Maryland Opioid Overdose Response Program Training for Potential

![Step 1: Rouse & Stimulate Noise: Shake person’s shoulders and yell: “[Name!] Are you Step 1: Rouse & Stimulate Noise: Shake person’s shoulders and yell: “[Name!] Are you](https://slidetodoc.com/presentation_image_h/1bc3a5b1de660e268b3a824b9bb23746/image-13.jpg)
- Slides: 31
Maryland Opioid Overdose Response Program Training for Potential Bystanders March 2015 Baltimore City Behavioral Health Administration Department of Health & Mental Hygiene dhmh. naloxone@maryland. gov
Program Overview I. Understanding Opioids II. Recognizing an Opioid Overdose (OD) III. Responding to an Opioid OD IV. Preventing Opioid OD V. Information & Resources VI. Receive Certificate and Kit 2
Overdose Deaths • Overdose deaths have increased nationwide. • In Baltimore City, most overdose deaths involve an opioid (like prescription pain medications or heroin). • Naloxone (Narcan) is a medicine that can reverse an opioid overdose. 3/1/2021 Maryland ORP Core Curriculum 3
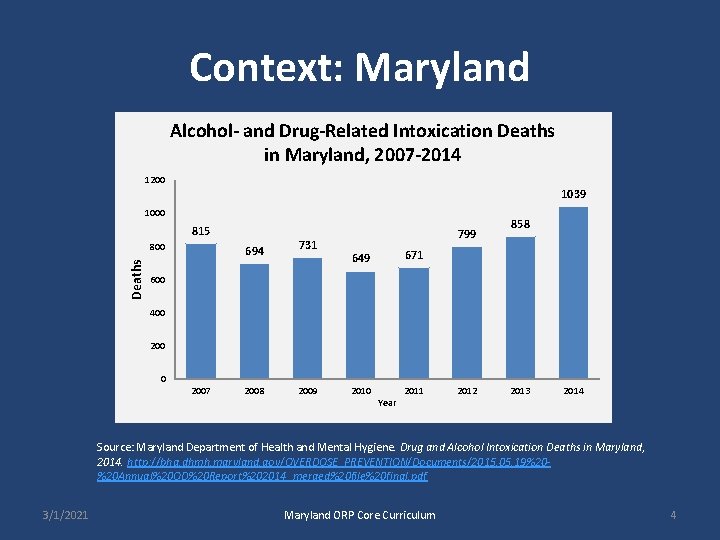
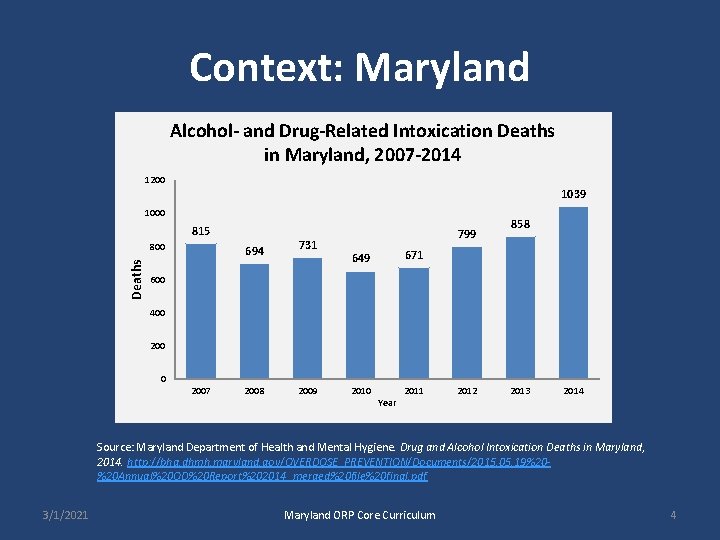
Context: Maryland Alcohol- and Drug-Related Intoxication Deaths in Maryland, 2007 -2014 1200 1039 1000 815 Deaths 800 694 731 799 858 671 649 600 400 2007 2008 2009 2010 Year 2011 2012 2013 2014 Source: Maryland Department of Health and Mental Hygiene. Drug and Alcohol Intoxication Deaths in Maryland, 2014. http: //bha. dhmh. maryland. gov/OVERDOSE_PREVENTION/Documents/2015. 05. 19%20%20 Annual%20 OD%20 Report%202014_merged%20 file%20 final. pdf 3/1/2021 Maryland ORP Core Curriculum 4
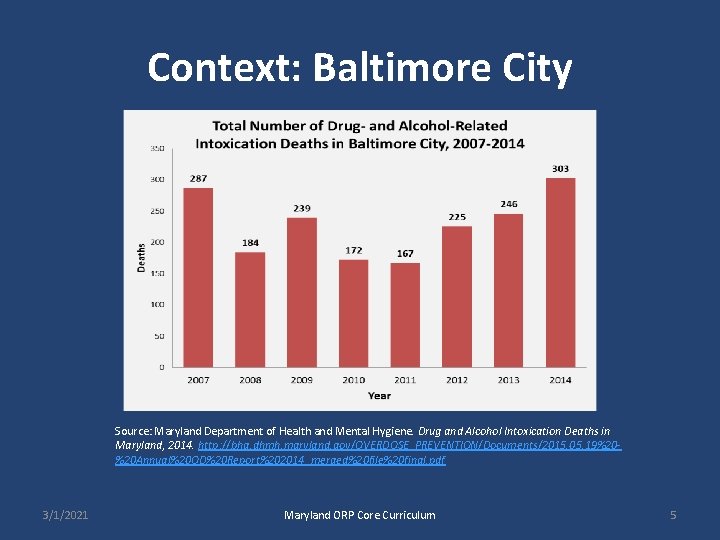
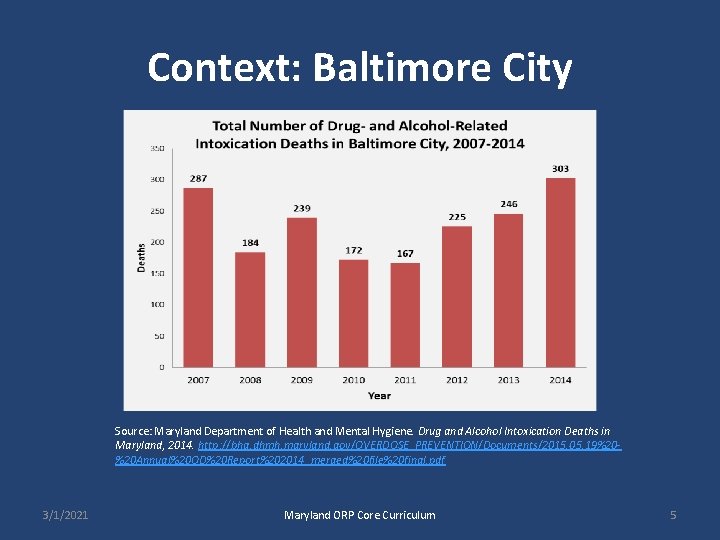
Context: Baltimore City Source: Maryland Department of Health and Mental Hygiene. Drug and Alcohol Intoxication Deaths in Maryland, 2014. http: //bha. dhmh. maryland. gov/OVERDOSE_PREVENTION/Documents/2015. 05. 19%20%20 Annual%20 OD%20 Report%202014_merged%20 file%20 final. pdf 3/1/2021 Maryland ORP Core Curriculum 5
What is an Opioid? 6
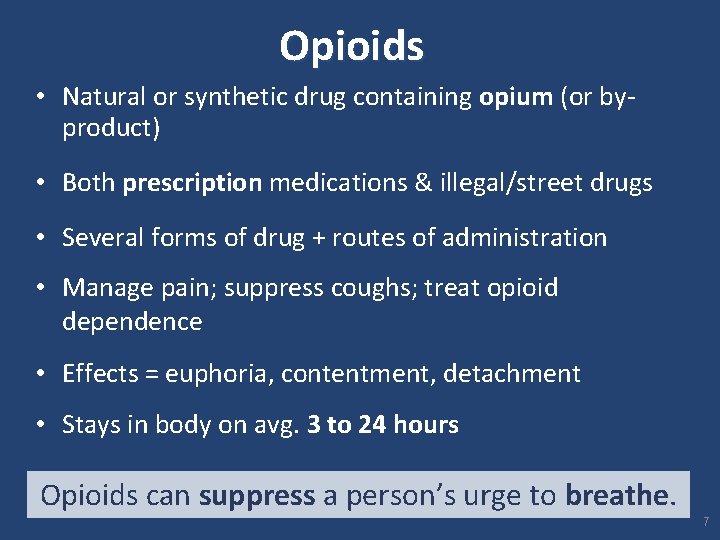
Opioids • Natural or synthetic drug containing opium (or by- product) • Both prescription medications & illegal/street drugs • Several forms of drug + routes of administration • Manage pain; suppress coughs; treat opioid dependence • Effects = euphoria, contentment, detachment • Stays in body on avg. 3 to 24 hours Opioids can suppress a person’s urge to breathe. 7
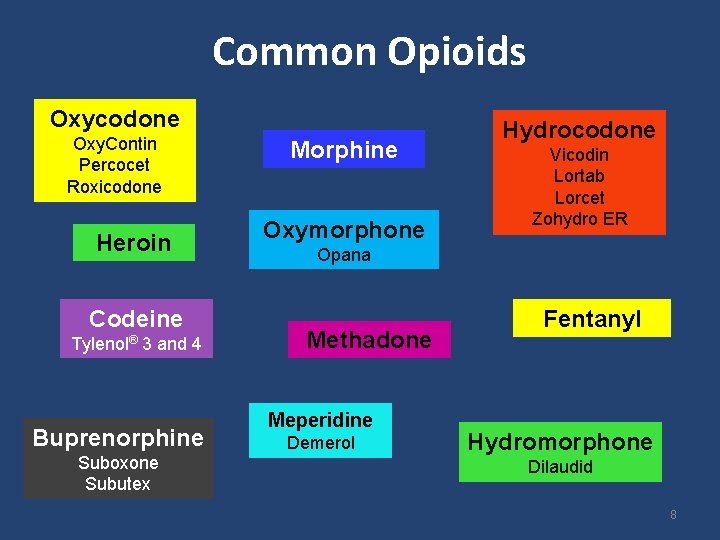
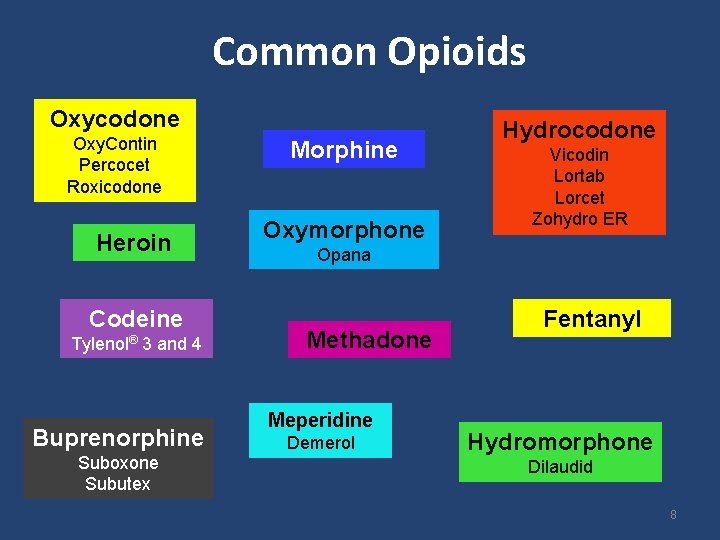
Common Opioids Oxycodone Oxy. Contin Percocet Roxicodone Heroin Codeine Tylenol® 3 and 4 Buprenorphine Suboxone Subutex Morphine Oxymorphone Hydrocodone Vicodin Lortab Lorcet Zohydro ER Opana Methadone Meperidine Demerol Fentanyl Hydromorphone Dilaudid 8
Recognizing an Opioid Overdose 9
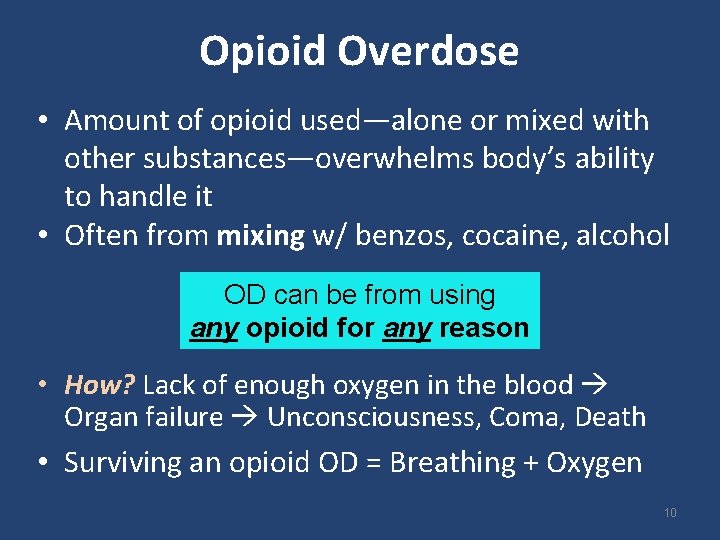
Opioid Overdose • Amount of opioid used—alone or mixed with other substances—overwhelms body’s ability to handle it • Often from mixing w/ benzos, cocaine, alcohol OD can be from using any opioid for any reason • How? Lack of enough oxygen in the blood Organ failure Unconsciousness, Coma, Death • Surviving an opioid OD = Breathing + Oxygen 10

Signs & Symptoms of Opioid OD § § § § Loud snoring or gurgling noises Body very limp Not responsive Skin pale/gray, clammy Lips/fingertips turn blue or gray Pulse slow or erratic Breathing very slow, shallow, or not at all Unconscious Maryland ORP Core Curriculum 11
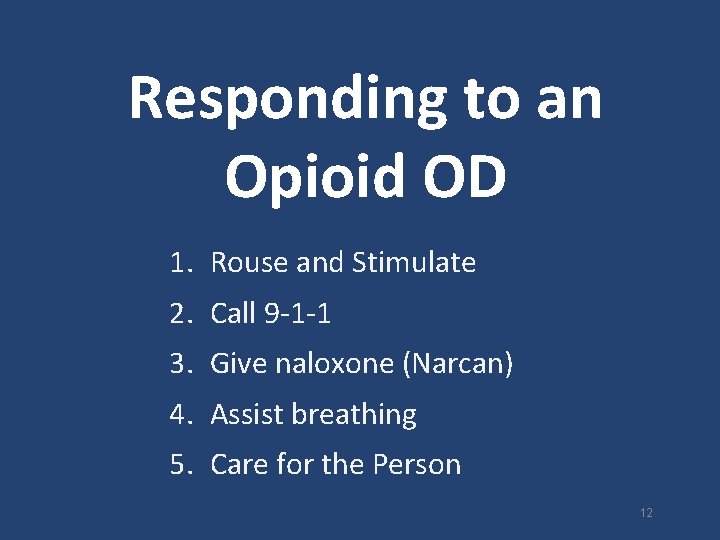
Responding to an Opioid OD 1. Rouse and Stimulate 2. Call 9 -1 -1 3. Give naloxone (Narcan) 4. Assist breathing 5. Care for the Person 12
![Step 1 Rouse Stimulate Noise Shake persons shoulders and yell Name Are you Step 1: Rouse & Stimulate Noise: Shake person’s shoulders and yell: “[Name!] Are you](https://slidetodoc.com/presentation_image_h/1bc3a5b1de660e268b3a824b9bb23746/image-13.jpg)
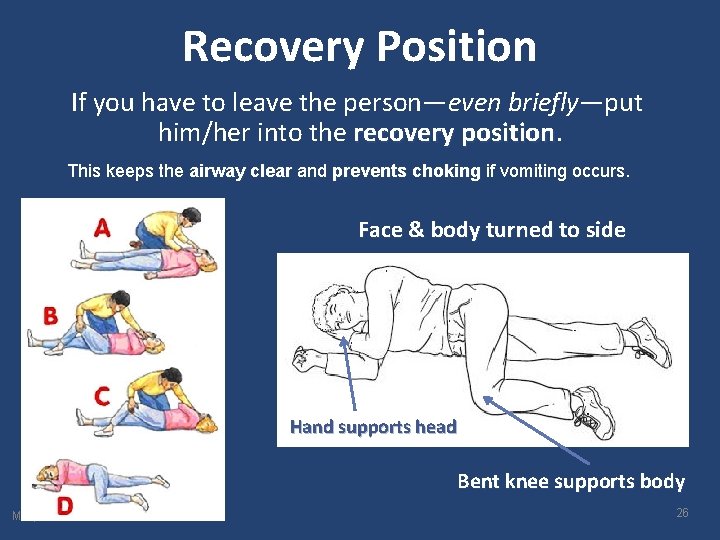
Step 1: Rouse & Stimulate Noise: Shake person’s shoulders and yell: “[Name!] Are you all right? Wake up!” Pain: If no answer, do a sternal (sternum) rub: rub Make a fist, rub your knuckles firmly up and down the breast bone. 13
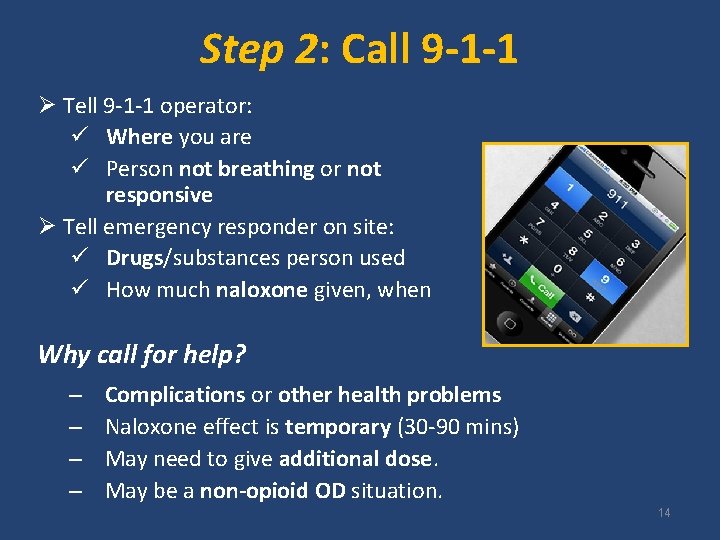
Step 2: Call 9 -1 -1 Ø Tell 9 -1 -1 operator: ü Where you are ü Person not breathing or not responsive Ø Tell emergency responder on site: ü Drugs/substances person used ü How much naloxone given, when Why call for help? – – Complications or other health problems Naloxone effect is temporary (30 -90 mins) May need to give additional dose. May be a non-opioid OD situation. 14
Good Samaritan Law Gives you some legal protections if you seek and/or provide medical assistance (i. e. Call 911) for someone experiencing an OD: • Immunity from arrest for certain minor crimes*, if the evidence was obtained solely as a result of your actions in trying to aid the victim. • Immunity extends to OD victim *Drug-related misdemeanors only *Does protect against felonies or loss of other benefits (e. g. financial aid, immigration) 15
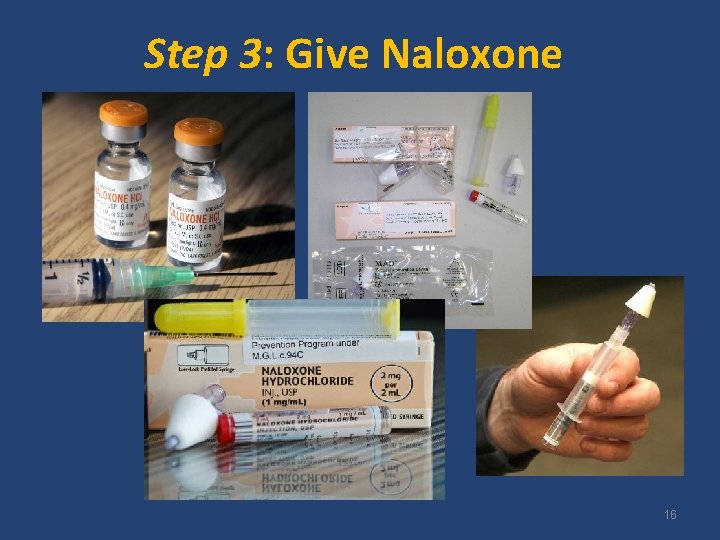
Step 3: Give Naloxone 16
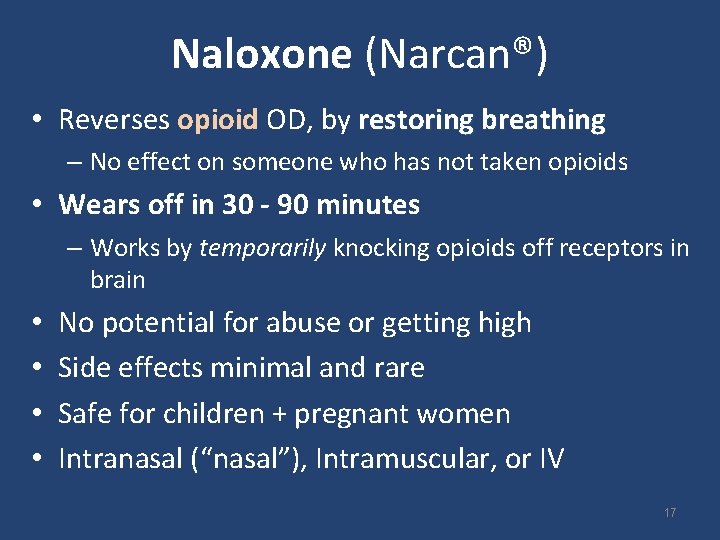
Naloxone (Narcan®) • Reverses opioid OD, by restoring breathing – No effect on someone who has not taken opioids • Wears off in 30 - 90 minutes – Works by temporarily knocking opioids off receptors in brain • • No potential for abuse or getting high Side effects minimal and rare Safe for children + pregnant women Intranasal (“nasal”), Intramuscular, or IV 17
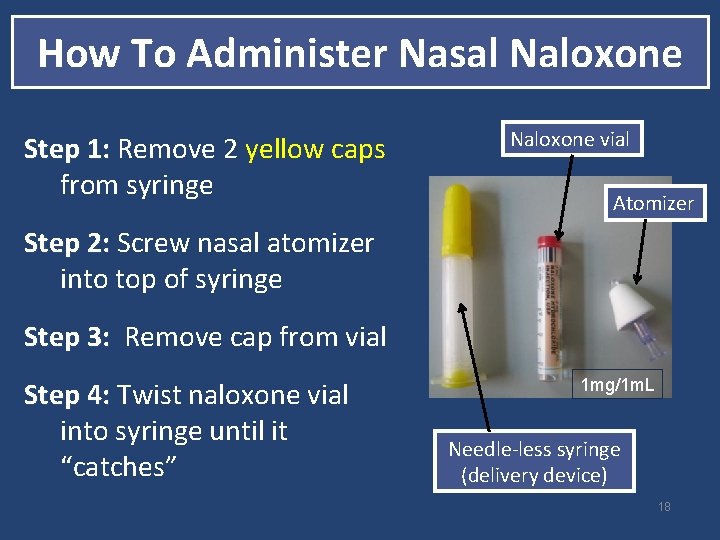
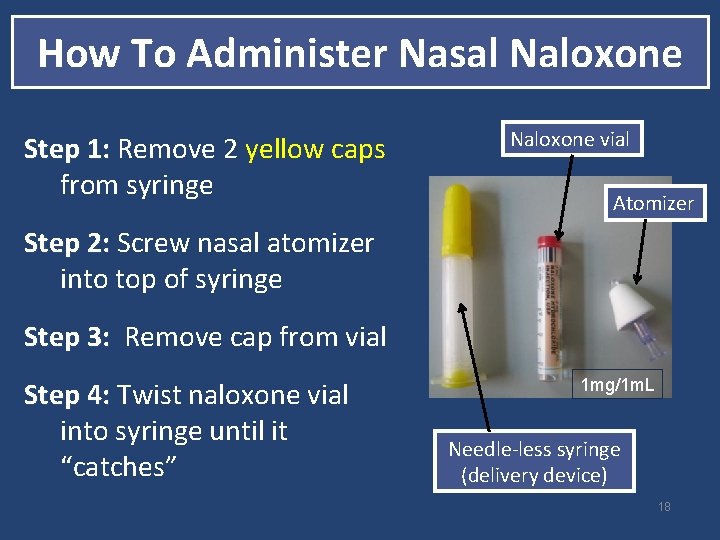
How To Administer Nasal Naloxone Step 1: Remove 2 yellow caps 1: from syringe Naloxone vial Atomizer Step 2: Screw nasal atomizer 2: into top of syringe Step 3: Remove cap from vial 3: Step 4: Twist naloxone vial into syringe until it “catches” 1 mg/1 m. L Needle-less syringe (delivery device) 18
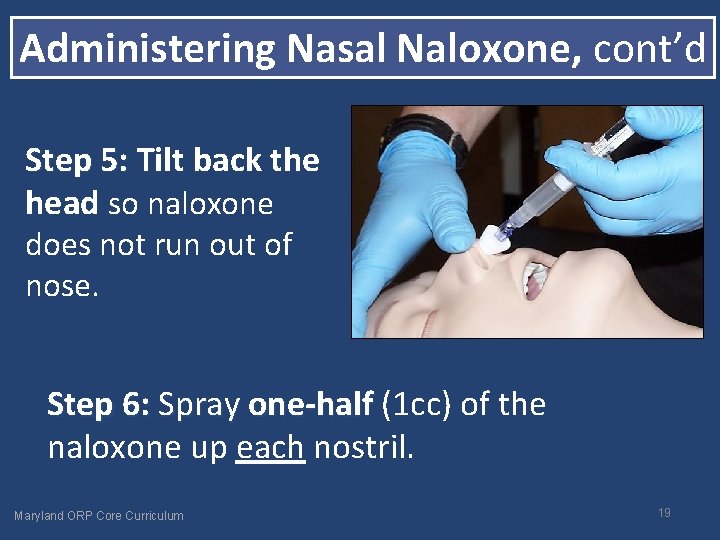
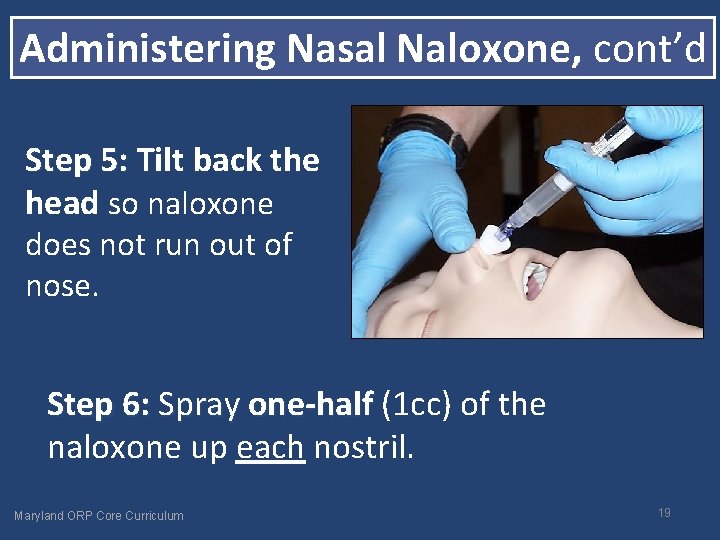
Administering Nasal Naloxone, cont’d Step 5: Tilt back the head so naloxone does not run out of nose. Step 6: Spray one-half (1 cc) of the naloxone up each nostril. Maryland ORP Core Curriculum 19
Administering Nasal Naloxone, cont’d Step 7: Begin rescue breathing while you allow 13 minutes for naloxone to work. Step 8: If no breathing after 2 -3 minutes, give a 8: second dose of naloxone. of Step 9: Continue rescue breaths until person wakes up or EMS arrives. 20
If no naloxone or waiting for it to work… Step 4: Rescue Breathing If person not breathing, or breath is shallow or short, Ø Give rescue breaths right away and/or Ø Follow 9 -1 -1 dispatcher’s instructions Continue breaths until person wakes up or medical help arrives. Rescue breathing is the quickest way to get oxygen into the body. 21
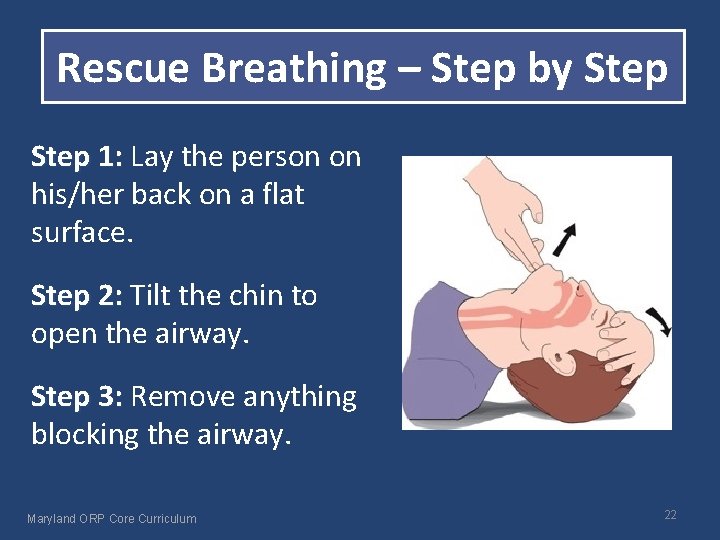
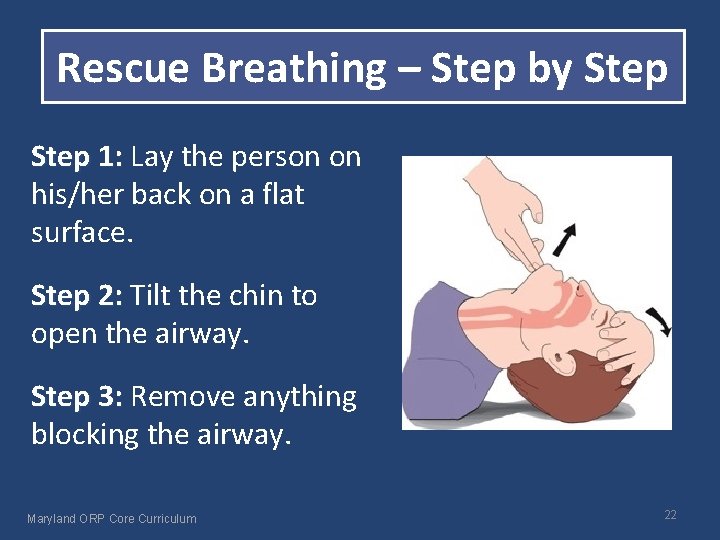
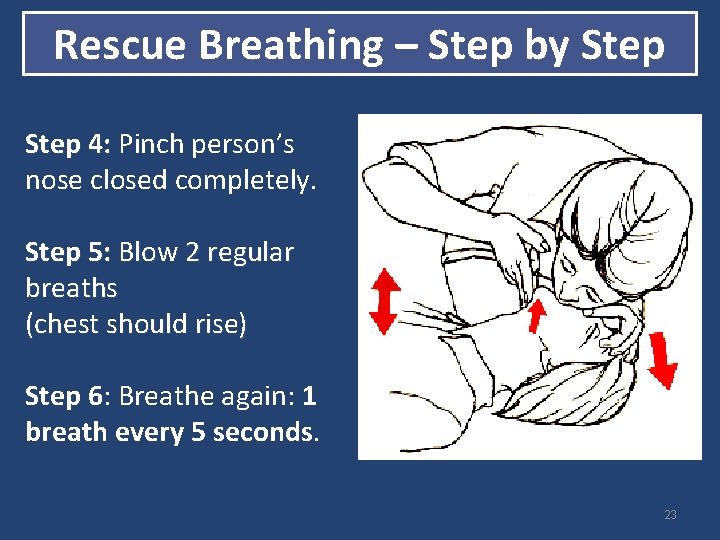
Rescue Breathing – Step by Step 1: Lay the person on 1: his/her back on a flat surface. Step 2: Tilt the chin to 2: open the airway. Step 3: Remove anything 3: blocking the airway. Maryland ORP Core Curriculum 22
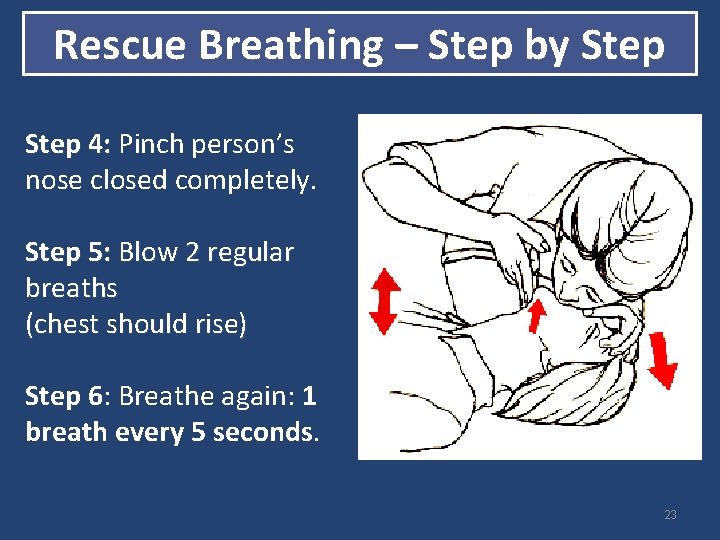
Rescue Breathing – Step by Step 4: Pinch person’s nose closed completely. Step 5: Blow 2 regular breaths (chest should rise) Step 6: Breathe again: 1 breath every 5 seconds. 23
Step 5: Care for the Person • Stay until medical help arrives • If breathing, put person in recovery position • After receiving naloxone, person may experience unpleasant withdrawal symptoms (not life-threatening) • Encourage person not to take more opioids for a while. • If overdose re-occurs, give another dose 24
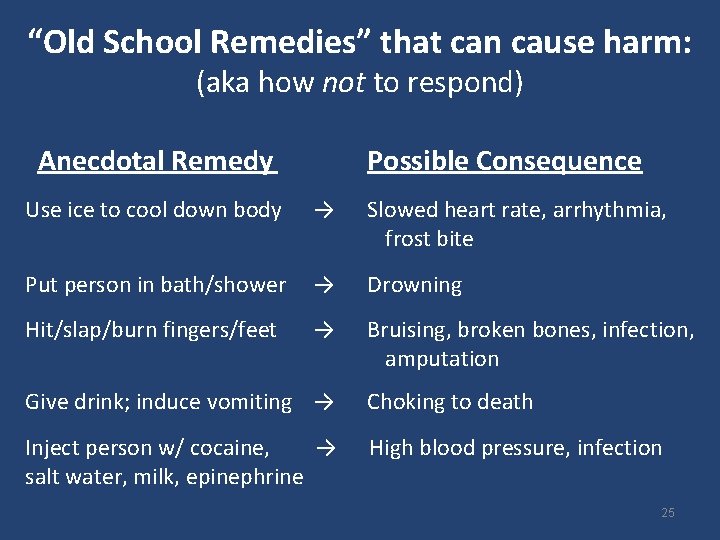
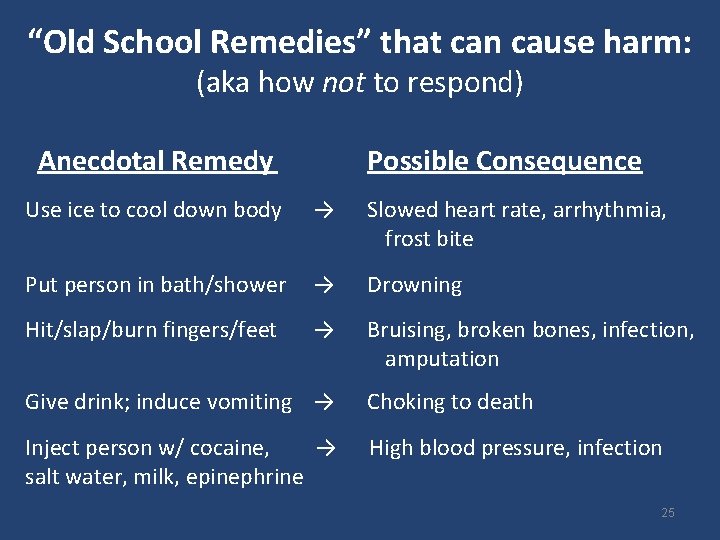
“Old School Remedies” that can cause harm: (aka how not to respond) Anecdotal Remedy Possible Consequence Use ice to cool down body → Slowed heart rate, arrhythmia, frost bite Put person in bath/shower → Drowning Hit/slap/burn fingers/feet → Bruising, broken bones, infection, amputation Give drink; induce vomiting → Choking to death Inject person w/ cocaine, → High blood pressure, infection salt water, milk, epinephrine 25
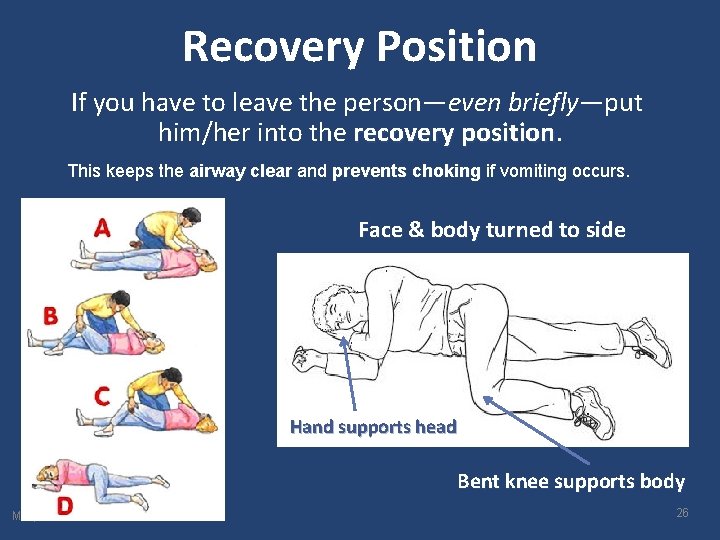
Recovery Position If you have to leave the person—even briefly—put him/her into the recovery position This keeps the airway clear and prevents choking if vomiting occurs. Face & body turned to side Hand supports head Bent knee supports body Maryland ORP Core Curriculum 26
Used your naloxone to save a life? Call the MD Poison Center: 1 -800 -222 -1222 and contact training entity that issued certificate *all info will be kept confidential* 27
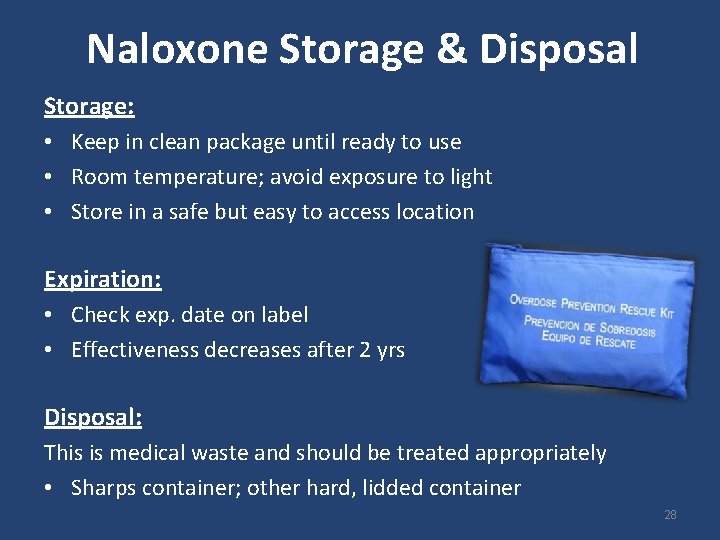
Naloxone Storage & Disposal Storage: • Keep in clean package until ready to use • Room temperature; avoid exposure to light • Store in a safe but easy to access location Expiration: • Check exp. date on label • Effectiveness decreases after 2 yrs Disposal: This is medical waste and should be treated appropriately • Sharps container; other hard, lidded container 28
Preventing Opioid OD v Use with someone else v If you have not used in a couple days or more, use less opioids than you normally would. Greatest risk for OD after abstinence! v Create overdose prevention plan share plan w/ someone to give you Narcan if needed v Be extra careful if you have breathing problems (asthma; sleep apnea) v Try not to mix with other substances • Ask doctor or pharmacist about potential interactions v Seek treatment for substance use issues, if willing. v Always keep naloxone on hand. 29
Information & Resources • Today you will receive a certificate and a prescription for naloxone – A certificate ≠ a prescription • Certificate expires after 2 years – Keep certificate in a safe place. It provides legal protections. • For another free kit: – 410 396 -3731 (Baltimore City Health Dept. : Staying Alive) – 410 -637 -1900 (Behavioral Health System Baltimore [BHSB]) • Can fill script for naloxone at any pharmacy • Can take certificate to a doctor or NP for another prescription • More resources in handout 30
What We Learned I. What are Opioids II. What is an Opioid OD III. How to Respond to Opioid OD - 5 steps IV. Tips to Prevent Opioid OD V. Information & Resources 3 1