MAPAM Payer Conference 51718 BMCHP 1 Agenda ACOs
MAPAM Payer Conference 5/17/18 BMCHP 1
Agenda §ACOs are provider-led BMCHP overview organizations that coordinate care, have an §enhanced Plan programs in 2018 role for primary care, and are rewarded for value – improving total cost of care and outcomes – not volume Ø Member ID review Ø Eligibility Verification The primary focus is on improving patient outcomes by: Ø Authorizations v Ø Promoting healthy behaviors Claims v Expanding population health management programs, and § BMCHP Clinical Vendors v Improving data exchange between payers and providers § ACO Plans Ø Provider Network Ø Community Partner Program § Questions 2
Who we are §ACOs are provider-led BMCHP is a non-profit managed care organizations that coordinate care, have an enhanced role for primary care, and are rewarded for value – committed to providing the highest quality healthcare improving total cost of care and outcomes – not coverage to underserved populations. volume The primary focus is on improving patient outcomes by: § Service Members via 4 Programs in MA and NH v Promoting healthy behaviors Ø v Mass. Health Expanding population health management programs, and Ø (under the trade name Well Sense Health Plan) v NH Medicaid Improving data exchange between payers and providers Ø MA Qualified Health Plan Ø MA Senior Care Options* *( Available in Barnstable, Bristol, Hamden Plymouth & Suffolk County) 3
BMCHP Mass. Health Plans include: § BMCHP Mass. Health MCO – Primary Care within the BMCHP MCO Network. § BMCHP Community Alliance ACO – Primary Care within the BMCHP Community Alliance ACO Network. § BMCHP Mercy Alliance ACO – Primary Care within the BMCHP Mercy Alliance ACO Network. § BMCHP Signature Alliance ACO – Primary Care within the BMCHP Signature Alliance ACO Network. § BMCHP Southcoast Alliance ACO – Primary Care within the BMCHP Southcoast Alliance ACO. BMCHP’s full network of Mass. Health contracted facilities, specialists and ancillary services is available for all above Plans 4
Additional BMCHP Plans include: § Connector. Care – BMCHP’s full network of Connector. Care contracted facilities, primary care, specialists and ancillary services is available. § Qualified Health Plans - BMCHP’s full network of Qualified Health Plan contracted facilities, primary care, specialists and ancillary services is available. § Senior Care Options - BMCHP’s full network of Senior Care Options contracted facilities, primary care, specialists and ancillary services is available. 5
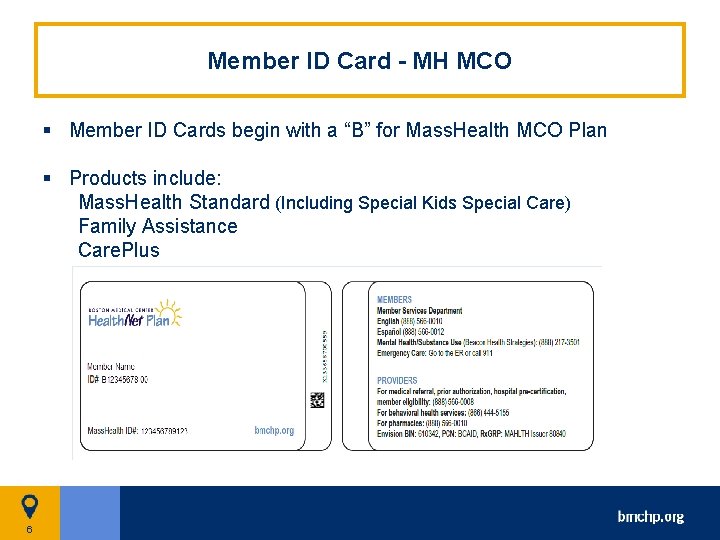
Member ID Card - MH MCO § Member ID Cards begin with a “B” for Mass. Health MCO Plan § Products include: Mass. Health Standard (Including Special Kids Special Care) Family Assistance Care. Plus 6
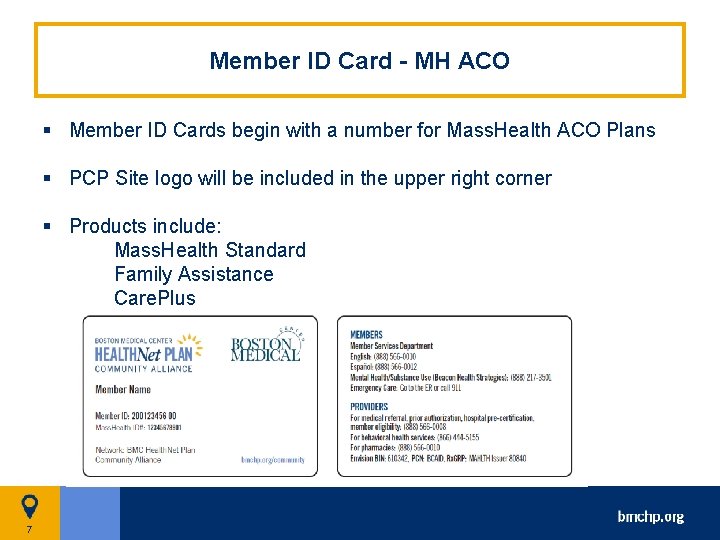
Member ID Card - MH ACO § Member ID Cards begin with a number for Mass. Health ACO Plans § PCP Site logo will be included in the upper right corner § Products include: Mass. Health Standard Family Assistance Care. Plus 7
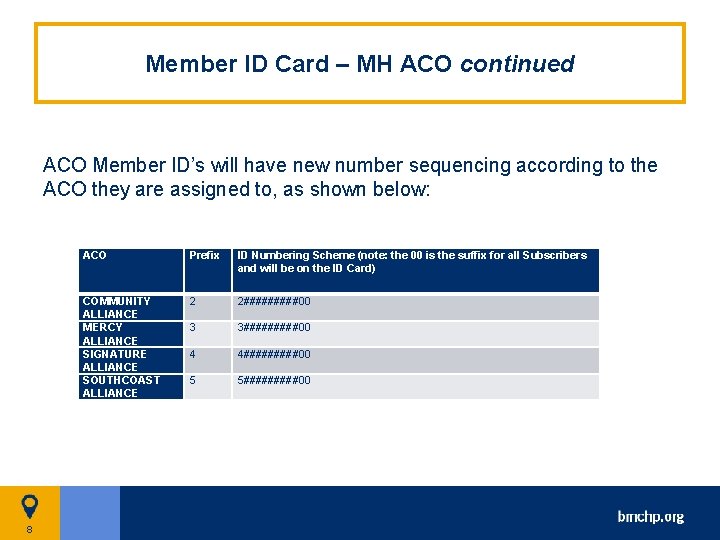
Member ID Card – MH ACO continued ACO Member ID’s will have new number sequencing according to the ACO they are assigned to, as shown below: 8 ACO Prefix ID Numbering Scheme (note: the 00 is the suffix for all Subscribers and will be on the ID Card) COMMUNITY ALLIANCE MERCY ALLIANCE SIGNATURE ALLIANCE SOUTHCOAST ALLIANCE 2 2#####00 3 3#####00 4 4#####00 5 5#####00
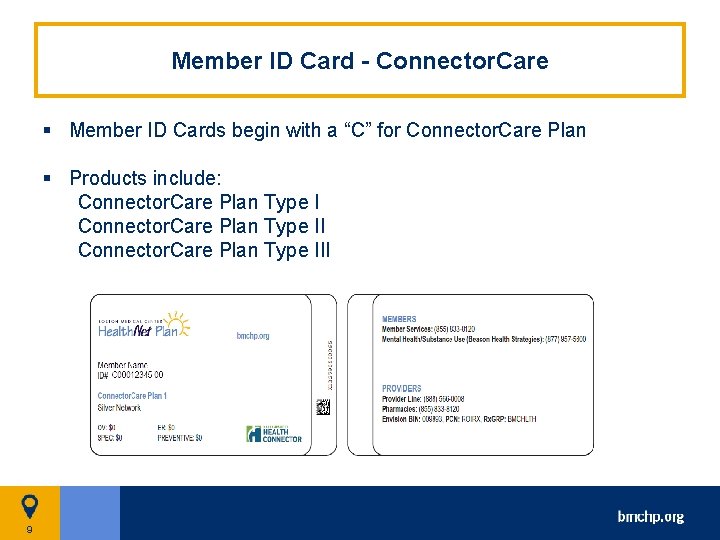
Member ID Card - Connector. Care § Member ID Cards begin with a “C” for Connector. Care Plan § Products include: Connector. Care Plan Type III 9
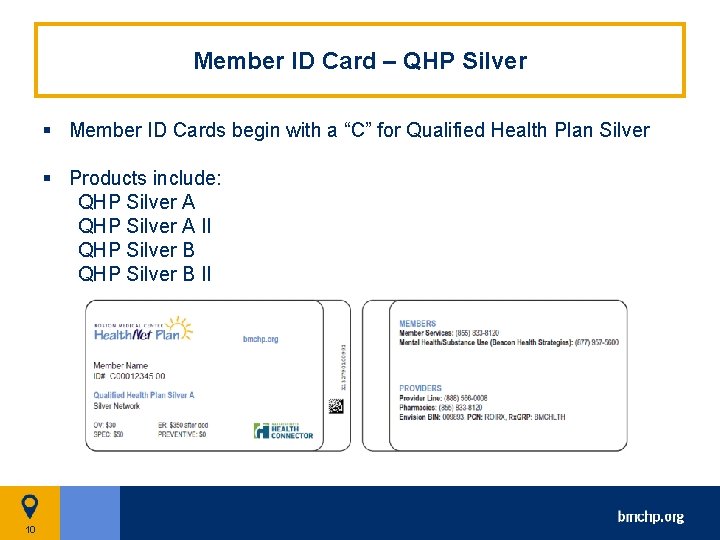
Member ID Card – QHP Silver § Member ID Cards begin with a “C” for Qualified Health Plan Silver § Products include: QHP Silver A II QHP Silver B II 10
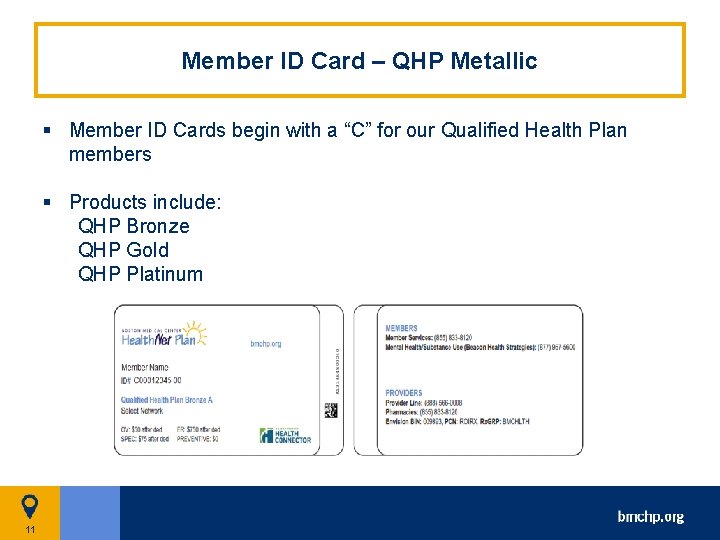
Member ID Card – QHP Metallic § Member ID Cards begin with a “C” for our Qualified Health Plan members § Products include: QHP Bronze QHP Gold QHP Platinum 11
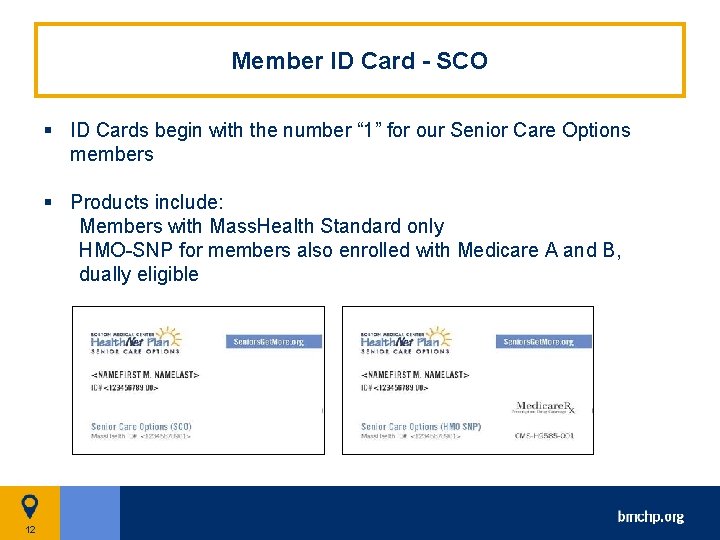
Member ID Card - SCO § ID Cards begin with the number “ 1” for our Senior Care Options members § Products include: Members with Mass. Health Standard only HMO-SNP for members also enrolled with Medicare A and B, dually eligible 12
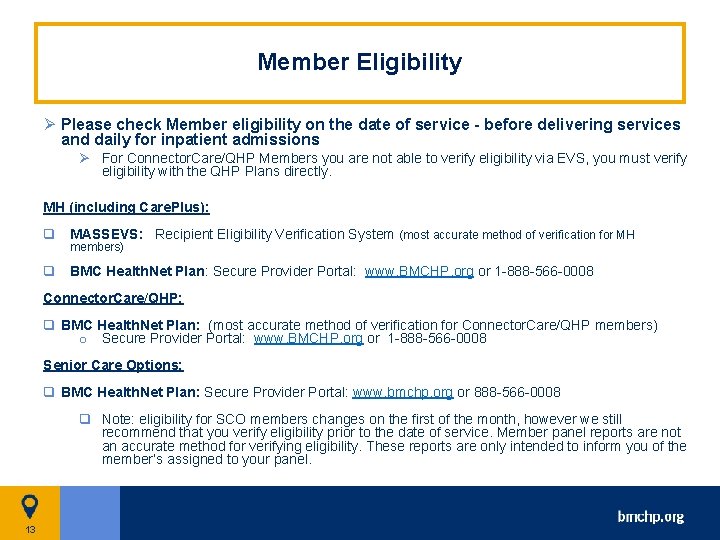
Member Eligibility Ø Please check Member eligibility on the date of service - before delivering services and daily for inpatient admissions Ø For Connector. Care/QHP Members you are not able to verify eligibility via EVS, you must verify eligibility with the QHP Plans directly. MH (including Care. Plus): q MASSEVS: Recipient Eligibility Verification System (most accurate method of verification for MH members) q BMC Health. Net Plan: Secure Provider Portal: www. BMCHP. org or 1 -888 -566 -0008 Connector. Care/QHP: q BMC Health. Net Plan: (most accurate method of verification for Connector. Care/QHP members) o Secure Provider Portal: www. BMCHP. org or 1 -888 -566 -0008 Senior Care Options: q BMC Health. Net Plan: Secure Provider Portal: www. bmchp. org or 888 -566 -0008 q Note: eligibility for SCO members changes on the first of the month, however we still recommend that you verify eligibility prior to the date of service. Member panel reports are not an accurate method for verifying eligibility. These reports are only intended to inform you of the member’s assigned to your panel. 13
14
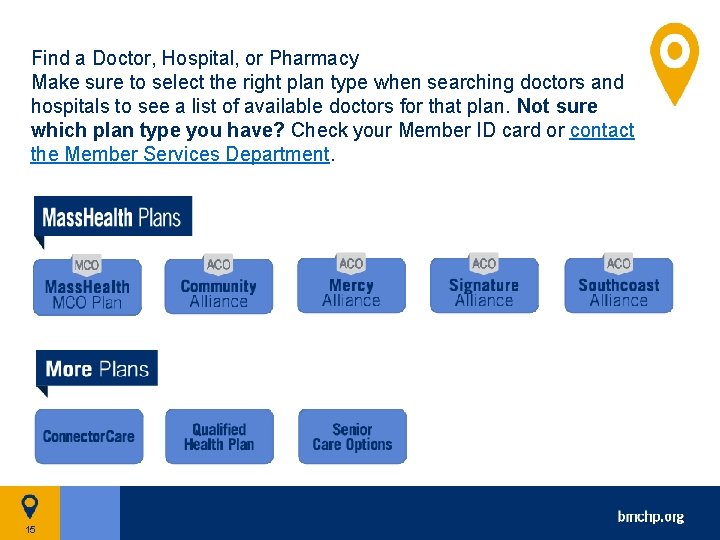
Find a Doctor, Hospital, or Pharmacy Make sure to select the right plan type when searching doctors and hospitals to see a list of available doctors for that plan. Not sure which plan type you have? Check your Member ID card or contact the Member Services Department. 15
What services need referrals (if any) and/or Prior Authorization? BMCHP does not require referrals. We do, however, have Prior Authorization requirements for select services which are outlined in the Prior Authorization (PA) Matrix and the PA look up tools at: https: //www. bmchp. org/providers/authorizations/check-service 16
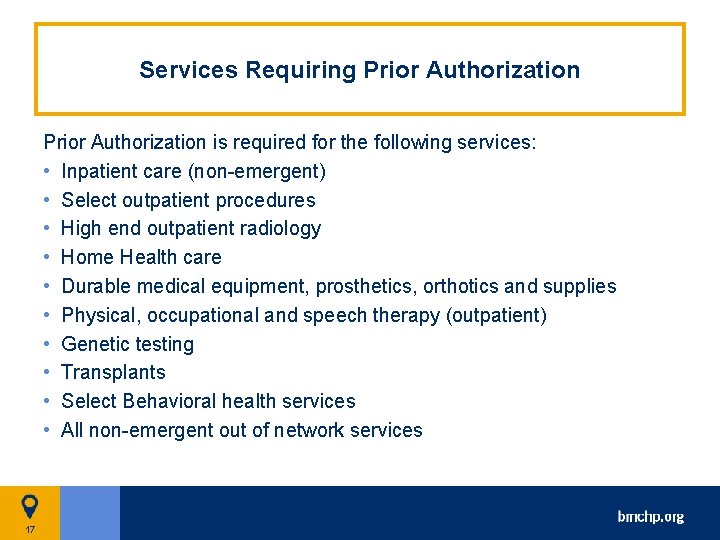
Services Requiring Prior Authorization is required for the following services: • Inpatient care (non-emergent) • Select outpatient procedures • High end outpatient radiology • Home Health care • Durable medical equipment, prosthetics, orthotics and supplies • Physical, occupational and speech therapy (outpatient) • Genetic testing • Transplants • Select Behavioral health services • All non-emergent out of network services 17
18
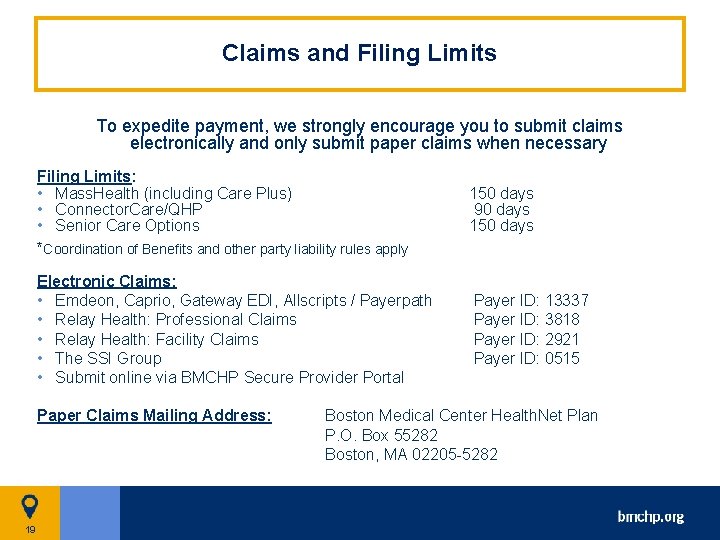
Claims and Filing Limits To expedite payment, we strongly encourage you to submit claims electronically and only submit paper claims when necessary Filing Limits: • Mass. Health (including Care Plus) • Connector. Care/QHP • Senior Care Options *Coordination of Benefits and other party liability rules apply 150 days 90 days 150 days Electronic Claims: • Emdeon, Caprio, Gateway EDI, Allscripts / Payerpath • Relay Health: Professional Claims • Relay Health: Facility Claims • The SSI Group • Submit online via BMCHP Secure Provider Portal Payer ID: 13337 Payer ID: 3818 Payer ID: 2921 Payer ID: 0515 Paper Claims Mailing Address: 19 Boston Medical Center Health. Net Plan P. O. Box 55282 Boston, MA 02205 -5282
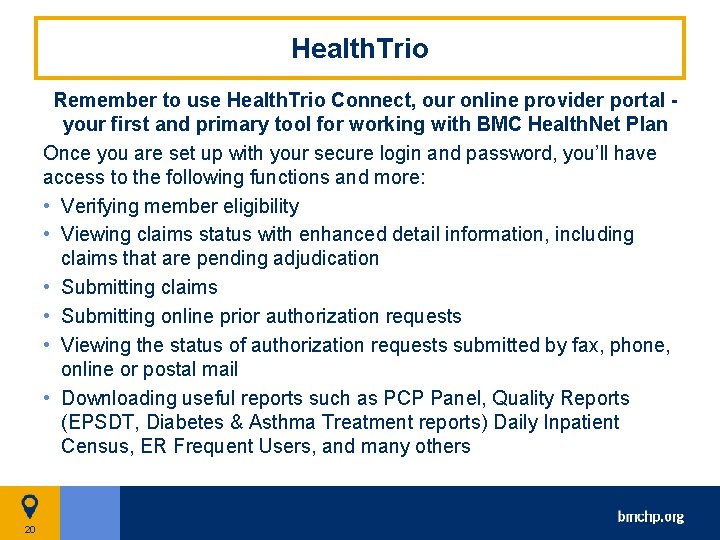
Health. Trio Remember to use Health. Trio Connect, our online provider portal your first and primary tool for working with BMC Health. Net Plan Once you are set up with your secure login and password, you’ll have access to the following functions and more: • Verifying member eligibility • Viewing claims status with enhanced detail information, including claims that are pending adjudication • Submitting claims • Submitting online prior authorization requests • Viewing the status of authorization requests submitted by fax, phone, online or postal mail • Downloading useful reports such as PCP Panel, Quality Reports (EPSDT, Diabetes & Asthma Treatment reports) Daily Inpatient Census, ER Frequent Users, and many others 20
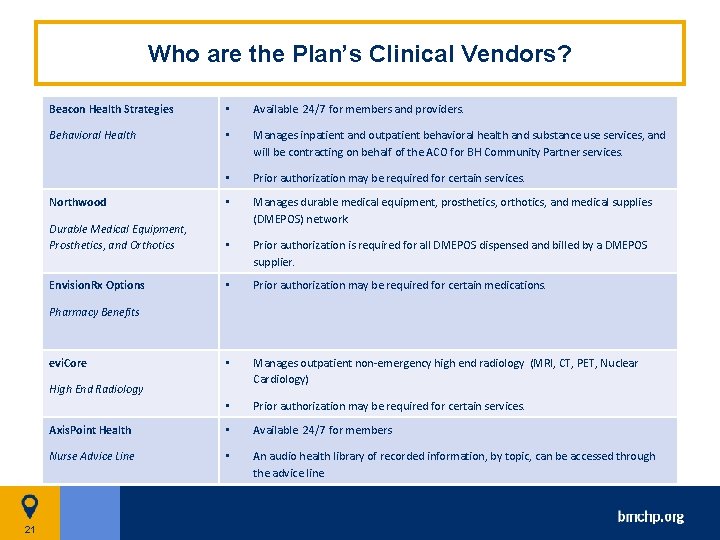
Who are the Plan’s Clinical Vendors? Beacon Health Strategies • Available 24/7 for members and providers. Behavioral Health • Manages inpatient and outpatient behavioral health and substance use services, and will be contracting on behalf of the ACO for BH Community Partner services. • Prior authorization may be required for certain services. Northwood • Durable Medical Equipment, Prosthetics, and Orthotics Manages durable medical equipment, prosthetics, orthotics, and medical supplies (DMEPOS) network. • Prior authorization is required for all DMEPOS dispensed and billed by a DMEPOS supplier. Envision. Rx Options • Prior authorization may be required for certain medications. • Manages outpatient non-emergency high end radiology (MRI, CT, PET, Nuclear Cardiology) • Prior authorization may be required for certain services. Axis. Point Health • Available 24/7 for members Nurse Advice Line • An audio health library of recorded information, by topic, can be accessed through the advice line Pharmacy Benefits evi. Core High End Radiology 21
What are the benefits and protections for members who are being shifted to the new ACO model? The core covered benefits will be the same for both ACO and MCO members. There may, however, be additional services or programs offered by each ACO members have the same protections and rights under the ACO program as they currently have under the MCO Program. 22
Billing, Eligibility Verification and Prior Authorization for ACO § There are no changes to the way you will bill for the services rendered to members enrolled in our ACO model § BMCHP will continue to use the same eligibility verification system. § We also have not changed any respective prior authorization requirements or processes at this time. 23
Where will ACO Members receive care? § Members will have a PCP in the ACO and must use that PCP for all primary care. Primary Care providers may only enroll in one ACO. § The PCP will make efforts to direct members to specialists and other providers within the ACO or with whom there is an established relationship. § However, members may go to any contracted specialist/other provider within the BMCHP network – subject to the specialist/provider obtaining a prior authorization for the service, if applicable. 24
ACOs and MCOs will contract with Community Partners for the purposes of integrated care delivery • Create opportunity for ACOs and MCOs to leverage the expertise and capabilities of existing community-based organizations serving populations with BH and LTSS needs • BH CPs will provide comprehensive care management including outreach & engagement, assessment, medication reconciliation, care transitions, health & wellness coaching as well as connections to social services and community resources • LTSS CPs will provide LTSS care coordination including outreach & engagement, care planning, care transitions, health & wellness coaching as well as connections to social services and community resources 25
Questions? Thank you! Provider Relations Provider. Info@bmchp-wellsense. org 26
- Slides: 26