Manajemen Gangguan Pertukaran Gas Gangguan pertukaran gas adalah


- Slides: 56
Manajemen Gangguan Pertukaran Gas
• Gangguan pertukaran gas adalah kelebihan dan kekurangan oksigen dan/ atau eliminasi karbondioksida di membrane kapiler-alveolar. (Zul Dahlan, 2000)
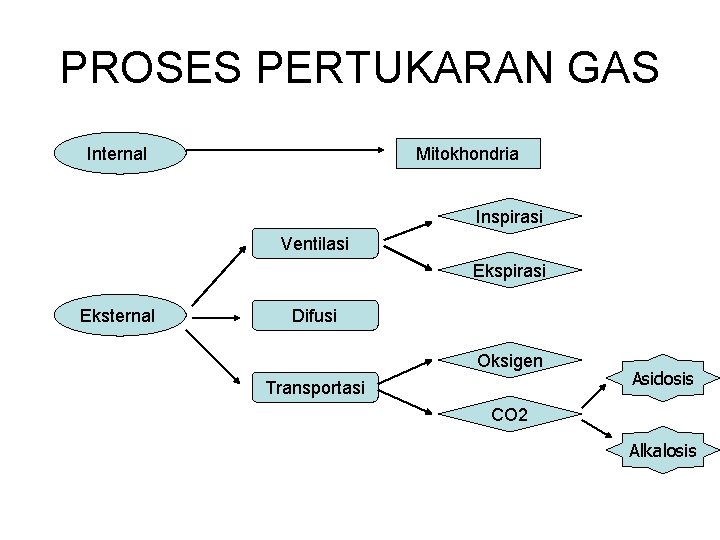
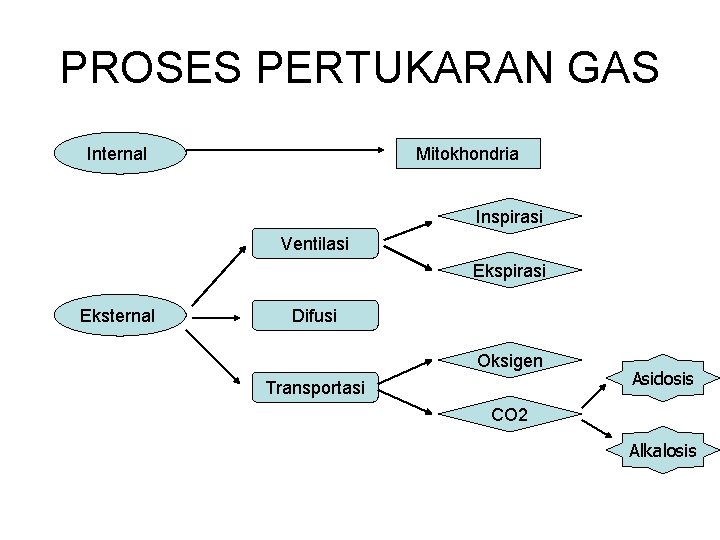
PROSES PERTUKARAN GAS Mitokhondria Internal Inspirasi Ventilasi Ekspirasi Eksternal Difusi Oksigen Transportasi Asidosis CO 2 Alkalosis
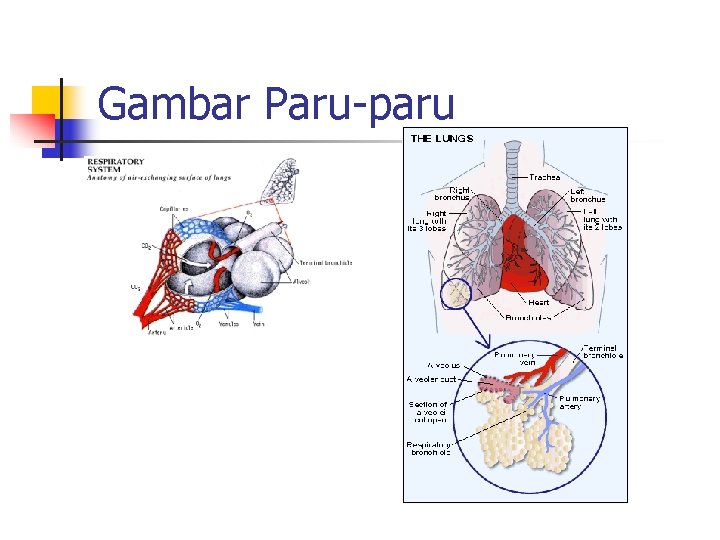
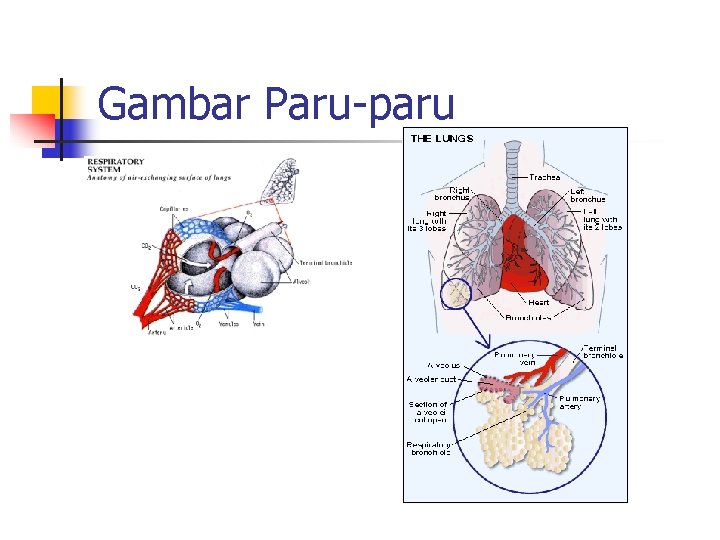
Gambar Paru-paru

Managemen Gangguan Pertukaran Gas
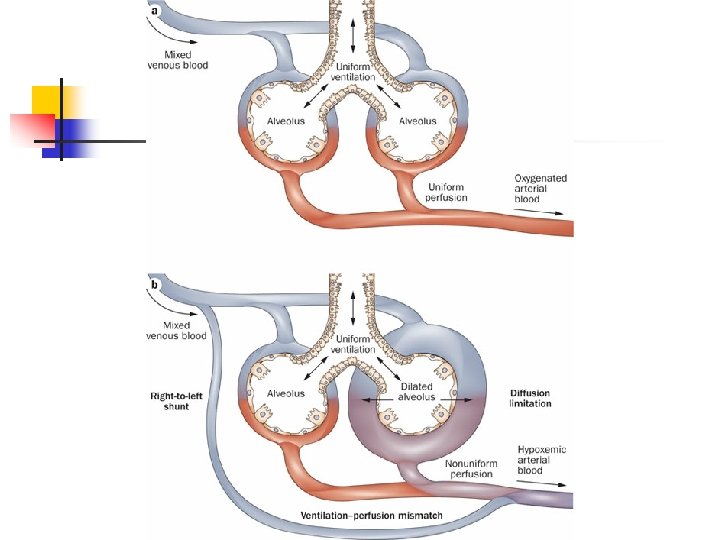
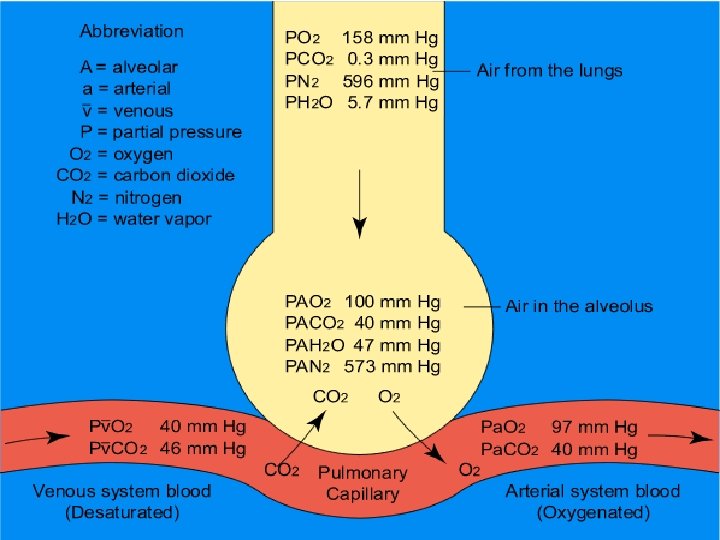
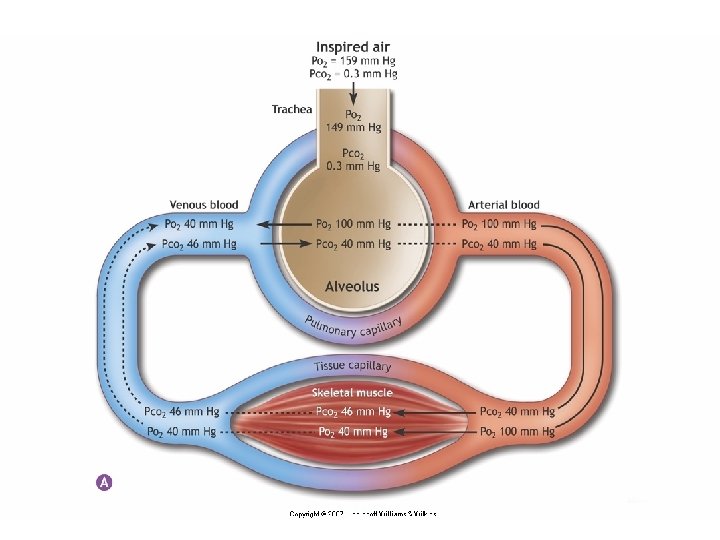
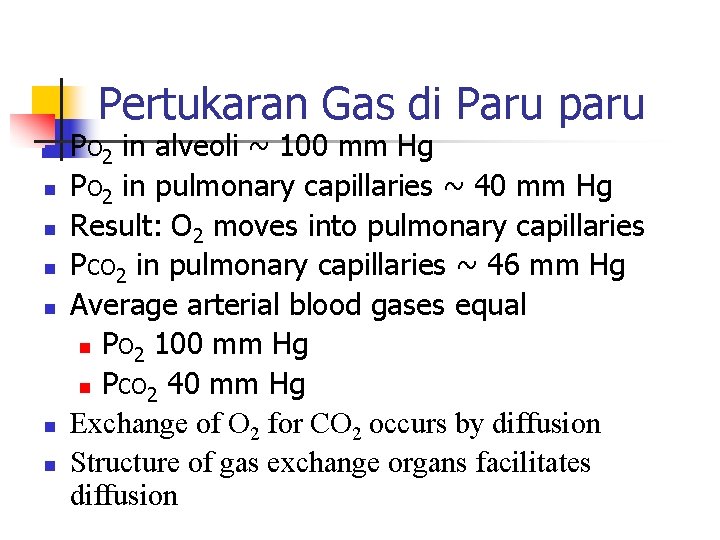
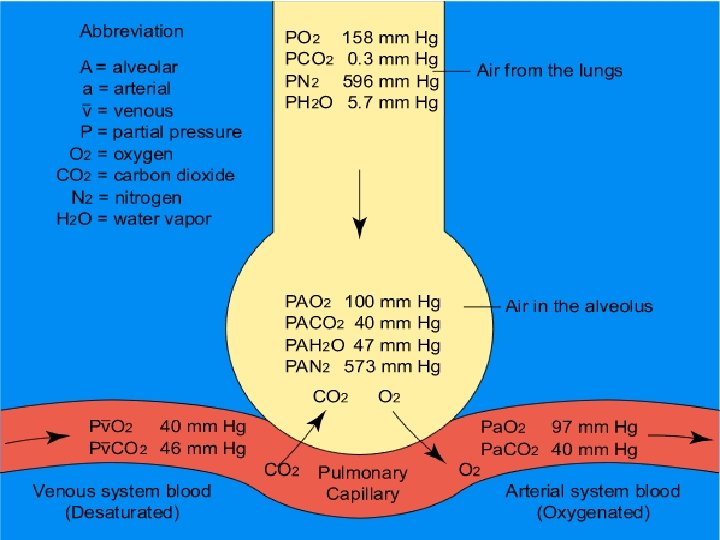
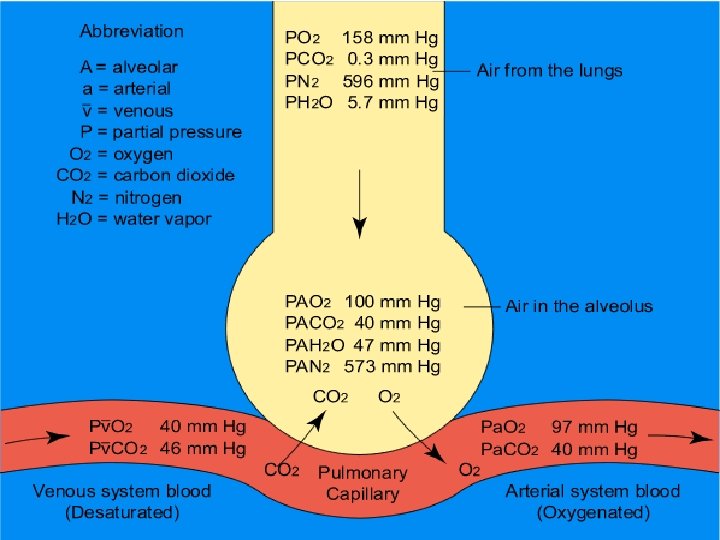
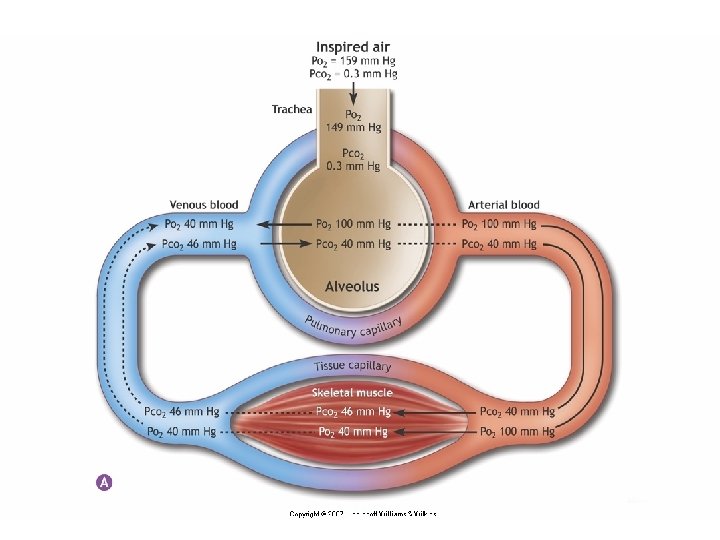
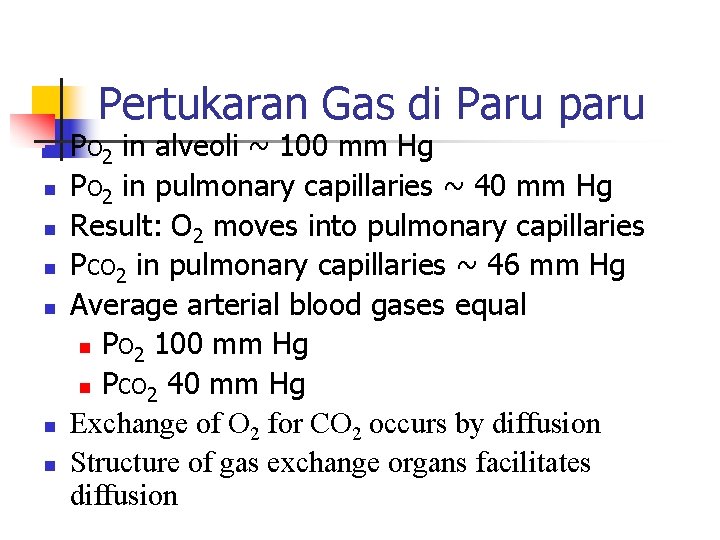
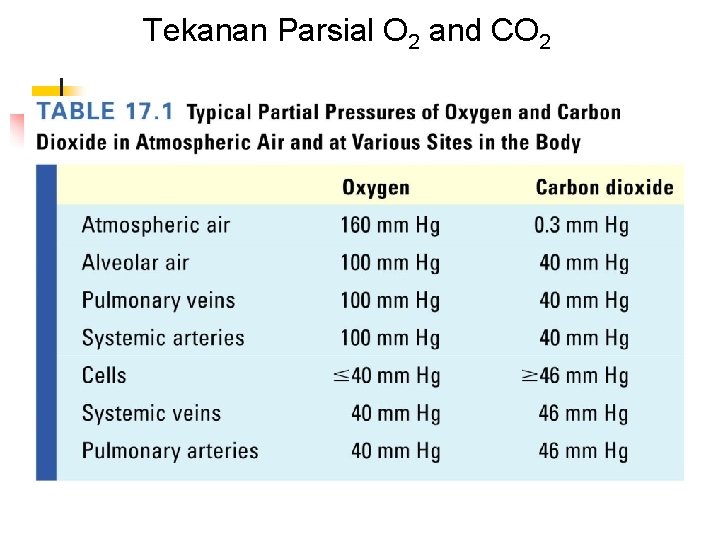
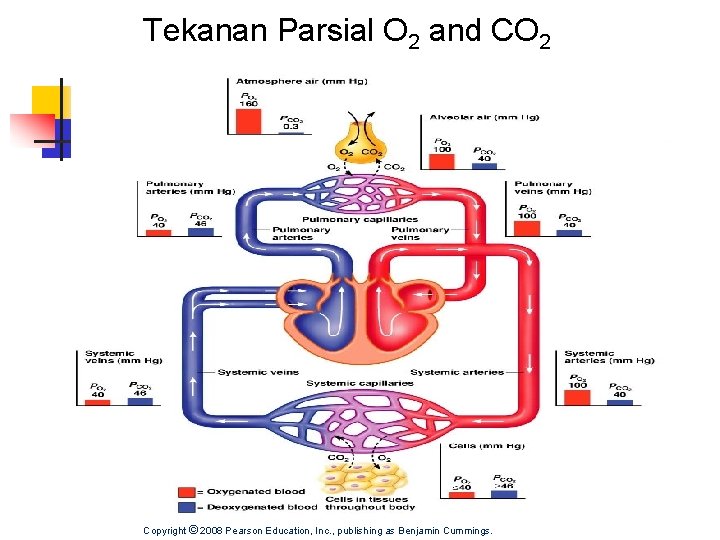
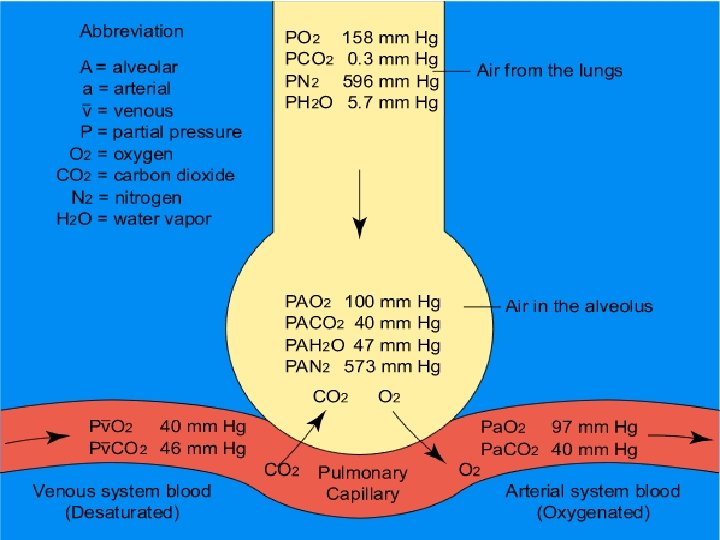
Pertukaran Gas di Paru paru n n n n PO 2 in alveoli ~ 100 mm Hg PO 2 in pulmonary capillaries ~ 40 mm Hg Result: O 2 moves into pulmonary capillaries PCO 2 in pulmonary capillaries ~ 46 mm Hg Average arterial blood gases equal n PO 2 100 mm Hg n PCO 2 40 mm Hg Exchange of O 2 for CO 2 occurs by diffusion Structure of gas exchange organs facilitates diffusion
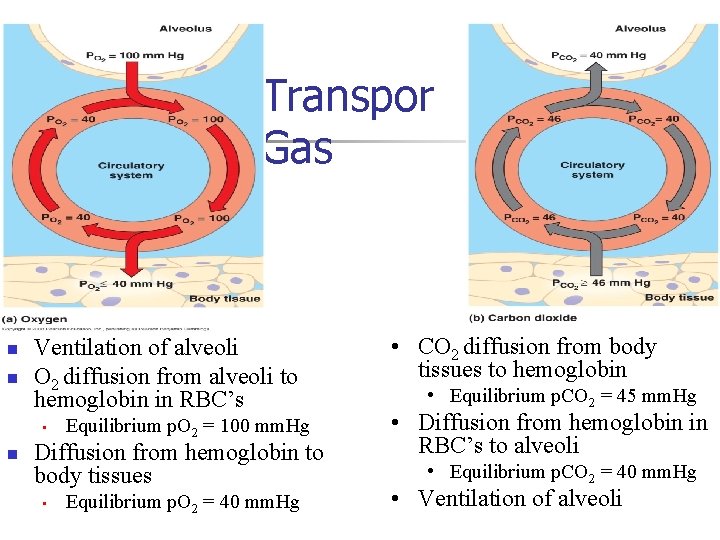
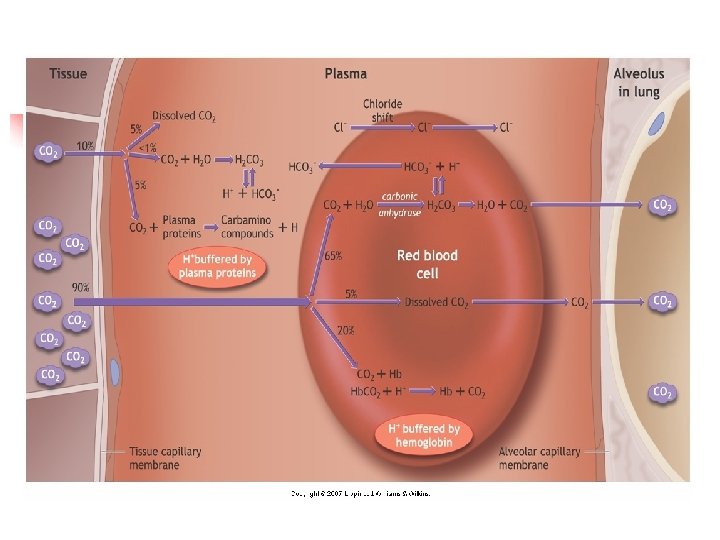
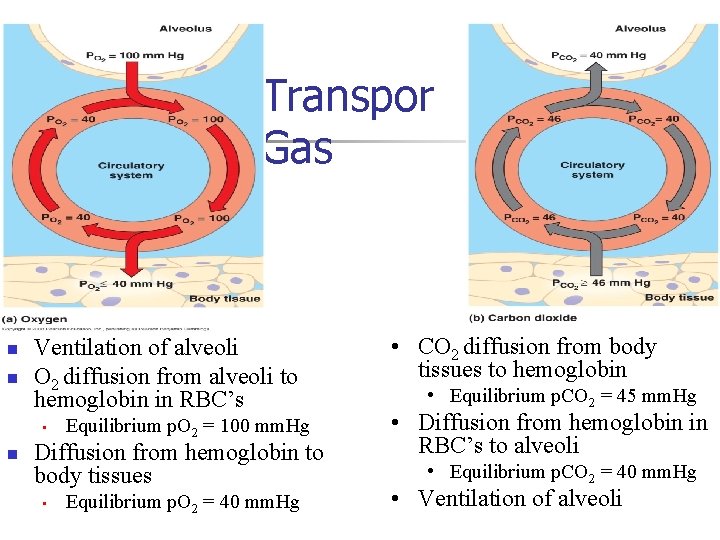
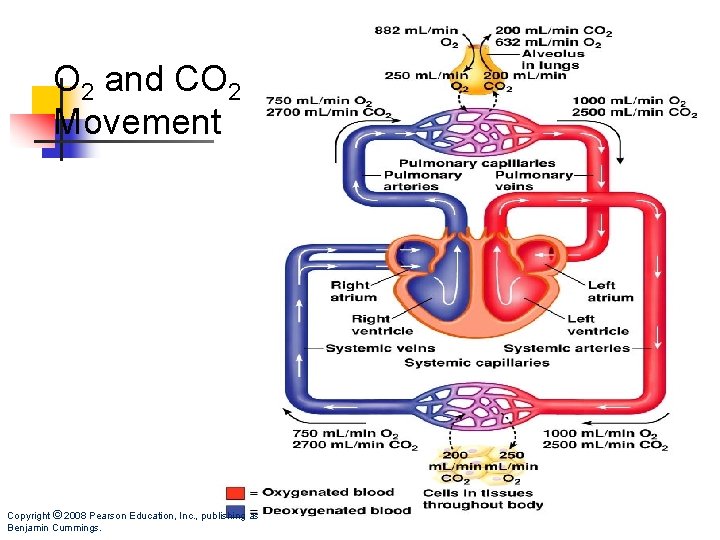
Transpor Gas n n Ventilation of alveoli O 2 diffusion from alveoli to hemoglobin in RBC’s • n Equilibrium p. O 2 = 100 mm. Hg Diffusion from hemoglobin to body tissues • Equilibrium p. O 2 = 40 mm. Hg • CO 2 diffusion from body tissues to hemoglobin • Equilibrium p. CO 2 = 45 mm. Hg • Diffusion from hemoglobin in RBC’s to alveoli • Equilibrium p. CO 2 = 40 mm. Hg • Ventilation of alveoli
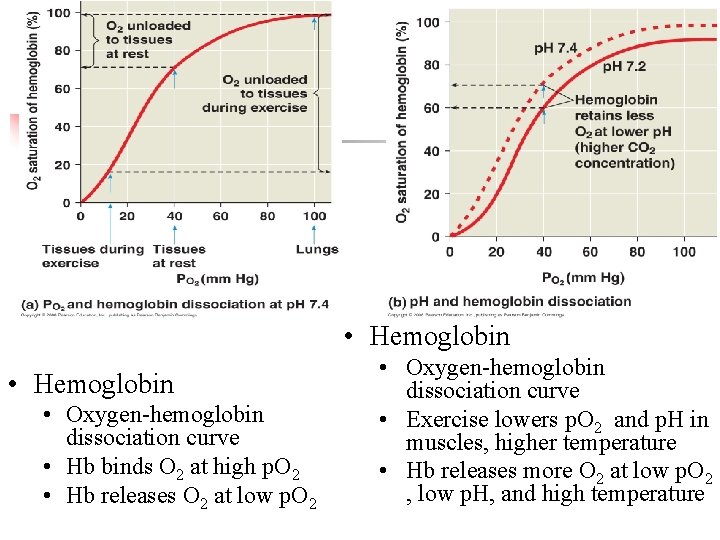
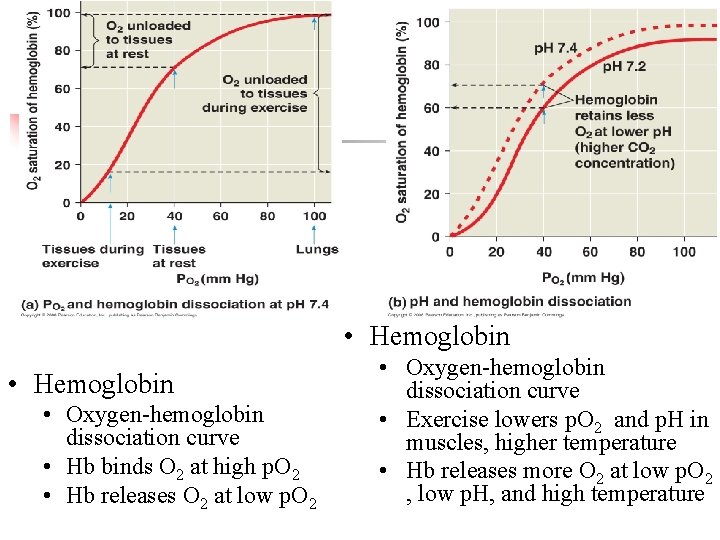
• Hemoglobin • Oxygen-hemoglobin dissociation curve • Hb binds O 2 at high p. O 2 • Hb releases O 2 at low p. O 2 • Oxygen-hemoglobin dissociation curve • Exercise lowers p. O 2 and p. H in muscles, higher temperature • Hb releases more O 2 at low p. O 2 , low p. H, and high temperature
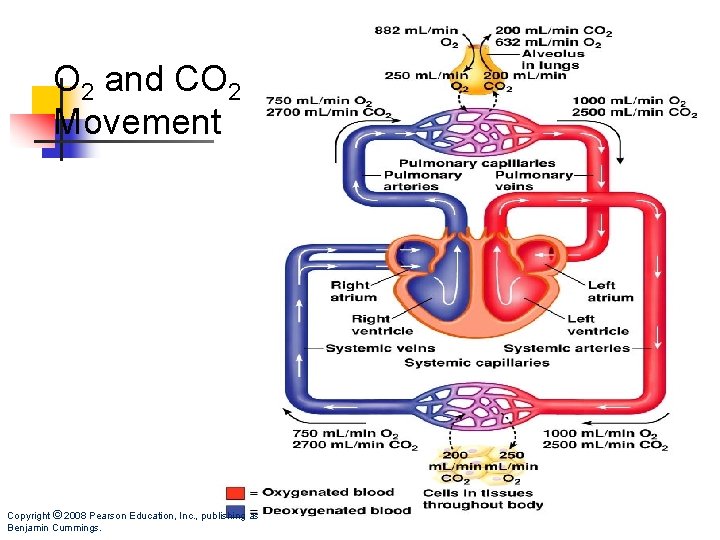
O 2 and CO 2 Movement Copyright © 2008 Pearson Education, Inc. , publishing as Benjamin Cummings.
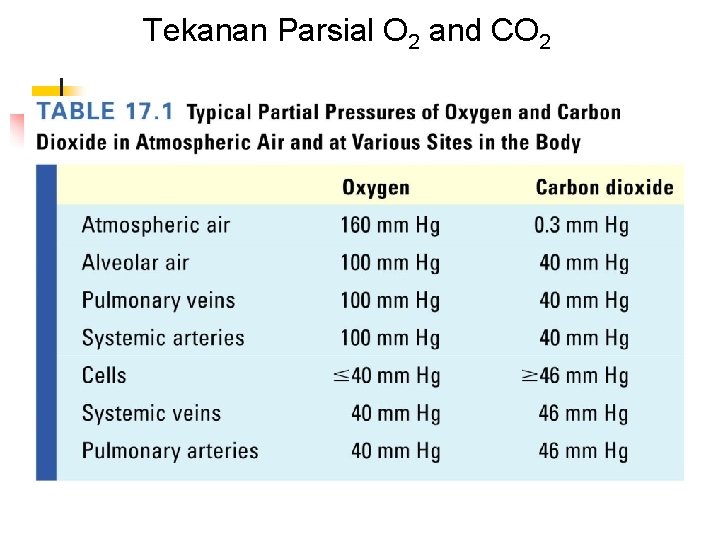
Tekanan Parsial O 2 and CO 2
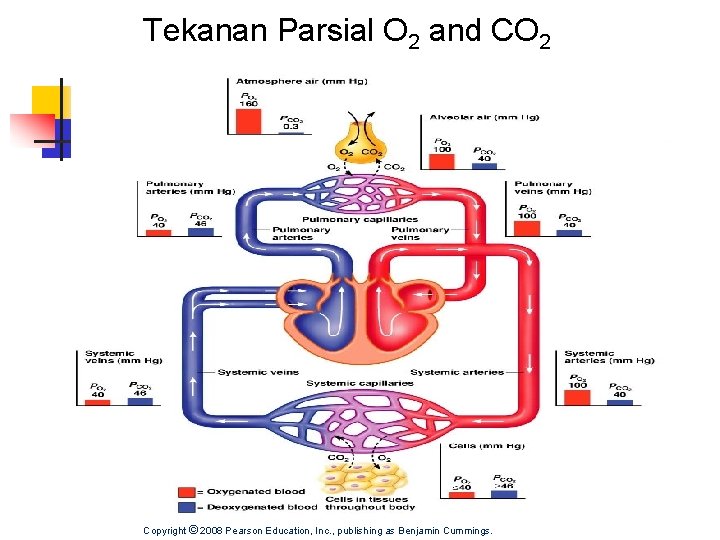
Tekanan Parsial O 2 and CO 2 Copyright © 2008 Pearson Education, Inc. , publishing as Benjamin Cummings.
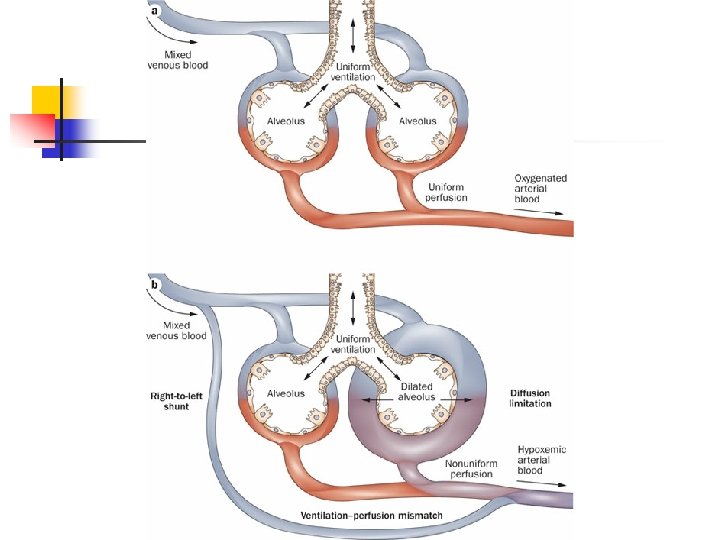
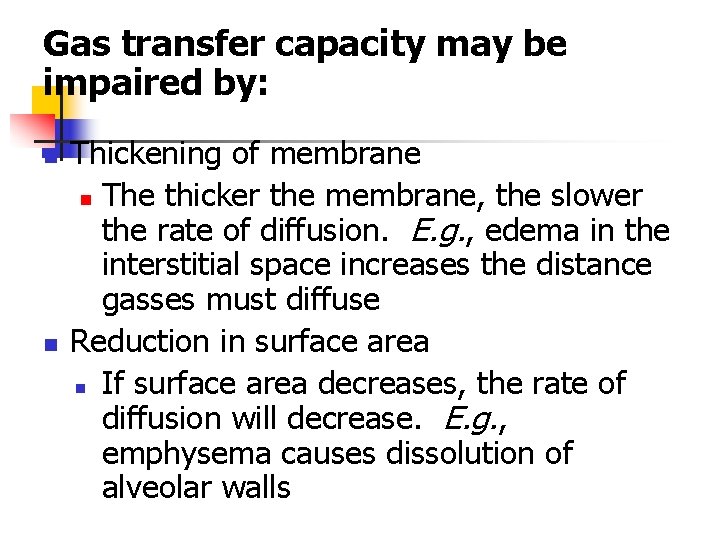
Gas transfer capacity may be impaired by: n n Thickening of membrane n The thicker the membrane, the slower the rate of diffusion. E. g. , edema in the interstitial space increases the distance gasses must diffuse Reduction in surface area n If surface area decreases, the rate of diffusion will decrease. E. g. , emphysema causes dissolution of alveolar walls
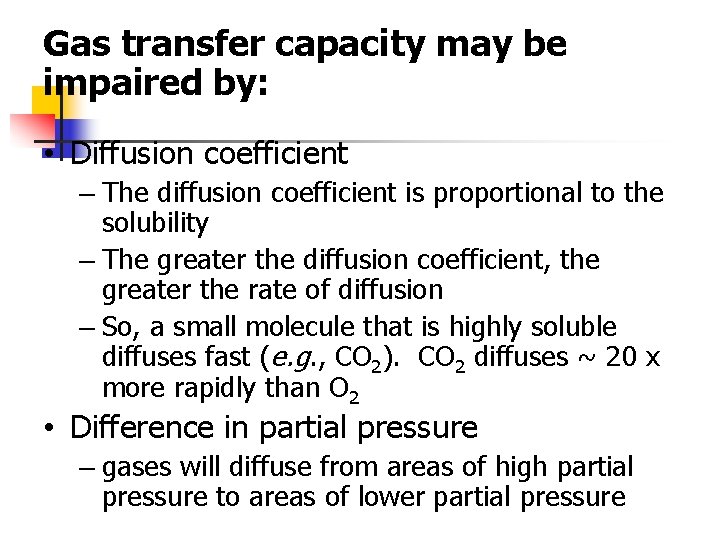
Gas transfer capacity may be impaired by: • Diffusion coefficient – The diffusion coefficient is proportional to the solubility – The greater the diffusion coefficient, the greater the rate of diffusion – So, a small molecule that is highly soluble diffuses fast (e. g. , CO 2). CO 2 diffuses ~ 20 x more rapidly than O 2 • Difference in partial pressure – gases will diffuse from areas of high partial pressure to areas of lower partial pressure
Copyright © 2008 Pearson Education, Inc. , publishing as Benjamin Cummings.
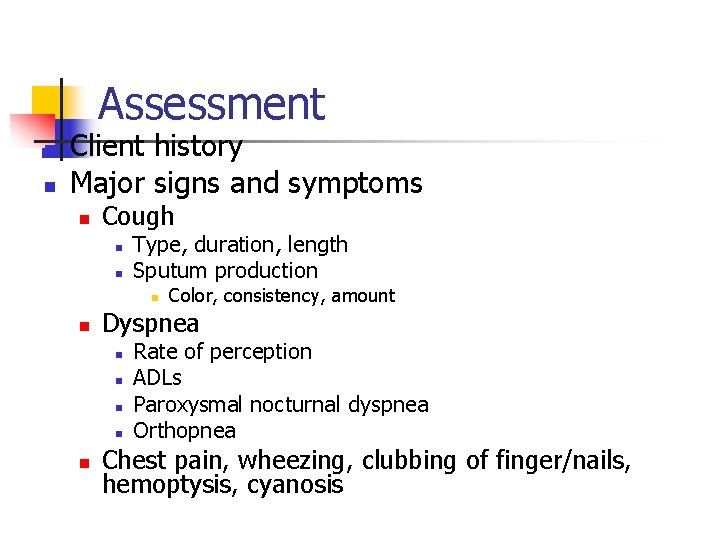
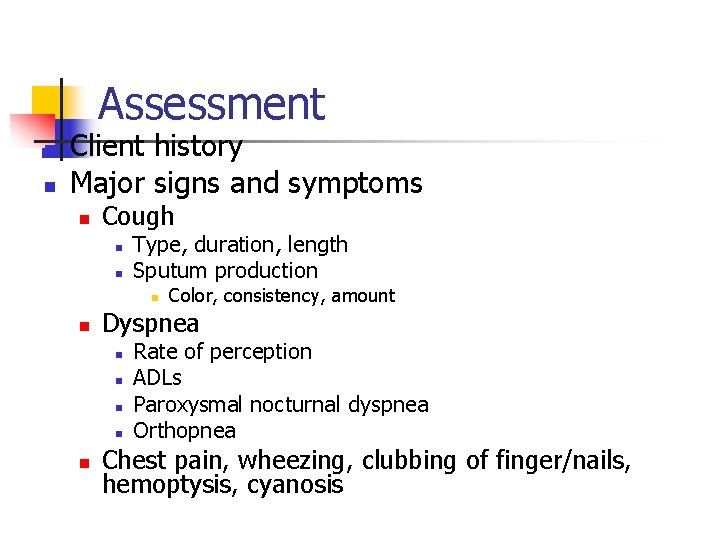
Assessment n n Client history Major signs and symptoms n Cough n n Type, duration, length Sputum production n n Dyspnea n n n Color, consistency, amount Rate of perception ADLs Paroxysmal nocturnal dyspnea Orthopnea Chest pain, wheezing, clubbing of finger/nails, hemoptysis, cyanosis
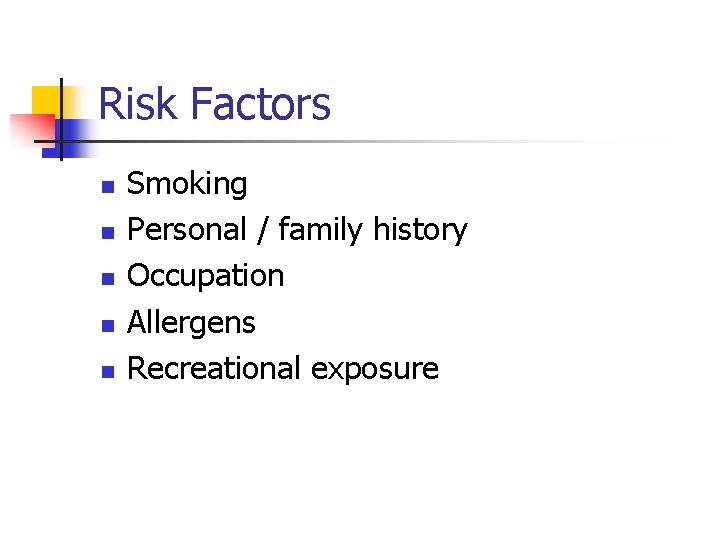
Risk Factors n n n Smoking Personal / family history Occupation Allergens Recreational exposure
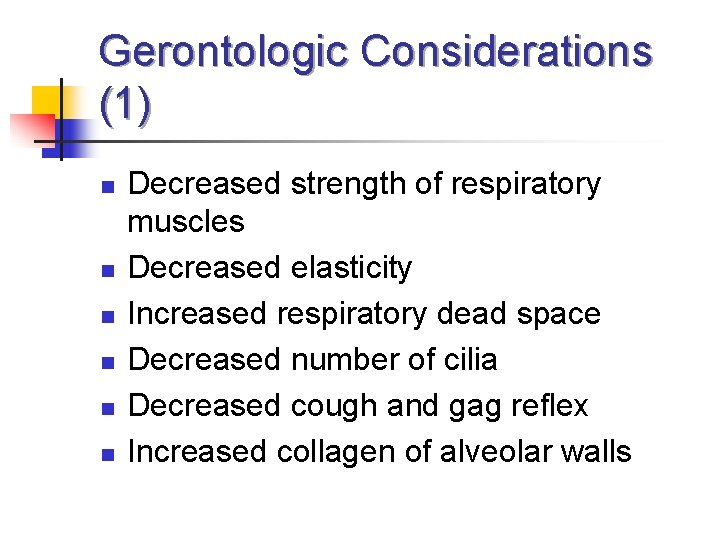
Gerontologic Considerations (1) n n n Decreased strength of respiratory muscles Decreased elasticity Increased respiratory dead space Decreased number of cilia Decreased cough and gag reflex Increased collagen of alveolar walls
Gerontologic Considerations (2) n n n Vital capacity and respiratory muscle strength peak between 20 -25 and then decrease Age 40 and older – surface area in alveoli is reduced Age 50 – alveoli loses elasticity Loss of chest wall mobility>decrease in vital capacity Amount of respiratory dead space increases with age Decreased diffusion capacity with age – lower oxygen level in arterial circulation
Common Management n n n n Position Environmental control Activity dan rest Oral Hygiene Adequate hydration Infection prevention and control Psychosocial support
Respiratory Pharmacologic agent n n Antimicrobials (Antibiotik) Bronchodilators a. b. n n n -adrenergics, seperti : albuterol (ventolin) Theophyline, seperti aminophyline Adrenal Glucocorticoids (Prednison) Antitusive Mucolitycs Antiallergenics Vasoconstristor dan Decongestan
Respiratory Assessment n n n n Health History Risk factors for respiratory disease-genetics, smoking, allergens, occupational and recreational exposure Dyspnea, orthopnea Cough, ? productive Chest pain Cyanosis Lung sounds Clubbing—indicates chronicity
Diagnostic Evaluation (1) n n PFTs-assess respiratory function, screening, assess response to therapy FVC—vital capacity performed with a maximally forced expiratory effort Forced expiratory volume—FEV 1—volume of air exhaled in the specified time during the performance of forced vital capacity. FEV 1 is volume exhaled in one second. FEV 1/FVC%--ratio of timed forced exp. volume to forced vital capacity
Diagnostic Evaluation (2) ABGs: 1. p. H 2. evaluate the Pa. CO 2 and HCO 33. Look to see if compensation has occurred. If CO 2 is >40, respiratory acidosis; If HCO 3 - <24, metabolic acidosis; next look at value other than primary disorder, if moving in same direction as primary value compensation is underway. n
Diagnostic Evaluation (3) n n n n Pulse oximetry—not reliable in severe anemia, high CO levels, or in shock CO 2 monitoring—tells us ventilation to lungs is occurring, that CO 2 is being transported to lungs, exp. CO 2 indicates adequate ventilation Cultures Imaging—chest xray, CT, MRI, lung scans (inject isotope, inhale radioactive gas), PET Bronchoscopy Thoracentesis others
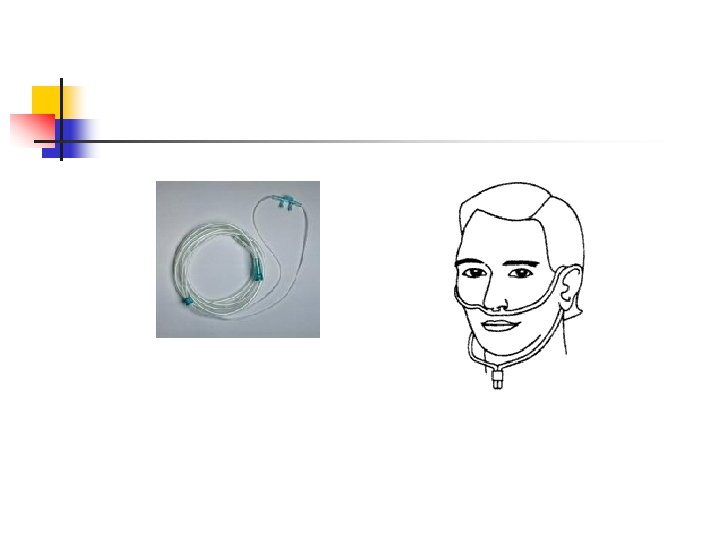
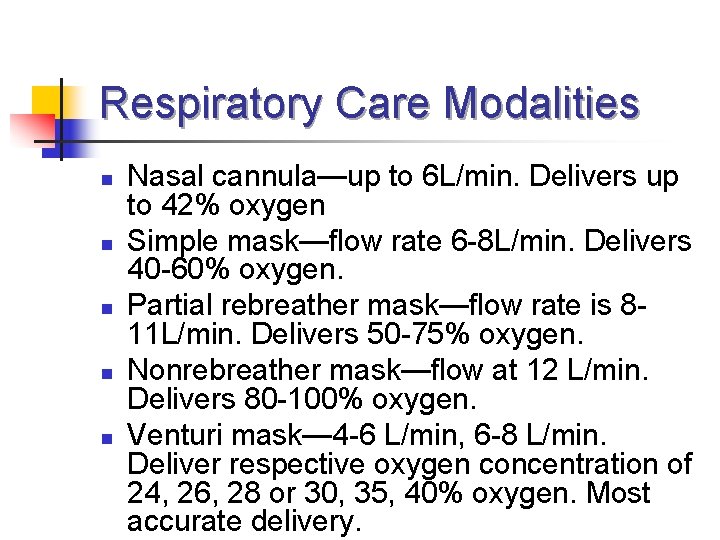
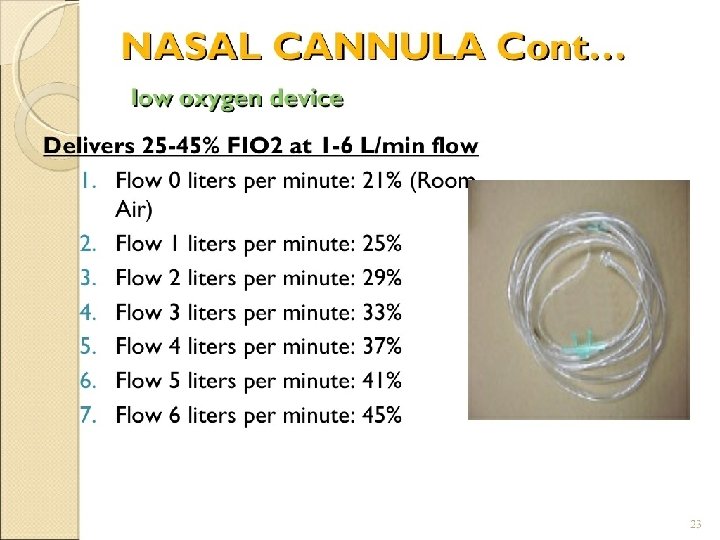
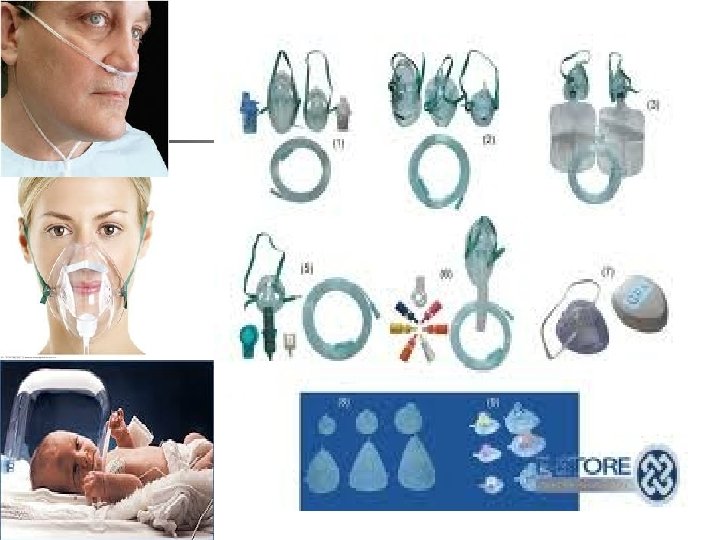
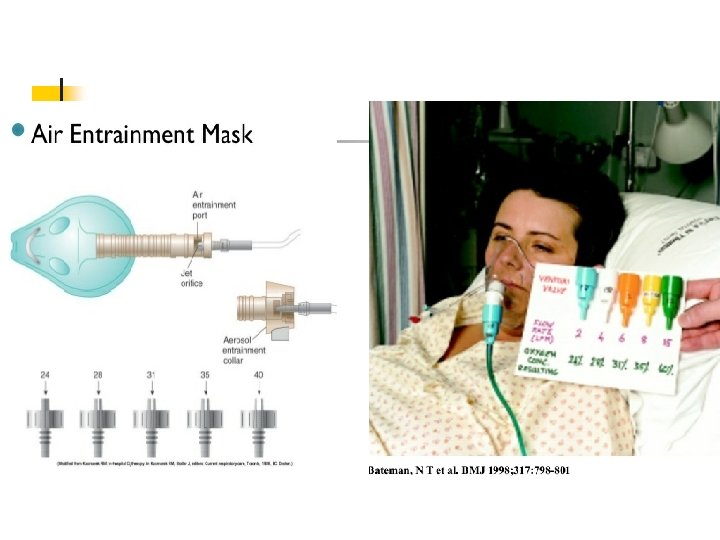
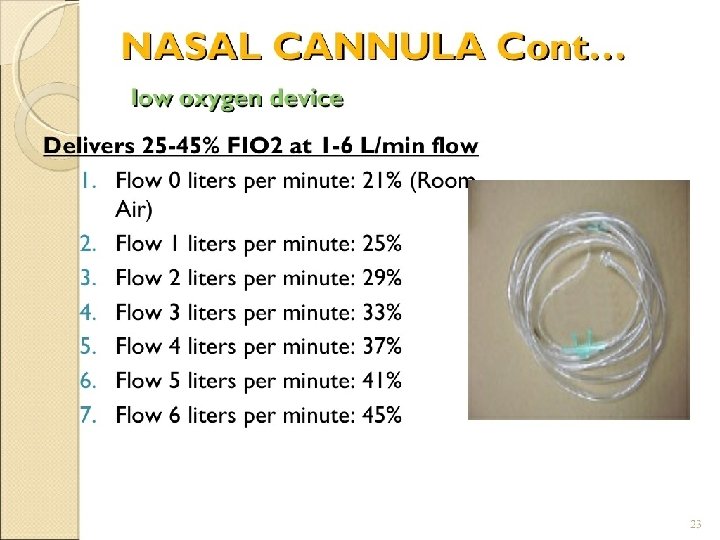
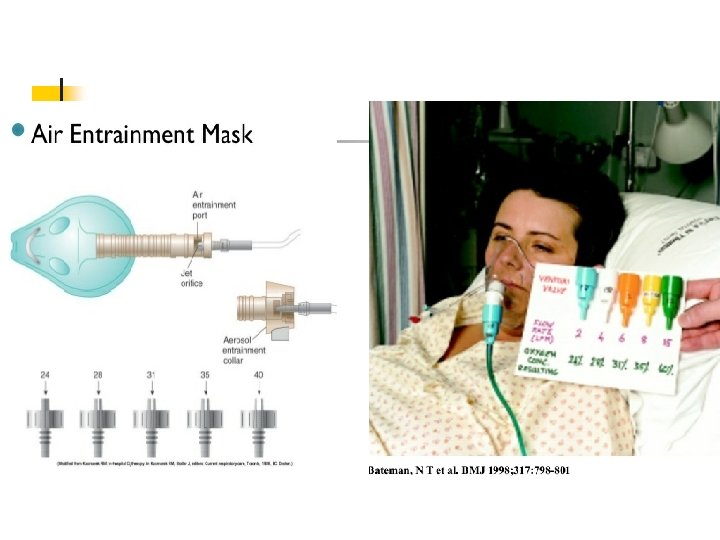
Respiratory Care Modalities n n n Nasal cannula—up to 6 L/min. Delivers up to 42% oxygen Simple mask—flow rate 6 -8 L/min. Delivers 40 -60% oxygen. Partial rebreather mask—flow rate is 811 L/min. Delivers 50 -75% oxygen. Nonrebreather mask—flow at 12 L/min. Delivers 80 -100% oxygen. Venturi mask— 4 -6 L/min, 6 -8 L/min. Deliver respective oxygen concentration of 24, 26, 28 or 30, 35, 40% oxygen. Most accurate delivery.
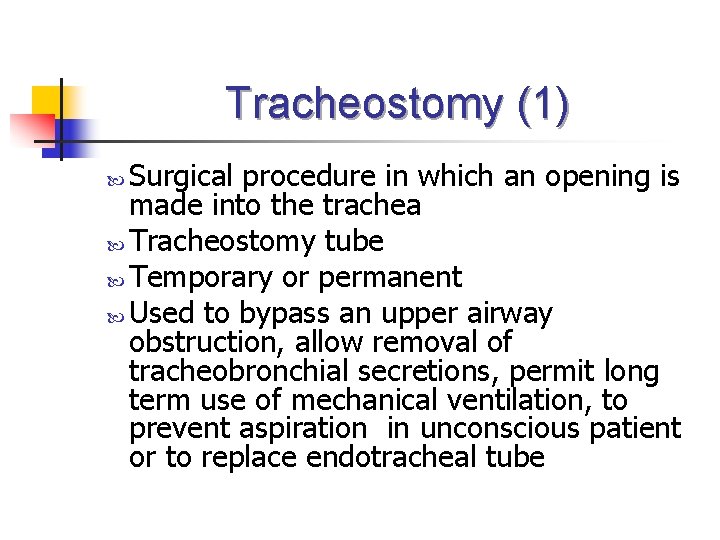
Tracheostomy (1) Surgical procedure in which an opening is made into the trachea Tracheostomy tube Temporary or permanent Used to bypass an upper airway obstruction, allow removal of tracheobronchial secretions, permit long term use of mechanical ventilation, to prevent aspiration in unconscious patient or to replace endotracheal tube
Tracheostomy (2) Complications of tracheostomy: n Bleeding, pneumothorax, air embolism, aspiration, subcutaneous or mediastinal emphysema, recurrent laryngeal nerve damage n Airway obstruction from accumulation of secretions , tracheoesophageal fistula, tracheal ischemia
Tracheostomy (3) Nursing care of the patient with tracheostomy: n Initially, semi-fowler’s position to facilitate ventilation, promote drainage, minimize edema, and prevent strain on the sutures n Allow method of communication n Ensure humidity to trach n Suction secretions as needed n Manage cuff—usually keep pressure less than 25 mm Hg but more than 15 mm Hg to prevent aspiration
Endotracheal Intubation n n n Pass ETT via nose or mouth into trachea Method of choice in emergency situation Passed with aid of a laryngoscope ETT generally has a cuff, ensure that cuff pressure is between 15 -20 mm Hg. Use warmed, humidified oxygen Should not be used for more than 3 week
Preventing Complications Associated with Endotracheal and Tracheostomy Tubes n n n n n Administer adequate warmed humidity Maintain cuff pressure at appropriate level Suction as needed Maintain skin integrity Auscultate lung sounds—ETT can lodge in right mainstem bronchus Monitor for s/s of infection Monitor for cyanosis Maintain hydration of patient Use sterile technique when suctioning and performing trach care Monitor O 2 sat
Mechanical Ventilation n Used to control patient’s respirations, to oxygenate when patient’s ventilatory efforts are inadequate, to rest respiratory muscles Can be positive pressure or negative pressure Key for the nurse is assess patient—not the ventilator
Indications for Mechanical Ventilation Pa. O 2 <50 mm Hg with Fi. O 2 >0. 60 n Pa. O 2 >50 mm Hg with p. H <7. 25 n Vital capacity < 2 times tidal volume n Negative inspiratory force < 25 cm H 20 n Respiratory rate > 35 bpm ( *vital capacity is dependent on age, gender, weight and body build. Usually is twice tidal volume. If < 10 m. L/kg, will need respiratory assist) n
Thoracic Surgeries (1) n n Pneumonectomy Lobectomy Segmental resection Lung volume reduction, etc Manage potential complication: n n n Monitor respiratory status Vitals For dysrhythmias For bleeding, atelectasis and infection Monitor chest tube drainage, for leaks, for tube kinks, for excessive drainage
Thoracic Surgeries (2) Care of patient after thoracotomy: n Maintain airway clearance n Positioning-lobectomy turn either side, pneumonectomy turn on affected side, segmental resection varies per doctor n Chest tube drainage/care n Relieve pain n Promote mobility n Maintain fluid volume and nutrition
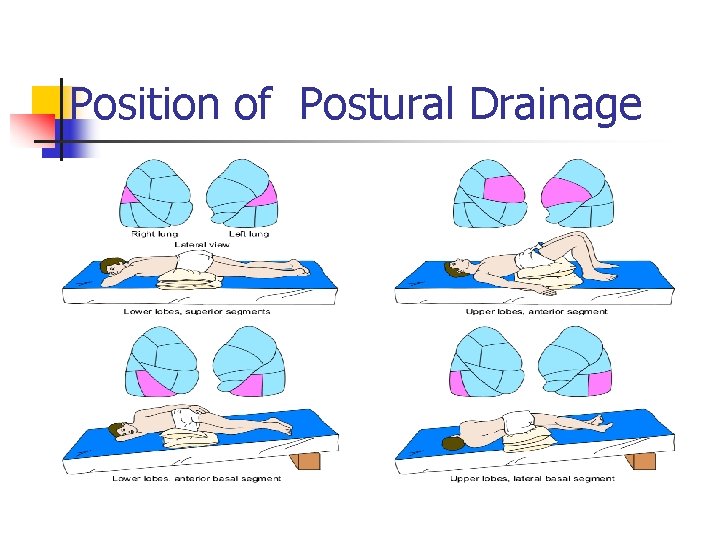
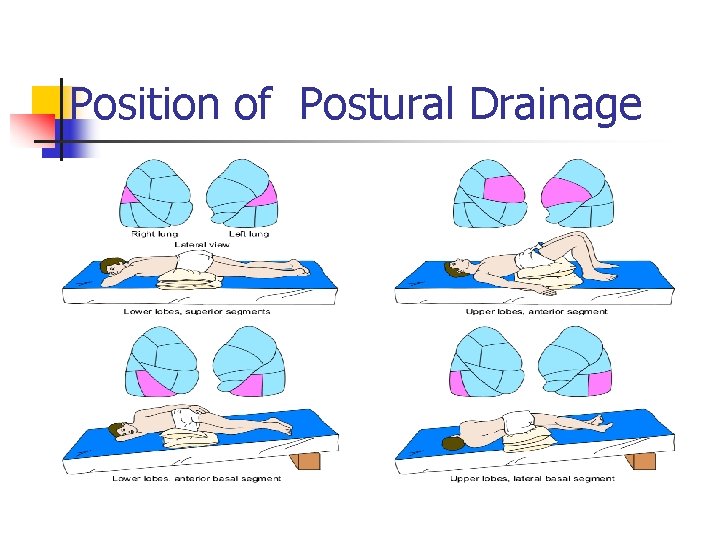
Position of Postural Drainage
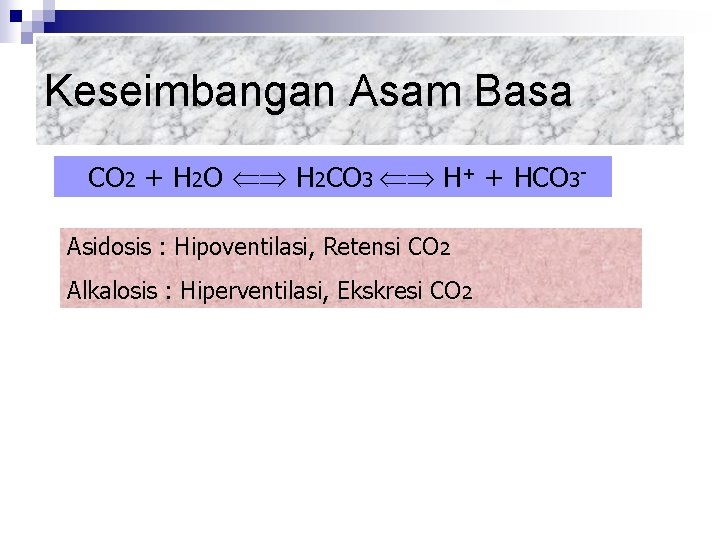
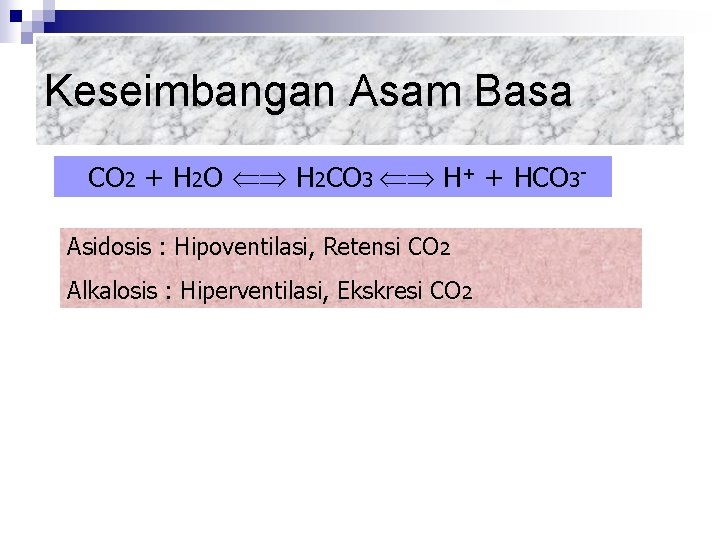
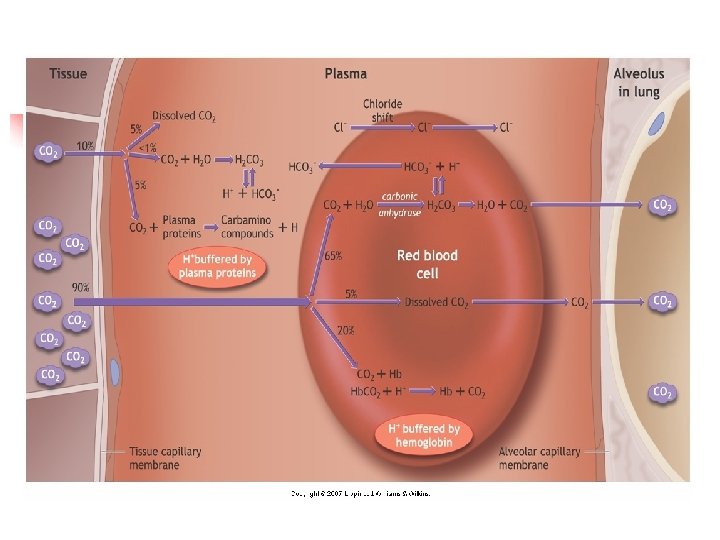
Keseimbangan Asam Basa CO 2 + H 2 O H 2 CO 3 H+ + HCO 3 Asidosis : Hipoventilasi, Retensi CO 2 Alkalosis : Hiperventilasi, Ekskresi CO 2
Kendali Pernafasan 1. 2. 3. 4. 5. 6. 7. 8. Faktor Lokal : Kontrol Medulla Oblongata : Kontrol Pons : transisi insp – eks Refleks Hering-Breur : Masukkan Korteks : Kendali Bio Kimiawi : Efek Latihan Jasmani : Efek Altitude/Ketinggian
Tindakan Umum 1. 2. 3. 4. 5. 6. 7. Posisi Kontrol Lingkungan Aktifitas dan Istirahat. Oral Hygiene. Hidrasi Adekuat Pencegahan dan Kontrol Infeksi Support Psikososial
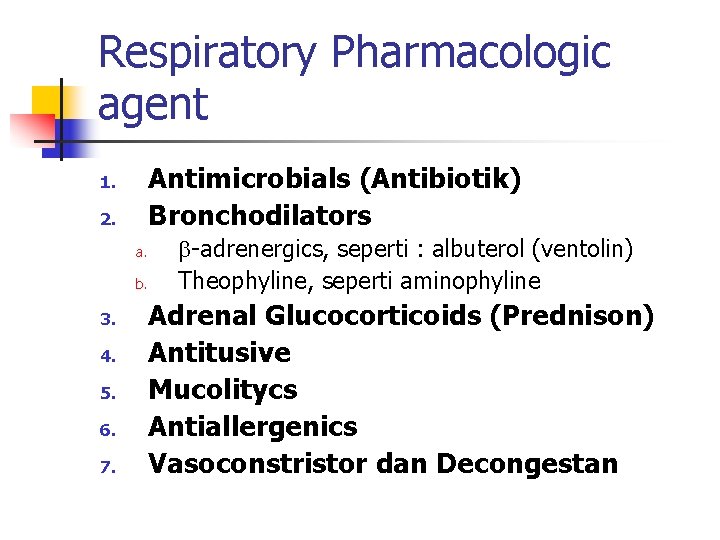
Respiratory Pharmacologic agent Antimicrobials (Antibiotik) Bronchodilators 1. 2. a. b. 3. 4. 5. 6. 7. -adrenergics, seperti : albuterol (ventolin) Theophyline, seperti aminophyline Adrenal Glucocorticoids (Prednison) Antitusive Mucolitycs Antiallergenics Vasoconstristor dan Decongestan
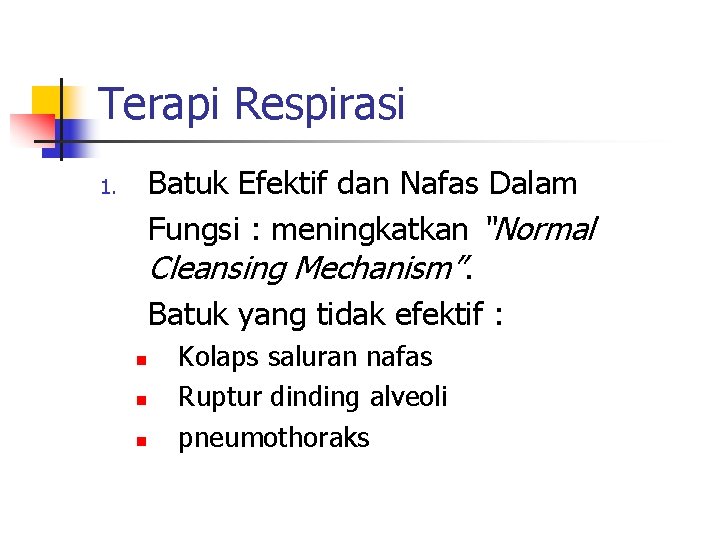
Terapi Respirasi Batuk Efektif dan Nafas Dalam Fungsi : meningkatkan “Normal Cleansing Mechanism”. Batuk yang tidak efektif : 1. n n n Kolaps saluran nafas Ruptur dinding alveoli pneumothoraks

Terapi………… n Fisioterapi dada : n n n Clapping Vibrasi Postural Drainage
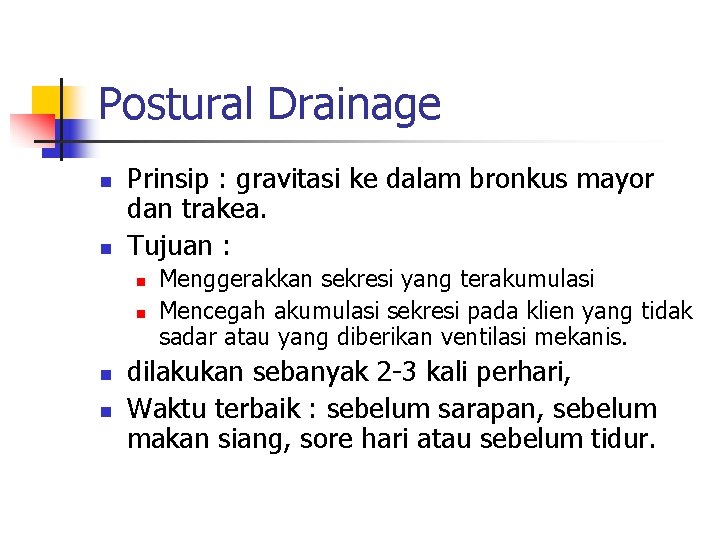
Postural Drainage n n Prinsip : gravitasi ke dalam bronkus mayor dan trakea. Tujuan : n n Menggerakkan sekresi yang terakumulasi Mencegah akumulasi sekresi pada klien yang tidak sadar atau yang diberikan ventilasi mekanis. dilakukan sebanyak 2 -3 kali perhari, Waktu terbaik : sebelum sarapan, sebelum makan siang, sore hari atau sebelum tidur.
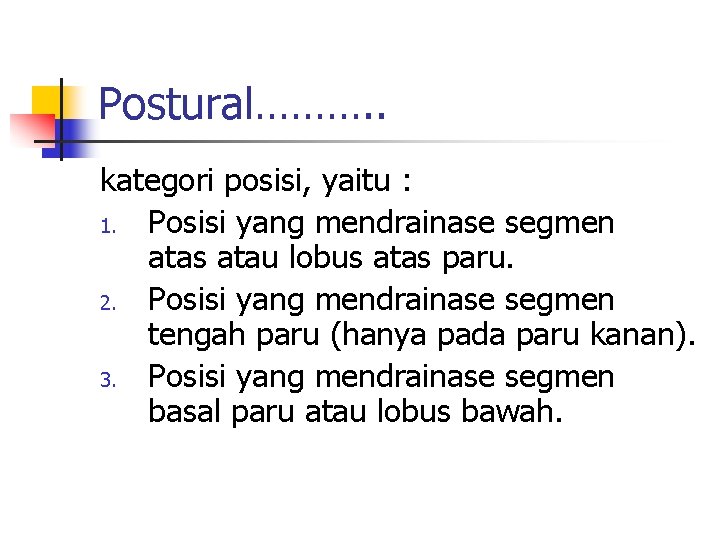
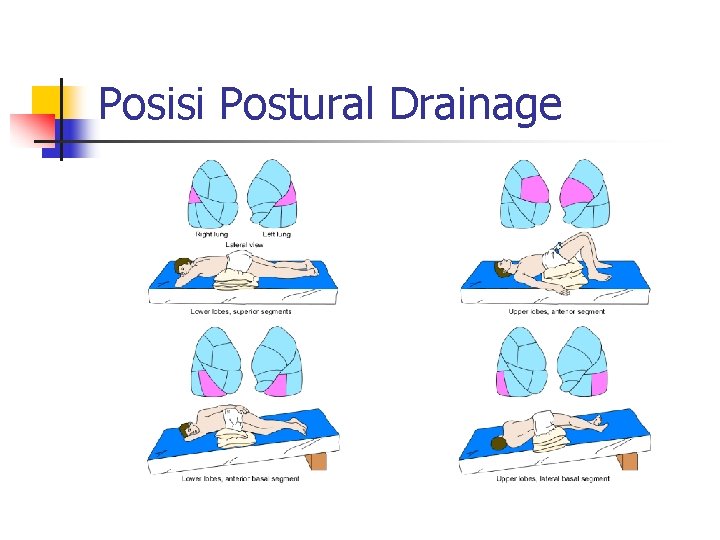
Postural………. . kategori posisi, yaitu : 1. Posisi yang mendrainase segmen atas atau lobus atas paru. 2. Posisi yang mendrainase segmen tengah paru (hanya pada paru kanan). 3. Posisi yang mendrainase segmen basal paru atau lobus bawah.
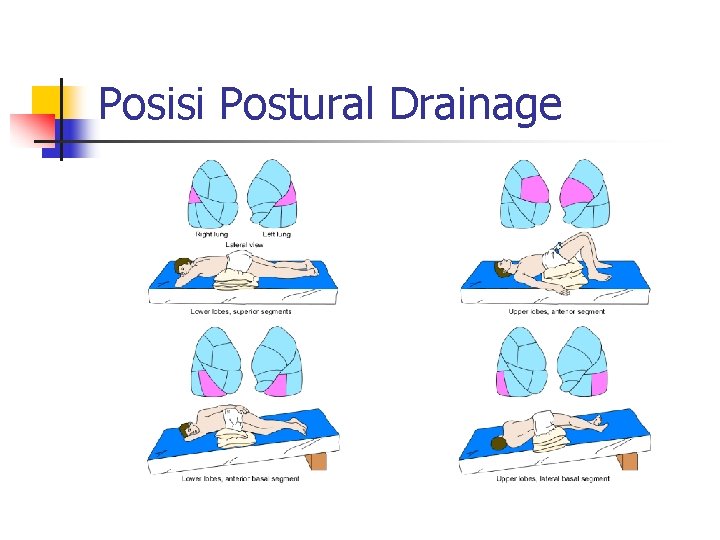
Posisi Postural Drainage
Oksigen n n Diberikan ketika hipoksemia timbul atau dicurigai akan timbul dimana dengan hipoksemia tertanggulangi maka hipoxia akan dapat dicegah. indikasi : n n n Menurunnya Arterial Blood Oxygen. Meningkatnya kerja nafas Kebutuhan untuk menurunkan kerja myocardial.
Komplikasi Oksigen 1. 2. 3. 4. Oxygen-induced Hypoventilation Oxygen Toxicity. Atelektasis Occular Damage.
Alat Pemberian O 2 n n Alat-alat oksigen aliran rendah : kanula nasal, masker sederhana, rebreather dan Non-rebreather. Alat-alat oksigen aliran tinggi adalah : masker venturi, masker aerosol, collar trakeostomi, T-Piece, sungkup.