Martinis Visual Anatomy and Physiology First Edition Martini
![Liver [ Hepat(o)- ] Round ligament is part of the falciform ligament that divides Liver [ Hepat(o)- ] Round ligament is part of the falciform ligament that divides](https://slidetodoc.com/presentation_image/fcee1992ed36d085115073b7e2a0199f/image-3.jpg)
![Gallbladder [Cyst(o)-] Figure from: Martini, Anatomy & Physiology, Prentice Hall, 2001 Main function is Gallbladder [Cyst(o)-] Figure from: Martini, Anatomy & Physiology, Prentice Hall, 2001 Main function is](https://slidetodoc.com/presentation_image/fcee1992ed36d085115073b7e2a0199f/image-8.jpg)
- Slides: 34
Martini’s Visual Anatomy and Physiology First Edition Martini w Ober Chapter 21 Digestive System III Lecture 9 1
Lecture Overview • Liver • Gall Bladder • Small Intestine • Large Intestine 2
![Liver Hepato Round ligament is part of the falciform ligament that divides Liver [ Hepat(o)- ] Round ligament is part of the falciform ligament that divides](https://slidetodoc.com/presentation_image/fcee1992ed36d085115073b7e2a0199f/image-3.jpg)
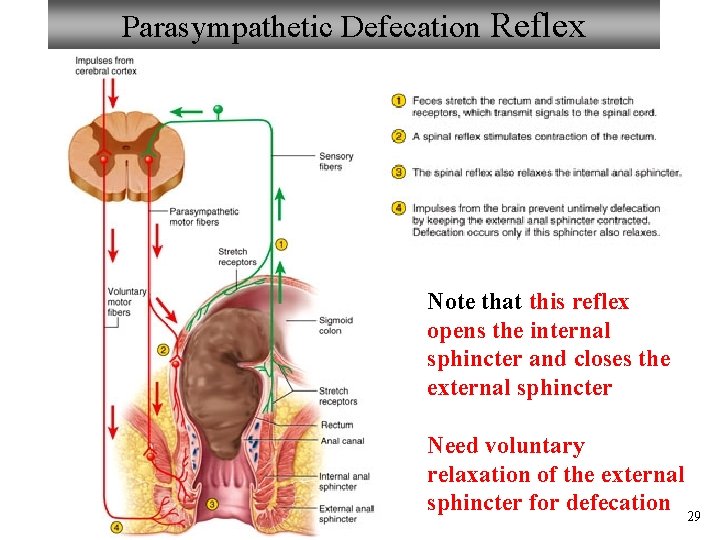
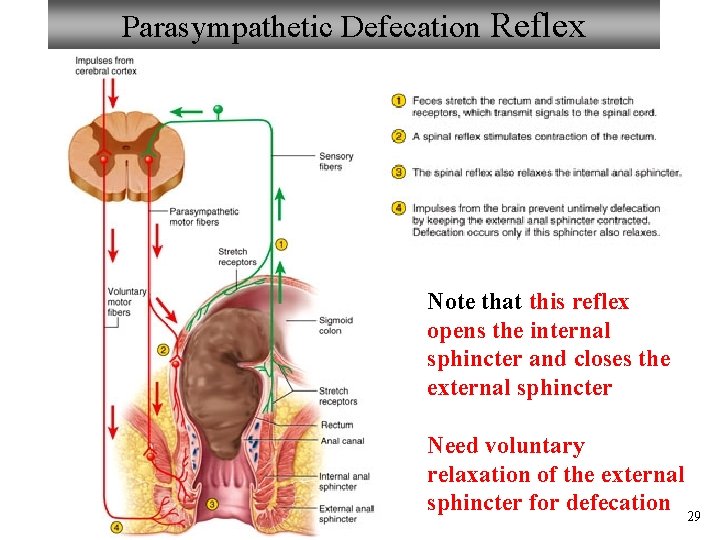
Liver [ Hepat(o)- ] Round ligament is part of the falciform ligament that divides the lobes; remnant of fetal umbilical vein. Note that the vena cava does not enter the liver; it passes by Figure from: Martini, Anatomy & Physiology, Pearson Education, 2004 3
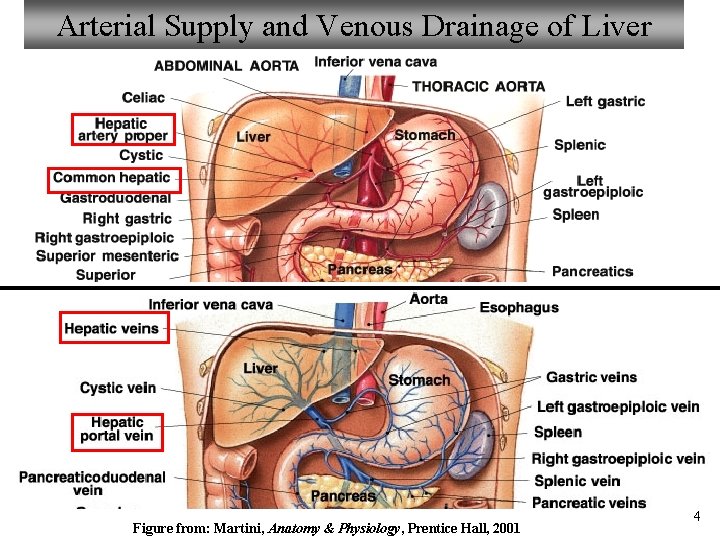
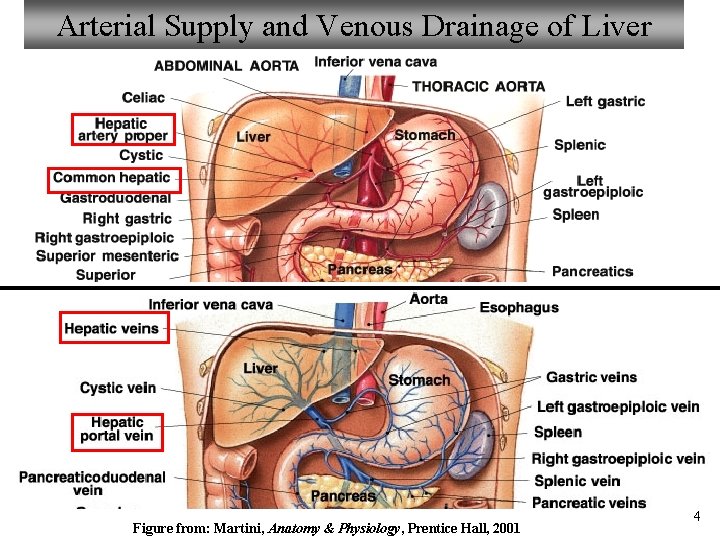
Arterial Supply and Venous Drainage of Liver Figure from: Martini, Anatomy & Physiology, Prentice Hall, 2001 4
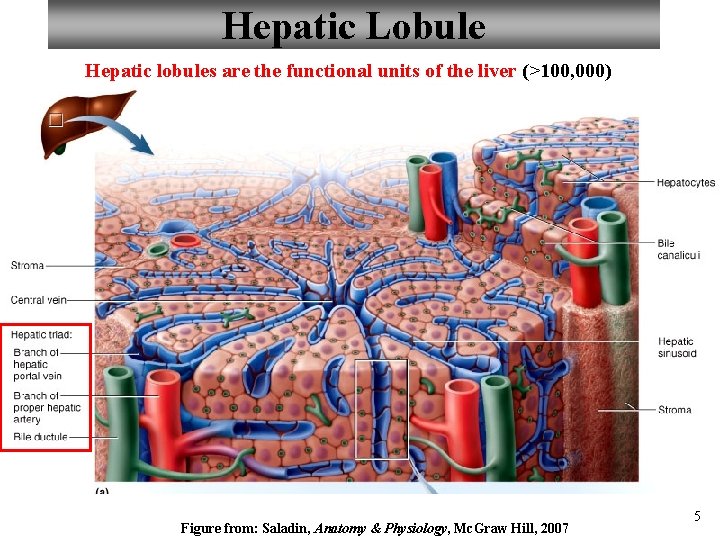
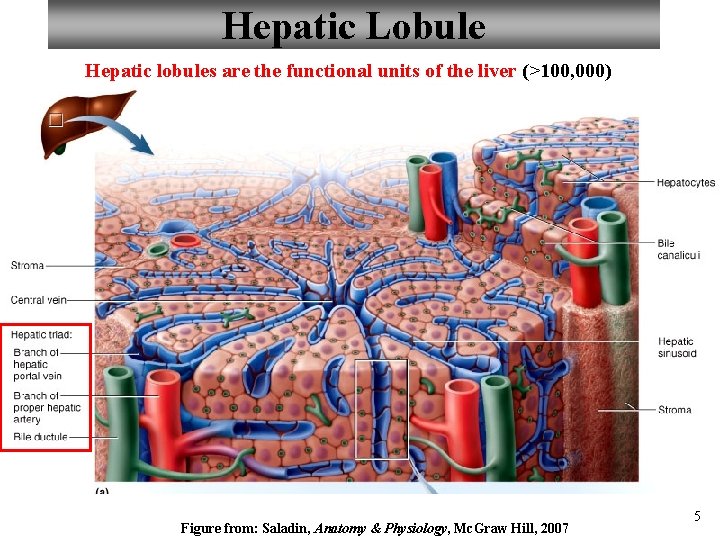
Hepatic Lobule Hepatic lobules are the functional units of the liver (>100, 000) Figure from: Saladin, Anatomy & Physiology, Mc. Graw Hill, 2007 5
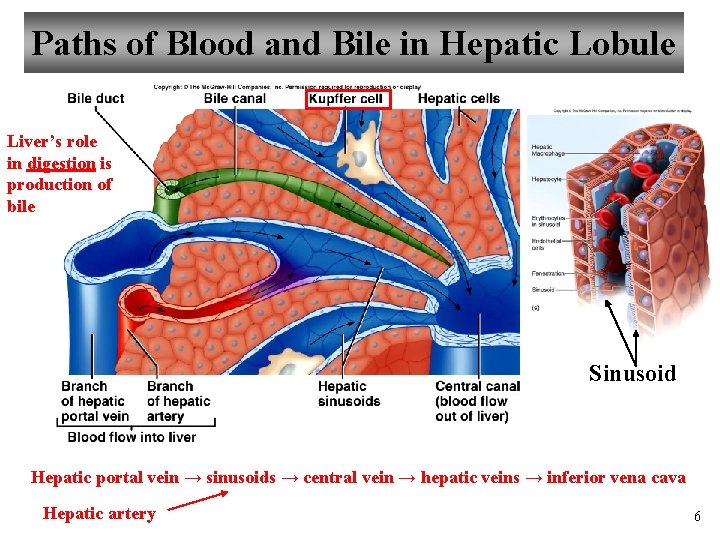
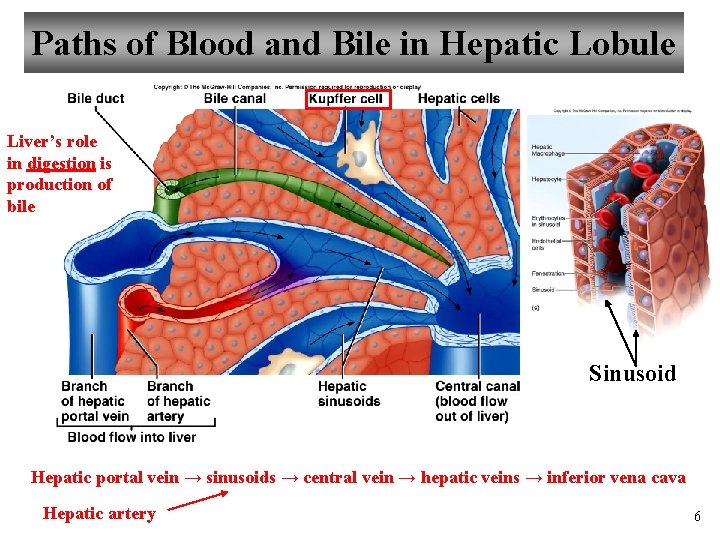
Paths of Blood and Bile in Hepatic Lobule Liver’s role in digestion is production of bile Sinusoid Hepatic portal vein → sinusoids → central vein → hepatic veins → inferior vena cava Hepatic artery 6
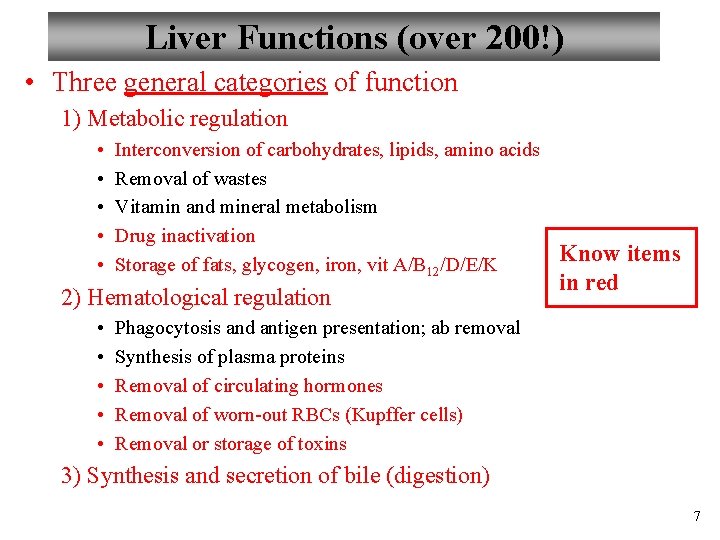
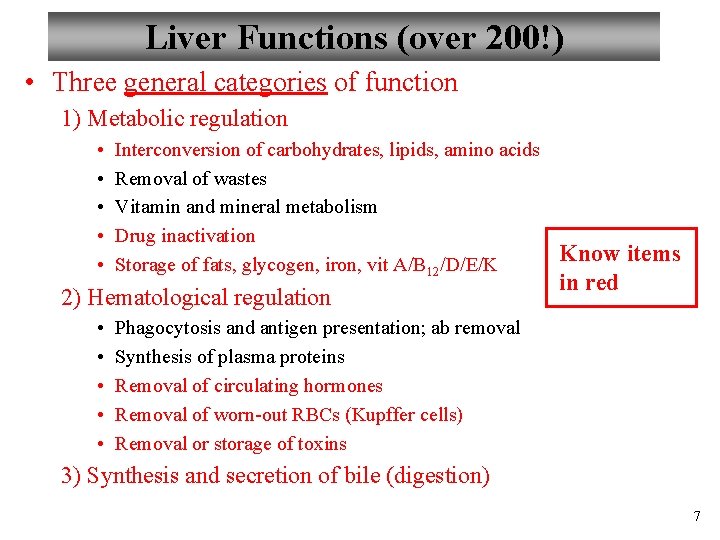
Liver Functions (over 200!) • Three general categories of function 1) Metabolic regulation • • • Interconversion of carbohydrates, lipids, amino acids Removal of wastes Vitamin and mineral metabolism Drug inactivation Storage of fats, glycogen, iron, vit A/B 12/D/E/K 2) Hematological regulation • • • Know items in red Phagocytosis and antigen presentation; ab removal Synthesis of plasma proteins Removal of circulating hormones Removal of worn-out RBCs (Kupffer cells) Removal or storage of toxins 3) Synthesis and secretion of bile (digestion) 7
![Gallbladder Cysto Figure from Martini Anatomy Physiology Prentice Hall 2001 Main function is Gallbladder [Cyst(o)-] Figure from: Martini, Anatomy & Physiology, Prentice Hall, 2001 Main function is](https://slidetodoc.com/presentation_image/fcee1992ed36d085115073b7e2a0199f/image-8.jpg)
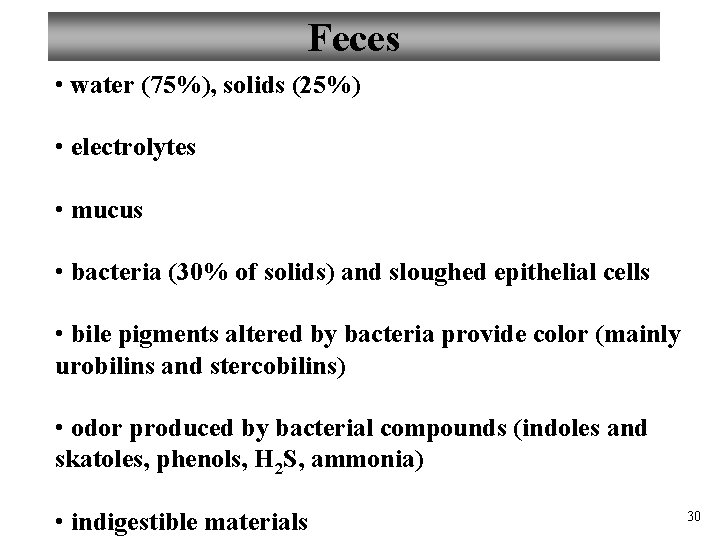
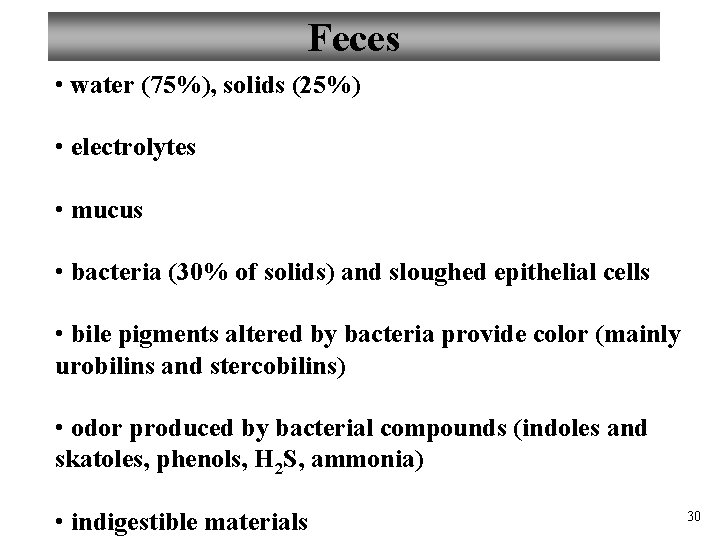
Gallbladder [Cyst(o)-] Figure from: Martini, Anatomy & Physiology, Prentice Hall, 2001 Main function is to store and concentrate bile between meals, and release bile under the influence of CCK 9
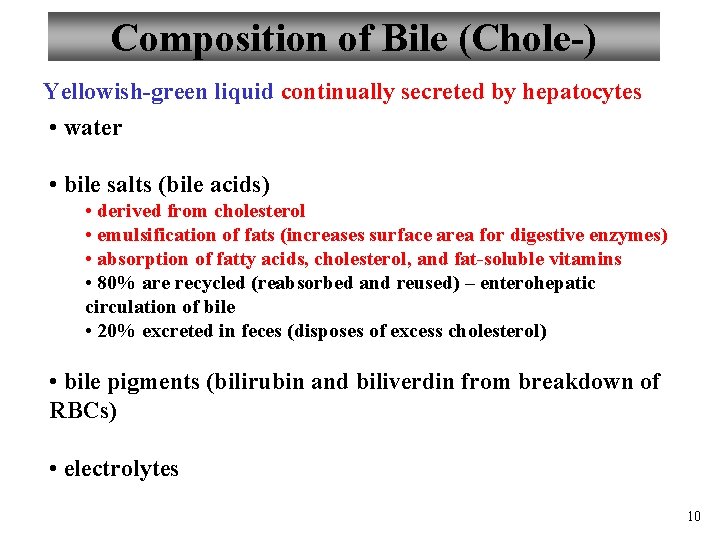
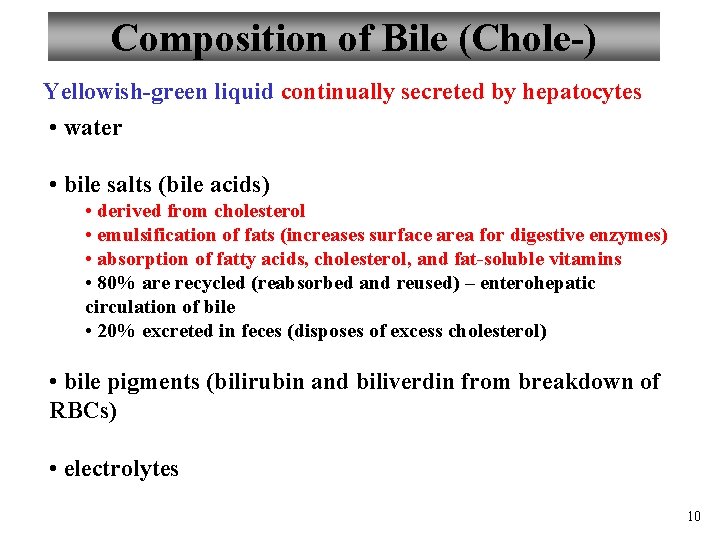
Composition of Bile (Chole-) Yellowish-green liquid continually secreted by hepatocytes • water • bile salts (bile acids) • derived from cholesterol • emulsification of fats (increases surface area for digestive enzymes) • absorption of fatty acids, cholesterol, and fat-soluble vitamins • 80% are recycled (reabsorbed and reused) – enterohepatic circulation of bile • 20% excreted in feces (disposes of excess cholesterol) • bile pigments (bilirubin and biliverdin from breakdown of RBCs) • electrolytes 10
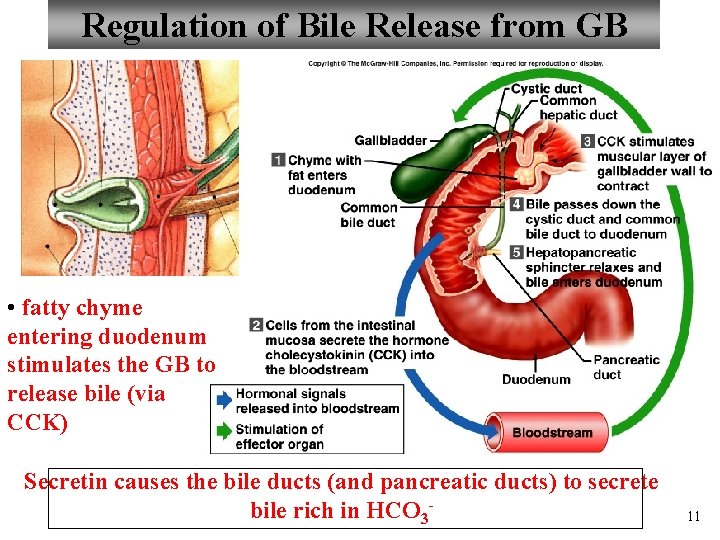
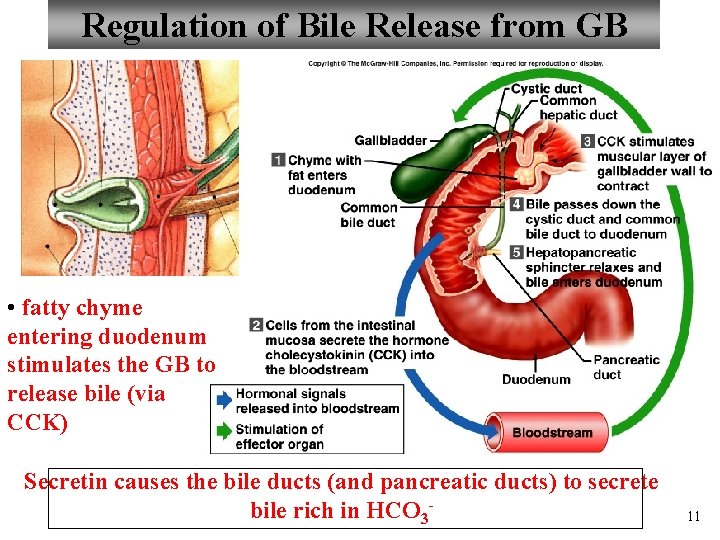
Regulation of Bile Release from GB • fatty chyme entering duodenum stimulates the GB to release bile (via CCK) Secretin causes the bile ducts (and pancreatic ducts) to secrete bile rich in HCO 3 - 11
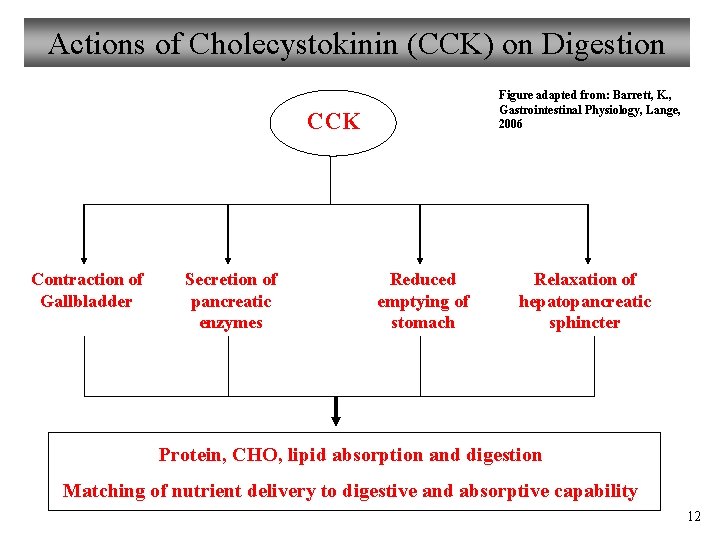
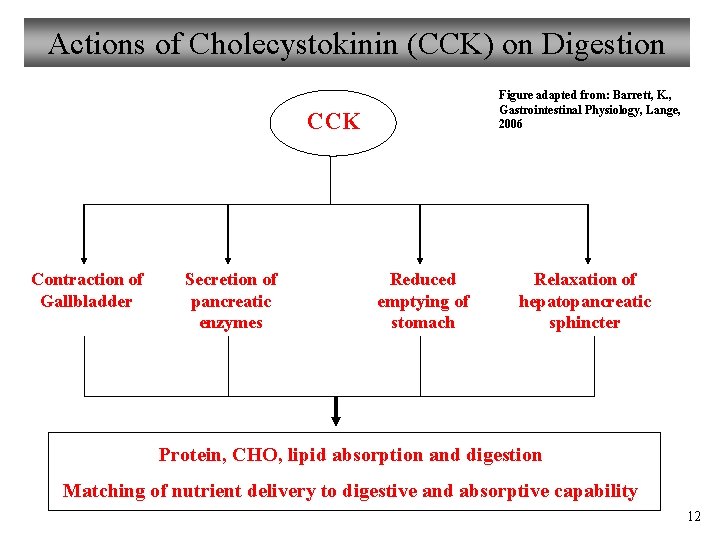
Actions of Cholecystokinin (CCK) on Digestion Figure adapted from: Barrett, K. , Gastrointestinal Physiology, Lange, 2006 CCK Contraction of Gallbladder Secretion of pancreatic enzymes Reduced emptying of stomach Relaxation of hepatopancreatic sphincter Protein, CHO, lipid absorption and digestion Matching of nutrient delivery to digestive and absorptive capability 12
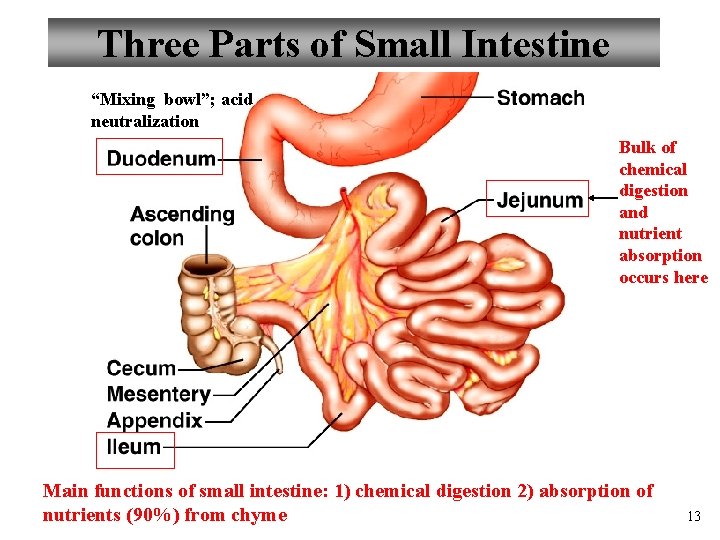
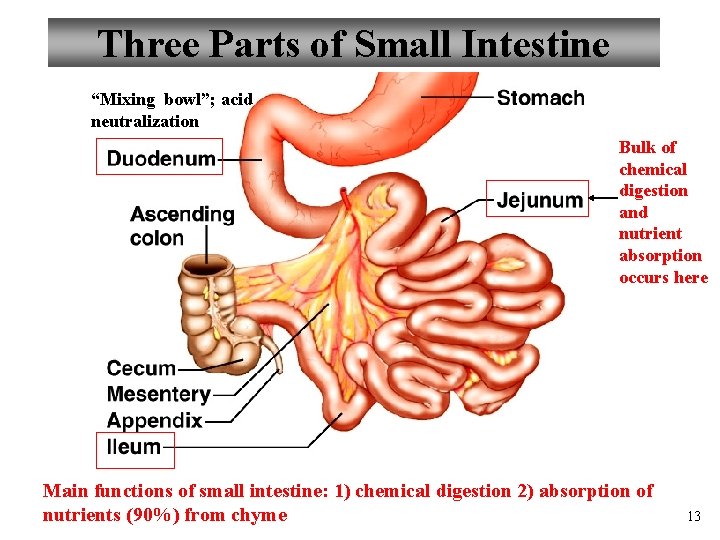
Three Parts of Small Intestine “Mixing bowl”; acid neutralization Bulk of chemical digestion and nutrient absorption occurs here Main functions of small intestine: 1) chemical digestion 2) absorption of nutrients (90%) from chyme 13
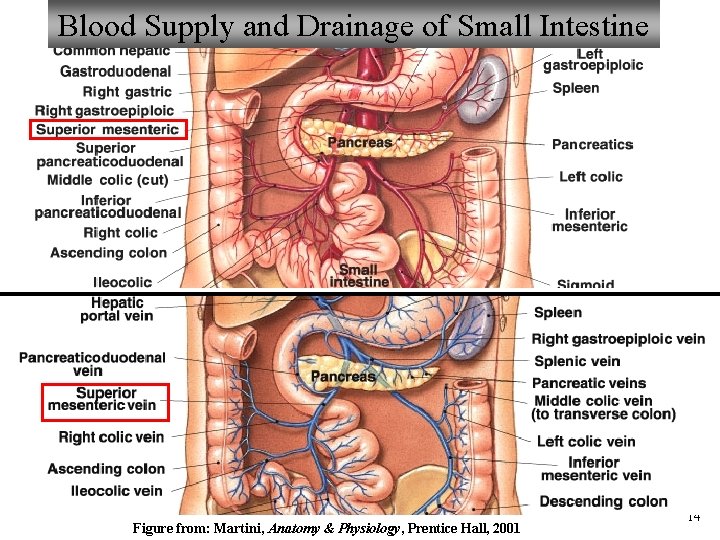
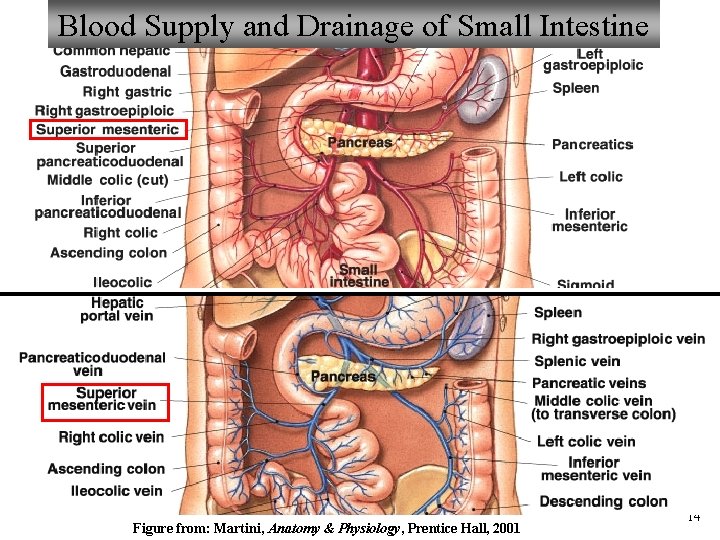
Blood Supply and Drainage of Small Intestine Figure from: Martini, Anatomy & Physiology, Prentice Hall, 2001 14
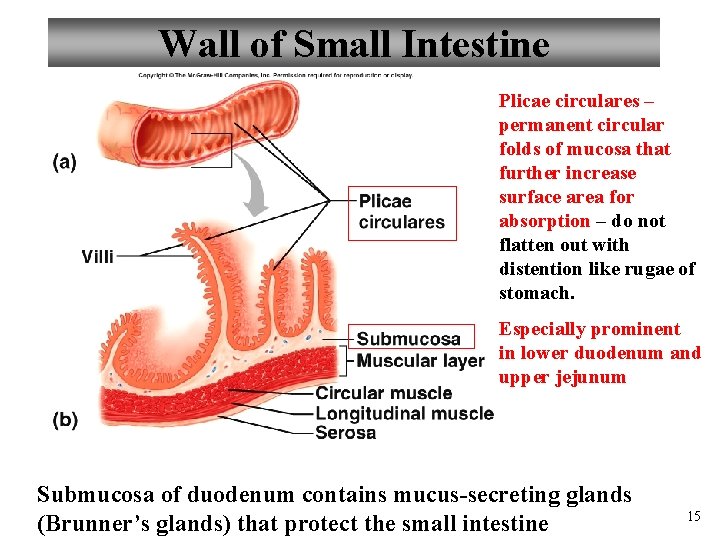
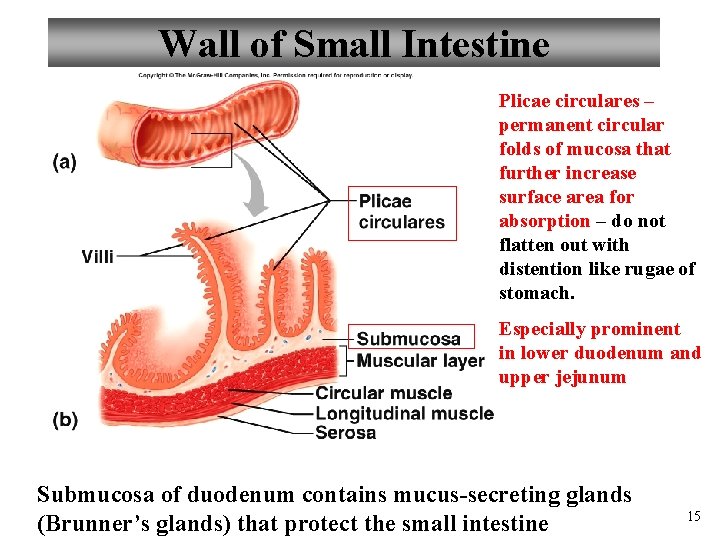
Wall of Small Intestine Plicae circulares – permanent circular folds of mucosa that further increase surface area for absorption – do not flatten out with distention like rugae of stomach. Especially prominent in lower duodenum and upper jejunum Submucosa of duodenum contains mucus-secreting glands (Brunner’s glands) that protect the small intestine 15
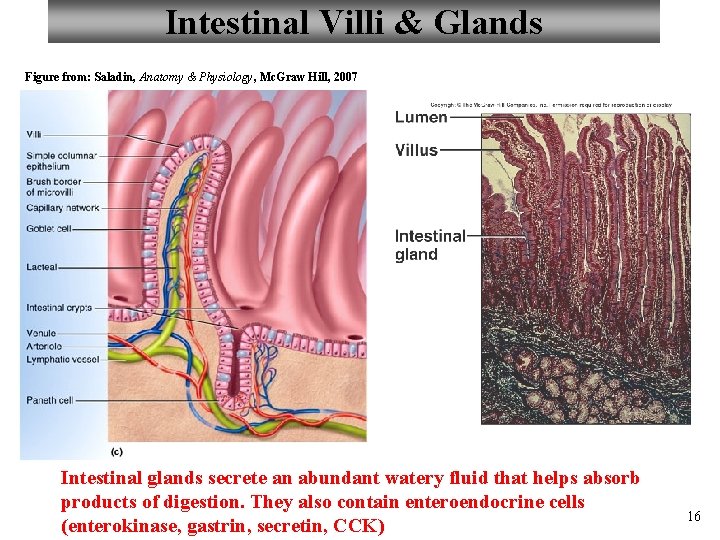
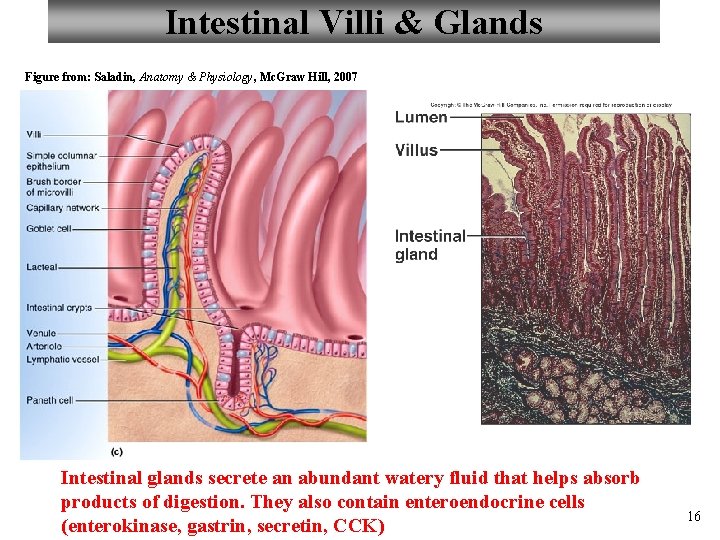
Intestinal Villi & Glands Figure from: Saladin, Anatomy & Physiology, Mc. Graw Hill, 2007 Intestinal glands secrete an abundant watery fluid that helps absorb products of digestion. They also contain enteroendocrine cells (enterokinase, gastrin, secretin, CCK) 16
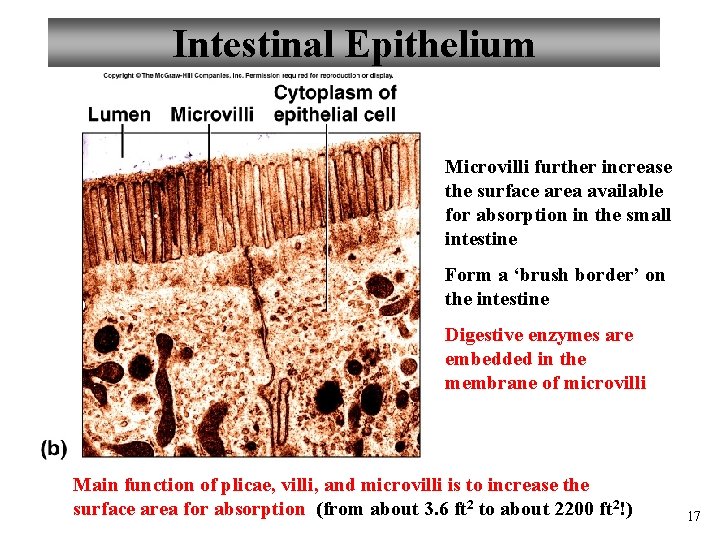
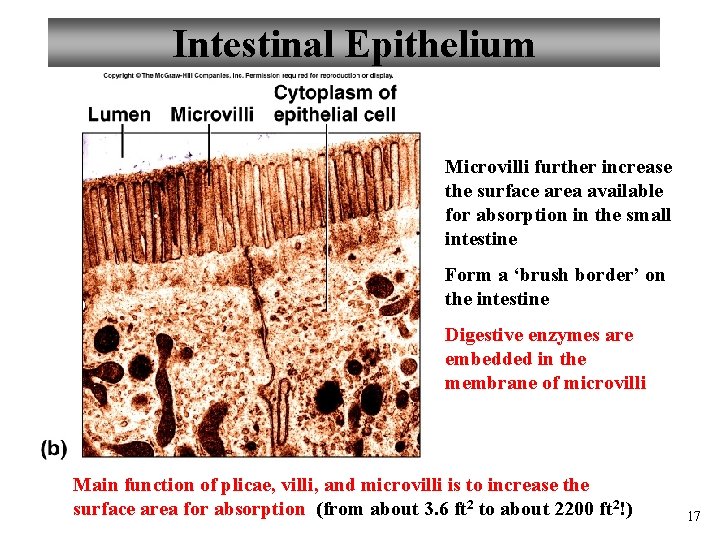
Intestinal Epithelium Microvilli further increase the surface area available for absorption in the small intestine Form a ‘brush border’ on the intestine Digestive enzymes are embedded in the membrane of microvilli Main function of plicae, villi, and microvilli is to increase the surface area for absorption (from about 3. 6 ft 2 to about 2200 ft 2!) 17
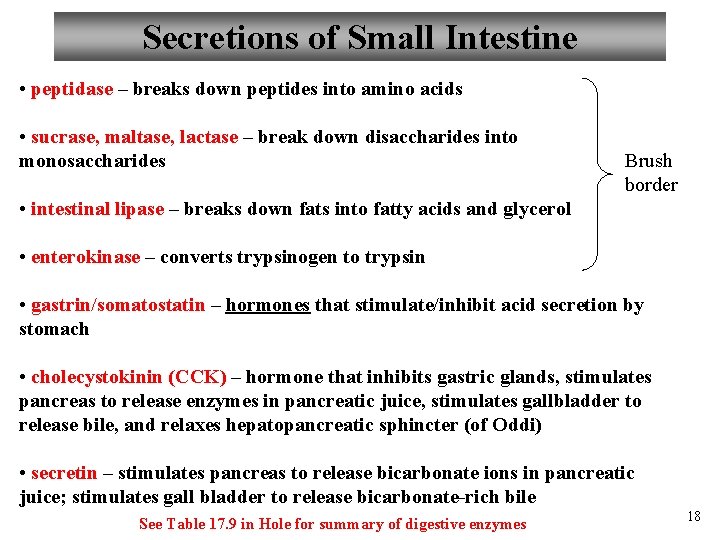
Secretions of Small Intestine • peptidase – breaks down peptides into amino acids • sucrase, maltase, lactase – break down disaccharides into monosaccharides Brush border • intestinal lipase – breaks down fats into fatty acids and glycerol • enterokinase – converts trypsinogen to trypsin • gastrin/somatostatin – hormones that stimulate/inhibit acid secretion by stomach • cholecystokinin (CCK) – hormone that inhibits gastric glands, stimulates pancreas to release enzymes in pancreatic juice, stimulates gallbladder to release bile, and relaxes hepatopancreatic sphincter (of Oddi) • secretin – stimulates pancreas to release bicarbonate ions in pancreatic juice; stimulates gall bladder to release bicarbonate-rich bile See Table 17. 9 in Hole for summary of digestive enzymes 18
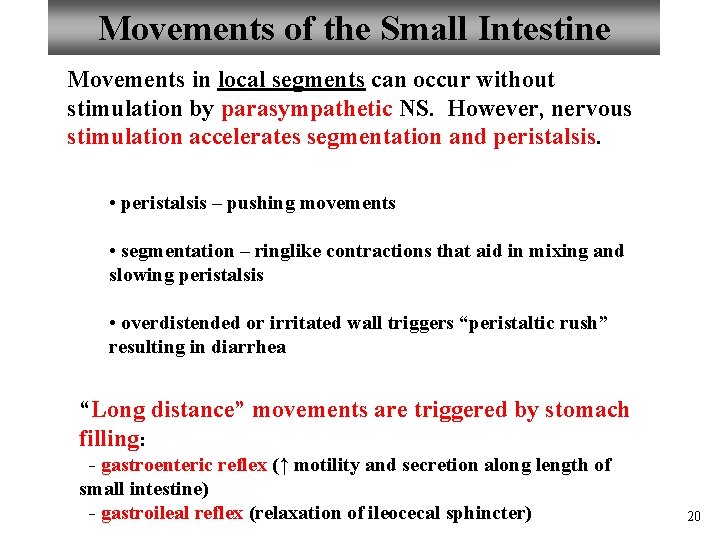
Movements of the Small Intestine Movements in local segments can occur without stimulation by parasympathetic NS. However, nervous stimulation accelerates segmentation and peristalsis. • peristalsis – pushing movements • segmentation – ringlike contractions that aid in mixing and slowing peristalsis • overdistended or irritated wall triggers “peristaltic rush” resulting in diarrhea “Long distance” movements are triggered by stomach filling: - gastroenteric reflex (↑ motility and secretion along length of small intestine) - gastroileal reflex (relaxation of ileocecal sphincter) 20
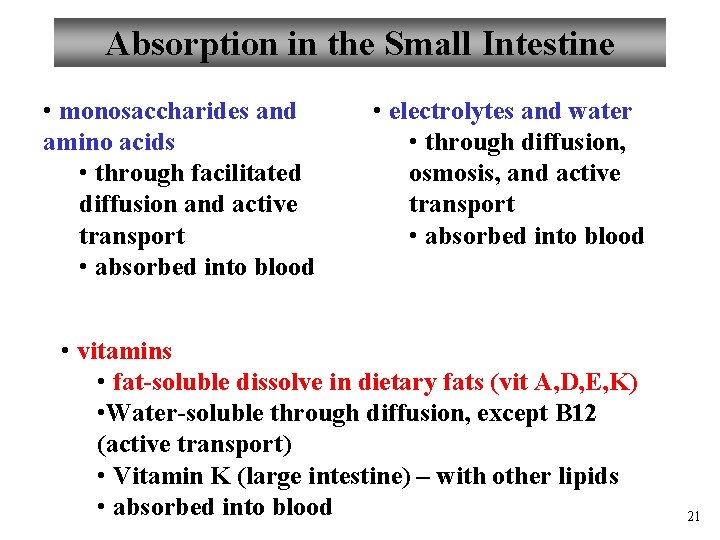
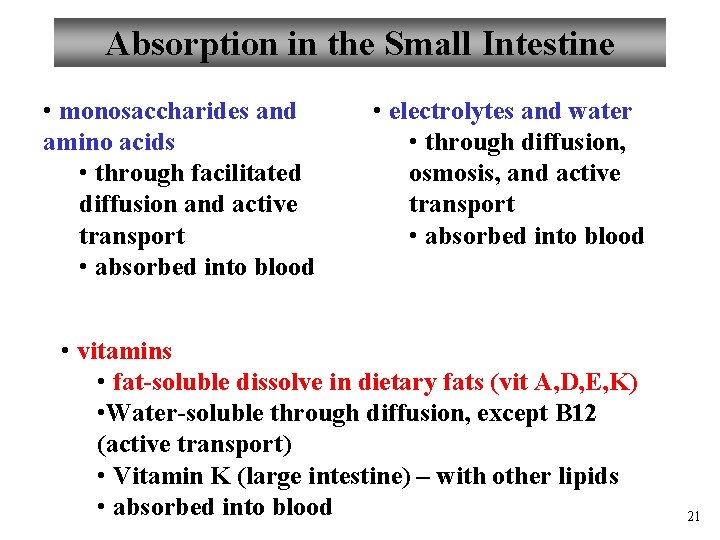
Absorption in the Small Intestine • monosaccharides and amino acids • through facilitated diffusion and active transport • absorbed into blood • electrolytes and water • through diffusion, osmosis, and active transport • absorbed into blood • vitamins • fat-soluble dissolve in dietary fats (vit A, D, E, K) • Water-soluble through diffusion, except B 12 (active transport) • Vitamin K (large intestine) – with other lipids • absorbed into blood 21
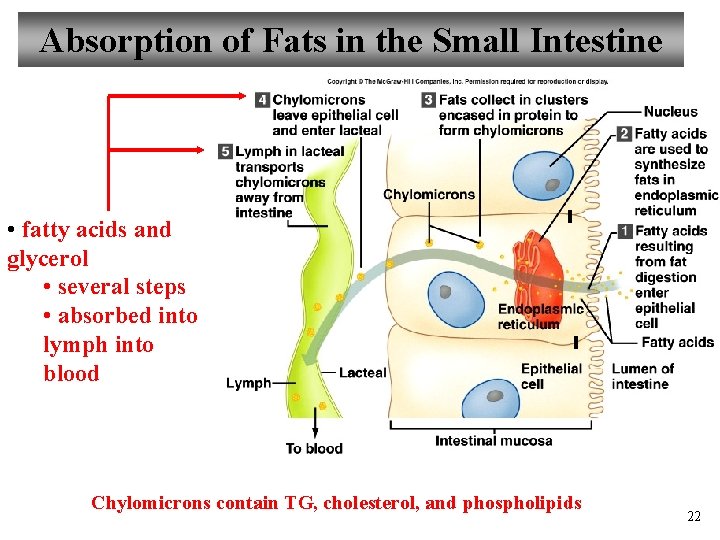
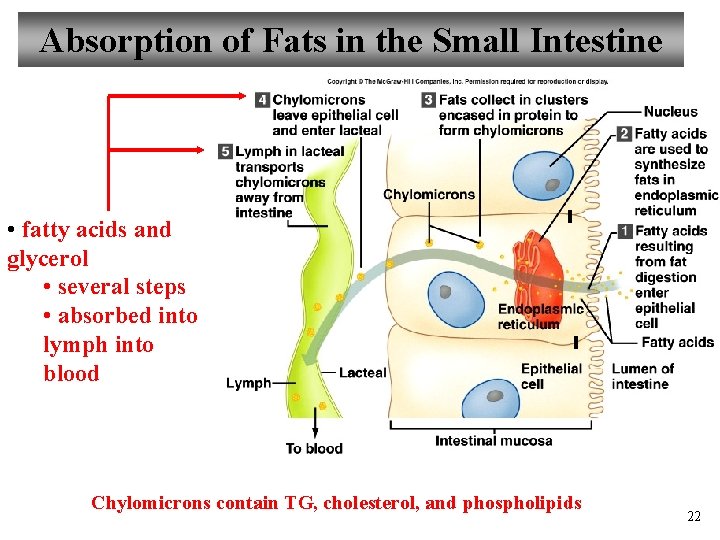
Absorption of Fats in the Small Intestine • fatty acids and glycerol • several steps • absorbed into lymph into blood Chylomicrons contain TG, cholesterol, and phospholipids 22
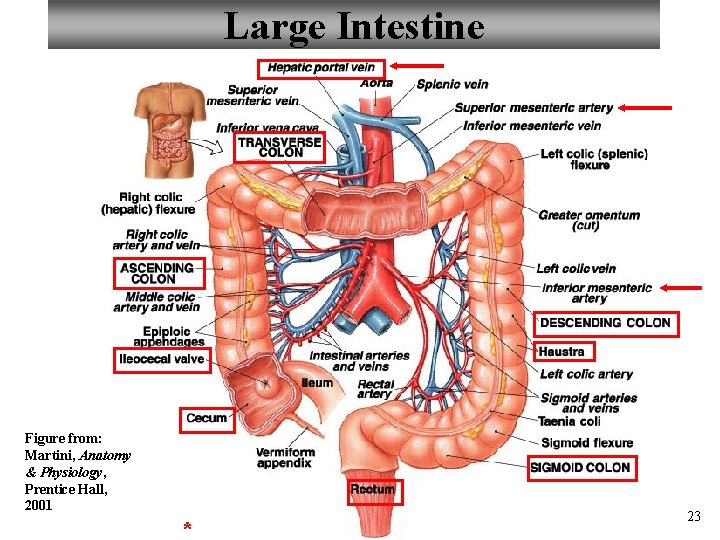
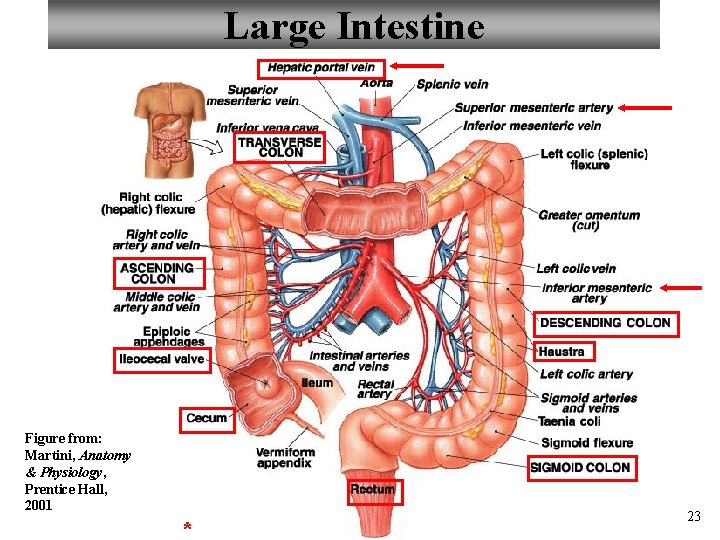
Large Intestine Figure from: Martini, Anatomy & Physiology, Prentice Hall, 2001 * 23
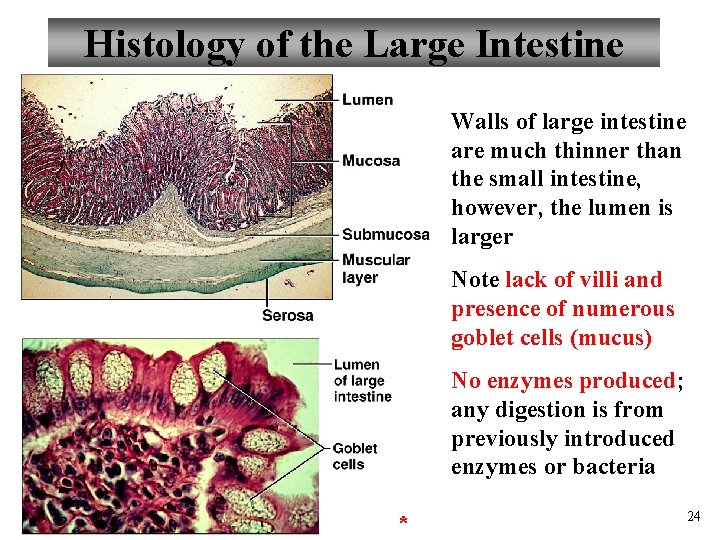
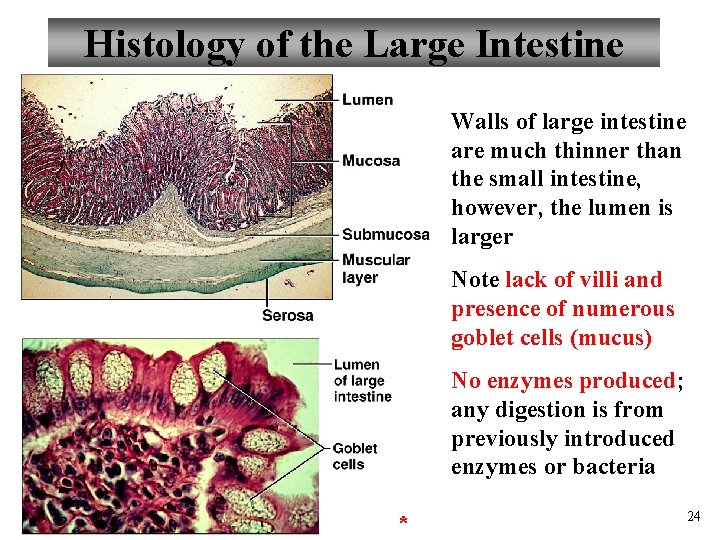
Histology of the Large Intestine Walls of large intestine are much thinner than the small intestine, however, the lumen is larger Note lack of villi and presence of numerous goblet cells (mucus) No enzymes produced; any digestion is from previously introduced enzymes or bacteria * 24
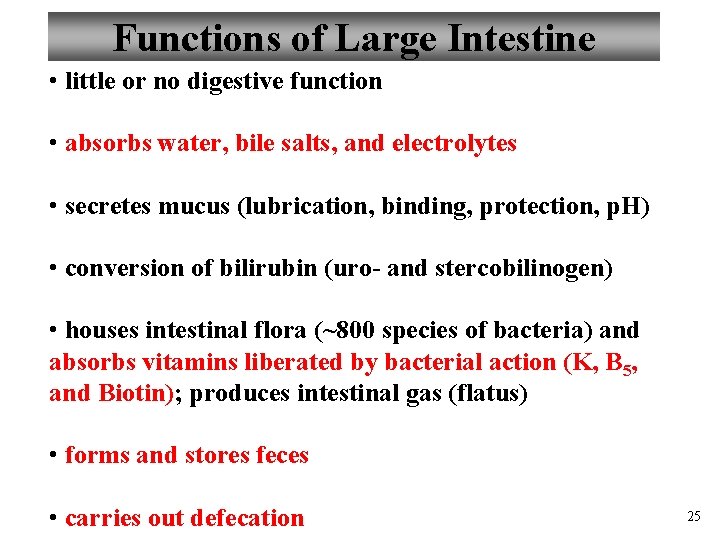
Functions of Large Intestine • little or no digestive function • absorbs water, bile salts, and electrolytes • secretes mucus (lubrication, binding, protection, p. H) • conversion of bilirubin (uro- and stercobilinogen) • houses intestinal flora (~800 species of bacteria) and absorbs vitamins liberated by bacterial action (K, B 5, and Biotin); produces intestinal gas (flatus) • forms and stores feces • carries out defecation 25
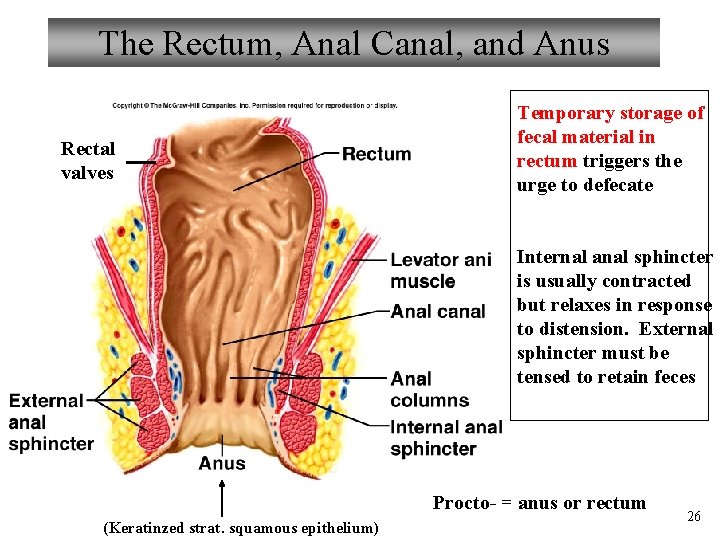
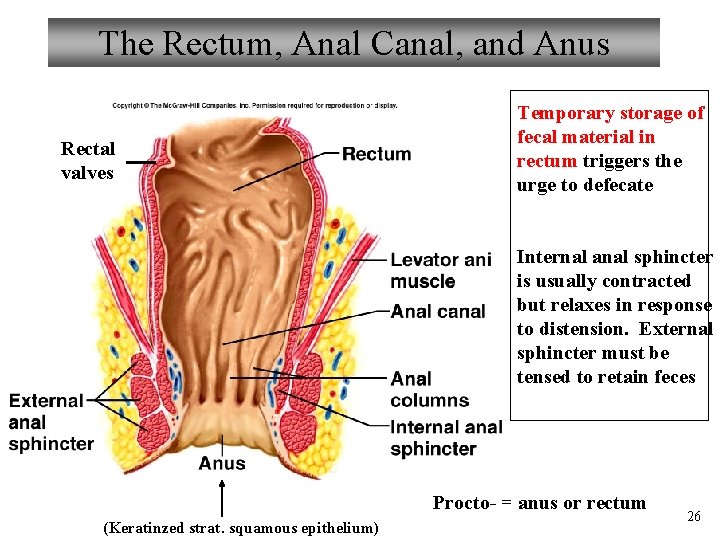
The Rectum, Anal Canal, and Anus Rectal valves Temporary storage of fecal material in rectum triggers the urge to defecate Internal anal sphincter is usually contracted but relaxes in response to distension. External sphincter must be tensed to retain feces Procto- = anus or rectum (Keratinzed strat. squamous epithelium) 26
Movements of Large Intestine • slower and less frequent than those of small intestine • mixing movements (haustral churning every 30 min) • mass movements - usually follow meals (stimulated by distension of stomach and duodenum) - gastrocolic reflex - duodenocolic reflex - peristaltic wave from transverse colon through rest of large intestine 27
All You Need to Know? ? ? 28
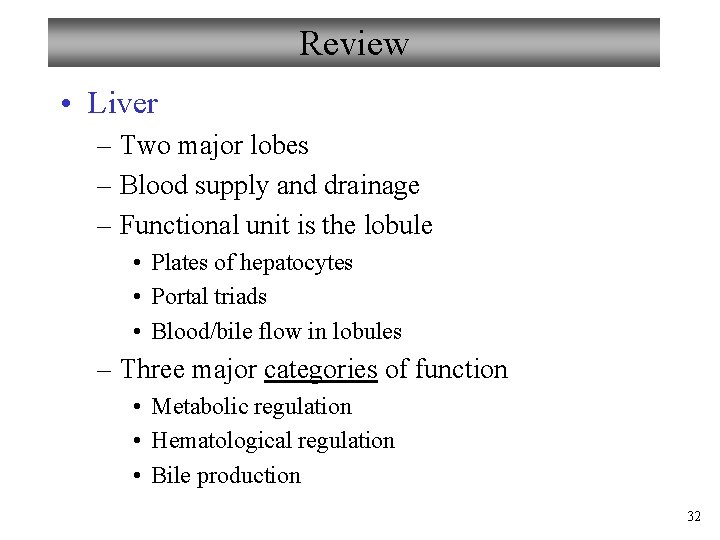
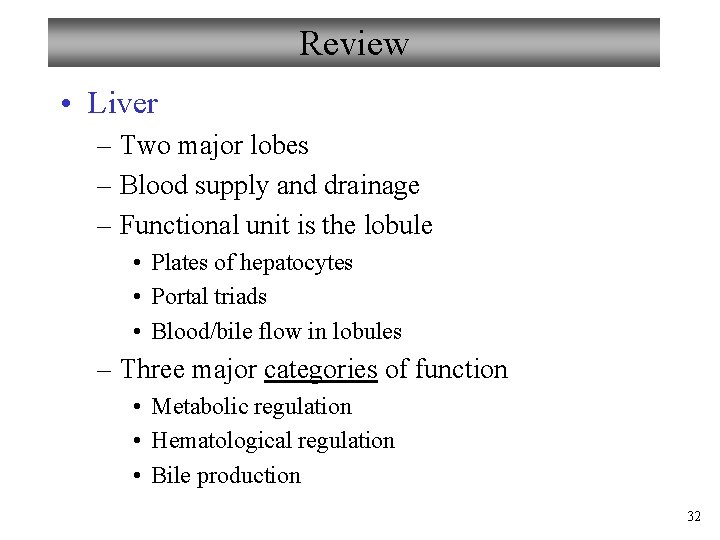
Parasympathetic Defecation Reflex Note that this reflex opens the internal sphincter and closes the external sphincter Need voluntary relaxation of the external sphincter for defecation 29
Feces • water (75%), solids (25%) • electrolytes • mucus • bacteria (30% of solids) and sloughed epithelial cells • bile pigments altered by bacteria provide color (mainly urobilins and stercobilins) • odor produced by bacterial compounds (indoles and skatoles, phenols, H 2 S, ammonia) • indigestible materials 30
Review • Liver – Two major lobes – Blood supply and drainage – Functional unit is the lobule • Plates of hepatocytes • Portal triads • Blood/bile flow in lobules – Three major categories of function • Metabolic regulation • Hematological regulation • Bile production 32
Review • Gall Bladder (GB) – Major function – storage and concentration of bile – Stimulated to contract by CCK – Path of bile from GB • • Cystic duct Common bile duct Hepatopancreatic sphincter (Oddi) – CCK relaxes Duodenal ampulla – Bile • Water, bile salts, bile pigments, electrolytes, cholesterol • Function is emulsification of fats for digestion • Absorption of fats 33
Review • Small Intestine – Three major parts • Duodenum – mixing chamber; mucus • Jejunum – digestion • Ileum – connects to cecum of large intestine – Blood supply and drainage – Suspended from the posterior abdominal wall by the mesentery – Surface area greatly increased by • Plicae • Villi • Microvilli 34
Review • Small Intestine (cont’d) – Secretions – Control of secretion and absorption – Absorption • Protein, CHO, electrolytes – facilitated diffusion • Fats via chylomicrons and lacteals -> circulation – Movements • Local via myenteric plexuses • Long distance via stomach filling – Gastroenteric reflex – Gastroileal reflex 35
Review • Large Intestine – Three major parts • Cecum (veriform appendix) • Colon (ascending, transverse, descending) • Rectum – Blood supply and drainage – Haustra (pouches) – Longitudinal muscle of external muscularis reduced to long strips (taeniae coli) – Wall is thinner than small intestine, less muscle, no villi 36
Review • Large Intestine (cont’d) – Rectum • Temporary storage of feces – urge to defecate • Internal sphincter contracted until distended • External sphincter is voluntary – Major Functions • Absorption of water, bile salts, and electrolytes • Absorbs vitamins produced by bacteria (K, biotin, B 5) • Converts bilirubin – Movements slower and less frequent than small intestine • Mass movements • Stimulated by gastric and duodenal distension 37