Managing Lower Limb Swelling Chronic Oedema and Lymphoedema
Managing Lower Limb Swelling, Chronic Oedema and Lymphoedema
Objective of session • Overview of Chronic Oedema and Lymphoedema • Management of Chronic Oedema/Lymphoedema • Compression Hosiery and Lymphoedema • Lymphoedema, facts and data overview • Hosiery prescribing challenges
Chronic Oedema ‘Chronic oedema is the broad term used to describe oedema which has been present for more than 3 months. Oedema which develops as a result in failure of the lymphatic system is referred to as Lymphoedema but chronic oedema may have a more complex underlying aetiology’ (Moffatt et al 2003)
Primary and Secondary Lymphoedema Primary Lymphoedema • Arises from an intrinsic defect in lymph pathways. It can be present at birth, in early childhood or in adult life. It may be inherited. Secondary Lymphoedema • This is a result of damage to the lymphatic system for e. g. cancer treatments (surgery or radiotherapy), trauma, inflammation and venous disease.

Referred to as the third part of the circulatory system or overflow pipe
What are the underlying causes of swelling? • Cardiac failure • Renal failure • Tumour obstructing lymph vessels/nodes • Surgery • Radiotherapy • Metastatic disease • Low serum protein/albumin • DVT • Malformation of the lymphatic system • Rheumatoid arthritis • Hypothyroidism • Paralysis/dependency • Filarisis • Venous disease • Drug induced e. g. NSAID’s • Obesity • Lipoedema

Primary Lymphoedema
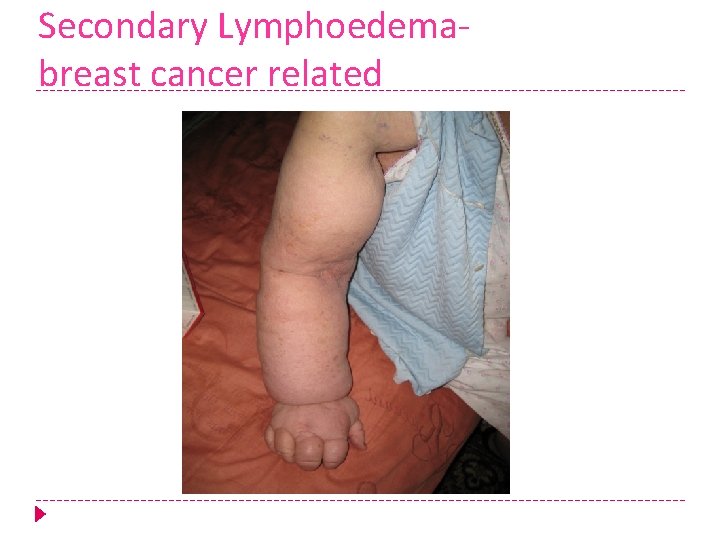
Secondary Lymphoedemabreast cancer related

Chronic Oedema

Lymphovenous Oedema

Obesity related Lymphoedema

Obesity related
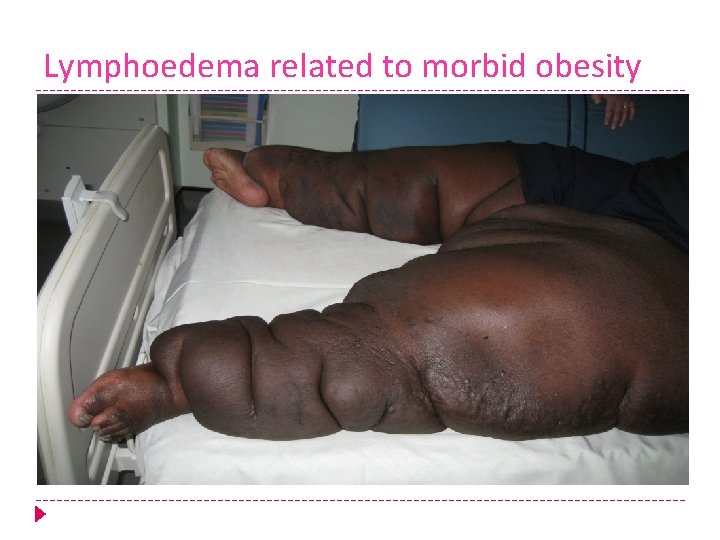
Lymphoedema related to morbid obesity

Lipoedema

Trauma Related

The Complexities !

Complexities
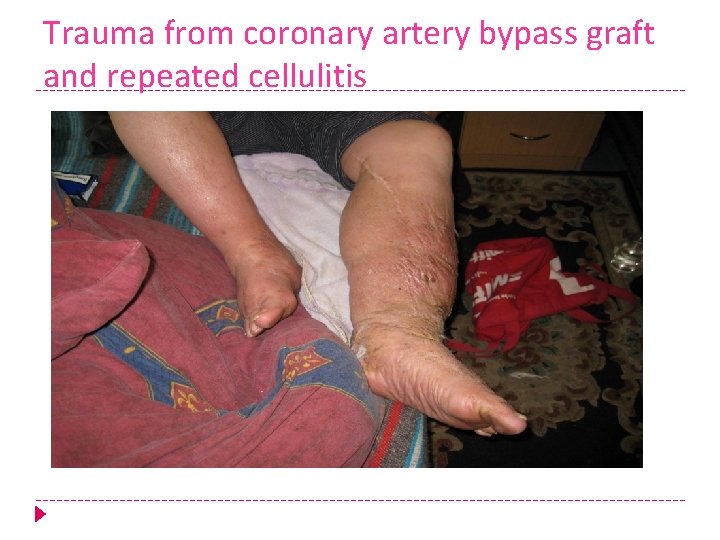
Trauma from coronary artery bypass graft and repeated cellulitis

Skin changes! Papilloma Peau d’orange

The effect on quality of life! Leaking Decreased mobility
Although there are multiple causes for swelling the biggest challenges for us will be! • Complex and chronic with often multiple underlying aetiologies • Obesity related oedema • Cardiac Oedema • Dependency (wet and weepy legs) • Prevention (particularly post surgery)
Understanding Lymphoedema Lack of knowledge leads to- • Misdiagnosis • Inappropriate treatment • Late referral to appropriate HCP • Development of co-morbidities • Negative impact on quality of life • Physical and psychosocial problems • Increased cost to NHS and the economy
Diagnosis of Lymphoedema • Swelling present for 3 months or longer • Swelling does not reduce overnight or on elevation • Skin changes- thickened, dry, dilated lymph vessels • Tissue changes in consistency, become firm/hard, maybe non pitting • Positive stemmer sign • Recurrent infections
Treatment and Management • Will depend on the diagnosis • Comprehensive assessment • Identifying risk factors any contraindications to treatment • Specific to the individual • Burden of treatment should not outweigh the benefits
Basic Cornerstones of Lymphoedema Care • Skin Care • Exercise • Compression ( garments/ bandaging) • Massage
Skin Care Ø Daily skin inspection Ø Appropriate hygiene (avoid soap and scented products) Emollient therapy (moisturise frequently) Ø Skin protection (avoid insect bites, cuts, burns) Ø To maintain skin integrity To prevent infections such as cellulitis To recognise signs of infection To improve skin appearance (self-image) (Skills for practice, 2009)
Exercise Muscle pumping exercises Ø Maintain range of motion Ø Encourage mobility & elevation at rest Ø Avoid high impact exercises or heavy weights Ø Beware of over exercising (increased muscle mass) Ø To promote lymphatic drainage To promote venous return To improve mobility & functional capacity To improve psychological wellbeing (Lymphoedema Framework, 2006)
Manual Lymphatic Drainage Ø Ø Gentle massage technique that aims to “encourage fluid away from congested areas by increasing activity of normal lymphatics” (Lymphoedema Framework, 2006) MLD has otherapeutic benefits: induces relaxation, relieves pain, and improves scar tissue (Willis, 2004) Has to be delivered by trained, qualified practitioners Sessions are opportunities to teach Simple Lymphatic Drainage and establish an effective patient-therapist relationship To promote lymphatic drainage To provide psychological & symptomatic benefits To promote patient education & self-management
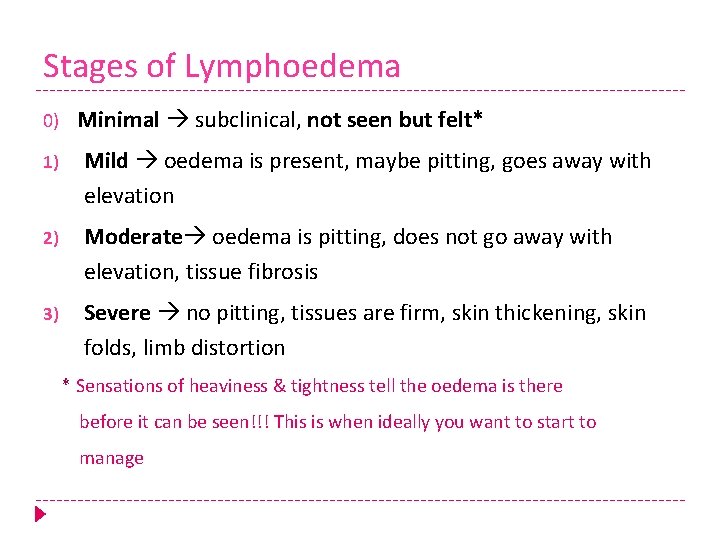
Stages of Lymphoedema 0) Minimal subclinical, not seen but felt* 1) Mild oedema is present, maybe pitting, goes away with elevation 2) Moderate oedema is pitting, does not go away with elevation, tissue fibrosis 3) Severe no pitting, tissues are firm, skin thickening, skin folds, limb distortion * Sensations of heaviness & tightness tell the oedema is there before it can be seen!!! This is when ideally you want to start to manage
Compression hosiery when? ? • Prophylaxis • Maintenance-initial treatment • Following intensive treatment • Variations apply in wear times

Vascular assessment ABPI: <0. 6 - 0. 8: reduced compression ABPI <0. 5: no compression ABPI – Discussion

How can we engage patients in long term maintenance? ØUnderstanding patient motivation ØPrevious experience, knowledge and understanding of management, future expectations Øinformation leaflets on prevention (e. g. leg elevation), hosiery management etc. ØRegular review in the early stages
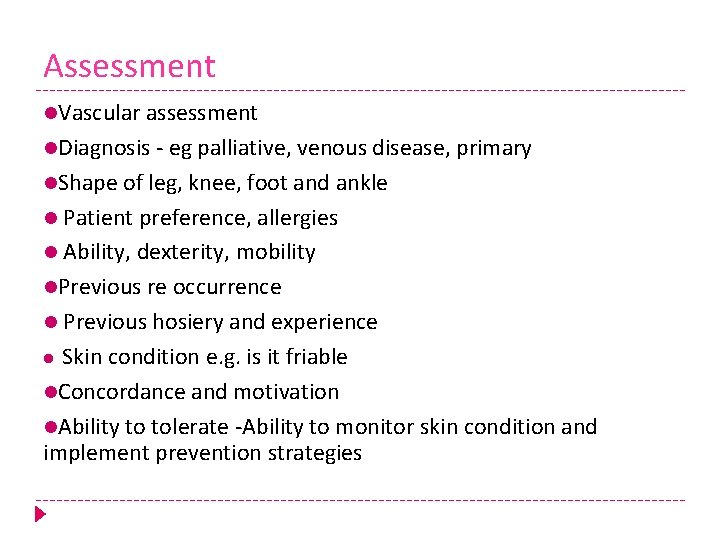
Assessment Vascular assessment Diagnosis - eg palliative, venous disease, primary Shape of leg, knee, foot and ankle Patient preference, allergies Ability, dexterity, mobility Previous re occurrence Previous hosiery and experience Skin condition e. g. is it friable Concordance and motivation Ability to tolerate -Ability to monitor skin condition and implement prevention strategies
Challenges Arthritis Breathlessness Overweight Cannot reach feet Ability to report a problem

Flat knit or circular knit!! Ø Flat knit useful for distortion or deep skin folds Ø Circular knit for regular shape Ø Consider stiffness alongside class? ? Ø What works for the patient? ? ?
Hosiery standard British Hosiery: Circular Knit is not really suitable for advanced stages of lymphoedema where the limb may be distorted as it tends to cut into the skin folds European or Continental Hosiery: Flat knit useful for distortion or deep skin folds (Parstch et al 2006: The stiffer garment will offer greater working pressures but similar resting pressures)
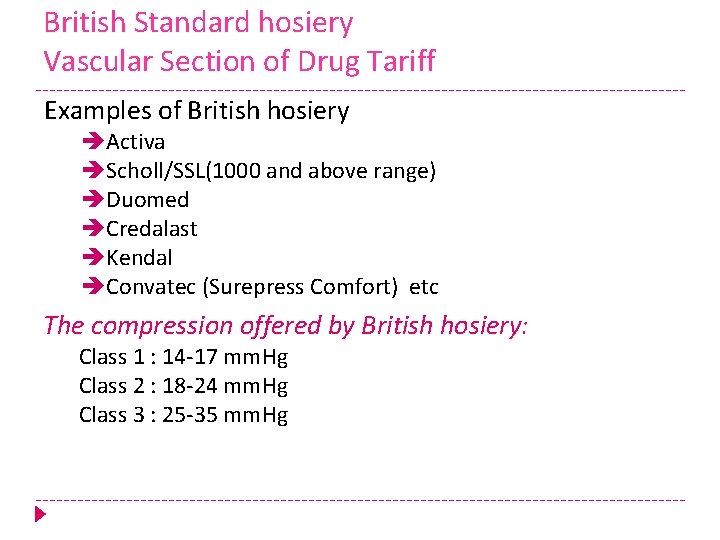
British Standard hosiery Vascular Section of Drug Tariff Examples of British hosiery Activa Scholl/SSL(1000 and above range) Duomed Credalast Kendal Convatec (Surepress Comfort) etc The compression offered by British hosiery: Class 1 : 14 -17 mm. Hg Class 2 : 18 -24 mm. Hg Class 3 : 25 -35 mm. Hg
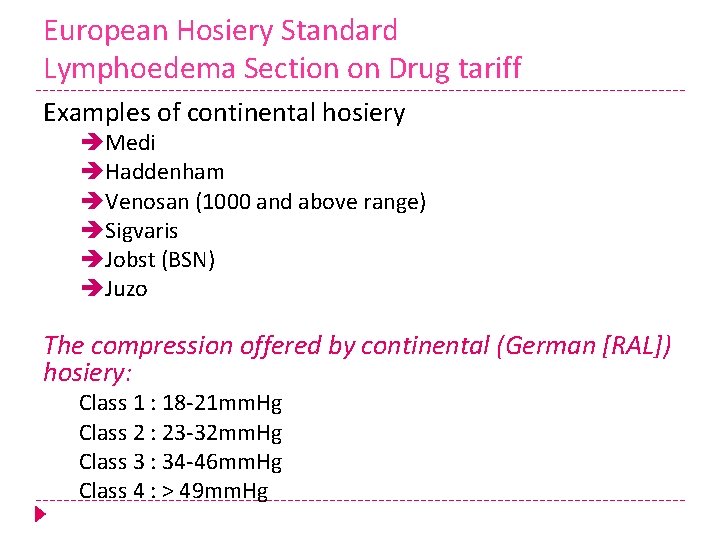
European Hosiery Standard Lymphoedema Section on Drug tariff Examples of continental hosiery Medi Haddenham Venosan (1000 and above range) Sigvaris Jobst (BSN) Juzo The compression offered by continental (German [RAL]) hosiery: Class 1 : 18 -21 mm. Hg Class 2 : 23 -32 mm. Hg Class 3 : 34 -46 mm. Hg Class 4 : > 49 mm. Hg
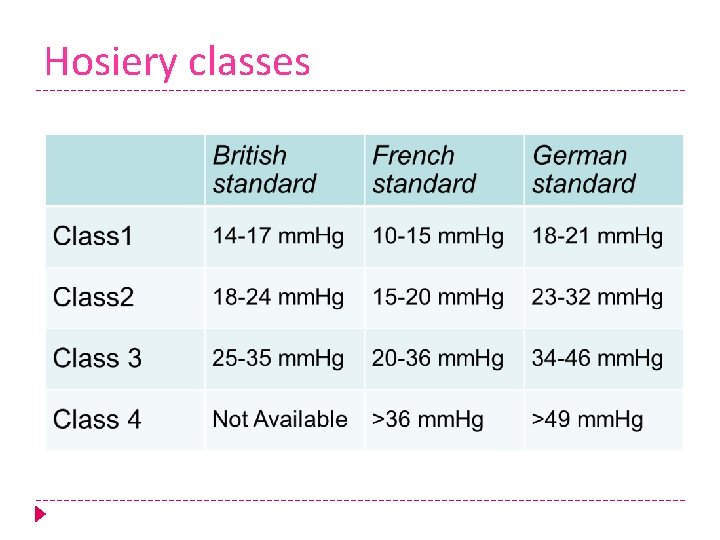
Hosiery classes

Toe garments

Aids to support self care A slip-aid or socket helps the hosiery over the dorsum of the foot Rubber gloves improve grip (if no latex allergy!) Keep nails short Two Class 1 socks may be easier to apply than one Class two All wrinkles should be smoothed out Do not pull the sock so much that there is excessive hosiery at the calf Use of hosiery aids - hosiery frames are only really of use if the client has a slim leg and a mobile ankle.
Lymphoedema Services Inequity continues limited services throughout the UK Community based Lymphoedema care has a significant impact in reducing cellulitis and Lymphorrhoea (leaky Legs) Long term management in maintaining the oedema creates a cost effective model Access to specialist care improves quality of life Early intervention stems the tide of chronicity

Map of London Boroughs
Prevalence – What we know! A previous study by Moffatt et al in 2003 indicated prevalence of chronic oedema to be 1. 33/1, 000 population In 2012 -2013 the prevalence within based on the population of Tower Hamlets being 254, 000 was 1. 95/1, 000 population In 2013 -2014 the prevalence based on the adjusted population 255, 245 was 2. 2/1, 000 population
Estimated prevalence based on 1. 33/1, 000 population Tower Hamlets-398 City and Hackney-416 CCG’s with no established pathway Newham-483 Waltham Forest- 473 Havering -526 Redbrige-497 Barking and Dagenham-324 Total estimated prevalence with no dedicated service 2, 303
From our experience what we might expect to see in a defined population Male/Female ratio is usually more weighted to female a 70%30% Predominant site will be bilateral lower limb, correlating with a high incidence of dependency and Lymphovenous oedema Cancer related Lymphoedema 15 -20% Aproximatley 50% of an established caseload will have multiple co morbidities Aproximatley 50% of the caseload patients will be obese and this will complicate management Incidence increases by age in the over 65’s 8 -10% of patients discharged, will require re referral to be supported in life long management
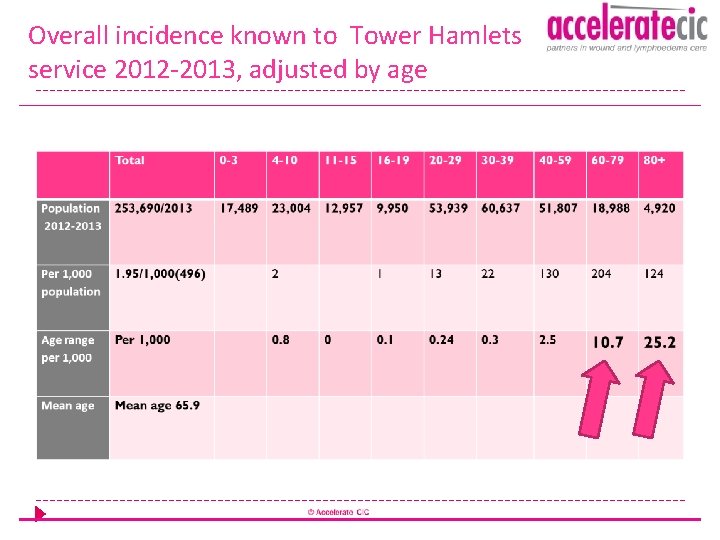
Overall incidence known to Tower Hamlets service 2012 -2013, adjusted by age
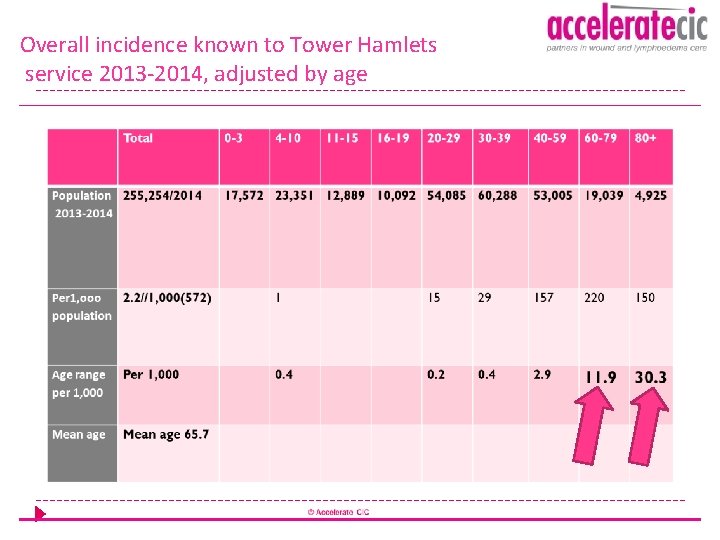
Overall incidence known to Tower Hamlets service 2013 -2014, adjusted by age

Prevalence of cellulitis prior to referral 30. 4% of all patients had at least one episode of cellulitis 2012 -2013 29. 8% of all patients had at least one episode of cellulitis 2013 -2014 28% of all patients had at least one episode of cellulitis 2014 -2015

Tower Hamlets Outcomes 2014 -2015 97% elimination of Lymphorrhoea 97% of patients achieved maintenance April 2014 -March 2015 A 90% reduction in cellulitis admissions post treatment has been achieved 88% reduction on cellulitis post treatment

City and Hackney Service -Launched April 2015 outcomes month 5 Ø 100% referral for Lymphorrhoea seen within 10 working days Ø 82% patients with Lymphorrhoea halted within 2 weeks Ø 100% patients with personalised care plans Ø 94% reduction in cellulitis episodes Ø 87% reduction in cellulitis admissions

Our Vision for Community Lymphoedema Services Early prevention and joined up, solution focussed care Joint working with Tissue Viability and Community Nursing recommended Ownership of chronic oedema required within a long term conditions framework!! Bring our motivation: deliver more specialist, bespoke and creative care Deliver for Commissioning through better economic evaluation of the system Empowered patients who demand change, understanding their triggers and schooled in self-management

Prescribing Challenges Discussion!

Accelerate Lymphoedema service will: • Take referrals from all healthcare professionals • Provide assessment , review and management both in clinics and home visits • Work with practitioners • Provide professional education • Work towards supporting patient
References 1) Skills for Practice (2009) Management of Chronic Oedema in the Community. Aberdeen: Wounds UK. 2) The Lymphoedema Framework (2006) Best Practice for the Management of Lymphoedema. International consensus. London: MEP Ltd. 3) The Lymphoedema Framework (2006) Best Practice for the Management of Lymphoedema. International consensus. London: MEP Ltd. 4) Willis, A. (2004) ‘Manual Lymphatic Drainage and its therapeutic benefits’, Positive Health, 104, pp. 51 -54

Thank You
- Slides: 56