Marieke de Groot Derek de Beurs Jos de

Marieke de Groot Derek de Beurs Jos de Keijser Ad Kerkhof
content & time frame 8. 30 - 09. 15 -10. 30 10. 45 -12. 30 13. 30 -15. 00 15. 15 -15. 30 -16. 30 -17. 00 introduction + epidemiology of suicidal behavior basic assumptions of dealing with suicidal behavior break systematic assessment of suicidal behavior break structure diagnosis of suicidal behavior break safety & continuity of care treatment & safety plan chronic suicidal conditions 2
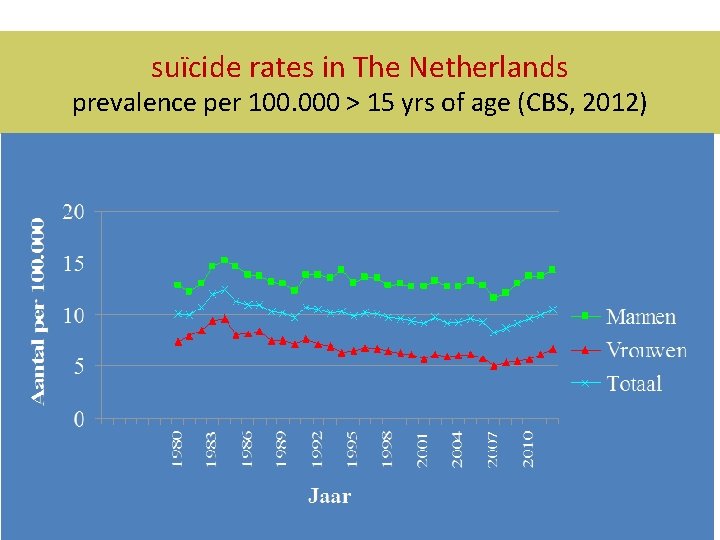
suïcide rates in The Netherlands prevalence per 100. 000 > 15 yrs of age (CBS, 2012) 3
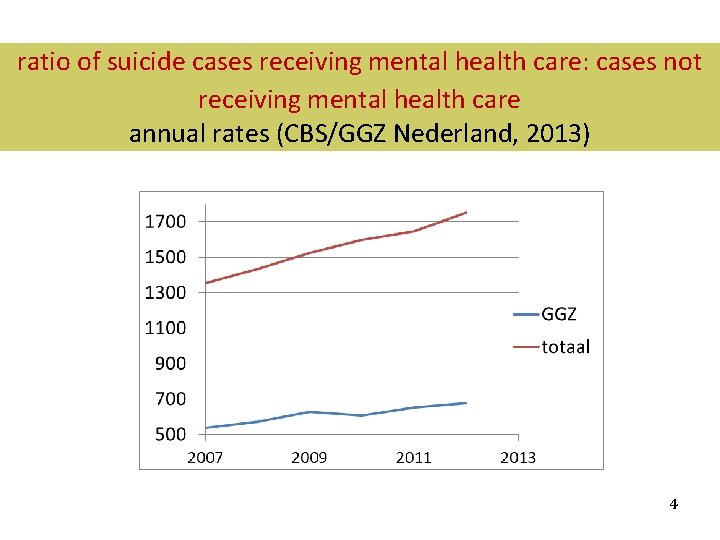
ratio of suicide cases receiving mental health care: cases not receiving mental health care annual rates (CBS/GGZ Nederland, 2013) 4
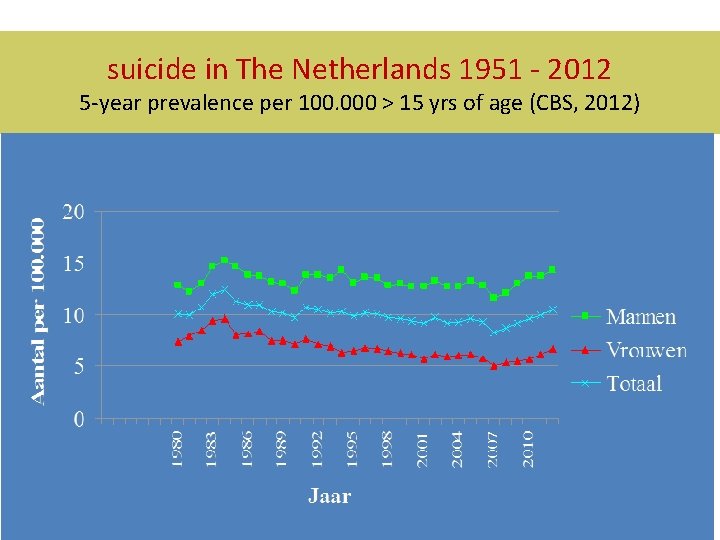
suicide in The Netherlands 1951 - 2012 5 -year prevalence per 100. 000 > 15 yrs of age (CBS, 2012) 5
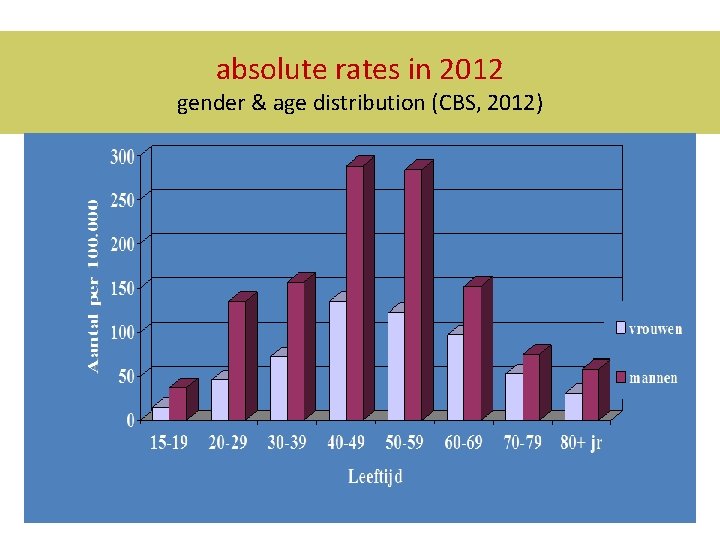
Aantal suïcides in 2010 absolute rates in 2012 Vrouwen en mannen naar leeftijd: aantallen gender & age distribution (CBS, 2012) 6 Centraal Bureau voor de Statistiek 2008
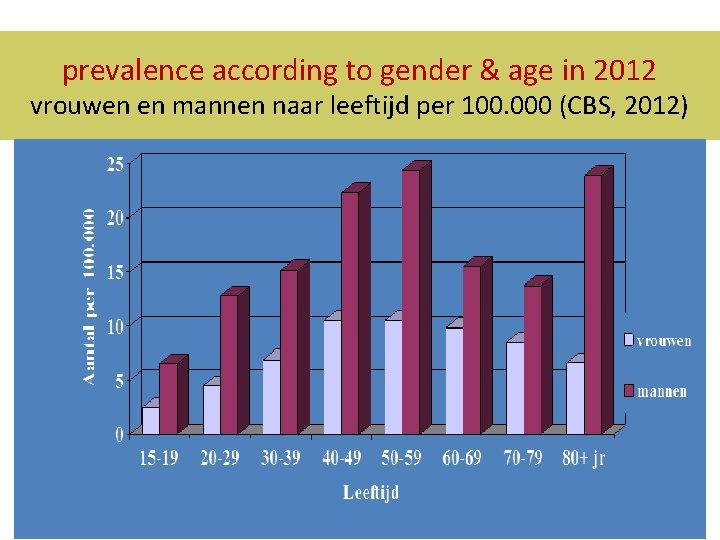
prevalence according to gender & age in 2012 vrouwen en mannen naar leeftijd per 100. 000 (CBS, 2012) 7
introduction rationale of training in guideline application § § § § suicide in mental health care (MHC): 40% received MHC at the time of the suicide; 75% ever received MHC new scientific knowledge; demands from clinical practice; professional and legal demand to follow state-of-the-art; guideline availability ; additional effort to implement guidelines is needed; PITSTOP suïcide study: training & research on the effects of guideline implementation strategies 8
content & time frame 8. 30 - 9. 15 -10. 30 10. 45 -12. 30 13. 30 -15. 00 15. 15 -15. 30 -16. 30 -17. 00 introduction + epidemiology of suicidal behavior basic assumptions of dealing with suicidal behavior break systematic assessment of suicidal behavior break structure diagnosis of suicidal behavior break safety & continuity of care treatment & safety plan chronic suicidal conditions 9
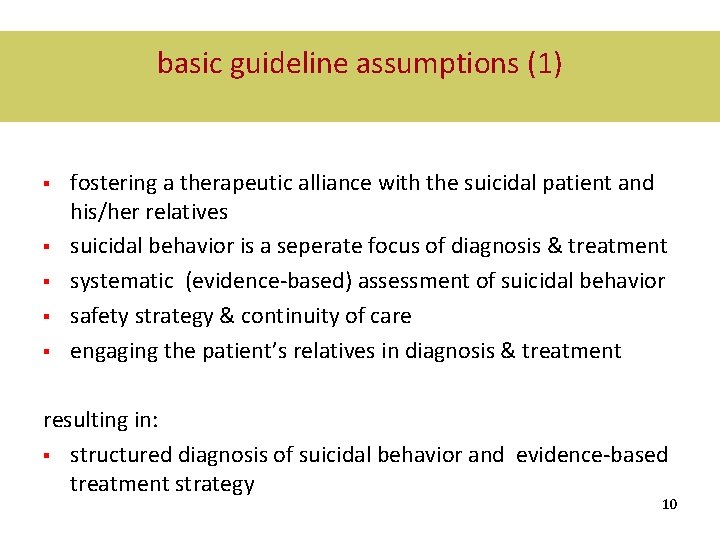
basic guideline assumptions (1) § § § fostering a therapeutic alliance with the suicidal patient and his/her relatives suicidal behavior is a seperate focus of diagnosis & treatment systematic (evidence-based) assessment of suicidal behavior safety strategy & continuity of care engaging the patient’s relatives in diagnosis & treatment resulting in: § structured diagnosis of suicidal behavior and evidence-based treatment strategy 10
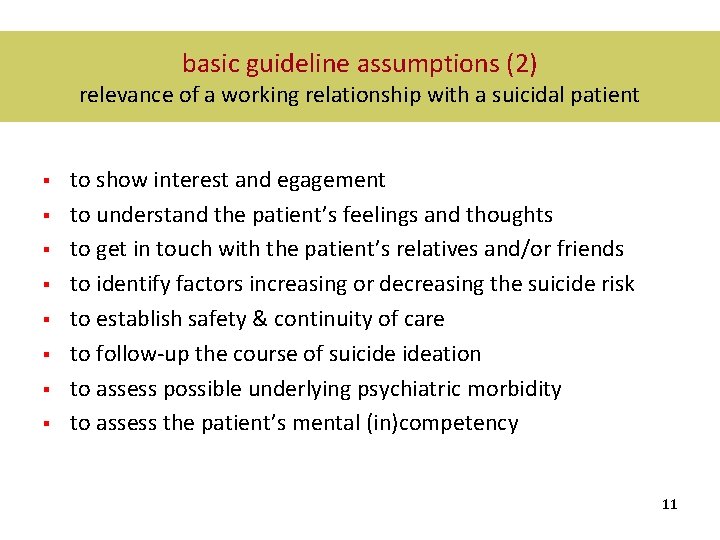
basic guideline assumptions (2) relevance of a working relationship with a suicidal patient § § § § to show interest and egagement to understand the patient’s feelings and thoughts to get in touch with the patient’s relatives and/or friends to identify factors increasing or decreasing the suicide risk to establish safety & continuity of care to follow-up the course of suicide ideation to assess possible underlying psychiatric morbidity to assess the patient’s mental (in)competency 11
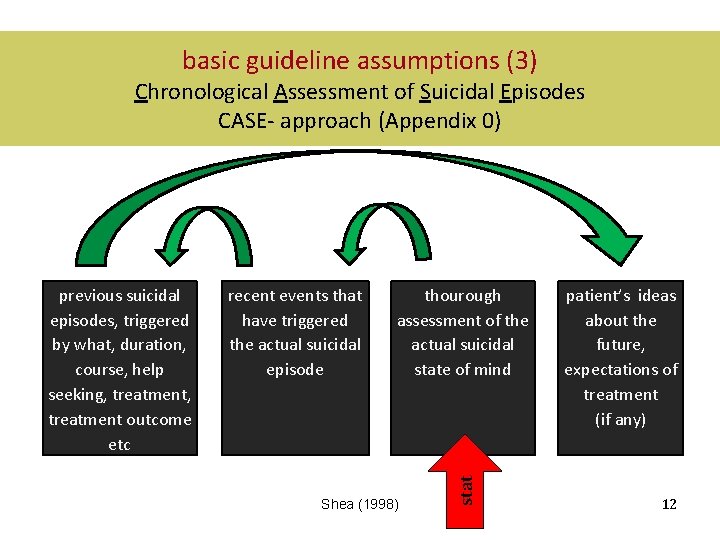
basic guideline assumptions (3) Chronological Assessment of Suicidal Episodes CASE- approach (Appendix 0) recent events that have triggered the actual suicidal episode thourough assessment of the actual suicidal state of mind Shea (1998) stat previous suicidal episodes, triggered by what, duration, course, help seeking, treatment outcome etc patient’s ideas about the future, expectations of treatment (if any) 12
PRACTICING 1 fostering therapeutic alliance with a suicidal patient aims fostering therpeutic alliance by: §thourough assessment of the actual suicidal condition §excercising with questions displayed in appendix 1 §responding to the patient’s narrative 13
PRACTICING 1 instructions § § § choose a fellow-trainee, one plays his most favorite suicidal patient , one ‘plays’ his/herself explore the patient’s actual suicidal state of mind take 20 minutes (don’t change roles) figure out what’s running through the patient’s mind (use questions displayed in Appendix 1) show interest, gather detailed information no solutions, just explore 14
PRACTICING 1 examples of targeted questions (Appendix 1) § § § § § do you consider to kill yourself? how are you going to kill yourself? how often do you think about it? how intrusive are your thoughts about killing yourself (volatile, transient, obsessive, like a nightmare) how much time is left? what problem will be solved if you are dead? what do you want to get rid of? what makes you think being dead is better than being alive? what makes that you are still alive/want to talk with me? what problem may (not, never) be resolved? 15
PRACTICING 1 plenary discussion § § § § how does it feel to ask these questions? how does it feel to be interviewed this way? did you get a detailed view on the patient’s actual suicidal state of mind? did you stick to the non-problem solving mode? what were the effects? is your information complete? do you need more? what exactly? from who? complete the checklist (Appendix 2 +3) 16
PRACTICING 1 evaluation complete the checklists (Appendix 2 +3) -the one who ‘played’ him/herself completes Appendix 2 -the one who played the patient completes Appendix 3 § § complete the checklists independently § subsequently, compare the outcomes discuss possible similarities and differences § 17

BREAK! 18
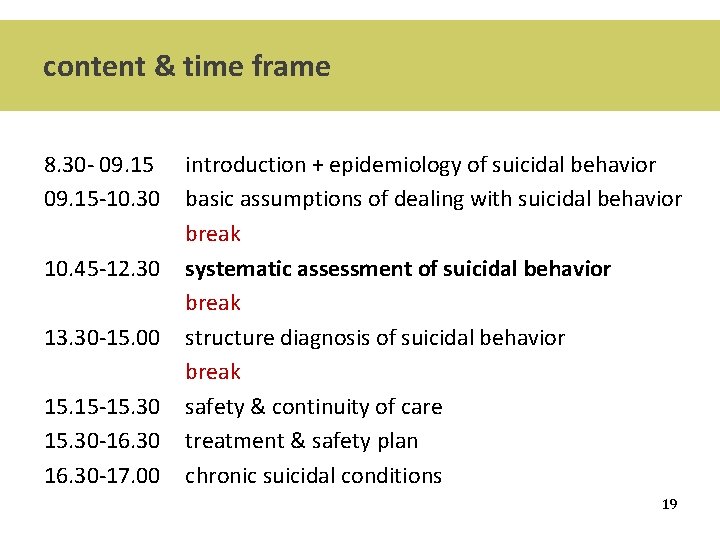
content & time frame 8. 30 - 09. 15 -10. 30 10. 45 -12. 30 13. 30 -15. 00 15. 15 -15. 30 -16. 30 -17. 00 introduction + epidemiology of suicidal behavior basic assumptions of dealing with suicidal behavior break systematic assessment of suicidal behavior break structure diagnosis of suicidal behavior break safety & continuity of care treatment & safety plan chronic suicidal conditions 19
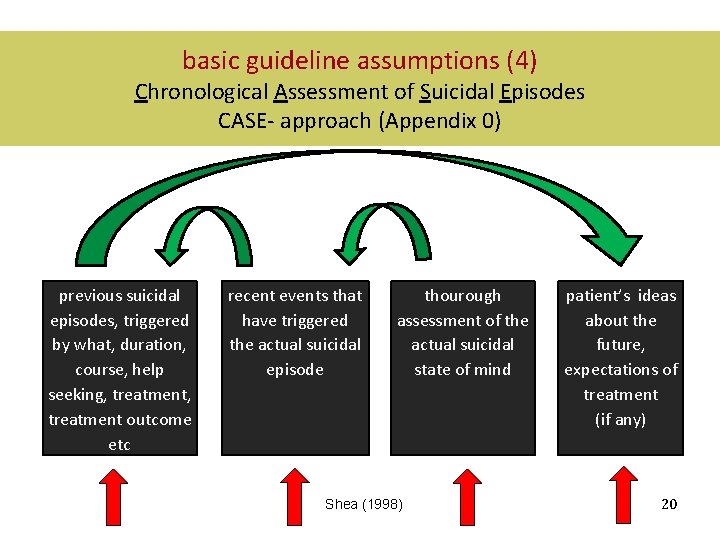
basic guideline assumptions (4) Chronological Assessment of Suicidal Episodes CASE- approach (Appendix 0) previous suicidal episodes, triggered by what, duration, course, help seeking, treatment outcome etc recent events that have triggered the actual suicidal episode thourough assessment of the actual suicidal state of mind Shea (1998) patient’s ideas about the future, expectations of treatment (if any) 20
PRACTICING 2 assessment of recent events & previous suicidal episodes aims § thorough assessment of the actual suicidal condition (Appendix 1) § assessment of events and thoughts triggering the actual suicidal state of mind assessment of events and thoughts in reference of previous suicidal episodes (triggers, course, help seeking, etc) assessment of risk and protection factors associated with the 21 current and previous suicidal episode(s) § §
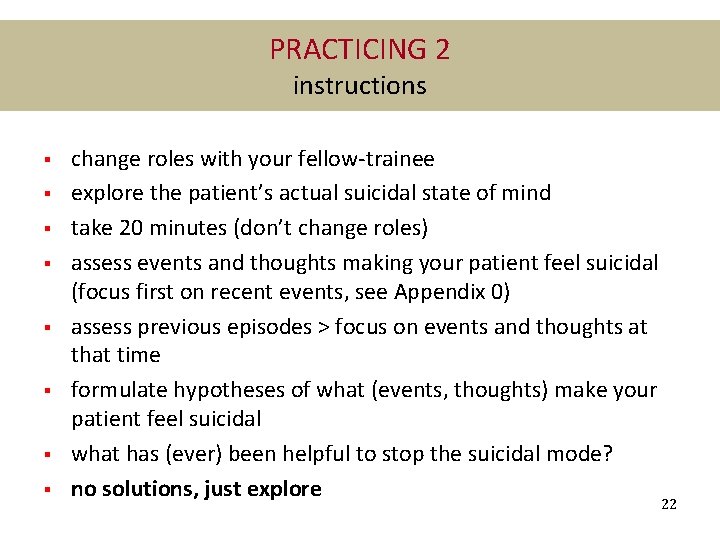
PRACTICING 2 instructions § § § § change roles with your fellow-trainee explore the patient’s actual suicidal state of mind take 20 minutes (don’t change roles) assess events and thoughts making your patient feel suicidal (focus first on recent events, see Appendix 0) assess previous episodes > focus on events and thoughts at that time formulate hypotheses of what (events, thoughts) make your patient feel suicidal what has (ever) been helpful to stop the suicidal mode? no solutions, just explore 22
PRACTICING 2 discussion § § § § did you find out what makes your patient feel suicidal? are there previous episodes? what made your patient felt suicidal at that time? what makes you think your patient is at risk (or not) to complete suicide? why do you think so? which additional information do you need to estimate the patient’s suicide risk? From whom? complete the checklists (Appendix 2 + 3) discuss the outcomes as you did in PRACTICING 1 23
BREAK! 24
content & time frame 8. 30 - 9. 15 -10. 30 10. 45 -12. 30 13. 30 -15. 00 15. 15 -15. 30 -16. 30 -17. 00 introduction + epidemiology of suicidal behavior basic assumptions of dealing with suicidal behavior break systematic assessment of suicidal behavior break structure diagnosis of suicidal behavior break safety & continuity of care treatment & safety plan chronic suicidal conditions 25
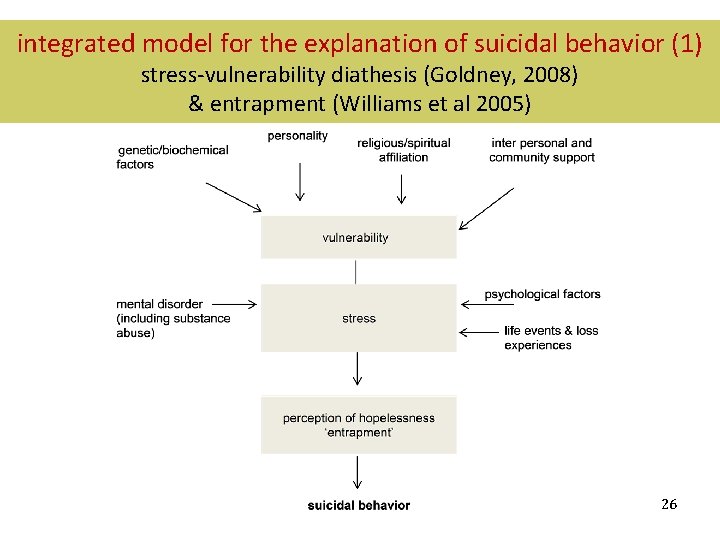
integrated model for the explanation of suicidal behavior (1) stress-vulnerability diathesis (Goldney, 2008) & entrapment (Williams et al 2005) 26
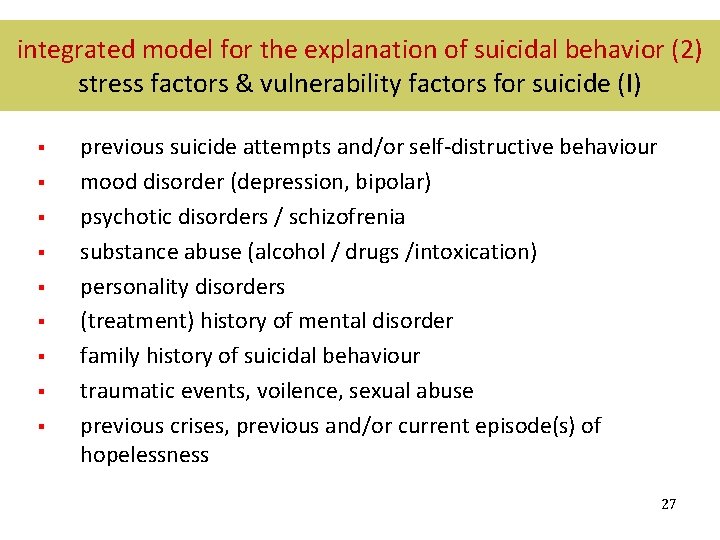
integrated model for the explanation of suicidal behavior (2) stress factors & vulnerability factors for suicide (I) § § § § § previous suicide attempts and/or self-distructive behaviour mood disorder (depression, bipolar) psychotic disorders / schizofrenia substance abuse (alcohol / drugs /intoxication) personality disorders (treatment) history of mental disorder family history of suicidal behaviour traumatic events, voilence, sexual abuse previous crises, previous and/or current episode(s) of hopelessness 27
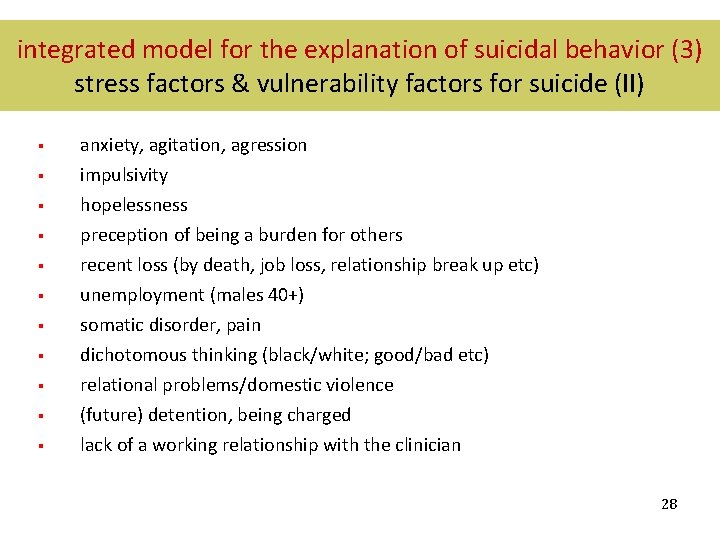
integrated model for the explanation of suicidal behavior (3) stress factors & vulnerability factors for suicide (II) § anxiety, agitation, agression § impulsivity hopelessness preception of being a burden for others recent loss (by death, job loss, relationship break up etc) unemployment (males 40+) somatic disorder, pain dichotomous thinking (black/white; good/bad etc) relational problems/domestic violence (future) detention, being charged lack of a working relationship with the clinician § § § § § 28
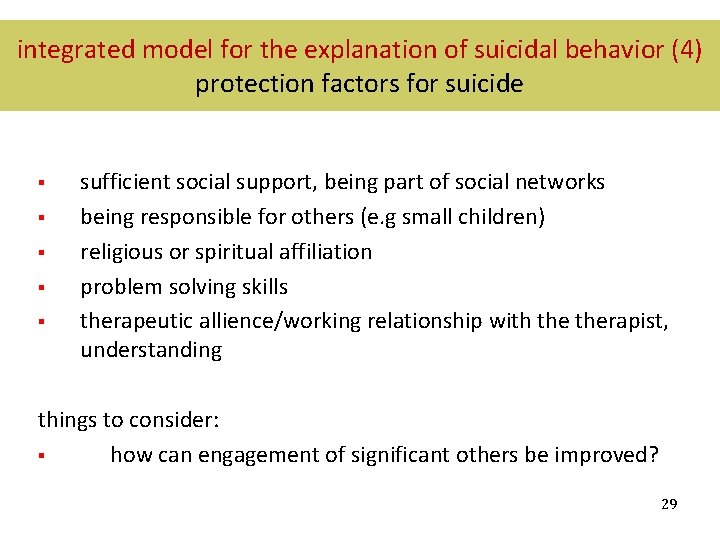
integrated model for the explanation of suicidal behavior (4) protection factors for suicide § § § sufficient social support, being part of social networks being responsible for others (e. g small children) religious or spiritual affiliation problem solving skills therapeutic allience/working relationship with therapist, understanding things to consider: § how can engagement of significant others be improved? 29
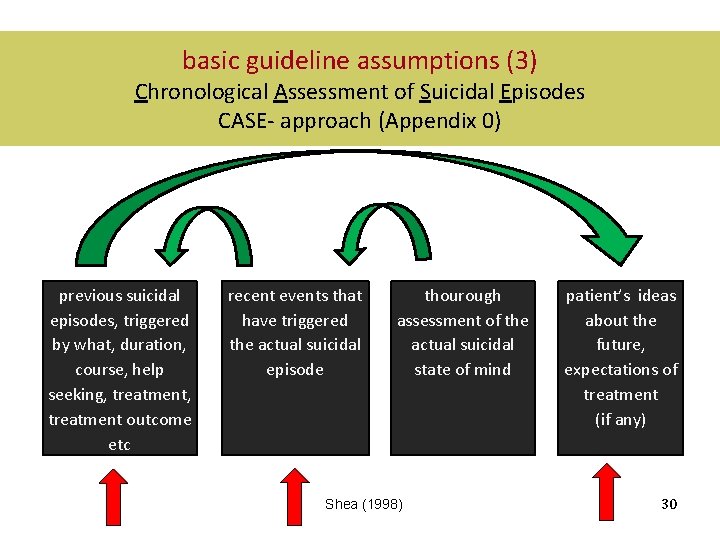
basic guideline assumptions (3) Chronological Assessment of Suicidal Episodes CASE- approach (Appendix 0) previous suicidal episodes, triggered by what, duration, course, help seeking, treatment outcome etc recent events that have triggered the actual suicidal episode thourough assessment of the actual suicidal state of mind Shea (1998) patient’s ideas about the future, expectations of treatment (if any) 30
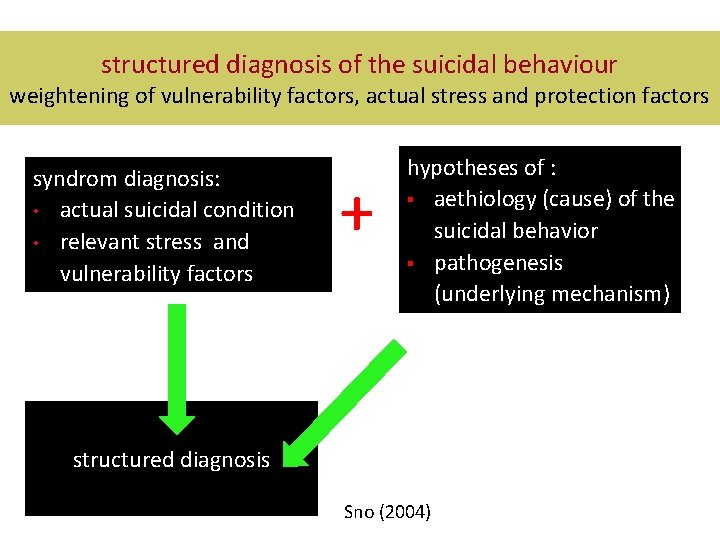
structured diagnosis of the suicidal behaviour weightening of vulnerability factors, actual stress and protection factors syndrom diagnosis: • actual suicidal condition • relevant stress and vulnerability factors + hypotheses of : § aethiology (cause) of the suicidal behavior § pathogenesis (underlying mechanism) structured diagnosis Sno (2004)
PRACTICING 3 structured diagnosis of the suicidal behaviour aims § thorough assessment of the actual suicidal condition (Appendix 1) § identifying stress and vulnerability factors § identifying protection factors (Appendix 5 +6) § investigation of the patient’s ideas about his/her future § formulation of a hypothesis of the ethiology and pathogenesis of the suicidal behaviour (= the base of treatment plan) 32
PRACTICING 3 structured diagnosis of the suicidal behaviour: instructions § § § § use the case and ‘play’ similar roles as in practicing 1 explore the patient’s suicidal behaviour with the caseinterview use questions from Appendix 1 (or make your own) asssess stress factors, vulnerability and protection factors (Appendix 4) assess the patient’s ideas about his/her future discuss your hypotheses of the ethiology and pathogenesis of the onset of the suicidal state with your patient check and if applicable, adjust the hypothesis until you achieve full consensus no solutions, just explore 33
PRACTICING 3 discussion § § § § did you find out what’s going in your patient’s mind? did you find out your patient’s ideas about his/her future? what stress factors are relevant for the onset of the current suicidal episode? what vulnerability factors are relevant? what protoction factors are relevant? whta is your hypothesis of the onset and maintanance of the suicidal state of mind? did you stay away from the promblem solving mode? what has been helpful to do so? 34
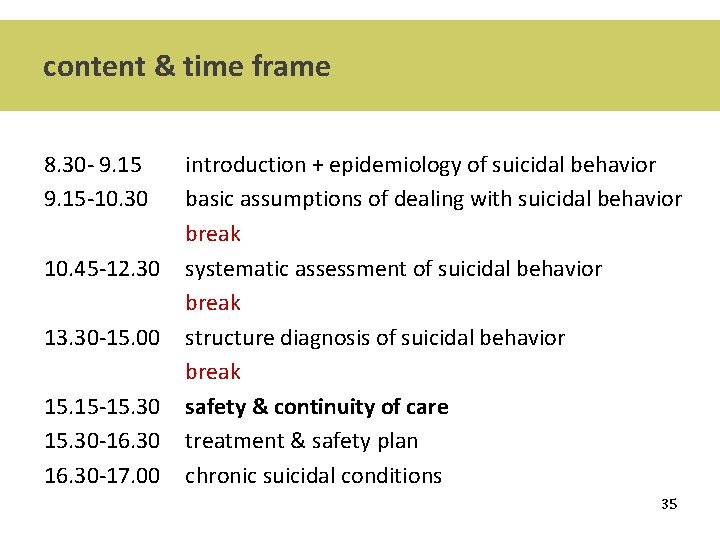
content & time frame 8. 30 - 9. 15 -10. 30 10. 45 -12. 30 13. 30 -15. 00 15. 15 -15. 30 -16. 30 -17. 00 introduction + epidemiology of suicidal behavior basic assumptions of dealing with suicidal behavior break systematic assessment of suicidal behavior break structure diagnosis of suicidal behavior break safety & continuity of care treatment & safety plan chronic suicidal conditions 35
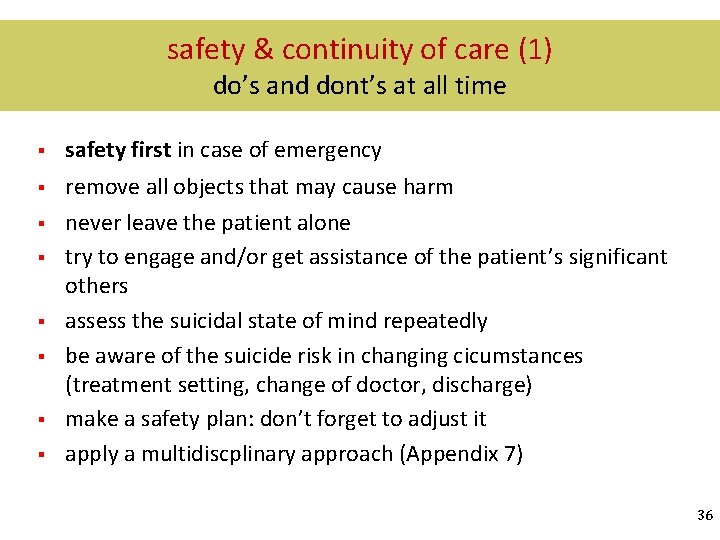
safety & continuity of care (1) do’s and dont’s at all time § safety first in case of emergency § remove all objects that may cause harm never leave the patient alone try to engage and/or get assistance of the patient’s significant others assess the suicidal state of mind repeatedly be aware of the suicide risk in changing cicumstances (treatment setting, change of doctor, discharge) make a safety plan: don’t forget to adjust it apply a multidiscplinary approach (Appendix 7) § § § 36
safety & continuity of care (2) (Appendix 7) insert 37
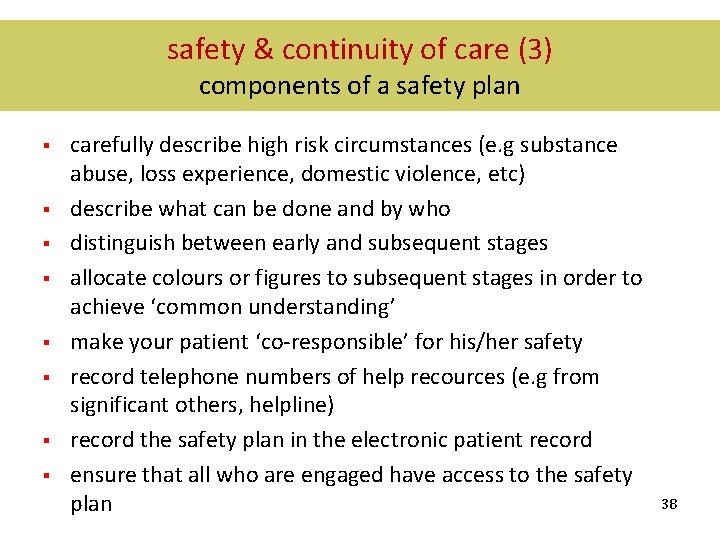
safety & continuity of care (3) components of a safety plan § § § § carefully describe high risk circumstances (e. g substance abuse, loss experience, domestic violence, etc) describe what can be done and by who distinguish between early and subsequent stages allocate colours or figures to subsequent stages in order to achieve ‘common understanding’ make your patient ‘co-responsible’ for his/her safety record telephone numbers of help recources (e. g from significant others, helpline) record the safety plan in the electronic patient record ensure that all who are engaged have access to the safety plan 38
content & time frame 8. 30 - 9. 15 -10. 30 10. 45 -12. 30 13. 30 -15. 00 15. 15 -15. 30 -16. 30 -17. 00 introduction + epidemiology of suicidal behavior basic assumptions of dealing with suicidal behavior break systematic assessment of suicidal behavior break structure diagnosis of suicidal behavior break safety & continuity of care treatment & safety plan chronic suicidal conditions 39
treatment options § pharmaco- and/or psychotherapy § suicidal behaviour as focus of treatment (hopelessness, ideas about the future, depressive cognitions etc) treatment of stress and/or vulnerability factors (depression, personality disorder, psychotic disorder) stregthen protective factors (improve engagement of significant others, improve self-management) consider treatment option targeting specific patient categories (adolescents, elderly, patient with personality disorder) consider treatment setting is most appropriate (in or out patient care, crisis intervention) organize follow-up care (frequency, by whom, location, etc) § § § 40
PRACTICING 4 establishing treatment strategy (1) aims § thorough assessment of the actual suicidal condition (Appendix 1) § identifying stress and vulnerability factors § identifying protection factors (Appendix 5 +6) § investigation of the patient’s ideas about his/her future § formulation of a hypothesis of the ethiology and pathogenesis of the suicidal behaviour (= the base of treatment plan) 41
PRACTICING 4 determining treatment (2) (Appendix 5) Aims § weightening short and long term suicide risk § considering treatment options § planning safety (make a safety plan) § planning of treatment (follow-up etc) § increasing continuity of care § engaging the patient’s relatives 42
PRACTICING 4 determining treatment (3) (Appendix 5) Be on the alert of: § § treatment & follow-up contacts patient safety continuity of care engagement of significant others 43
PRACTICING 4 plenary discussion § What treatment options did you consider. Why? Did you make a safety plan? What is in? How are significant others involved? Continuity of care facilitated? § Arrangements all clear to everyone? § § § 44
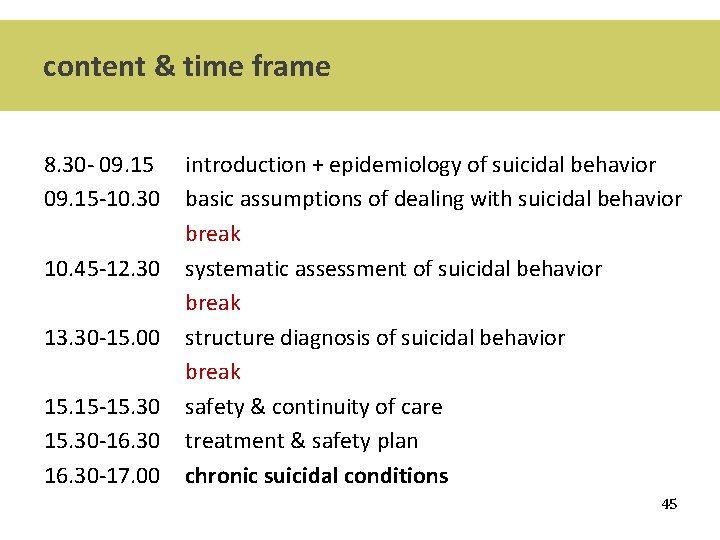
content & time frame 8. 30 - 09. 15 -10. 30 10. 45 -12. 30 13. 30 -15. 00 15. 15 -15. 30 -16. 30 -17. 00 introduction + epidemiology of suicidal behavior basic assumptions of dealing with suicidal behavior break systematic assessment of suicidal behavior break structure diagnosis of suicidal behavior break safety & continuity of care treatment & safety plan chronic suicidal conditions 45
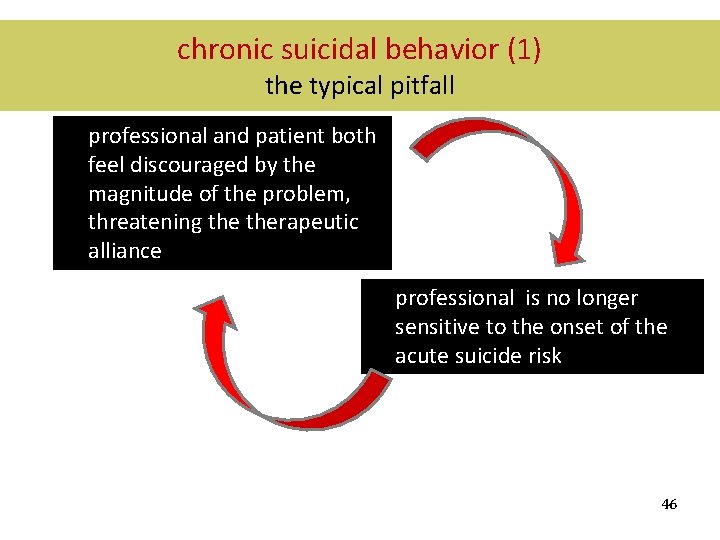
chronic suicidal behavior (1) the typical pitfall professional and patient both feel discouraged by the magnitude of the problem, threatening therapeutic alliance professional is no longer sensitive to the onset of the acute suicide risk 46
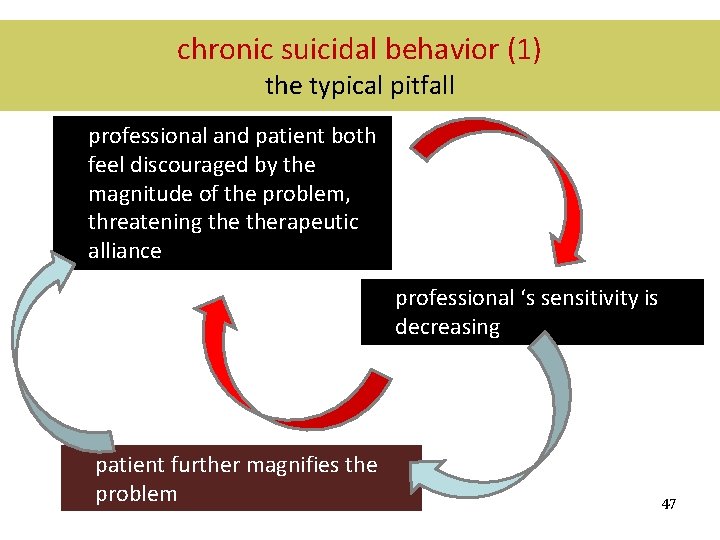
chronic suicidal behavior (1) the typical pitfall professional and patient both feel discouraged by the magnitude of the problem, threatening therapeutic alliance professional ‘s sensitivity is decreasing patient further magnifies the problem 47
chronic suicidal behavior (2) cluster B personality disorder § § § Borderline Personality Disorder: suicidal behavior is a diagnostic criterium 75% of the patients make suicide attempts; 10% of the patients die by suicide often caused by poor impuls control (substance abuse may be the cause as well as the effect) delibarate self-harm and suicidal behavior often occur at the same time suicide risk is increased in depressed cluster B patients and/or in case of substance abuse (alcohol /drugs) prone to crises; may lead to ‘acute suicide risk in chronic suicidal patients’ 48
chronic suicidal behavior (3) cluster B personality disorder In crises: § Assessment of what causes ‘acute suicide risk’ > pay attention to acute stress factors (CASE-interview) Treatment at 3 levels: § psychiatric (co)morbidity § stress factors causing and maintaining the suicidal condition § psycho-social revalidation enhancing safety and continuity of care 49
- Slides: 49