Managing TAVR Rhythm Disturbances New LBBB Bradyarrhythmias and

Managing TAVR Rhythm Disturbances: New LBBB, Bradyarrhythmias and Temporary and Permanent Pacemakers Lutz Buellesfeld MD FSCAI FESC Department of Cardiology Bern University Hospital Switzerland

Lutz Buellesfeld, MD Consulting: Mitralign Medtronic Core. Valve Edwards Lifesciences, LLC Abbott Vascular
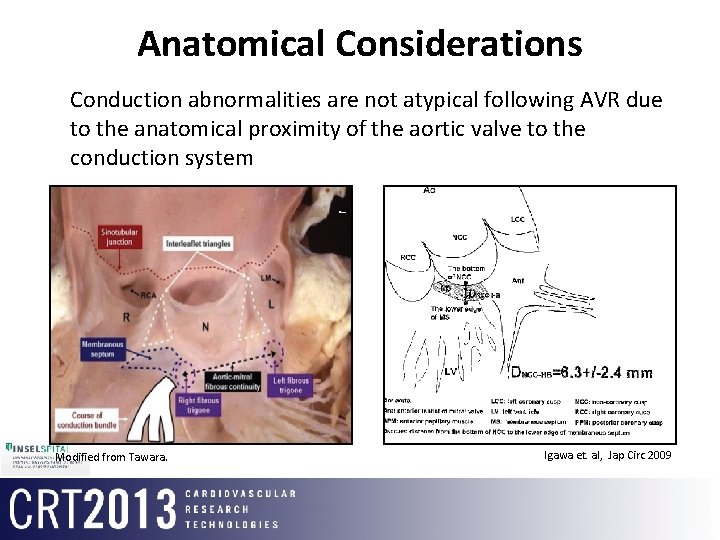
Anatomical Considerations • Conduction abnormalities are not atypical following AVR due to the anatomical proximity of the aortic valve to the conduction system Modified from Tawara. Igawa et. al, Jap Circ 2009
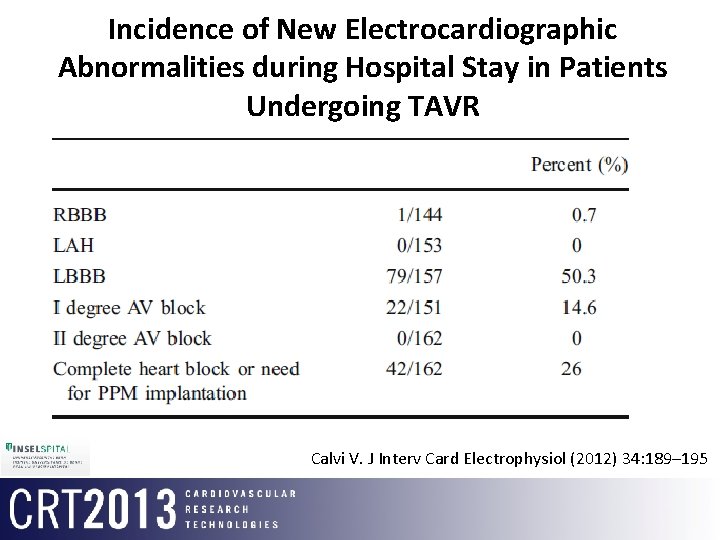
Incidence of New Electrocardiographic Abnormalities during Hospital Stay in Patients Undergoing TAVR Calvi V. J Interv Card Electrophysiol (2012) 34: 189– 195
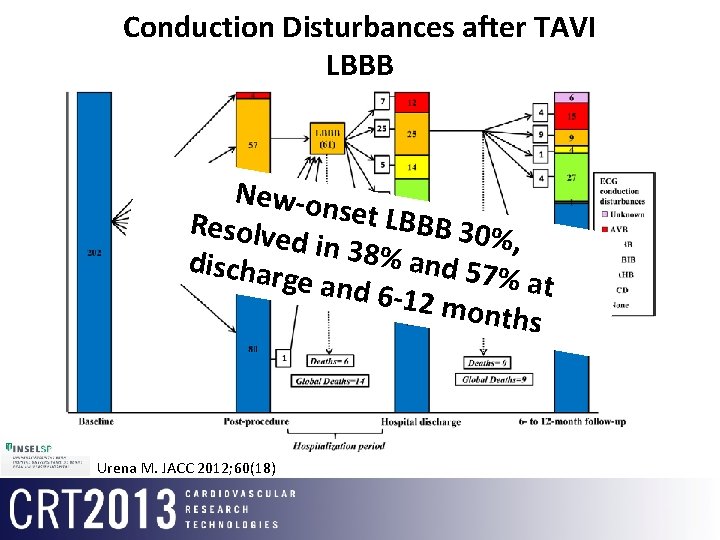
Conduction Disturbances after TAVI LBBB New-on s et LBBB Resolve 30%, d in 38% and 57% dischar ge and 6 -12 mo at nths Urena M. JACC 2012; 60(18)
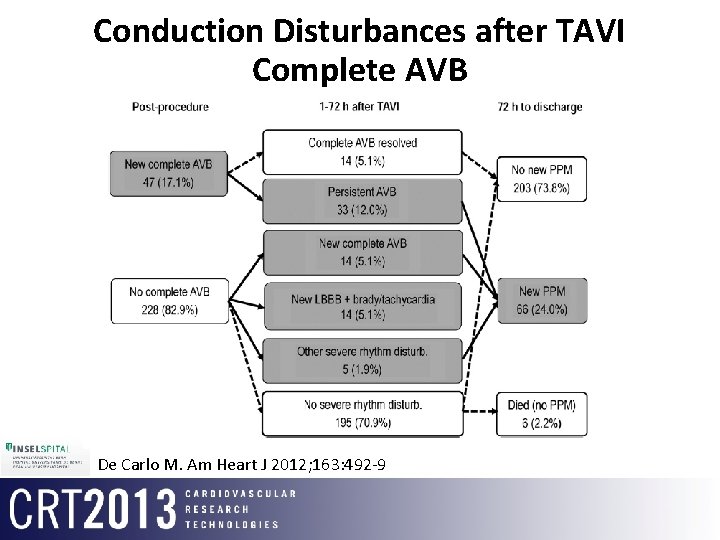
Conduction Disturbances after TAVI Complete AVB De Carlo M. Am Heart J 2012; 163: 492 -9
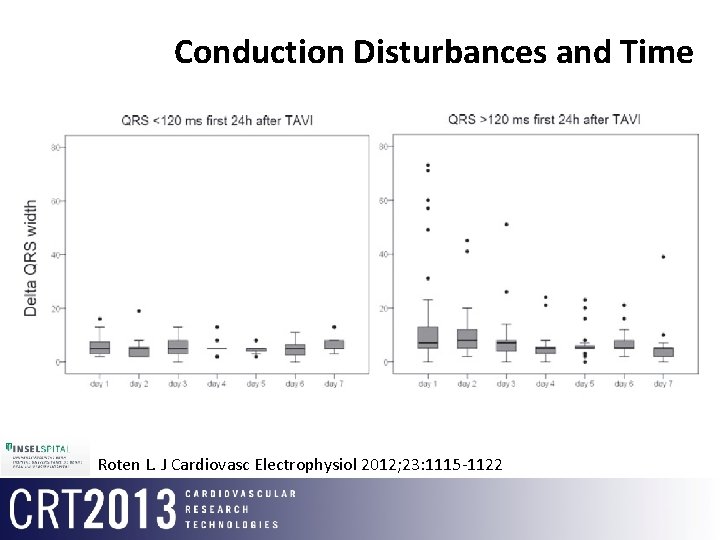
Conduction Disturbances and Time Roten L. J Cardiovasc Electrophysiol 2012; 23: 1115 -1122
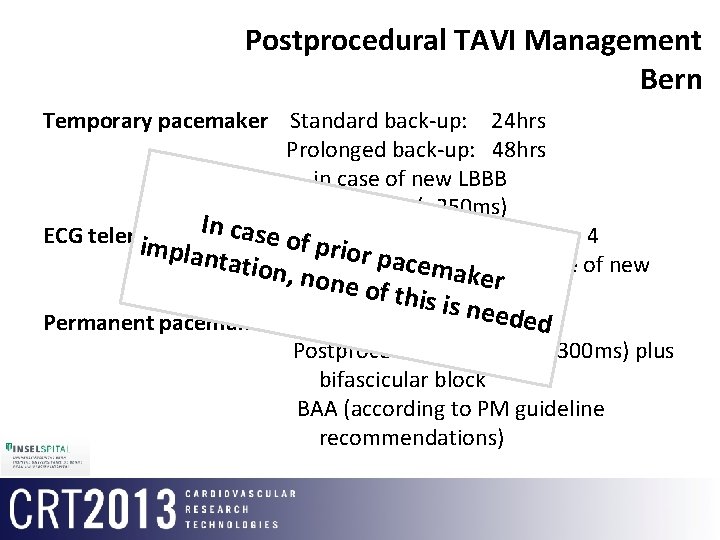
Postprocedural TAVI Management Bern Temporary pacemaker Standard back-up: 24 hrs Prolonged back-up: 48 hrs in case of new LBBB plus AVB I (>250 ms) In case Standard monitoring until day 4 ECG telemetry of prio implan r pamonitoring tation, Prolonged c none o emaker in case of new f thisdisturbances conduction is need ed. II Permanent pacemaker Postprocedural AVB III or Postprocedural AVB I (PQ >300 ms) plus bifascicular block BAA (according to PM guideline recommendations)
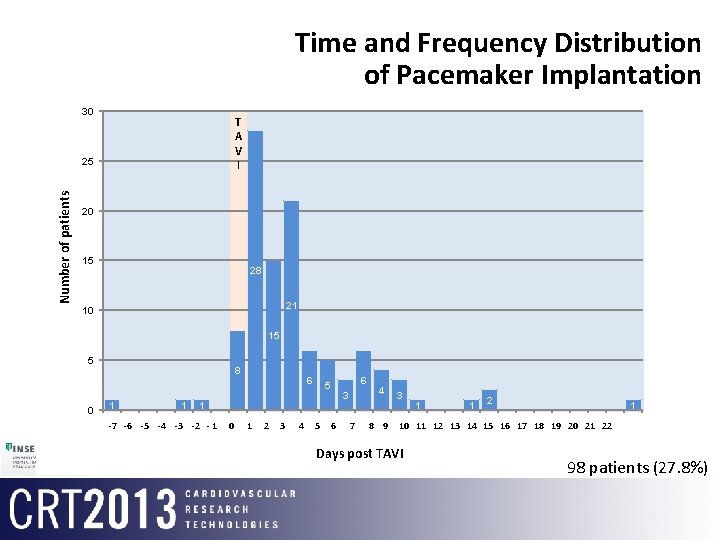
Time and Frequency Distribution of Pacemaker Implantation 30 T A V I Number of patients 25 20 15 28 21 10 15 5 0 8 1 1 1 6 5 6 3 4 3 1 1 2 1 1 -62 -53 -44 -35 -26 - 17 0 8 1 9 210 3 11 4 125 136 147 158 169 17 22 16 23 17 24 18 25 1926 2027 21282229 30 -7 10 18 11 19 12 20 13 21 14 15 Days post TAVI 98 patients (27. 8%)
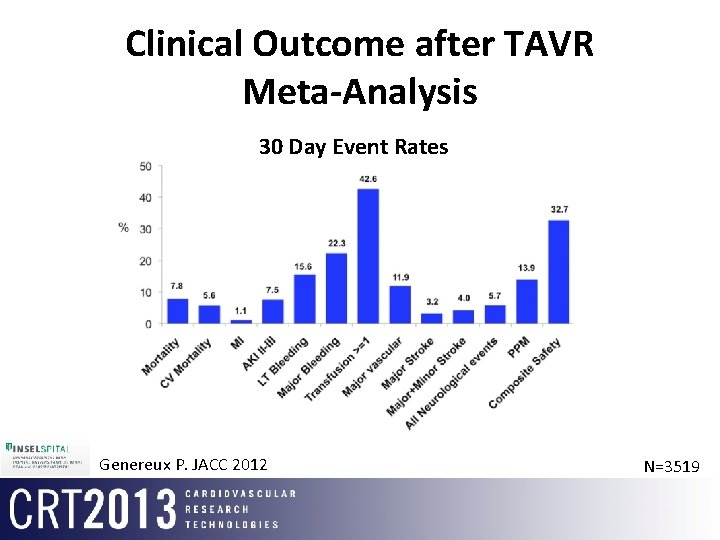
Clinical Outcome after TAVR Meta-Analysis 30 Day Event Rates Genereux P. JACC 2012 N=3519
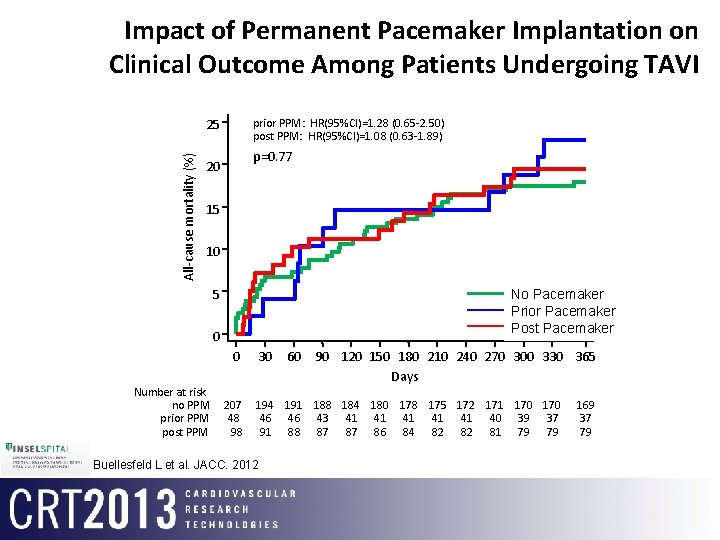
Impact of Permanent Pacemaker Implantation on Clinical Outcome Among Patients Undergoing TAVI All-cause mortality (%) 25 prior PPM: HR(95%CI)=1. 28 (0. 65 -2. 50) post PPM: HR(95%CI)=1. 08 (0. 63 -1. 89) p=0. 77 20 15 10 5 PPM Nono. Pacemaker prior. Pacemaker PPM Prior post. Pacemaker PPM Post 0 0 Number at risk no PPM prior PPM post PPM 207 48 98 30 60 90 120 150 180 210 240 270 300 330 365 Days 194 191 188 184 180 178 175 172 171 170 46 46 43 41 41 41 40 39 37 91 88 87 87 86 84 82 82 81 79 79 Buellesfeld L et al. JACC. 2012 169 37 79
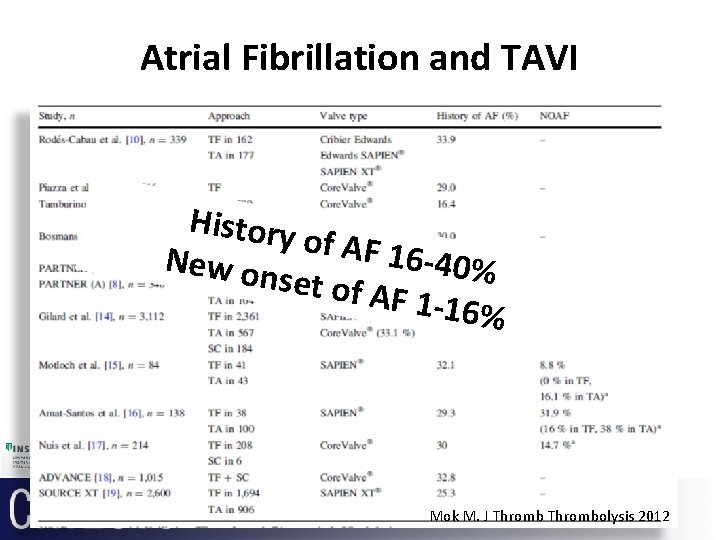
Atrial Fibrillation and TAVI History of AF 16 New on -40% set of A F 1 -16% Mok M. J Thrombolysis 2012
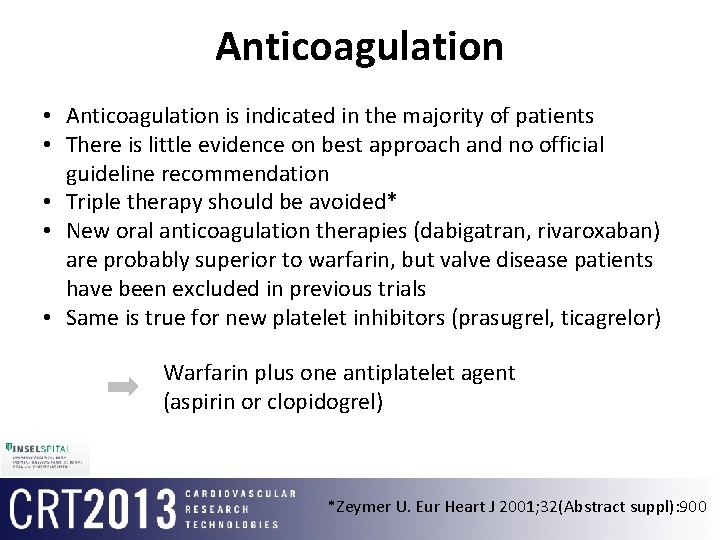
Anticoagulation • Anticoagulation is indicated in the majority of patients • There is little evidence on best approach and no official guideline recommendation • Triple therapy should be avoided* • New oral anticoagulation therapies (dabigatran, rivaroxaban) are probably superior to warfarin, but valve disease patients have been excluded in previous trials • Same is true for new platelet inhibitors (prasugrel, ticagrelor) Warfarin plus one antiplatelet agent (aspirin or clopidogrel) *Zeymer U. Eur Heart J 2001; 32(Abstract suppl): 900
Thank you
- Slides: 14