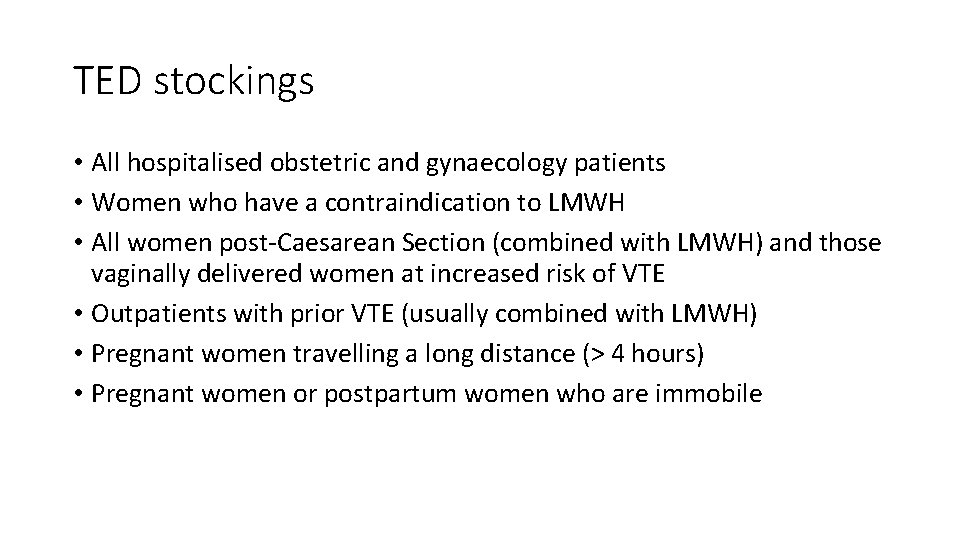
TED stockings • All hospitalised obstetric and gynaecology patients • Women who have a contraindication to LMWH • All women post-Caesarean Section (combined with LMWH) and those vaginally delivered women at increased risk of VTE • Outpatients with prior VTE (usually combined with LMWH) • Pregnant women travelling a long distance (> 4 hours) • Pregnant women or postpartum women who are immobile
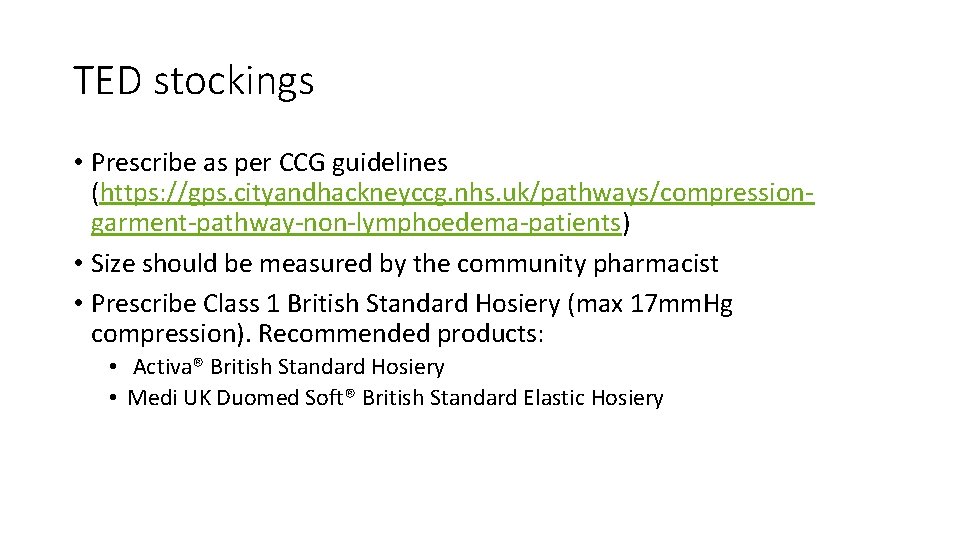
TED stockings • Prescribe as per CCG guidelines (https: //gps. cityandhackneyccg. nhs. uk/pathways/compressiongarment-pathway-non-lymphoedema-patients) • Size should be measured by the community pharmacist • Prescribe Class 1 British Standard Hosiery (max 17 mm. Hg compression). Recommended products: • Activa® British Standard Hosiery • Medi UK Duomed Soft® British Standard Elastic Hosiery
Women that are high risk for VTE • The first presentation antenatal appointment template on EMIS has been updated to include a VTE risk assessment. • If a woman scores ≥ 4 and requires LMWH in the first trimester, this should be started as soon as possible. This should be prescribed by the GP after discussion with the on call haematologist and obstetrician and the woman be referred urgently to the antenatal Obstetrics Medical Clinic (OMC) • In theses cases, clexane should start as early in pregnancy as possible and continue post delivery unless the risk factor has been removed (e. g. resolution of OHSS). This is because most antenatal VTE occurs in the first trimester. • Women on antenatal thromboprophylaxis should be advised about its implications for regional anaesthesia and analgesia
• If a woman is on warfarin at first presentation, the GP should indicate that the referral is URGENT and contact the on-call haematology consultant through Homerton switchboard (0208 501 5555) who is available 24/7. They should discuss and agree a plan for her anticoagulation that day. • Any queries can be directed to the obstetric query email (obstetricquery@homerton. nhs. uk).
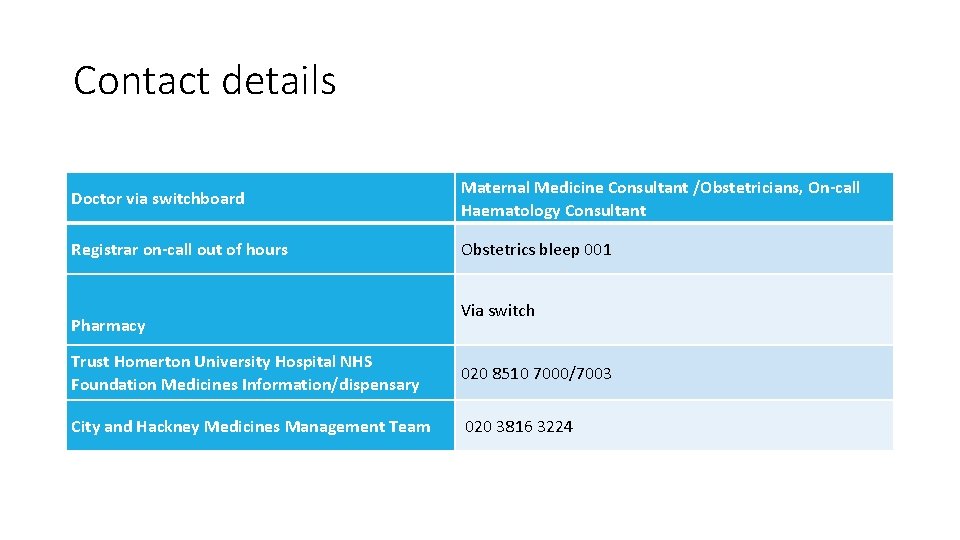
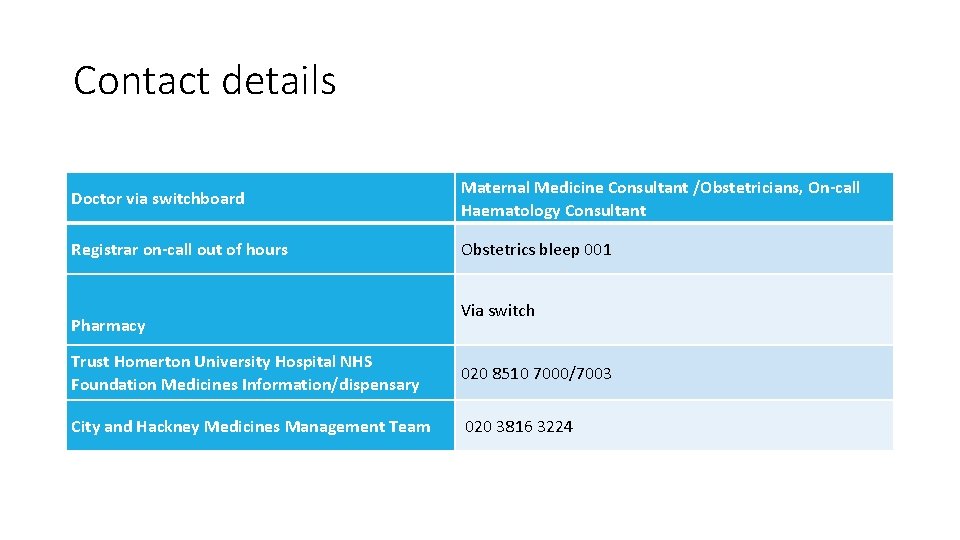
Contact details Doctor via switchboard Maternal Medicine Consultant /Obstetricians, On-call Haematology Consultant Registrar on-call out of hours Obstetrics bleep 001 Pharmacy Via switch Trust Homerton University Hospital NHS Foundation Medicines Information/dispensary 020 8510 7000/7003 City and Hackney Medicines Management Team 020 3816 3224
Referral updates
Preconception clinic • Now available on e-RS for • • • Diabetes Epilepsy Hypertension Thyroid disease Other – complex obstetric Hx, gastroenterology, haematology, cardiology etc • Referral forms on CCG website/EMIS • Also patient leaflets are available on the CCG website
Referral forms • Antenatal referrals are now done via e. RS with referral form available on EMIS • Healthy start referral form also now available on EMIS and is autopopulated