Many Pathways to Depression There are many pathways




- Slides: 62
Many Pathways to Depression • There are many pathways to depression; Trauma is only one of them, but it’s a common contributor. • When trauma plays a significant role in the development of depression, we can think in terms of posttraumatic depression. (Allen, J. 2005, Coping with Trauma)
The Trauma Spectrum Cumulative adverse experiences since childhood create vulnerability: • Primary trauma-Adverse childhood events • Secondary trauma-Impact of observation • Neglect / Poor Attachment • Out of control high levels of stress • Culturally endorsed trauma

The Trauma Spectrum (con’t. ) Adult traumatic experiences build on and exacerbate childhood traumatic experiences • Abusive relationships • Assaults • Death of loved ones • Losses, i. e. , employment, disease, relationships • War • Accidents • Natural Disasters
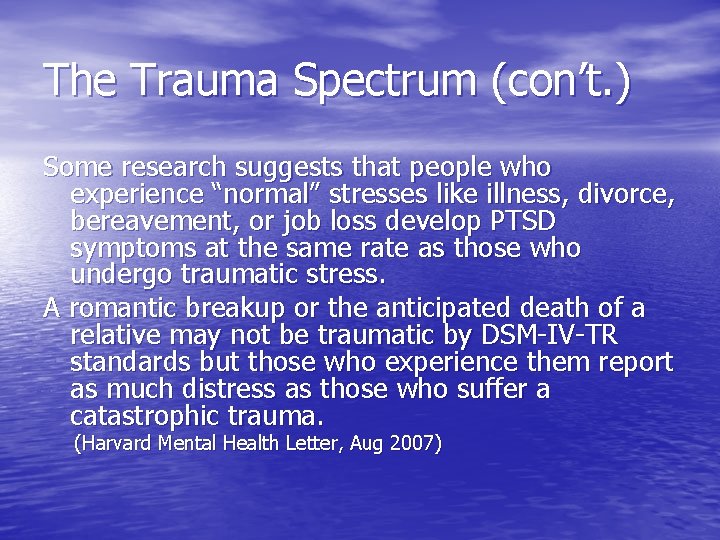
The Trauma Spectrum (con’t. ) Some research suggests that people who experience “normal” stresses like illness, divorce, bereavement, or job loss develop PTSD symptoms at the same rate as those who undergo traumatic stress. A romantic breakup or the anticipated death of a relative may not be traumatic by DSM-IV-TR standards but those who experience them report as much distress as those who suffer a catastrophic trauma. (Harvard Mental Health Letter, Aug 2007)
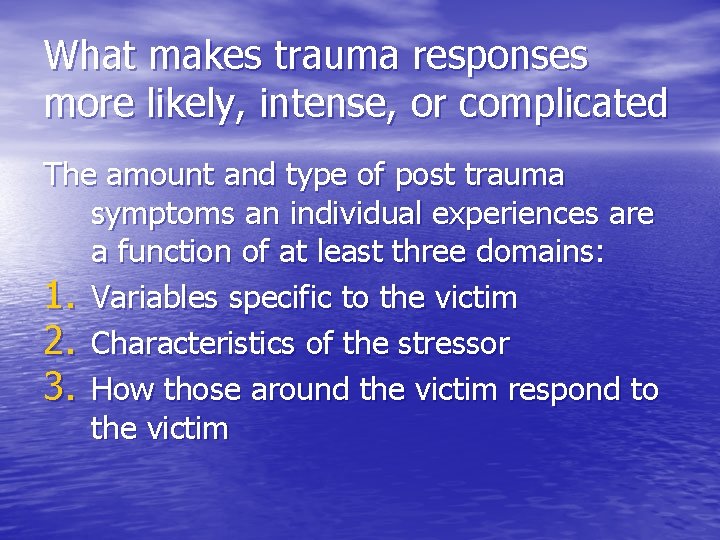
What makes trauma responses more likely, intense, or complicated The amount and type of post trauma symptoms an individual experiences are a function of at least three domains: 1. Variables specific to the victim 2. Characteristics of the stressor 3. How those around the victim respond to the victim
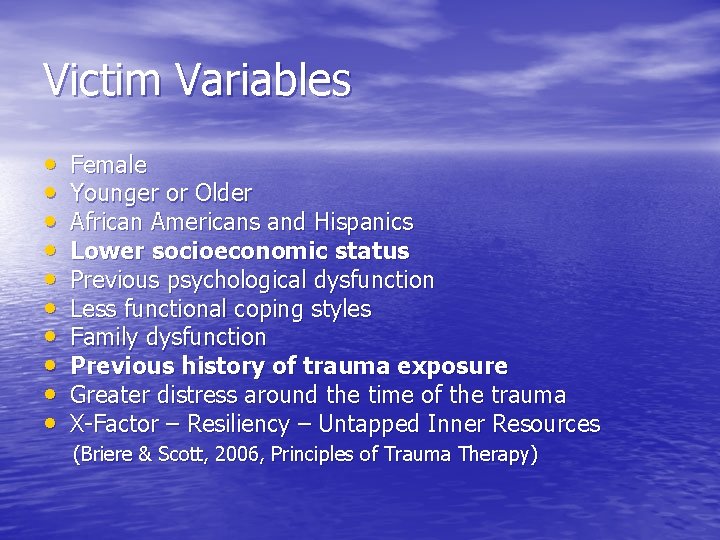
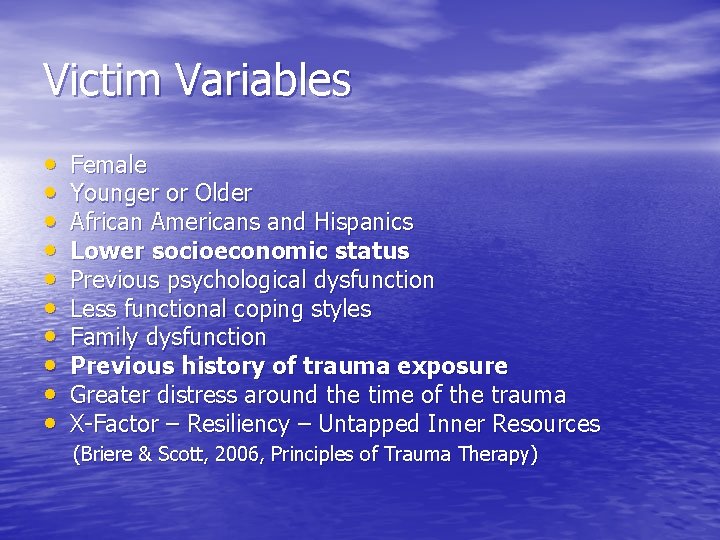
Victim Variables • • • Female Younger or Older African Americans and Hispanics Lower socioeconomic status Previous psychological dysfunction Less functional coping styles Family dysfunction Previous history of trauma exposure Greater distress around the time of the trauma X-Factor – Resiliency – Untapped Inner Resources (Briere & Scott, 2006, Principles of Trauma Therapy)
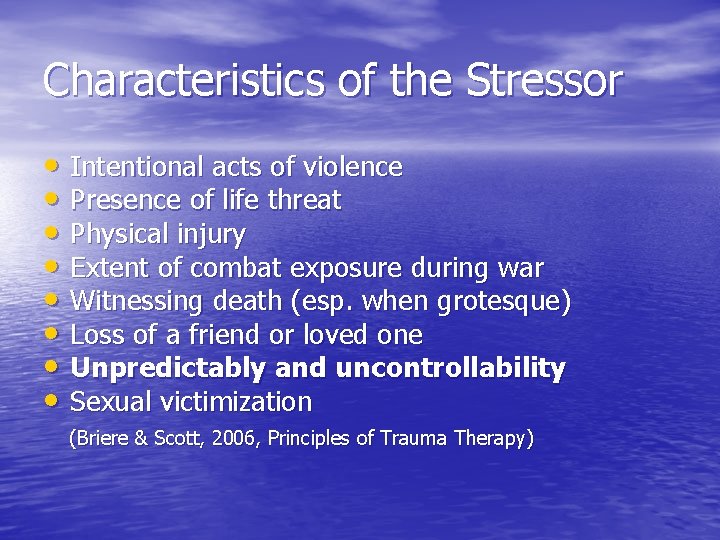
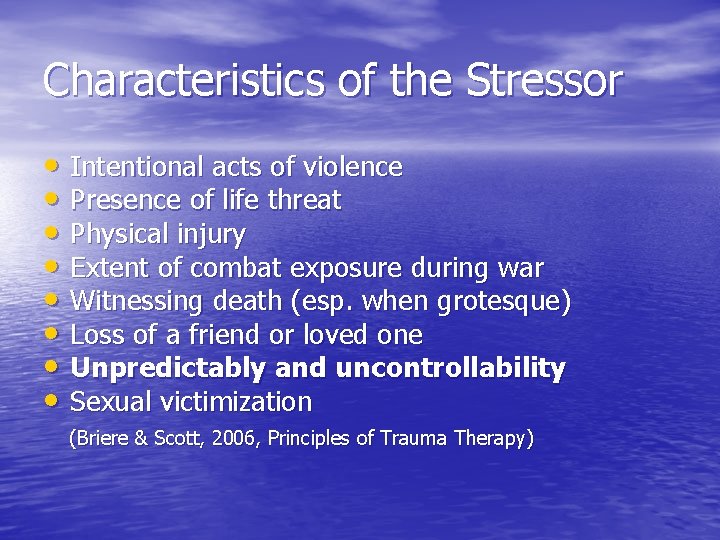
Characteristics of the Stressor • Intentional acts of violence • Presence of life threat • Physical injury • Extent of combat exposure during war • Witnessing death (esp. when grotesque) • Loss of a friend or loved one • Unpredictably and uncontrollability • Sexual victimization (Briere & Scott, 2006, Principles of Trauma Therapy)
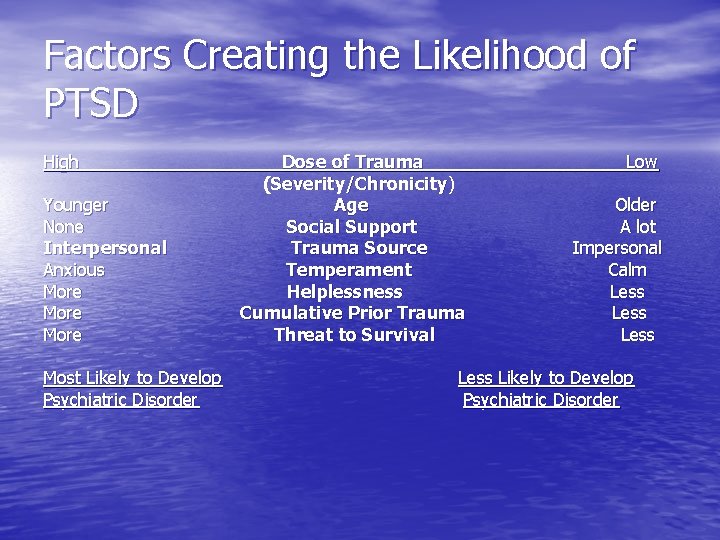
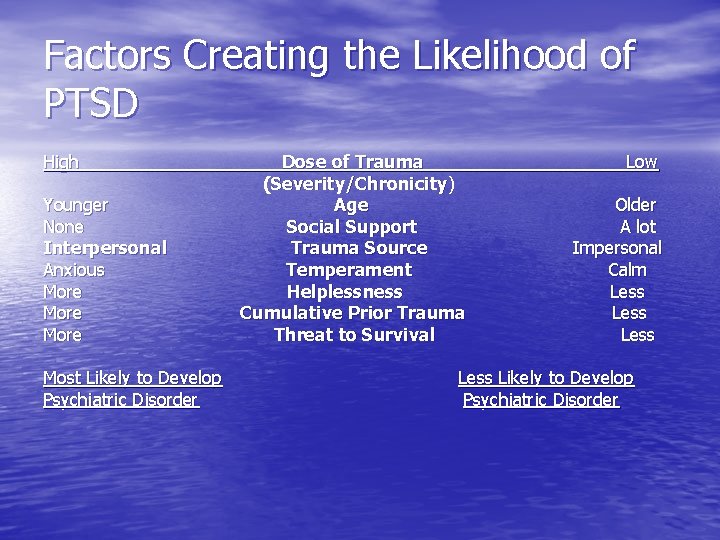
Factors Creating the Likelihood of PTSD High Younger None Interpersonal Anxious More Most Likely to Develop Psychiatric Disorder Dose of Trauma (Severity/Chronicity) Age Social Support Trauma Source Temperament Helplessness Cumulative Prior Trauma Threat to Survival Low Older A lot Impersonal Calm Less Likely to Develop Psychiatric Disorder
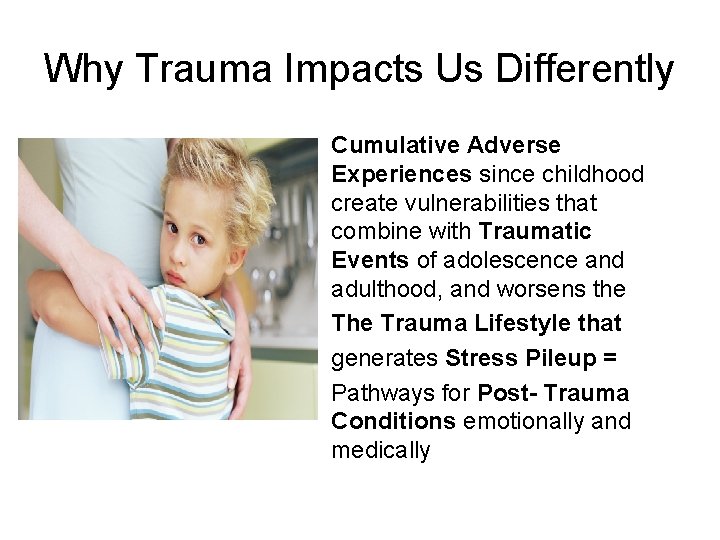
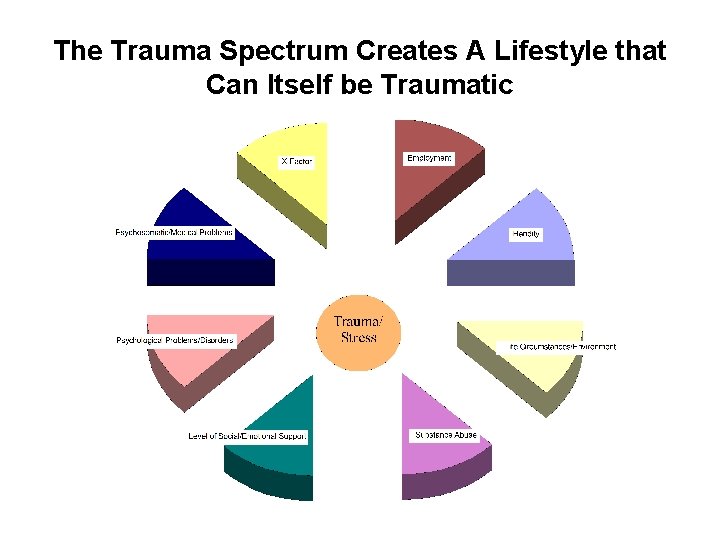
Why Trauma Impacts Us Differently Cumulative Adverse Experiences since childhood create vulnerabilities that combine with Traumatic Events of adolescence and adulthood, and worsens the Trauma Lifestyle that generates Stress Pileup = Pathways for Post- Trauma Conditions emotionally and medically
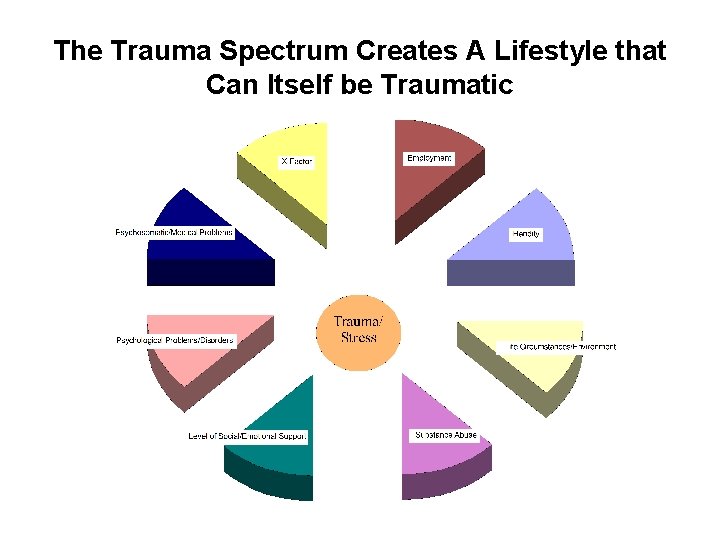
The Trauma Spectrum Creates A Lifestyle that Can Itself be Traumatic
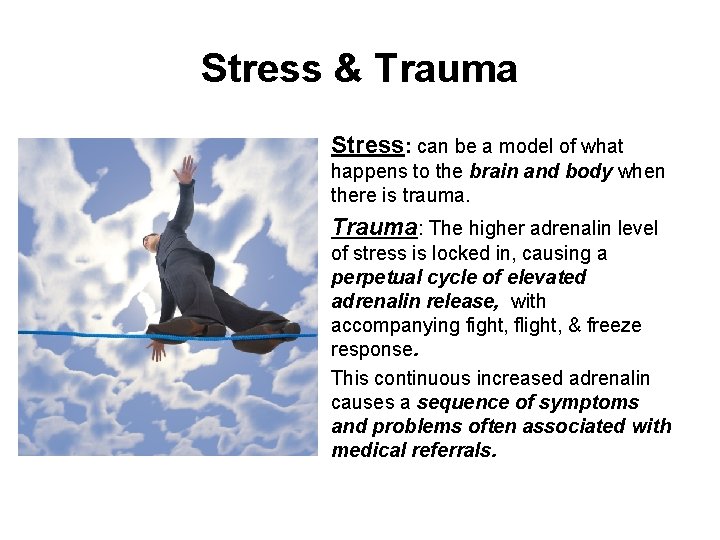
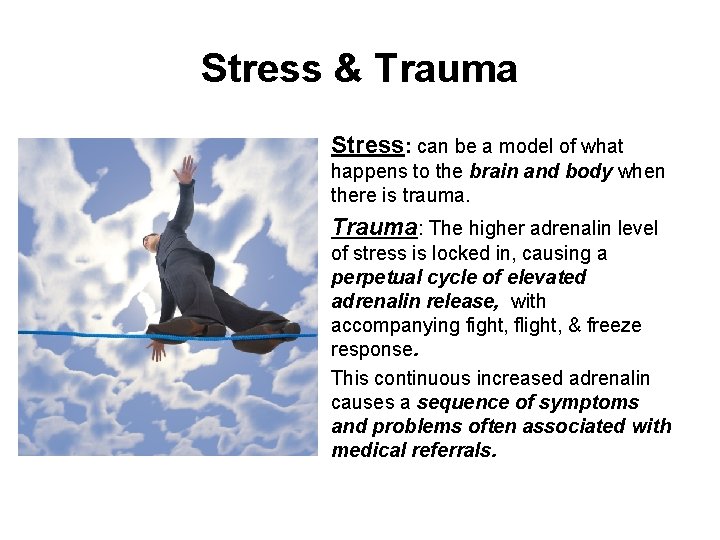
Stress & Trauma Stress: can be a model of what happens to the brain and body when there is trauma. Trauma: The higher adrenalin level of stress is locked in, causing a perpetual cycle of elevated adrenalin release, with accompanying fight, flight, & freeze response. This continuous increased adrenalin causes a sequence of symptoms and problems often associated with medical referrals.
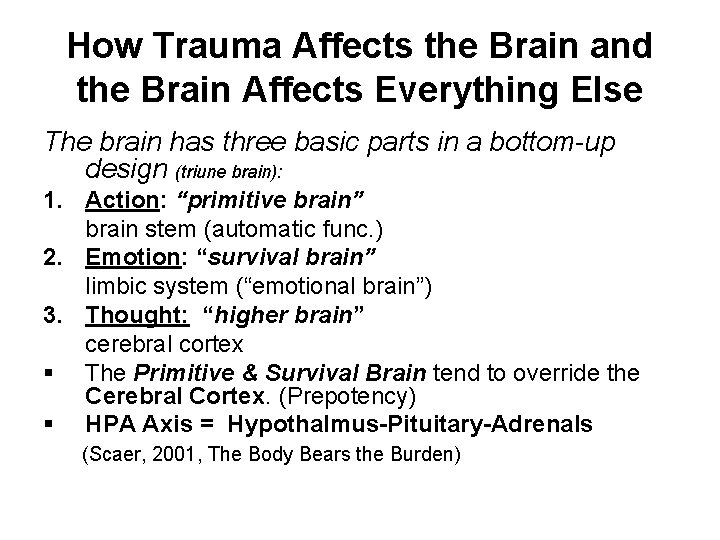
How Trauma Affects the Brain and the Brain Affects Everything Else The brain has three basic parts in a bottom-up design (triune brain): 1. Action: “primitive brain” brain stem (automatic func. ) 2. Emotion: “survival brain” limbic system (“emotional brain”) 3. Thought: “higher brain” cerebral cortex § The Primitive & Survival Brain tend to override the Cerebral Cortex. (Prepotency) § HPA Axis = Hypothalmus-Pituitary-Adrenals (Scaer, 2001, The Body Bears the Burden)
Stress & Trauma (con’t. ) Perpetual High Levels of Adrenalin: Like having a car in drive, with the accelerator and brake to the floor. The major organ systems of the body wear out Chronic fatigue and chronic pain sets in. The survivor’s long term ability to function is undermined. Depression results from sustained, unresolvable stress.
Adverse Childhood Experience ACE Study (Felittti, V. , 1998) A strong and consistent relationship between level of exposure of childhood emotional, physical or sexual abuse, and household dysfunction and. . . Adult health risk behavior and disease in adulthood Multiple categories of trauma exposure create multiple risk factors later in life and lead to early death. Childhood traumas are one of the basic causes of disease and death in adult life.
Medical Impact of Trauma • Ten Health Risk Factors Studied (these are the leading contributors to the major causes of death and disease) 1. Smoking 2. Severe Obesity 3. Physical inactivity partners 4. Depressed mood 5. Suicide Attempts 6. Alcoholism 7. Any drug abuse 8. Parental drug abuse 9. High lifetime number of sexual partners (> or = to 50) 10. History of having a sexually transmitted disease
Medical Impact of Trauma • Major Causes of Disease and Death 1. Heart disease 2. Cancer 3. Stroke 4. Respiratory Diseases 5. Accidents 6. Pneumonia and Influenza 7. Diabetes 8. Suicide 9. Kidney Disease 10. Liver Disease
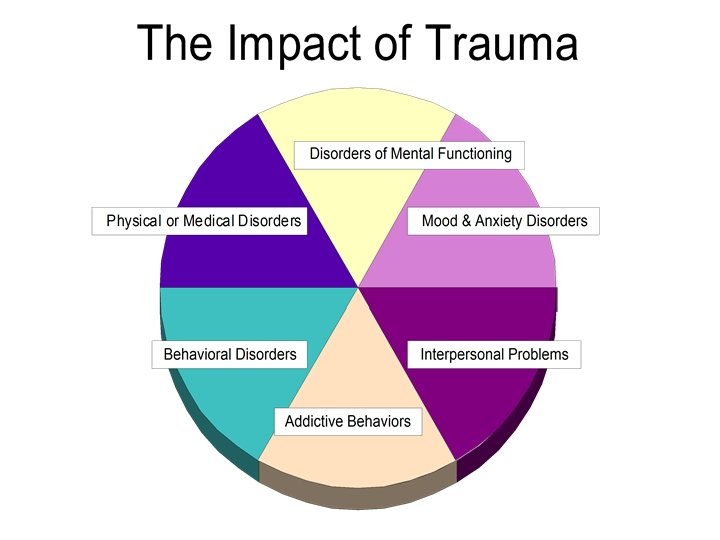
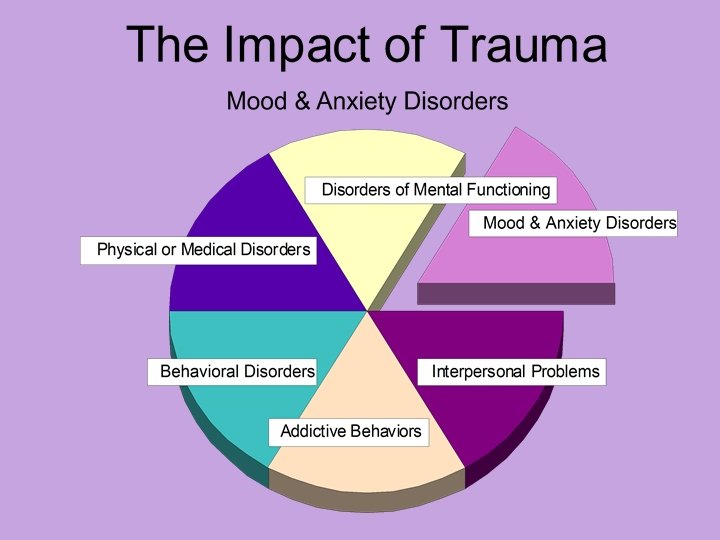
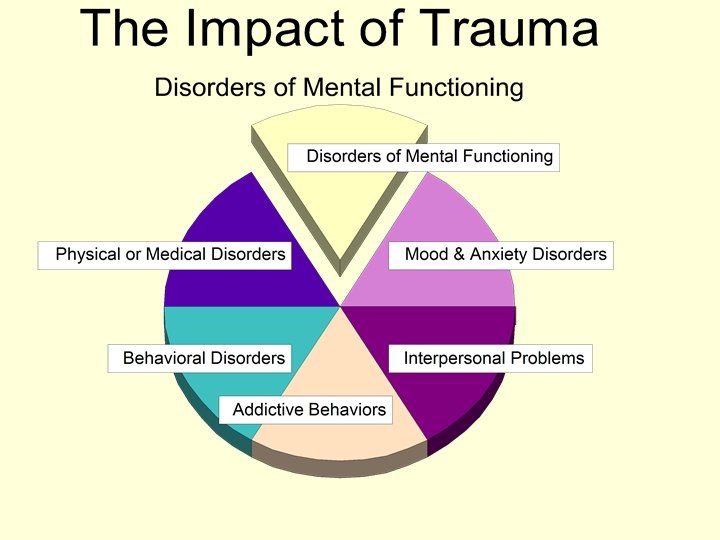
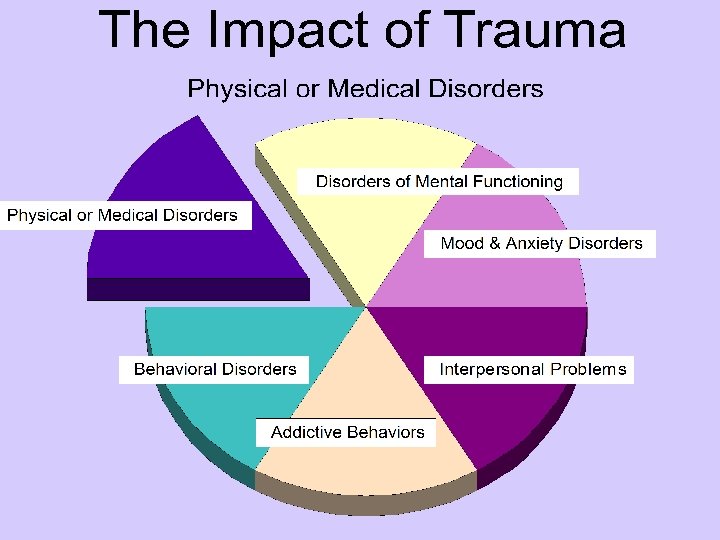
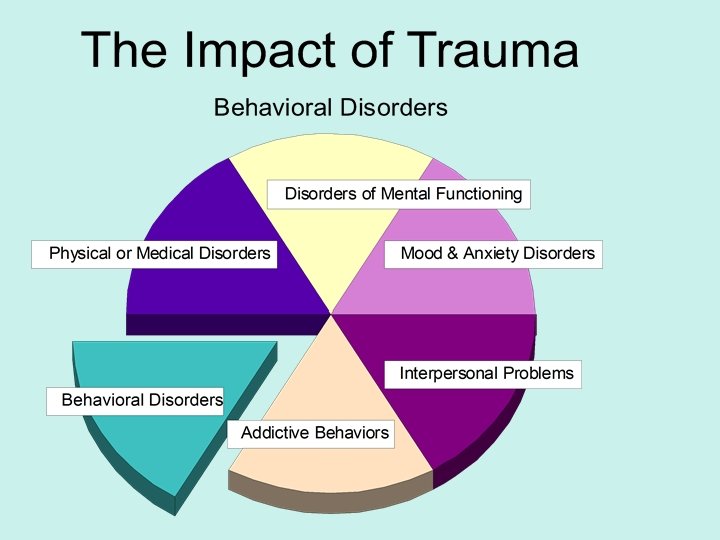
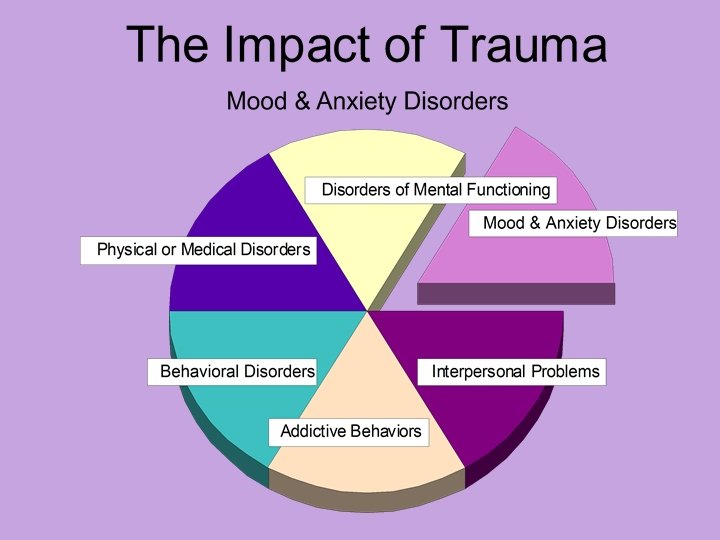
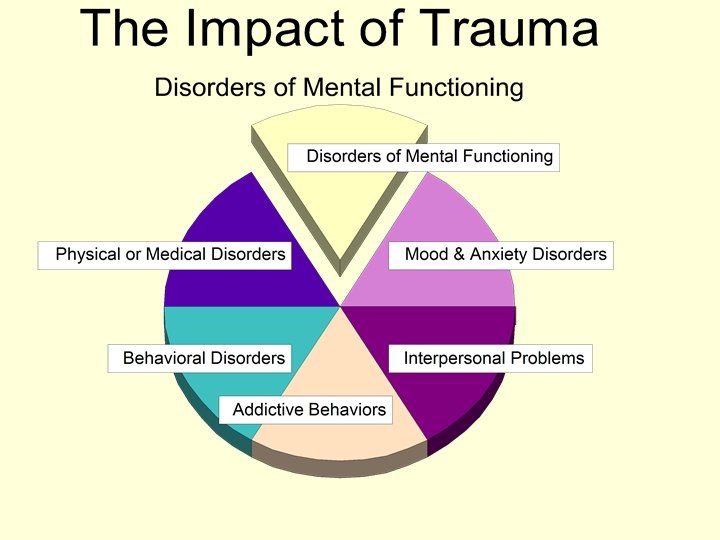
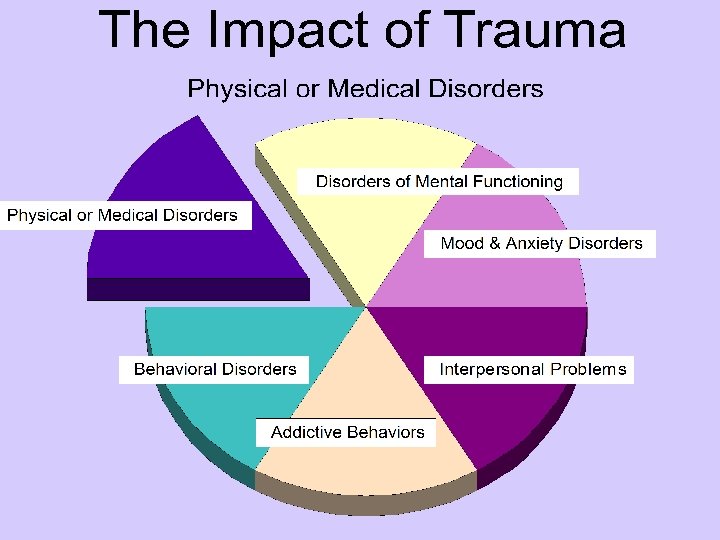
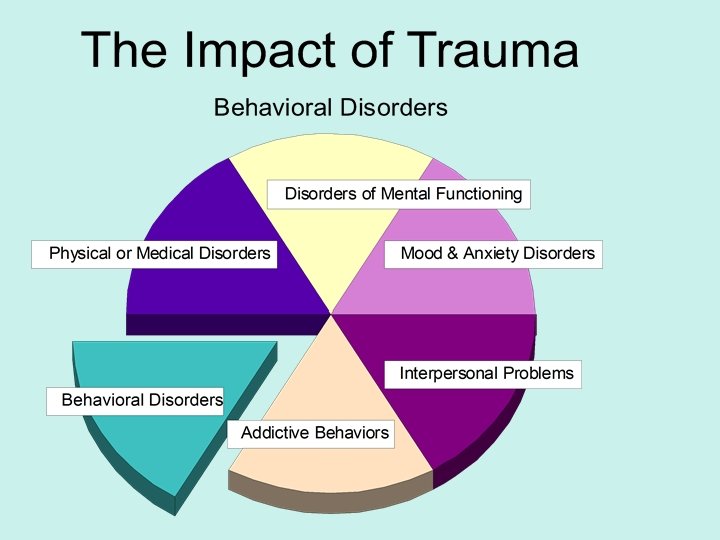
The Impact of Trauma Like the hub of a wheel, psychological trauma can generate multiple disorders. Depression & Anxiety are primary (80%) when there is PTSD Most clients have multiple disorders:
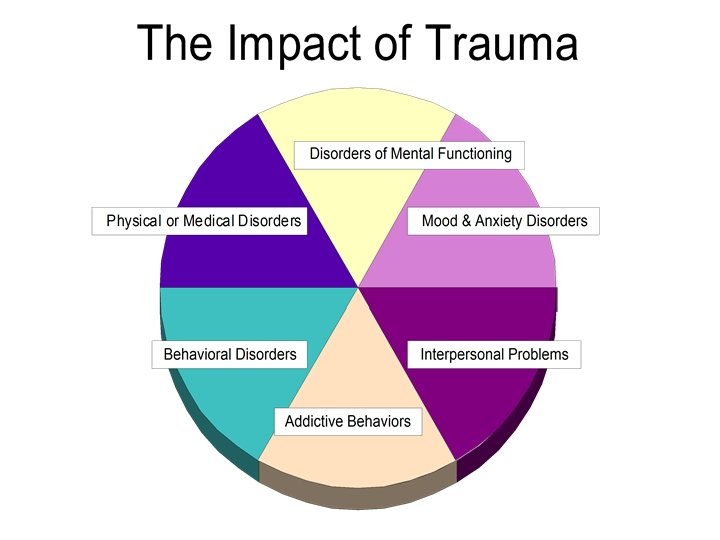
Considerable Co-Morbidity in Cases We have discovered over the last 16 years that reducing the trauma core brings simultaneous relief to a number of co-existing problems and improves ability to function
The Trauma Core can have many different “heads”

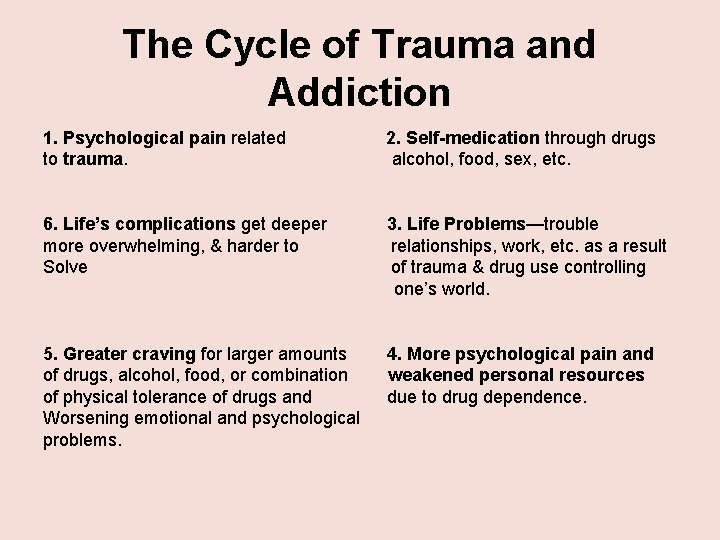
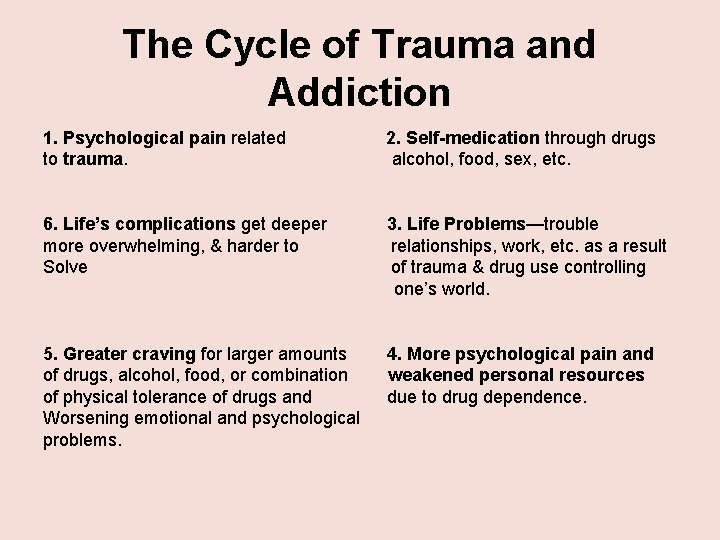
The Cycle of Trauma and Addiction 1. Psychological pain related to trauma. 2. Self-medication through drugs alcohol, food, sex, etc. 6. Life’s complications get deeper more overwhelming, & harder to Solve 3. Life Problems—trouble relationships, work, etc. as a result of trauma & drug use controlling one’s world. 5. Greater craving for larger amounts of drugs, alcohol, food, or combination of physical tolerance of drugs and Worsening emotional and psychological problems. 4. More psychological pain and weakened personal resources due to drug dependence.
A self-destructive cycle develops in which trauma’s psychological pain leads to:
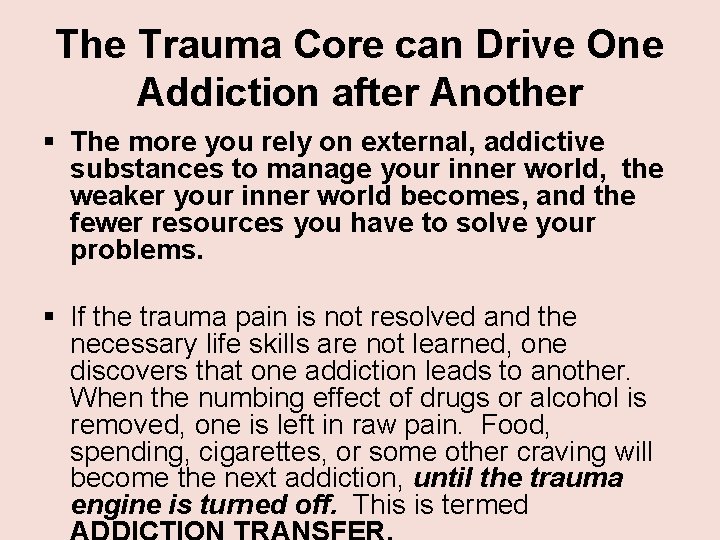
The Trauma Core can Drive One Addiction after Another § The more you rely on external, addictive substances to manage your inner world, the weaker your inner world becomes, and the fewer resources you have to solve your problems. § If the trauma pain is not resolved and the necessary life skills are not learned, one discovers that one addiction leads to another. When the numbing effect of drugs or alcohol is removed, one is left in raw pain. Food, spending, cigarettes, or some other craving will become the next addiction, until the trauma engine is turned off. This is termed

Why Trauma & Depression Often Co-exist 1. According to DSM-IV, A traumatic event entails a person experiencing or witnessing an event that threatens death or serious injury & the person’s response involves intense fear, helplessness, or horror. Helplessness is a key feature of depression.
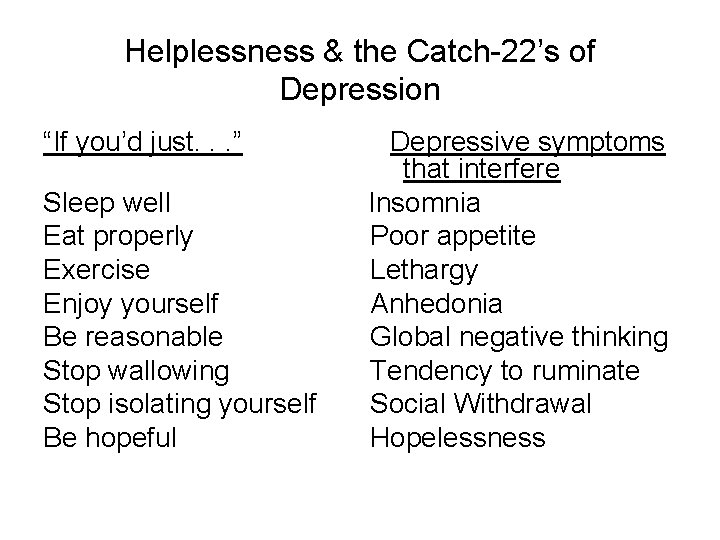
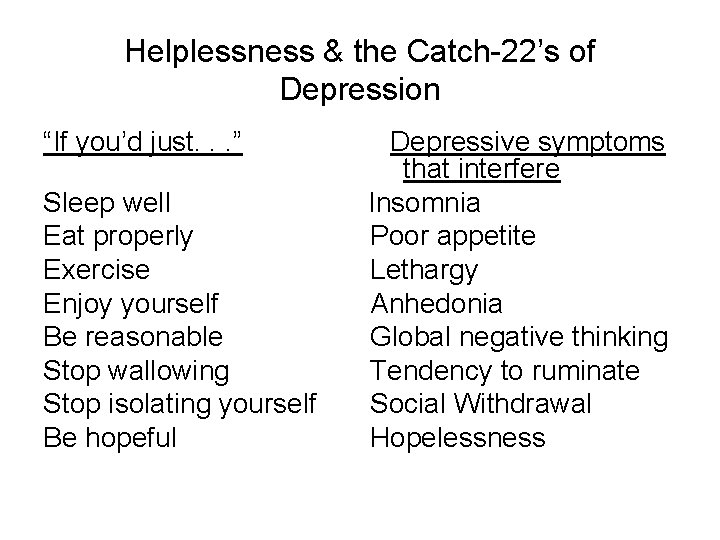
Helplessness & the Catch-22’s of Depression “If you’d just. . . ” Sleep well Eat properly Exercise Enjoy yourself Be reasonable Stop wallowing Stop isolating yourself Be hopeful Depressive symptoms that interfere Insomnia Poor appetite Lethargy Anhedonia Global negative thinking Tendency to ruminate Social Withdrawal Hopelessness
Why Trauma & Depression Often Co-exist 2. The defining symptom of PTSD are intrusive experiences: • flashbacks of the traumatic event • nightmares • internal or external cues that trigger the traumatic event. Intrusive experiences reinforce the original helplessness of the traumatic event.

Why Trauma & Depression Often Co-exist 3. Avoidance of anything associated with the trauma and numbing responsiveness associate with the intrusive experiences. Efforts to avoid conversations, activities, places or people associated with the trauma; Diminished interest or participation; Feelings of detachment or alienation from others; Restricted range of affect (i. e. , absence of loving feelings); Sense of foreshortened future (e. g. does not expect to have a career, marriage, children, or normal life span). The PTSD avoidance and numbing symptoms are inherent in Major Depression
Why Trauma & Depression Often Co-exist 4. In addition to the avoidance and numbing there is an increased arousal manifested in: Difficulty falling asleep or staying asleep Irritability or outbursts of anger, Difficulty concentrating, Hyper-vigilance Heightened startle response The distress and impairment in social, occupational, or other areas of functioning are integral to depression. Sleep is a major element of impairment
Self-Defeating Sleep Cycles of PTSD & Depession • Like flashbacks, nightmares may be replicas of traumatic experience • Yet nightmares may express emotional impact of trauma metaphorically • Both nightmares and flashbacks keep trauma memory networks primed escalating in vicious cycles • PTSD anxiety/hyperarousal interferes w/ sleep • Abnormal movements of reliving trauma exper. • Fear of nightmares prevent deep sleep-sleep phobias • Nocturnal panic Improving Sleep a Central Tx Focus (Mc. Kenna, P. 2009)
Why Trauma & Depression Often Co-exist 5. The experience of trauma over a lifetime creates inner conditions that spawn chronic, debilitating diseases unexplainable by current concepts of health and disease. Chronic diseases make up the majority of symptoms causing doctor visits, and contribute significantly to depression.
Why Trauma & Depression Often Co-exist 6. Self Medication is a common feature of PTSD highly correlated with depression. Around 65% of substance abusers have trauma back-grounds. This fits self-medication model. Another 35% have trauma experiences while using drugs. D&A contribute to Avoidance & Numbing Research shows depression and D&A are often in a cyclic relationship
Why Trauma & Depression Often Co-exist 7. Complex PTSD (Developmental Trauma Disorder – van der Kolk • Dysregulation in Presence to Trauma Cues (affective, somatic, relational, cognitive, behavioral, self-attribution) • Persistently Altered Attributions (Negative self-attribution, distrust, loss of expectation of protection and help, inevitability of future victimization) • Functional Impairment (Educational, familial, peer, legal, • Identity, Boundary, Personal Connection Issues vocational)
Why Trauma & Depression Often Co-exist Trauma often leads to a loss of meaning which is the essence of “existential depression. ” Key element is helplessness, loss of control Existential Depression = conviction life is meaningless/no importance in anything one does. 8.
Why Trauma & Depression Often Co-exist On the Other Side of Existential Depression • Wisdom in the wound that leads to deeper lifeparticipations, to more becoming. • There is a natural human tendency to downsize life to feel safe using denial. Thru inner work a more realistic connection with life can be made. • Trauma overwhelms the ego’s illusion of omnipotence & allows more of its functioning to be replaced by the deeper self. • Empathy is created out of pain that is embraced. • The weakest links in our identity must be replaced, changed, grown. (Grant, 1996, The Way of the Wound)
Why Trauma & Depression Often Co-exist 9. Social/Emotional Support – Angry or inappropriate reactions may drive away tenuous but needed support. Self-sabotage (driven by unconscious causes) is common. Interpersonal problems are a primary feature of PTSD & Depression
Treatment Considerations 1. Intake Assessment should include symptom clusters associated with trauma: somatic, anxiety, depression, anger, sleep problems, addictions, interpersonal issues, thought disorders, bipolar, ADD, intrusive symptoms, dissociation (traumaawareness. org) Also include a non-invasive way to identify childhood and adult traumas. Measure dissociation with Dissociative Experience Scale (DES). (traumaawareness. org)
Treatment Considerations 2. Psycho-Education: If trauma is present provide basic information about trauma. Include trauma sources, four elements of PTSD, two categories of trauma-simple & complex, 3 brains. Explain the relationship of trauma and depression. See “trauma brochure” at (traumaawareness. org) Client learns to “normalize” her trauma responses and symptoms
Treatment Considerations 3. Client learns to develop and utilize inner resources and strengths. Goal: Client learns to use the principle: “The same strengths required to survive traumatic experiences can be used to overcome the effects of the trauma”
Discovering Personal Strengths As a child I dreamed: My dream now is: My childhood strengths were (artistic ability, sense of humor, sensitivity, etc. ) My strengths now are: I felt happy when: I felt strong when: Three things that mattered most to me in the past are: As a child, when I was sad or upset I turned to: A parent A sibling A peer A teacher A grandparent A neighbor/Family Friend Member of my religious faith Kept to myself The family pet A toy or object T. V. Other Before 16, I felt the most comfort from involvement with: People Animals Nature God Art Reading Dance Music Writing Athletics Other
Treatment Considerations Developing Inner Resources Reasons People Don’t Let Go of Their Pain: Premature forgiveness of offender/ It’s my identity/Shame & Unworthiness/ It’s my punishment/Fear of a new life/Fear of ___ Pain is a source of strength/It’s a friend/ It’s a distraction/A way to avoid responsibility/A way to avoid people/It’s a way of life/It’s an escape/What if I’m whole & still not good enough? /How do I fill the void? Refer to “Why People Don’t Let Go of Pain” traumaawareness. org
Treatment Considerations 4. Follow the organization of the brain when resolving trauma. In addition to the general pain removal, the client can resolve significant, specific traumatic events, such as an assault or violent act that requires focused treatment
Treatment Considerations Following the Organization of the Brain (con’t. ) • Research by Charcot, Janet, and Freud demonstrates the powerful reality that trauma pain is stored in the sub-conscious. Research in recent years indicates trauma pain is stored throughout the body- e. g. , “tissue memory. ” • The Limbic System interfaces with the subconscious. Pain removal is more basic to healing than memory narration. The subconscious has many avenues for pain removal. • Research ego states, body memory, energy work.
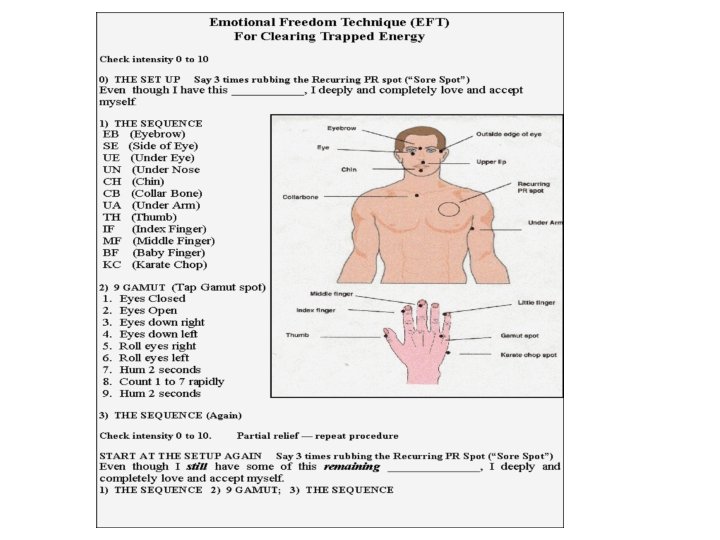
EFT Continued • Try it on just about anything: Emotional Problems, Physical Problems, Overcoming Unhealthy Cravings, Changing bad habits. • For detailed training go to http: //emofree. com/ to download a free manual and sign up for a weekly newsletter.
COME TO YOUR SENSES • Bridging is being in the moment and connecting with your senses in a way that quiets the mind. As you bridge, your awareness expands since you are getting away from your busy and distracting mind. • As you learn to bridge you can neutralize your “Identity System” which contains worry, clutter and noise. (Block, S. 2005, “Come to Your Senses”)
Treatment Considerations 5. CBT should generally follow trauma resolution methods It is more effective to resolve the Core of trauma before other interventions Trauma Tx Should not Depend on Language A trauma brain is right brain not left brain With the mid and primitive brains quieted the cerebral cortex is more receptive to change dysfunctional thinking.
Treatment Considerations 6. Life Skills enhancement is essential when there is trauma and depression. HEALTHY CONTROL ASSERTIVENESS EMPOWERMENT Transactional Analysis with the Parent. Adult-Child paradigm is useful. “Letting Go” of unhealthy relationships is usually inevitable (There are practical considerations).
Treatment Considerations Life Skill Enhancement (con’t. ) Life skill enhancement in the physical realm promotes mental/emotional healing Traumatized people need to have physical sensory experience to: 1. Unlock bodies 2. Activate effective fight/flight 3. Tolerate their sensations 4. Befriend their inner experiences 5. Activate new action patterns (rewire circuits) (van der Kolk, B. 2007, Presentation)
Treatment Considerations Life Skill Enhancement (con’t. ) • • As part of the Life Skills Package remember NATURAL SEROTONIN (traumaawareness. org) Nutritious Food (Pratt, 2004, Superfoods) Nature Exercise Food for the Mind- Literature (find your vein) Connection through Contribution Mini-Vacations (traumaawareness. org) Assert what Matters to You Keep a Journal
Treatment Considerations 7. Harnessing the Powers of the Sub. Conscious can be an effective way to Solve Life’s Problems. Clients can learn to use their sub-conscious for selfempowerment, changing bad habits and addictions, acquiring social skills, mood management, solving problems, and reducing stress and health problems.
Treatment Considerations 8. Always give the Client Hope Involving the 3 Brains in the Healing Process Connects the Client with her heart That’s where courage and hope is found
Review of Tx Considerations Phase 1: BRAIN STEM 1. Grounding 2. Cardio exercise to change biochemistry 3. Sensory experience to unlock bodies, tolerate sensations, befriend inner experience. 4. Use body to overcome powerlessness. 5. Calm animal brain down-be in present. 6. Purposeful action 7. Yoga and Meditation-major pathway to animal brain
Review of Tx Considerations Phase 2 MID-BRAIN Chronic Complex -Pain release via body work & subconscious Single Incident- EMD/R, TFT. . . & Journaling, Art, Sand Tray, Psycho-drama. . Learn to have a memory instead of being a memory
Review of Tx Considerations Phase 3 PREFRONTAL CORTEX • Cognitive Behavioral Therapy(CBT) • Use the human capacity to create new realities-creativity and reason • Challenge the neural grooves by seeking new experience
Importance of Reaching the traumatized who are deeply depressed “The tragedy is the loneliness; the inability to convey the inner experience and knowing that I cannot get out of it without going through it again. ”
LIFE IS NOT ABOUT ACHIEVING IT’S ABOUT OVERCOMING