Massive Fluid Resuscitation D John Doyle MD Ph




![What Fluids to Give? • Crystalloids [start with crystalloids] – Ringers – Saline – What Fluids to Give? • Crystalloids [start with crystalloids] – Ringers – Saline –](https://slidetodoc.com/presentation_image/9d1a02eddae745de5f1915e2908a603c/image-11.jpg)














- Slides: 60
Massive Fluid Resuscitation D. John Doyle MD Ph. D FRCPC Cleveland Clinic Foundation March 2003
Outline • • Clinical Need for Massive Fluid Resuscitation What to Fluids to Give? When to Give Colloids When to Give Blood Products Things to Look Out For Avoiding Overzealous Resuscitation Limits to Hydroxyethyl Starch Administration
What is Massive Fluid Resuscitation? • • No strict definition Over 10 liters of crystalloid / colloid (? ) Usually involves an unstable patient May involve massive transfusion

What is a Massive Transfusion? Massive transfusion is the replacement of more than one blood volume (about 65 ml/kg) with blood components within several hours. (Some authors say 10 units of blood in under 24 hours).
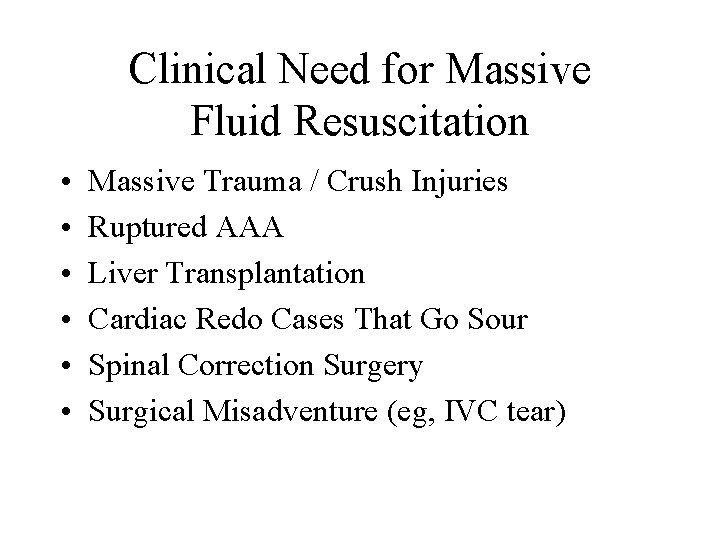
Clinical Need for Massive Fluid Resuscitation • • • Massive Trauma / Crush Injuries Ruptured AAA Liver Transplantation Cardiac Redo Cases That Go Sour Spinal Correction Surgery Surgical Misadventure (eg, IVC tear)

Some Sources of Massive Blood Loss Car Accidents from www. trauma. org (trauma image bank) Earthquakes Penetrating Trauma

Penetrating Trauma from www. trauma. org (trauma image bank) 28 yr old male, motorcycle collision, fall over pieces of wood. The patient was haemodynamically normal, conscious, just demanding the removal of the stick. Nevertheless, he was submitted to an emergent left thoracotomy, and left laparotomy. The piece of wood was just located behind the sternum and in front of the heart with no major vascular or cardiac injury found, only a perforation of the diaphragm. Intraabdominally, the piece passed between the left lobe of the liver and the spleen with no further injury. We found this almost unbelievable! Source: Luis Filipe Pinheiro, Viseu, Portugal

from www. trauma. org (trauma image bank) Widened Mediastinum from Aortic Tear
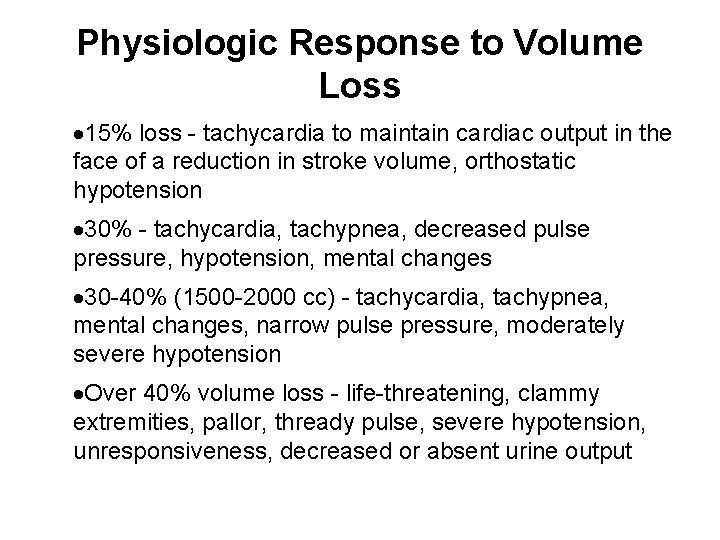
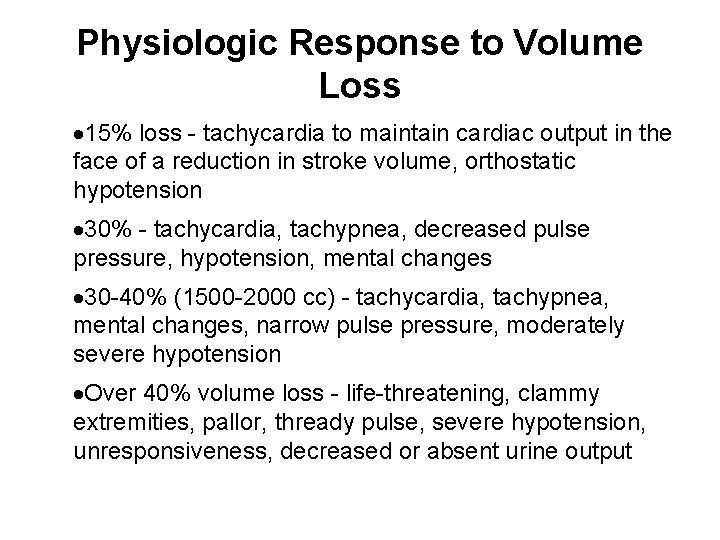
Physiologic Response to Volume Loss · 15% loss - tachycardia to maintain cardiac output in the face of a reduction in stroke volume, orthostatic hypotension · 30% - tachycardia, tachypnea, decreased pulse pressure, hypotension, mental changes · 30 -40% (1500 -2000 cc) - tachycardia, tachypnea, mental changes, narrow pulse pressure, moderately severe hypotension ·Over 40% volume loss - life-threatening, clammy extremities, pallor, thready pulse, severe hypotension, unresponsiveness, decreased or absent urine output
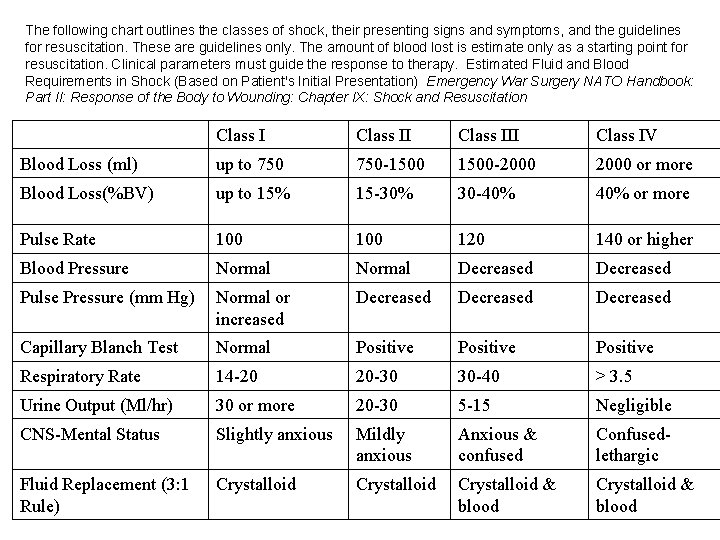
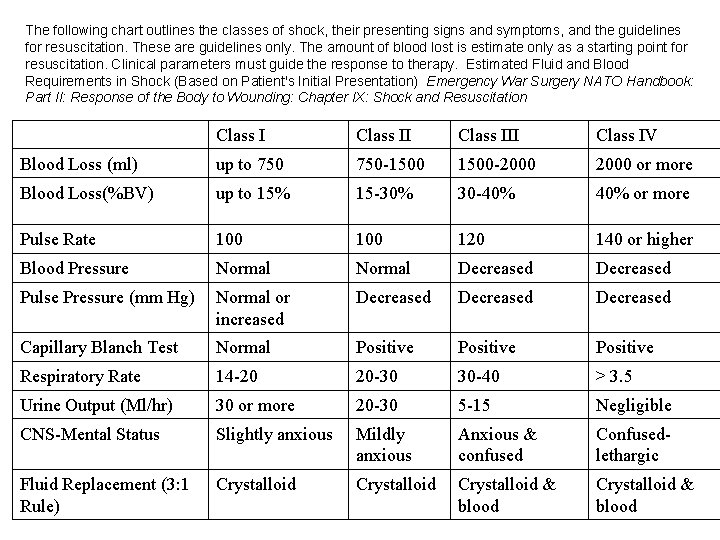
The following chart outlines the classes of shock, their presenting signs and symptoms, and the guidelines for resuscitation. These are guidelines only. The amount of blood lost is estimate only as a starting point for resuscitation. Clinical parameters must guide the response to therapy. Estimated Fluid and Blood Requirements in Shock (Based on Patient's Initial Presentation) Emergency War Surgery NATO Handbook: Part II: Response of the Body to Wounding: Chapter IX: Shock and Resuscitation Class III Class IV Blood Loss (ml) up to 750 -1500 1500 -2000 or more Blood Loss(%BV) up to 15% 15 -30% 30 -40% or more Pulse Rate 100 120 140 or higher Blood Pressure Normal Decreased Pulse Pressure (mm Hg) Normal or increased Decreased Capillary Blanch Test Normal Positive Respiratory Rate 14 -20 20 -30 30 -40 > 3. 5 Urine Output (Ml/hr) 30 or more 20 -30 5 -15 Negligible CNS-Mental Status Slightly anxious Mildly anxious Anxious & confused Confusedlethargic Crystalloid & blood Fluid Replacement (3: 1 Rule) Crystalloid & blood
![What Fluids to Give Crystalloids start with crystalloids Ringers Saline What Fluids to Give? • Crystalloids [start with crystalloids] – Ringers – Saline –](https://slidetodoc.com/presentation_image/9d1a02eddae745de5f1915e2908a603c/image-11.jpg)
What Fluids to Give? • Crystalloids [start with crystalloids] – Ringers – Saline – Special crystalloids • Colloids [rule of thumb: start colloids at 15 - 20% blood volume loss] – – Blood Products Albumin Pentaspan Special colloids
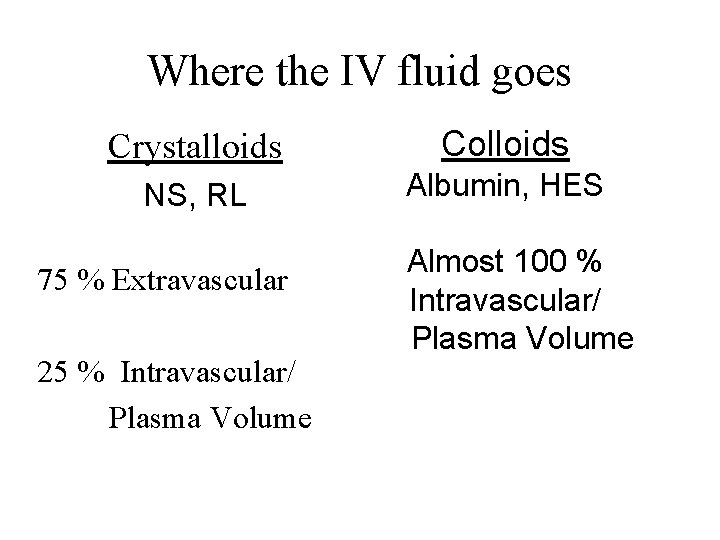
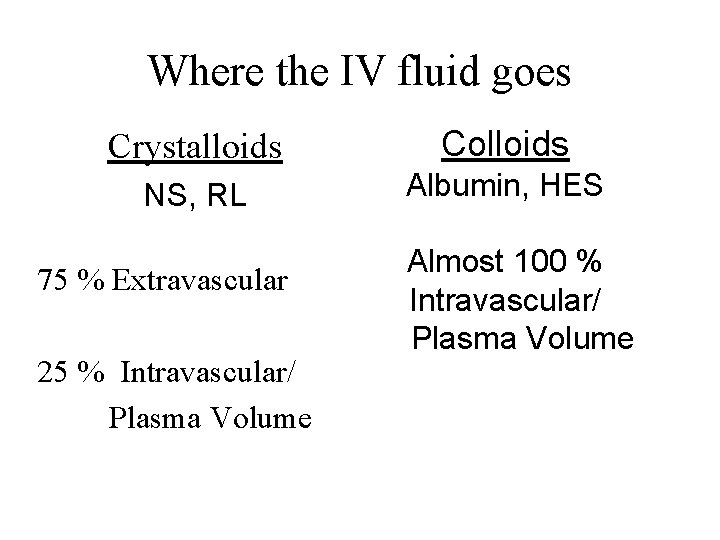
Where the IV fluid goes Crystalloids Colloids NS, RL Albumin, HES 75 % Extravascular 25 % Intravascular/ Plasma Volume Almost 100 % Intravascular/ Plasma Volume

Rule of thumb: Start Colloids at 15 - 20% Blood Volume Loss Example (20% blood loss rule of thumb) n 77 kg man n Blood volume estimated at 65 ml/kg x 77 kg = 5 liters n 20% blood volume = 1 liter of blood n Crystalloid replacement for 1 liter blood is 3 -4 liters n Thus, consider starting a colloid after 3 -4 liters of crystalloid given to replace lost blood
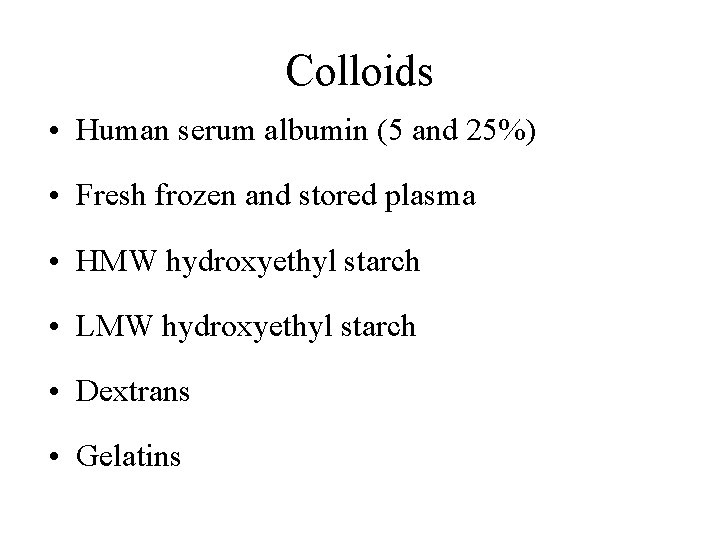
Colloids • Human serum albumin (5 and 25%) • Fresh frozen and stored plasma • HMW hydroxyethyl starch • LMW hydroxyethyl starch • Dextrans • Gelatins
Advantages of Colloids • Less edema • Less volume administered • Less thermal load effect for given level of plasma volume expansion • Volume administer stays in intravascular space longer

Concerns with Colloids • Decreased hemoglobin • Dilution of plasma proteins (Dextrans, HES) • Dilution of coagulation factors (PT, PTT) • Pulmonary edema • Allergic reaction
Artificial Colloid Solutions • Hydroxyethyl Starches (HESs) – LMW (Pentraspan, Penta. Lyte) – HMW (Hespan, Hextend) • Dextrans • Gelatins Artificial colloids, unlike crystalloids, are complex entities that undergo a regulatory approval process similar to that for a drug.
Human Serum Albumin • Most abundant protein in the plasma • MW 69, 000 daltons • Prepared from human donor plasma in isotonic saline • Source of unending controversy
Dextrans • Linear polysaccharides produced from sucrose by Leuconostoc Mesenteroides bacterium • Much less common use today • Two main forms – Dextran 70 (MWw 70 K) – Dextran 40 (MWw 40 K)
Hespan (6 % Hydroxyethyl Starch) • Available as 6% solution in normal saline w/ osmolarity of 310 m. Osm/l; • Plasma volume expansion for more than 24 hrs • Like Dextran, can be associated w/ urticarial & anaphylactoid reactions • Half life for 90% of particles is 17 days, whereas that of remaining 10% is 48 days • Dosage: - usually 500 -1000 ml (do not usually exceed 1500 ml/day) IV at a rate not to exeed 20 ml/kg/hr; ); • Precautions: - Not a substitute for blood or plasma; - Contraindicated in patients with severe bleeding disorders, severe CHF, or renal failure with oliguria or anuria;
Hespan and Heparin mix-ups Problem: A fatal error occurred when a nurse mistakenly selected and administered two heparin 25, 000 unit per 500 m. L premixed bags instead of HESPAN (hetastarch) for a patient who was actively bleeding. Such mix-ups have been reported on several occasions to USP, ISMP and FDA. Although this is primarily a nomenclature issue (both names include the characters h-e-p-a and n in the same sequence), the drugs are also found in similar IV bags with blue and red labeling. Since Hespan may be used in patients who are actively bleeding, the danger of inadvertent heparin administration is obvious. Recommendation: Since hetastarch is now manufactured generically by other companies, consider using an alternate to Hespan and refer to hetastarch products by generic name. If Hespan remains in stock, do not store alphabetically next to premixed heparin products. Label products, storage bins, and automated dispensing machine pockets with a reminder about error potential. ISMP has communicated with FDA and the manufacturer about this serious problem. http: //www. ismp. org/MSAarticles/A 4 Q 99 Action. html
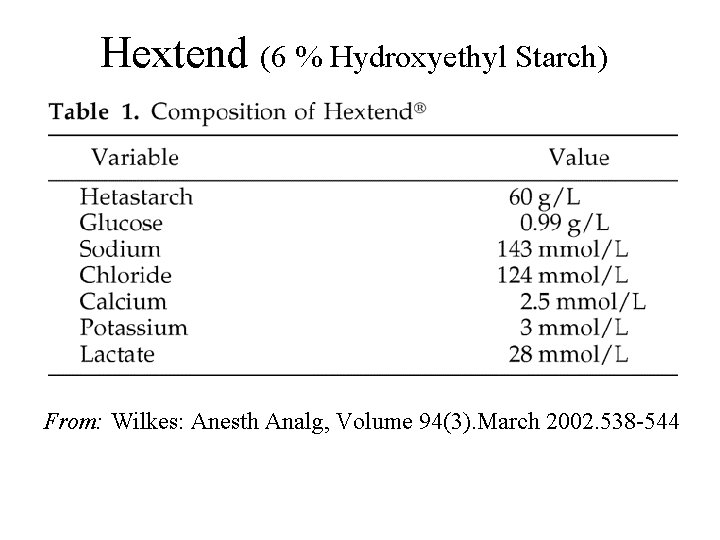
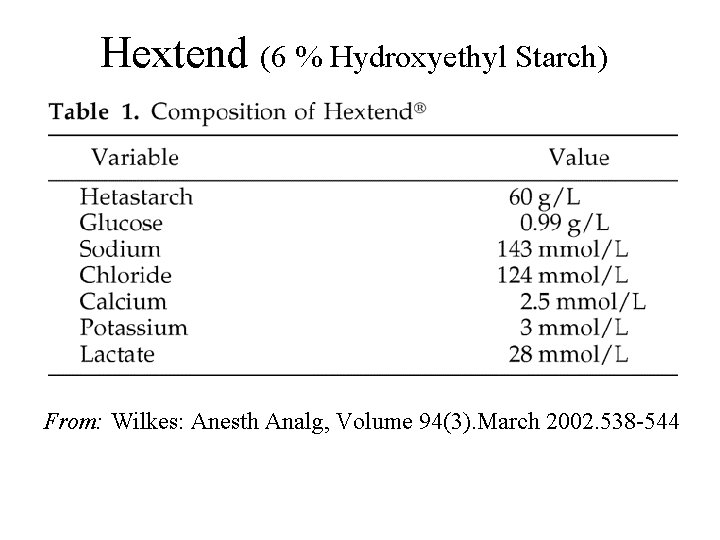
Hextend (6 % Hydroxyethyl Starch) From: Wilkes: Anesth Analg, Volume 94(3). March 2002. 538 -544

HES - Pentaspan • Synthetic plasma volume expander • Average MW 200, 000 – 300, 000 daltons • Plasma volume expansion exceeds volume of Pentaspan infused – lasting 18 -24 h • 12 -24 h improvement in hemodynamic status • 70% excreted in the urine in 24 hr • Metabolised by serum amylases

Source: Bio. Time, Inc.
Massive Fluid Resuscitation: Sources of Trouble • Not enough experience (lack of proactive management) • Not enough help • Not enough lines • Not enough fluid warmers • Not monitoring coagulation

Massive Fluid Resuscitation: Things to Look Out For • • • Hypothermia Hypocalcemia and hypomagnesemia Coagulopathy Acidosis Severe anemia Airway edema
Predicting Life-Threatening Coagulopathy in the Massively Transfused Trauma Patient Cosgriff N, Moore EE, Sauaia A, Kenny-Moynihan M, Burch JM, Galloway B Predicting life-threatening coagulopathy in the massively transfused trauma patient: hypothermia and acidoses revisited. J Trauma 1997 May; 42(5): 857 -61; Postinjury life-threatening coagulopathy in the seriously injured requiring massive transfusion is predicted by persistent hypothermia and progressive metabolic acidosis.

What Mechanisms Lead to Coagulopathy in Massive Transfusions? Coagulation defects develop primarily from dilution of protein coagulation factors and platelets when crystalloid, colloid and red blood cells are used to replace lost volume. Hypothermia frequently also plays a role.

Massive Fluid Resuscitation Using Plasma-Poor Red Cells “Hypofibrinogenemia develops first followed by other coagulation factor deficits and later by thrombocytopenia. Therefore the use of fresh frozen plasma (FFP) is the primary intervention to treat abnormal bleeding encountered in the replacement of massive blood loss with plasma-poor red cells. ” Replacement of massive blood loss. Hiippala S. Vox Sang 1998; 74 Suppl 2: 399 -407
Characteristics of Coagulopathy with Massive Transfusions Coagulopathy associated with massive transfusion is characterized clinically by microvascular bleeding or oozing from the mucosa, wound and puncture sites. Surgeons will complain that clot formation ins impaired.

How Should Coagulopathy From Massive Transfusions Ideally be Treated? Empirical formulas using ratios of various components to volume administered are often inadequate to appropriately treat or prevent coagulopathy of massive transfusion. Treatment should include restoration of systemic perfusion, maintenance of normal temperature and blood component therapy supported by laboratory tests.
Consequences of Using Plasma-Poor Red Cells • Plasma-poor red cells are now commonly used instead of whole blood or packed red blood cells to supply hemoglobin during blood loss. • Since the plasma content of plasma-poor red cells is rather small, a deficit of plasma and coagulation factors develops earlier than during transfusion of whole blood or packed red blood cells.

When to Give Blood Products • Rules for homologous packed cells • Rules for autologous whole blood • Rules for plasma, FFP • Rules for platelets • Rules for cryoprecipitate • Rules for albumin • Rules for synthetic blood (investigational)

Platelets • In patients with thrombocytopenia, the risk of hemorrhage increases progressively once the platelet count drops below 100, 000/µL. • With normally functioning platelets, most major surgery can be safely performed if the count remains within the range of 50, 00075, 000/µL.
Are Prophylactic Platelets and FFP Indicated in Massive Transfusion? “Platelets should not be routinely administered during massive transfusion. While thrombocytopenia may develop in massively transfused patients, administration of platelets should be reserved for the patient exhibiting microvascular bleeding and a platelet count less than 50 x 109/L. Platelet transfusion may be necessary for patients with intermediate platelet counts (50 -100 x 109/L) if it is determined the risk for more bleeding is significant. ” [http: //www. asahq. org/Prof. Info/Transfusion/Massive. html]
Are Prophylactic Platelets and FFP Indicated in Massive Transfusion? “As the development of thrombocytopenia is a highly individual phenomenon, the transfusion of platelets should be guided by repeatedly determined platelet counts. ” Replacement of massive blood loss. Hiippala S. Vox Sang 1998; 74 Suppl 2: 399 -407
Clotting Factors • Blood normally contains a relative abundance of each clotting factor and hemorrhage is a rare occurrence unless any one of these factors is reduced to less than 50% of normal. • Deficiency of a single factor is usually the result of an inherited coagulation deficiency disorder. • Acquired coagulation disorders are usually the result of multiple factor deficiencies.
Are Prophylactic Platelets and FFP Indicated in Massive Transfusion? “FFP also should not be administered prophylactically for massive transfusion. In the massively transfused patient, clinical bleeding associated with coagulation factor deficiencies is unlikely until factor levels fall below 20 percent of normal. In the clinical setting, this usually does not occur until greater than one blood volume has been replaced and the PT and PTT are less than 1. 5 times control values. In the event the PT and PTT cannot be obtained in a timely fashion, FFP may be administered for correction of microvascular bleeding in patients transfused with more than one blood volume. ” [http: //www. asahq. org/Prof. Info/Transfusion/Massive. html]
Another Viewpoint on Massive Blood Transfusions In the past, prophylactic fresh-frozen plasma (FFP) and platelets transfusion has been said to have no place. However, relying on a specific biological diagnosis of the hemostatic defect is an unrealistic view in high bleeding rate situations. ” “ “Considering the time scale for laboratory screening and blood components availability, the use of FFP is advocated as soon as one blood volume has been replaced. ” “ If platelet counts and units may be more easily obtained, platelets transfusion may be guided by repeatedly determined platelet counts. ” Massive blood transfusion, blood volume expansion and hemostasis Hématologie. Vol. 6, Issue 3, May - June 2000: 191 -7, Reviews http: //www. john-libbey-eurotext. fr/articles/hma/6/3/191 -7/en-resum. htm

How Should Coagulation be Monitored During Massive Transfusion? Routine coagulation tests that evaluate protein coagulant activity, ( PT, PTT, INR and thrombin time), do not reliably predict perioperative bleeding, but they help identify patients with deficiencies of coagulation factors. Standard laboratory tests along with platelet count and fibrinogen level should guide the use of component therapy. Bleeding time is not predictive of perioperative bleeding and is rarely accessible in the operating room setting. The activated clotting time (ACT) is influenced by both hypofibrinogenemia and coagulation factor deficiencies, and this lack of specificity limits ACT as a useful test during massive transfusion. [Modified from http: //www. asahq. org/Prof. Info/Transfusion/Massive. html]
How Should Coagulation be Monitored During Massive Transfusion? Whole blood clotting analysis, as seen with the Thromboelastograph® (TEG) and Sonoclot®, provides a dynamic picture of the entire clotting process. Both the TEG and Sonoclot® measure the viscoelastic properties of blood. These tests evaluate the development of a blood clot from the initial fibrin strands to eventual clot retraction or lysis. The usefulness of TEG or Sonoclot® during massive transfusion has not been established. [http: //www. asahq. org/Prof. Info/Transfusion/Massive. html]
HES and Massive Blood Transfusions “Hydroxyethyl starch (HES) solutions are frequently used and differ in their pharmacological properties. ” “An acquired von Willebrand syndrome may result from the infusion of high molecular weight (MW) or of large volumes of medium MW HES solutions. ” “ HES solutions infusions should be restricted according to recommended dose limits. ” Massive blood transfusion, blood volume expansion and hemostasis Hématologie. Vol. 6, Issue 3, May - June 2000: 191 -7, Reviews http: //www. john-libbey-eurotext. fr/articles/hma/6/3/191 -7/en-resum. htm

Example: Disastrous Liver Transplant • Preexisting coagulopathy • “Bad feeling” about outcome • 5 IVs to start, 2 more (femorals) started during the case • 142 units packed cells • Arrived in ICU alive, but died soon after
MEGA TRANSFUSION FOR LIVER TRANSPLANTATION (Posting to GASNet Anesthesiology Discussion Group) D. John Doyle Two weeks ago my resident and I (with help from nurses and others) gave the following blood products in the on-going resuscitation of a patient undergoing an eleven hour liver transplant: - 142 units of packed cells - 61 units of fresh frozen plasma - 15 liters of 5% albumin As well, cryoprecipitate and platelets were given, along with about 25 liters of crystalloid. We had seven IVs, of which four were warmed. All blood bags were pressurized to 400 mm. Hg with a wrap-around bag system. The hemoglobin concentration on arrival (alive!) in the surgical ICU was 11. 3 g/dl. This may be something of a record. Does anyone know of similar stories either from the literature or from personal experience?
Reply 1 You were just getting warmed up! I personally assisted in getting 500 donor units in the room for one patient, and I have been told by a reliable source whose name you would recognize that over 1000 units have been used in a single case. Both of these were some years ago, and it is my impression that the overall situation is now much improved. The case I knew of personally did not survive to leave the operating room. It might be hard to get data on the actual records, as those who know about them might not want to confess. I am now somewhat out of touch with this, as I have not done livers myself for the past 11. 5 years.
Reply 2 Bravo! I have given 195 packed red cells for a liver transplant, but we were using a rapid infusion system. The reservoir filter got clogged and we had to replace it during ongoing blood loss. Not fun. I guess you now have powerfully developed forearms from pumping up those bags.
Reply 3 My experience with these mega transfusions for liver transplants (> 100 units) is that although they usually arrive in the ICU, they usually do not leave the hospital alive. I wonder if we shouldn't have the surgeons pack the wound after a fixed amount of blood is given, (and the liver seems to be adequately sutured in place), and then return the patient to the OR on the next day if the patient is still alive. The amount of blood wasted seems a shame.
Reply 4 Your message prompted several questions, which I hope will stimulate discussion: 1) is the patient still alive? ; 2) if not, was the expenditure of such expensive resources worth it? ; 3)if so, does it appear s/he's going to make it? ; 4) is liver transplantation something we should be doing, something we should be investing such resources in? Thoughts, everyone.
Reply 5 - Response to Replies 1 -4 More on Megatransfusions in Liver Transplantation In response to discussion on the above topic, I am providing the additional information about my mega-transfusion case (142 units of packed cells). Yes, the patient died (no suprise), but he lasted over 48 hours in the ICU with increasingly more aggressive inotropic support (dopamine +epinephrine +levophed), continuing replacement of blood losses, and even high-frequency jet ventilation on and off. He gained about 50 kg (preop under 100 kg; 150 kg at death) from third spacing.
Reply 5 - Continued We did not use a rapid infusor as (eg, Level One), but avoided hand pumping by using a air regulator system set at a pressure of 400 mm. Hg hooked up to four or more "wrap around" pressure bags with velcro tabs. All blood was filtered to avoid clogging the filters in the blood sets; filters were changed after 3 or so bags (otherwise the filter resistance would be too high). Despite four blood warmers, a heated humidifier, two forced air heaters and a very warm OR, nasopharyngeal temperature was only 32. 2 Celsius at the time of unclamping. (We have seen V Fib on unclamping with colder temperatures) We used the QT interval to "monitor" calcium levels. Despite giving calcium periodically, at one point the ionized calcium was 10% of the lower limit of normal! (At that point we drew up 6 g of Ca. Cl 2 in a 60 cc syringe and gave it over about 30 minutes. )
Reply 5 - Continued This case gave us (and the surgeons) much to think about in terms of patient selection. Some of my colleagues are particularly distressed to find that some (many) of the patients are (reformed) alcoholics. D. John Doyle
Minimal Volume Resuscitation Recent studies have shown possible adverse outcomes with aggressive fluid resuscitation and restoration of blood pressure prior to control of bleeding source, esp. in penetrating torso trauma. (Minimal volume fluid resuscitation : Aim for MAP of 40 mm Hg or a SBP of 60 to 80 mm Hg)
Immediate Versus Delayed Fluid Resuscitation for Hypotensive Patients With Penetrating Torso Injuries g Bickell, W. H. , et al, N Engl J Med 331: 1105, 1994 g Prospective trial of 598 patients with penetrating torso trauma and systolic BP < 90 mm Hg g Standard resuscitation vs limited resuscitation (until time of surgical intervention)
Limited resuscitation g 375 mls IV fluid g Initial BP 72 mm Hg systolic g 30% mortality g 23% complication rate

Standard Resuscitation g 2, 480 mls IV fluid g Initial BP 78 mm Hg systolic g 38% mortality (p=0. 04) g 30% complication rate
Comment by Dr. Edward Crosby Two solitudes are evolving regarding the optimum timing and scale of fluid administration after penetrating trauma. One view is that immediate fluid resuscitation should be avoided in victims of penetrating trauma, since restoration of the blood pressure may promote further hemorrhage. This may result in the need for massive blood transfusion with resultant dilutional coagulopathy, and technical surgical difficulties. Dr. Edward Crosby, University of Ottawa
Comment by Dr. Edward Crosby The opposing (and more conventional) view is that fluid resuscitation should be started immediately since the longer the period of shock the greater the risk of developing multiple system organ failure. An argument against fluid restriction is that the blood pressure at presentation is an important factor influencing survival following trauma with the incidence of multisystem complications correlating with the duration and intensity of shock. An additional concern is that, should there be barriers to rapid surgical intervention, non-resuscitated patients may exsanguinate while awaiting operation.

Comment by Dr. Edward Crosby The majority of patients assessed by Bickell were in hospital within 30 min of reported injury and entered the operating room in less than one hour of hospital time. Finally, it must be recognized that the reviewed studies (animal and human) address models and clinical situations relating to penetrating injury and are not generalizable to the patient population with blunt traumatic injury. Dr. Edward Crosby, University of Ottawa
Special. Ops. Medicine. Com “The only benefit of "controlled shock" management of a patient with penetrating body cavity trauma and an uncontrolled internal arterial hemorrhage is a hope that the hemorrhage will eventually clot. Hopefully, a stasis at a low BP will occur allowing a clot to form. Studies have shown, in the early stages of fibrinogen clot formation, raising the systolic pressure above 80 mm Hg will weaken or break the clot formation causing the bleeding to resume. That’s why a therapeutic goal of 70 -80 mm Hg and a pulse of <120 BPM is desired to prevent this clot from weakening. The state of controlled shock can only be maintained for a short period of time (1 -2 hours) before systemic complications and organ failure begin to occur. Rapid evacuation and transport to a surgeon, and an infusion of the whole blood are the only treatments that will save the patient’s life. ”
The End