Mastering the Basics of RISK ADJUSTMENT Made Clear

Mastering the Basics of RISK ADJUSTMENT Made Clear & Simple 1

Risk Adjustment requires a NEW way of Thinking! Historically you are accustomed to submitting CPT & ICD diagnosis codes on claims to validate reimbursement for services already rendered. In Risk Adjustment payment models, your submitted I-10 codes that risk adjust will be used by a payer to calculate each of your patients’ Risk Adjustment Score. These scores will determine the projected ‘spending budget’ and prospective payments during the coming calendar year. Profitability or losses will depend on the net difference between Risk Adjusted payments and actual utilization costs for care rendered. 2
In other words, CPT/HCPCS codes submitted on a claim to a payer have been a financial transactional event, e. g. , invoice for payment(s) based on services/procedures already rendered. Going forward, Value-Based payments will be driven by I-10 Risk Adjustment coding combined with CPT/HCPCS HEDIS/PQRS compliance coding. 3
Physicians just want to take care of patients like we were trained to do! We aren’t accountants and don’t like hassles! But things have changed! The most $uccessful physicians will Robustly Embrace and Master Risk Adjustment! Let’s see why! 4
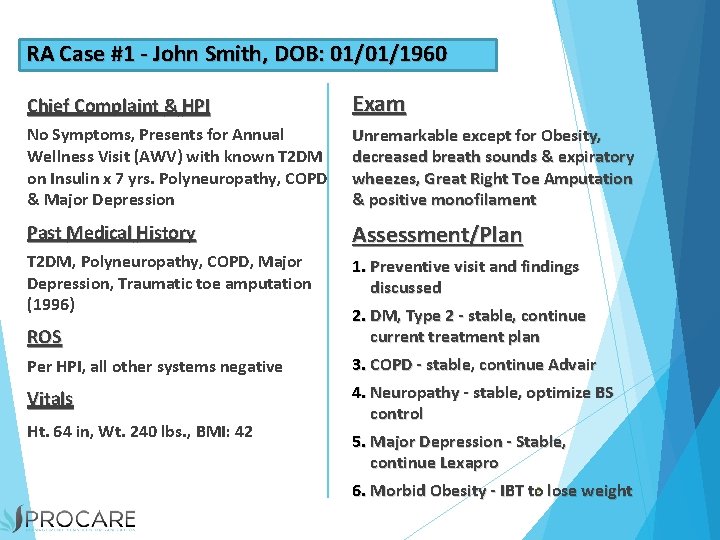
RA Case #1 - John Smith, DOB: 01/01/1960 Chief Complaint & HPI Exam No Symptoms, Presents for Annual Wellness Visit (AWV) with known T 2 DM on Insulin x 7 yrs. Polyneuropathy, COPD & Major Depression Unremarkable except for Obesity, decreased breath sounds & expiratory wheezes, Great Right Toe Amputation & positive monofilament Past Medical History Assessment/Plan T 2 DM, Polyneuropathy, COPD, Major Depression, Traumatic toe amputation (1996) ROS Per HPI, all other systems negative Vitals Ht. 64 in, Wt. 240 lbs. , BMI: 42 1. Preventive visit and findings discussed 2. DM, Type 2 - stable, continue current treatment plan 3. COPD - stable, continue Advair 4. Neuropathy - stable, optimize BS control 5. Major Depression - Stable, continue Lexapro 6. Morbid Obesity - IBT to 5 lose weight
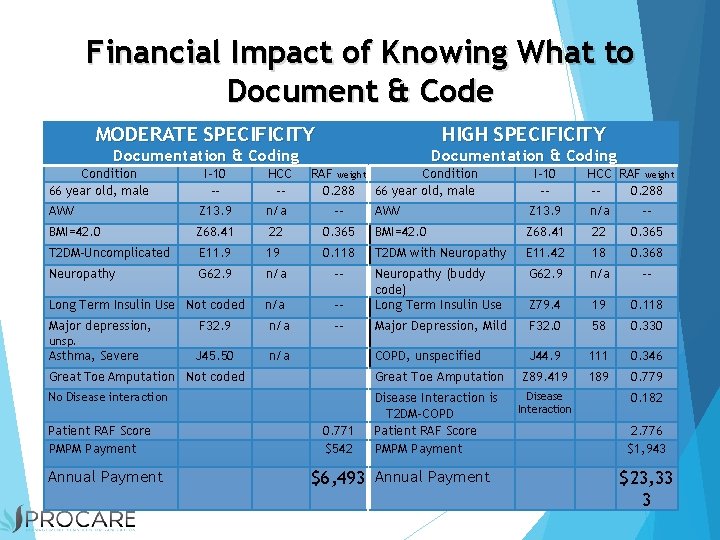
Financial Impact of Knowing What to Document & Code MODERATE SPECIFICITY HIGH SPECIFICITY Documentation & Coding Condition 66 year old, male Documentation & Coding I-10 -- HCC -- AWV Z 13. 9 n/a -- BMI=42. 0 Z 68. 41 22 T 2 DM-Uncomplicated E 11. 9 Neuropathy G 62. 9 Long Term Insulin Use Not coded Major depression, RAF weight Condition 0. 288 66 year old, male I-10 -- HCC RAF weight -0. 288 AWV Z 13. 9 n/a -- 0. 365 BMI=42. 0 Z 68. 41 22 0. 365 19 0. 118 T 2 DM with Neuropathy E 11. 42 18 0. 368 n/a -- G 62. 9 n/a -- Neuropathy (buddy code) Long Term Insulin Use Z 79. 4 19 0. 118 -- Major Depression, Mild F 32. 0 58 0. 330 COPD, unspecified J 44. 9 111 0. 346 Z 89. 419 189 0. 779 F 32. 9 n/a J 45. 50 n/a unsp. Asthma, Severe Great Toe Amputation Not coded Great Toe Amputation No Disease interaction Disease Interaction is T 2 DM-COPD Patient RAF Score PMPM Payment Annual Payment 0. 771 $542 $6, 493 Annual Payment Disease Interaction 0. 182 2. 776 $1, 943 $23, 33 3
The most financially impactful is the ICD-10 Risk Scoring of Patients based on: 1. The 8, 830 Risk Adjusting I-10 codes, better known as the CMS HCC-RAF codes, found within the 140, 000 total I-10 codes. 2. There are ~10, 500 Risk Adjusting I-10 codes for most commercial payers that utilize proprietary Risk Scoring grouper models 7

The 4 Essential Keys to Improving Healthcare Quality & Financial Outcomes are: 1. Mastering Risk Adjustment Factor (RAF) Recognition, Documentation & Coding! 2. Mastering HEDIS/PQRS quality measures compliance 3. Eliminating Inefficient Spending & Resource Consumption! 4. Delivering Exceptional Customer Service to Achieve Outstanding Patient Experiences! 8
The most successful healthcare providers will formulate and implement strategies to: 1. Better manage spending, utilization and resource consumption. 2. Capture & satisfy quality measures HEDIS/PQRS/MACRA. 3. And more importantly, robustly embrace the recognition, documentation & coding of Risk Adjustment Factor opportunities to the highest levels of accuracy and specificity to insure the lowest possible Medical Loss Ratios (MLRs). 9

What is Risk Adjustment? 10
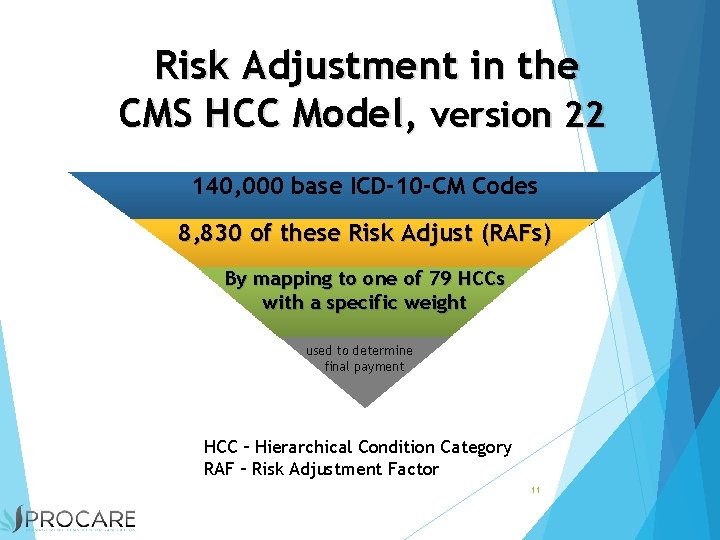
Risk Adjustment in the CMS HCC Model, version 22 140, 000 base ICD-10 -CM Codes 8, 830 of these Risk Adjust (RAFs) By mapping to one of 79 HCCs with a specific weight used to determine final payment HCC – Hierarchical Condition Category RAF – Risk Adjustment Factor 11
How is a HCC-RAF captured? ~ First, you must ‘recognize’ it! ~ Secondly, you must accurately and thoroughly document it with M. E. A. T. ! ~ Thirdly, you must code it correctly! Don’t delegate RAF coding to a coder! A ‘best practice’ strategy is to utilize the ‘Quick HCC-RAF Recognition’ tool by SH&WS in every exam room. 12
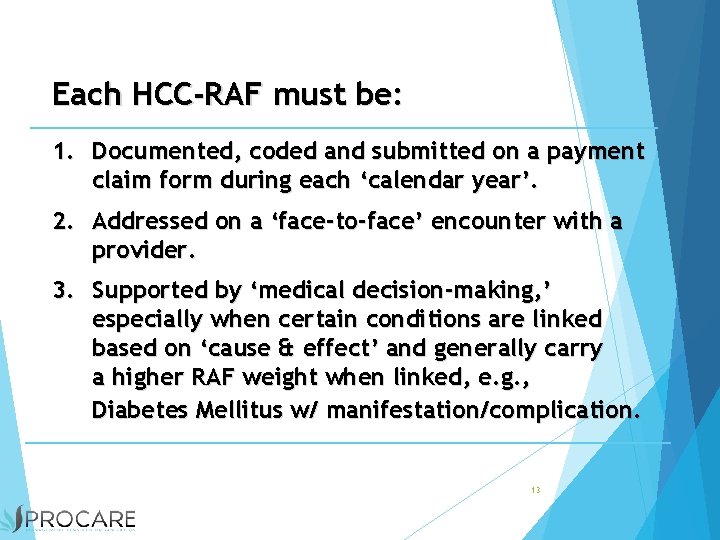
Each HCC-RAF must be: 1. Documented, coded and submitted on a payment claim form during each ‘calendar year’. 2. Addressed on a ‘face-to-face’ encounter with a provider. 3. Supported by ‘medical decision-making, ’ especially when certain conditions are linked based on ‘cause & effect’ and generally carry a higher RAF weight when linked, e. g. , Diabetes Mellitus w/ manifestation/complication. 13
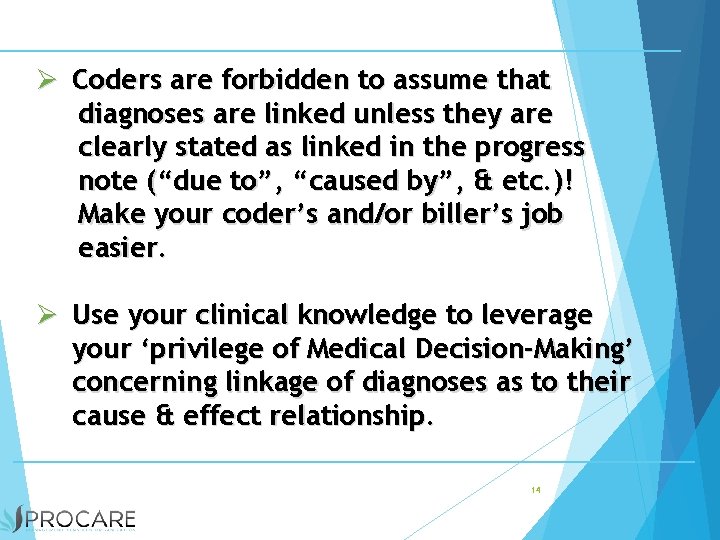
Ø Coders are forbidden to assume that diagnoses are linked unless they are clearly stated as linked in the progress note (“due to”, “caused by”, & etc. )! Make your coder’s and/or biller’s job easier. Ø Use your clinical knowledge to leverage your ‘privilege of Medical Decision-Making’ concerning linkage of diagnoses as to their cause & effect relationship. 14
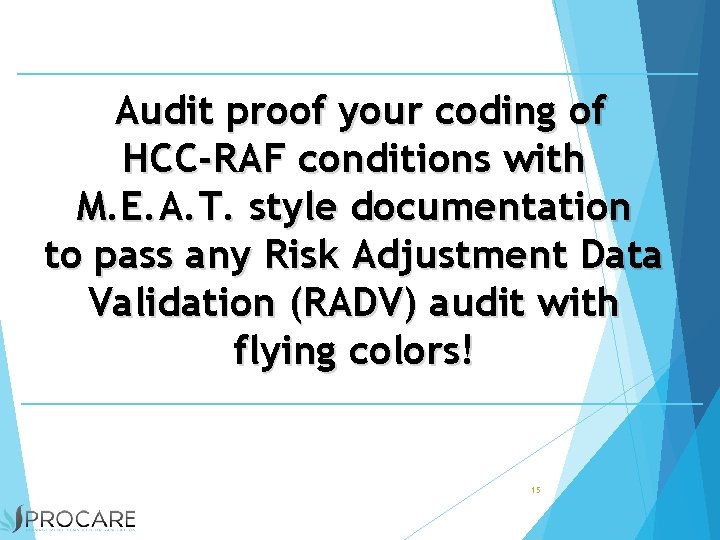
Audit proof your coding of HCC-RAF conditions with M. E. A. T. style documentation to pass any Risk Adjustment Data Validation (RADV) audit with flying colors! 15
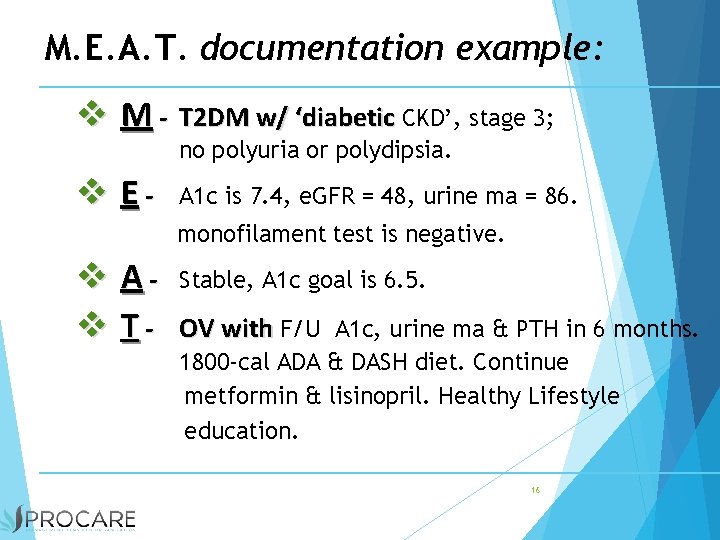
M. E. A. T. documentation example: M - T 2 DM w/ ‘diabetic CKD’, stage 3; no polyuria or polydipsia. E- A 1 c is 7. 4, e. GFR = 48, urine ma = 86. monofilament test is negative. A T- Stable, A 1 c goal is 6. 5. OV with F/U A 1 c, urine ma & PTH in 6 months. 1800 -cal ADA & DASH diet. Continue metformin & lisinopril. Healthy Lifestyle education. 16
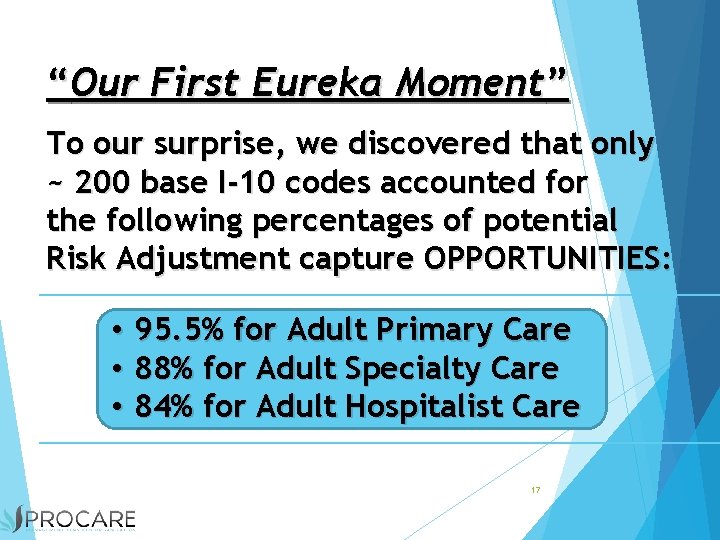
“Our First Eureka Moment” To our surprise, we discovered that only ~ 200 base I-10 codes accounted for the following percentages of potential Risk Adjustment capture OPPORTUNITIES: • 95. 5% for Adult Primary Care • 88% for Adult Specialty Care • 84% for Adult Hospitalist Care 17
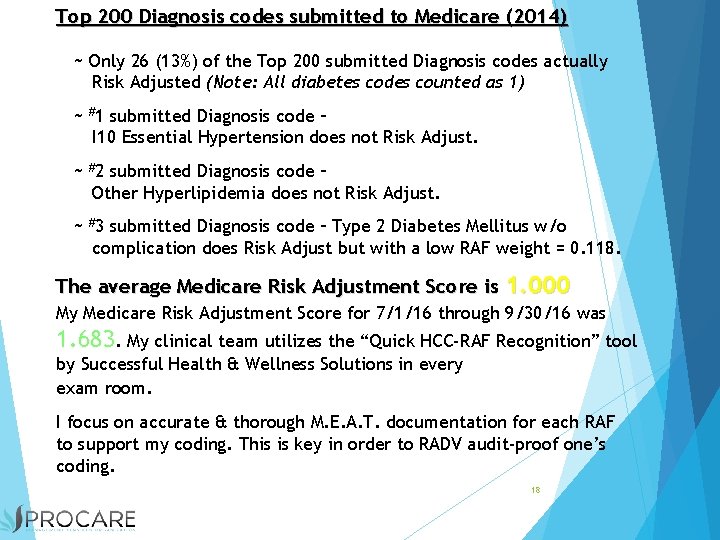
Top 200 Diagnosis codes submitted to Medicare (2014) ~ Only 26 (13%) of the Top 200 submitted Diagnosis codes actually Risk Adjusted (Note: All diabetes codes counted as 1) ~ #1 submitted Diagnosis code – I 10 Essential Hypertension does not Risk Adjust. ~ #2 submitted Diagnosis code – Other Hyperlipidemia does not Risk Adjust. ~ #3 submitted Diagnosis code – Type 2 Diabetes Mellitus w/o complication does Risk Adjust but with a low RAF weight = 0. 118. The average Medicare Risk Adjustment Score is 1. 000 My Medicare Risk Adjustment Score for 7/1/16 through 9/30/16 was 1. 683. My clinical team utilizes the “Quick HCC-RAF Recognition” tool by Successful Health & Wellness Solutions in every exam room. I focus on accurate & thorough M. E. A. T. documentation for each RAF to support my coding. This is key in order to RADV audit-proof one’s coding. 18
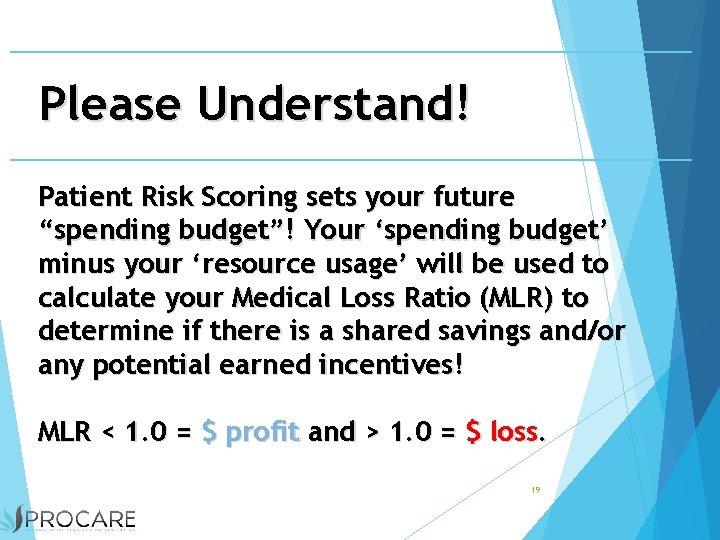
Please Understand! Patient Risk Scoring sets your future “spending budget”! Your ‘spending budget’ minus your ‘resource usage’ will be used to calculate your Medical Loss Ratio (MLR) to determine if there is a shared savings and/or any potential earned incentives! MLR < 1. 0 = $ profit and > 1. 0 = $ loss. 19
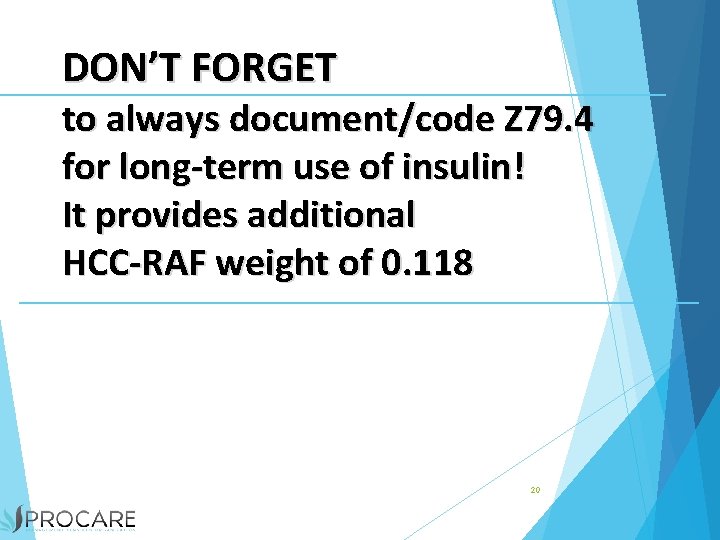
DON’T FORGET to always document/code Z 79. 4 for long-term use of insulin! It provides additional HCC-RAF weight of 0. 118 20
Primary Care Providers should Always perform an ‘ANNUAL WELLNESS VISIT’ (AWV) for Medicare Patients, part B & C, or an ‘ANNUAL PREVENTATIVE EXAM’ (APE) for Commercial Insurance Patients 21
We do the unthinkable by: 1. Putting the patient front and center 2. Teaching physicians to connect with patients through emotional intelligence and shared decision-making 3. Transforming medical practices from fragmented, reactive, episodic sick care to proactive, continuous, wholistic well-care 4. Re-vitalizing the team-based health caring approach. 5. Leveraging the most underutilized care team members 1. Nurses 2. Coaches/Nutritionists 3. Pharmacists 22
We are in the midst of a major shift in healthcare reimbursement for providers. This is happening in every aspect of the healthcare industry. Physician's office Hospitals Home Health Skilled Nursing 23
Value Based Care requires a NEW way of Thinking! Historically Providers: ► Document the history of a patient when the patient is new- They do not document on an annual basis ► Submit CPT & ICD diagnosis codes on claims to validate reimbursement for services already rendered. ► Look at outcomes from a financial perspective. ► Treat chronic conditions as maintenance visits ► Preventive care was treated as an option to patients because traditionally is was not a covered service 24
Two challenges to keep in mind: 25
Physician Burnout… 63% for Primary Care according to the Mayo Clinic’s ongoing study… * 36% in 2013 ~ Improving providers time, flow and operations is fundamental in helping them succeed in the transition to value based care. 26
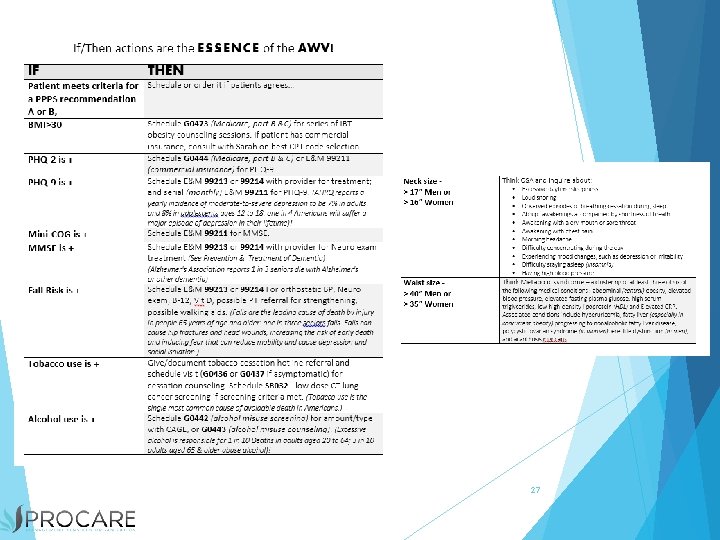
27
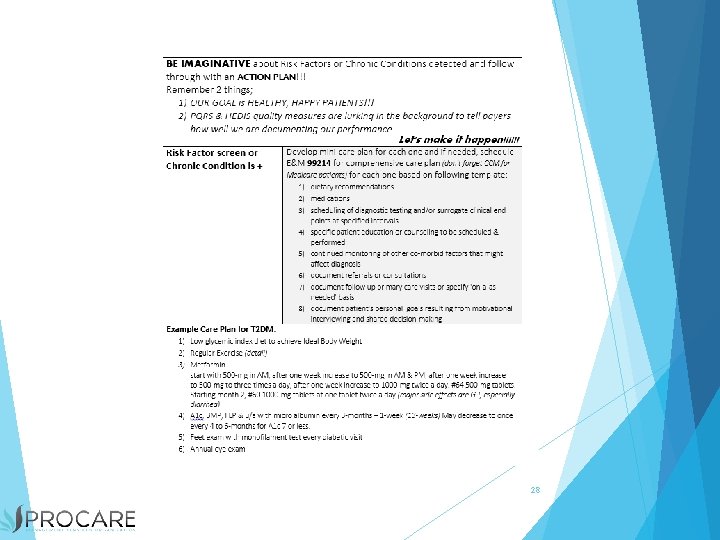
28

Knowledge Transfer “Successful knowledge transfer involves neither computers nor documents but rather interactions among people”

The Goal is…. HEALTHY, HAPPY PATIENTS 30
- Slides: 30