Manifestation of Novel Social Challenges of the European

- Slides: 22

Manifestation of Novel Social Challenges of the European Union in the Teaching Material of Medical Biotechnology Master’s Programmes at the University of Pécs and at the University of Debrecen Identification number: TÁMOP-4. 1. 2 -08/1/A-2009 -0011
Manifestation of Novel Social Challenges of the European Union in the Teaching Material of Medical Biotechnology Master’s Programmes at the University of Pécs and at the University of Debrecen Identification number: TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Gyula Bakó and Erika Pétervári Molecular and Clinical Basics of Gerontology – Lecture 6 DISORDERS AND DISEASES OF LOCOMOTOR ORGANS PART 1
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Outline • Changes of the musculoskeletal system in the elderly • Common diseases of locomotor organs in the elderly – causes of falls, chronic immobilization and disability • Immobilization and remobilization in the elderly
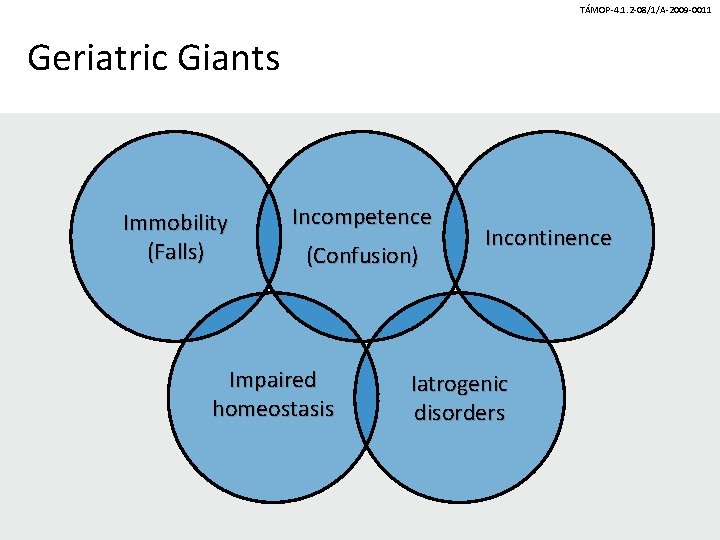
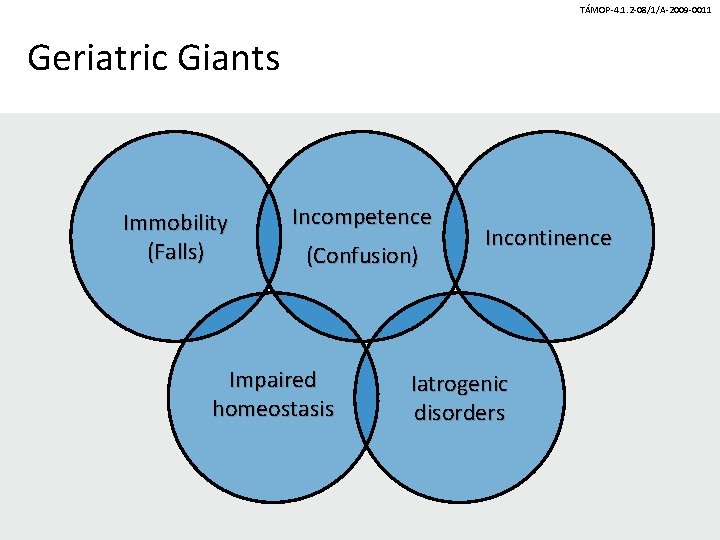
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Geriatric Giants Immobility (Falls) Incompetence (Confusion) Impaired homeostasis Incontinence Iatrogenic disorders
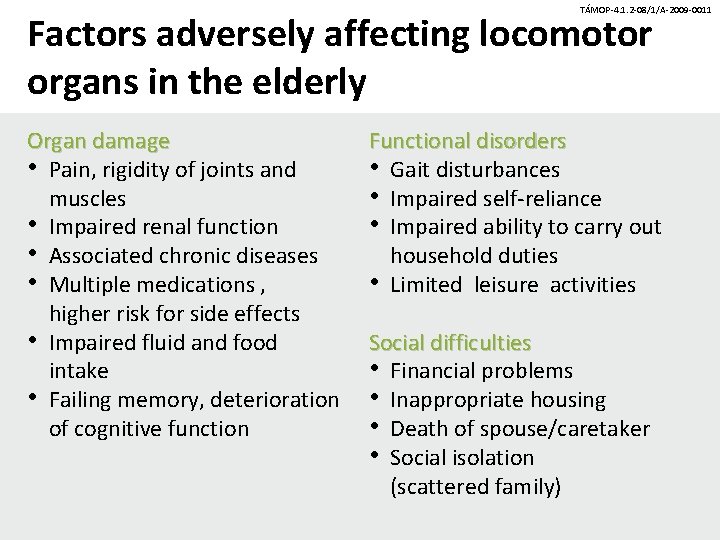
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Factors adversely affecting locomotor organs in the elderly Organ damage • Pain, rigidity of joints and muscles • Impaired renal function • Associated chronic diseases • Multiple medications , higher risk for side effects • Impaired fluid and food intake • Failing memory, deterioration of cognitive function Functional disorders • Gait disturbances • Impaired self-reliance • Impaired ability to carry out household duties • Limited leisure activities Social difficulties • Financial problems • Inappropriate housing • Death of spouse/caretaker • Social isolation (scattered family)
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Changes of the musculoskeletal system in the elderly IChanges and dysfunction of the skeletal muscles in the elderly IIAging-associated changes in the joints IIIAging-associated changes in the bones
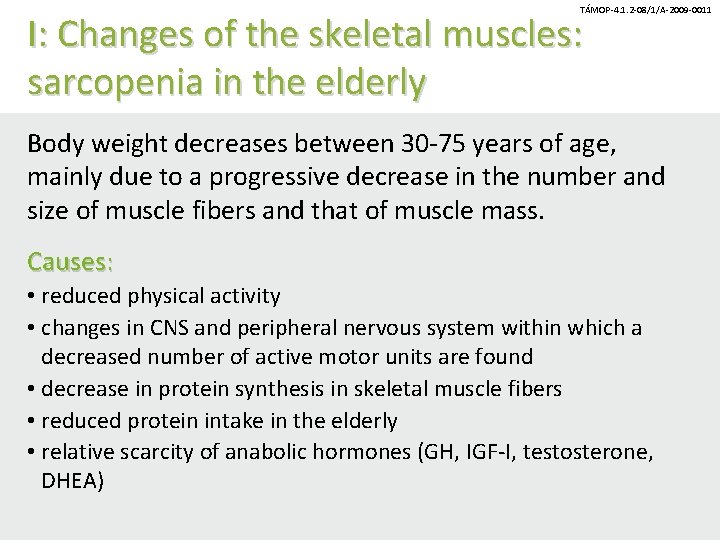
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 I: Changes of the skeletal muscles: sarcopenia in the elderly Body weight decreases between 30 -75 years of age, mainly due to a progressive decrease in the number and size of muscle fibers and that of muscle mass. Causes: • reduced physical activity • changes in CNS and peripheral nervous system within which a decreased number of active motor units are found • decrease in protein synthesis in skeletal muscle fibers • reduced protein intake in the elderly • relative scarcity of anabolic hormones (GH, IGF-I, testosterone, DHEA)
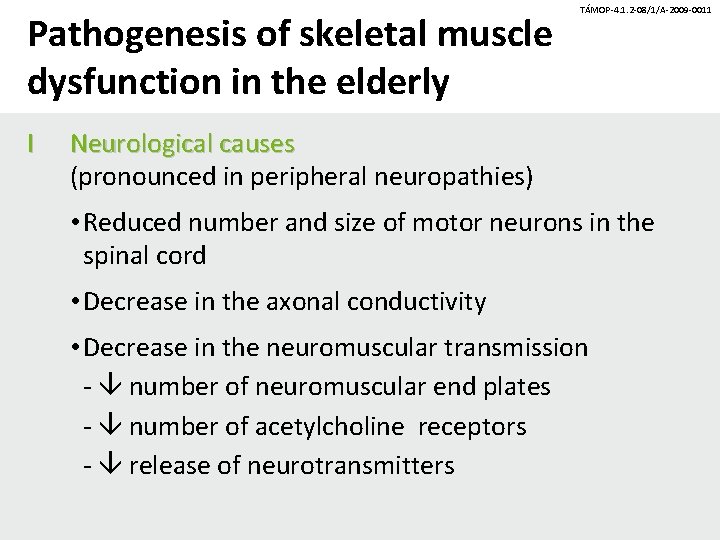
Pathogenesis of skeletal muscle dysfunction in the elderly I TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Neurological causes (pronounced in peripheral neuropathies) • Reduced number and size of motor neurons in the spinal cord • Decrease in the axonal conductivity • Decrease in the neuromuscular transmission - number of neuromuscular end plates - number of acetylcholine receptors - release of neurotransmitters
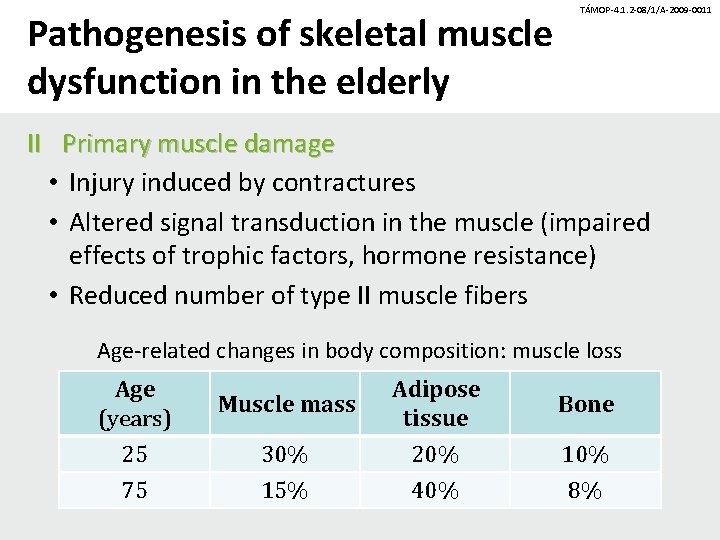
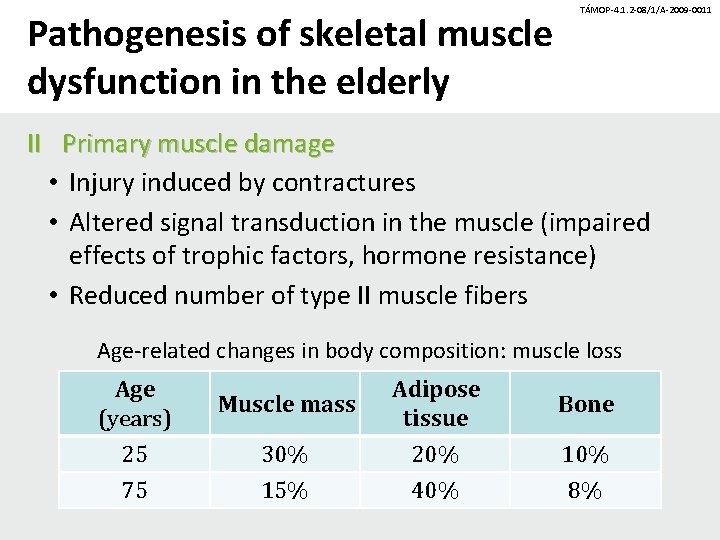
Pathogenesis of skeletal muscle dysfunction in the elderly TÁMOP-4. 1. 2 -08/1/A-2009 -0011 II Primary muscle damage • Injury induced by contractures • Altered signal transduction in the muscle (impaired effects of trophic factors, hormone resistance) • Reduced number of type II muscle fibers Age-related changes in body composition: muscle loss Age (years) Muscle mass Adipose tissue Bone 25 75 30% 15% 20% 40% 10% 8%
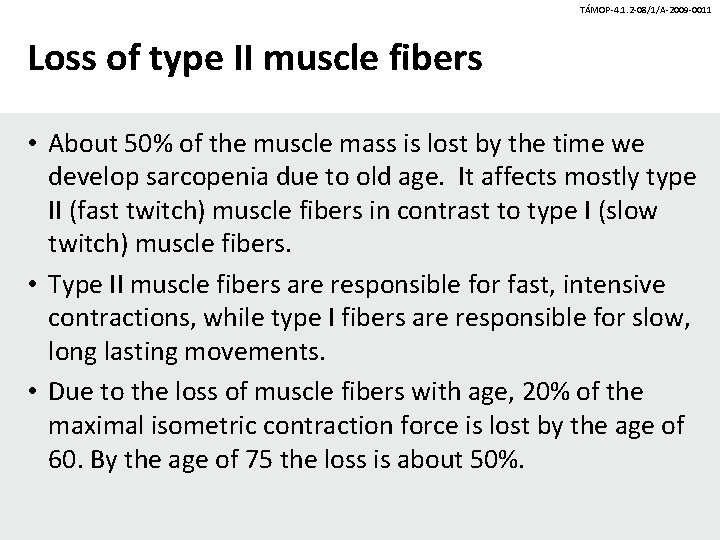
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Loss of type II muscle fibers • About 50% of the muscle mass is lost by the time we develop sarcopenia due to old age. It affects mostly type II (fast twitch) muscle fibers in contrast to type I (slow twitch) muscle fibers. • Type II muscle fibers are responsible for fast, intensive contractions, while type I fibers are responsible for slow, long lasting movements. • Due to the loss of muscle fibers with age, 20% of the maximal isometric contraction force is lost by the age of 60. By the age of 75 the loss is about 50%.
Pathogenesis of skeletal muscle dysfunction in the elderly (cont. ) TÁMOP-4. 1. 2 -08/1/A-2009 -0011 III Combined neuromuscular mechanisms • Disorders of the electric discharge of muscle fibers • The stimulus- contraction process is disrupted IV Common abnormal biochemical processes affecting the muscle • oxidative stress • mutation in the mitochondrial DNA • vasculopathies developing with age
II: Aging-associated changes in the joints TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Cartilage coating the bone endings contains chondrocytes, which produce collagen fibers, hyaluronic acid and proteoglycans building a high water-containing, elastic substance. The proteoglycans attached to hyaluronic acid and aggregated within the collagen network are saturated with water and thus provide the cartilage with the capacity to resist compression and to re-expand after compression. In the elderly, the amount and water content of the cartilage mass decrease, its resistance against mechanical impacts is less effective. Impacts from every direction destroy the joints as the ligaments become more rigid. (Overweight. )
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Aging of the joints arthrosis • water binding of hyaluronic acid • changed composition (not the amount) of proteoglycans Reduced water content (in arthrosis it increases) and amount of cartilage mass lead to less resilient cartilage. Without the protective effects of the proteoglycans, the collagen fibers of the cartilage become susceptible to degradation. • Decreased viscosity of the synovial fluid.
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Aging in soft tissues • Impairment of collagene synthesis, that of posttranslational modification of collagene • Alterations in the quantity and quality of intercellular matrix (menisci, intervertebral discs) • Deposition of calcium crystals in connective tissue Mechanical resistance of soft tissues are decreased
III: Aging-associated changes in the bones TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Bone mass decreases from the age of 55 by around 1%/year in men and by 3 -4%/year in women (peak bone mass is reached at 25 -35 years of age, its value is higher in men). During the course of aging metabolic activity of osteoblasts is decreasing. Causes of deterioration of bone mass: inactivity, vitamin D deficiency; hormones: estrogen, progesterone, calcitonin, parathormone (secondary hyperparathyroidism), cortisol; alcohol; smoking. Consequences: osteopenia, osteoporosis, fractures.
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Common diseases of locomotor organs in the elderly • Osteoarthrosis, Osteoarthrosis the most common disease of locomotor organs of people over 50 • Rheumatoid arthritis • Gout • CPPD arthritis (pseudo-gout) • Osteoporosis
Osteoarthrosis (OA) degenerative joint disease TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Definition: Each element of the joint becomes gradually and progressively injured causing swelling, pain, stiffness and functional loss. A degenerative process leads to incongruence of the articular cartilage surfaces, inflammation of the joint capsule (synovitis), muscle atrophy and a crackling noise (called “crepitus”) when the affected joint is moved. It commonly affects the large weight bearing joints (hips, knees).
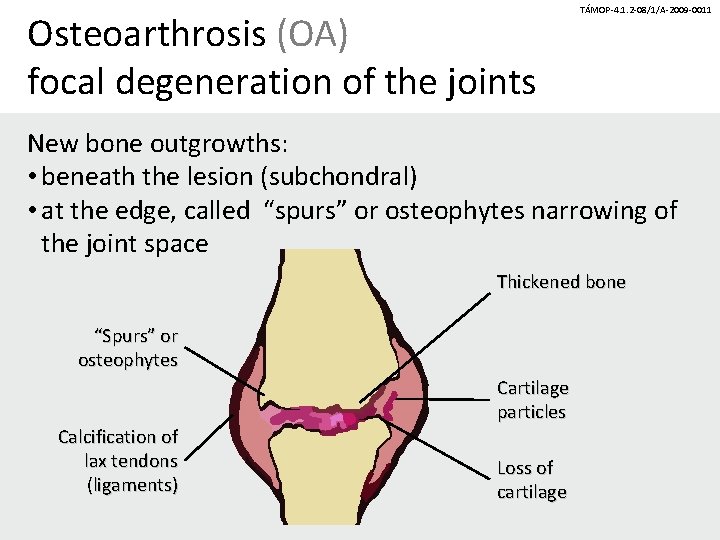
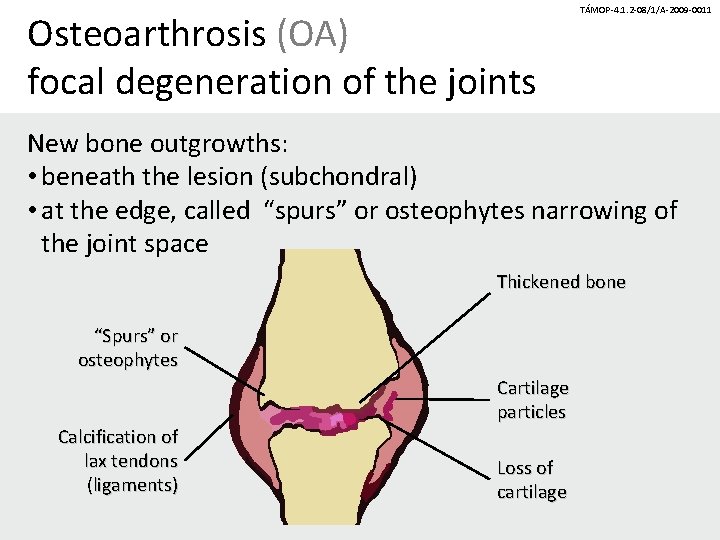
Osteoarthrosis (OA) focal degeneration of the joints TÁMOP-4. 1. 2 -08/1/A-2009 -0011 New bone outgrowths: • beneath the lesion (subchondral) • at the edge, called “spurs” or osteophytes narrowing of the joint space Thickened bone “Spurs” or osteophytes Calcification of lax tendons (ligaments) Cartilage particles Loss of cartilage
Osteoarthrosis (OA) degenerative joint disease TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Prevalence: It affects 30% of the adult population. 90% of people over 60 have radiological signs of arthrosis. Incidence: 88 (hip joints), 20 (knee), and 300 (hand)/100, 000/year Significance: It is the most common cause of disablement and NSAIDs’ (non-steroidal anti-inflammatory drugs) prescriptions.
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 OA a multifactorial degenerative joint disease Causes: Basic causes: • bipedalism (erect posture and work), increased burden on the joints at the knees • extended life span Risk factors for faster progression: • Mechanical causes: obesity, congenital disorders, macro- and microtrauma, overuse, previous inflammation of the joints and bone necrosis. • Metabolic causes: defects in collagen synthesis, diabetes, hyperthyroidism, hypothyroidism, hyperparathyroidism, hemochromatosis, acromegaly, ochronosis, etc.
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Clinical signs of OA • • • Usually above 40 years of age Moderate pain in one or more joints Pain at initiation of movement In the beginning, the pain ameliorates at rest, later it is aggravated by rest Morning stiffness < 30 minutes Impaired function: instability, diminished movements , decrease in muscle strength Crepitation, crackling noise Swelling, deformity Abnormal alteration of the axis Lack of systemic symptoms
TÁMOP-4. 1. 2 -08/1/A-2009 -0011 Therapeutic measures Pharmacological treatment • Pain killers/analgetics • NSAID • Intra-articular steroids Psycho-social treatment • Patient education • Improvement of life-style and diet • Psychological support • Patient clubs Weight reduction Consultations with patients Orthoses (amputee knee shell, knee brace, orthotic heel support, arch support ) Other treatments • Physiotherapy • Surgical intervention
 Newer drug delivery system
Newer drug delivery system Manifestation physique
Manifestation physique Manifestation commerciale exemple
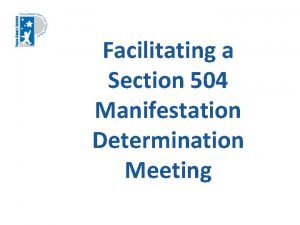
Manifestation commerciale exemple Manifestation determination meeting agenda
Manifestation determination meeting agenda Manifestation determination flowchart
Manifestation determination flowchart Manifestation determination flowchart
Manifestation determination flowchart Manifestation shamballa
Manifestation shamballa The manifestation of the holy spirit
The manifestation of the holy spirit Besoin fondamentaux de virginia henderson
Besoin fondamentaux de virginia henderson Manifestation determination process
Manifestation determination process Fault is manifestation of which defect
Fault is manifestation of which defect Manifestation names
Manifestation names Hepatomogaly
Hepatomogaly Colossians 1:17-19
Colossians 1:17-19 Cchf
Cchf Vocabulaire manifestation
Vocabulaire manifestation Manifestation of sunnatullah
Manifestation of sunnatullah Friday manifestation
Friday manifestation Scabies clinical manifestation
Scabies clinical manifestation Apa itu social thinking
Apa itu social thinking Social thinking social influence social relations
Social thinking social influence social relations Social challenges
Social challenges Social challenges
Social challenges