Managing Complications in Postpartum Period Puerperal Sepsis Learning
- Slides: 9
Managing Complications in Postpartum Period: Puerperal Sepsis
Learning Objectives By the end of this session, the learners will be able to: • Define maternal/puerperal sepsis • Enumerate the risk factors for maternal sepsis • Explain ways to prevent sepsis • Describe the causes, symptoms, signs and management of sepsis • List the indications for antibiotics in mother • Discuss the Go. I’s recommendation of broad spectrum antibiotics 2
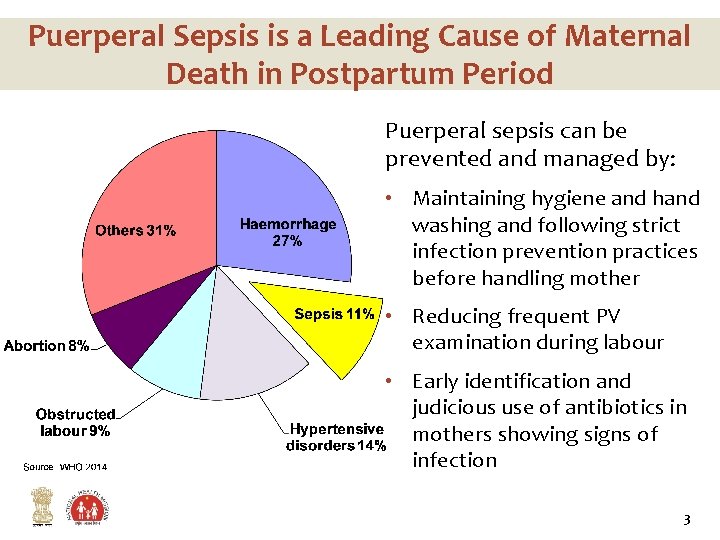
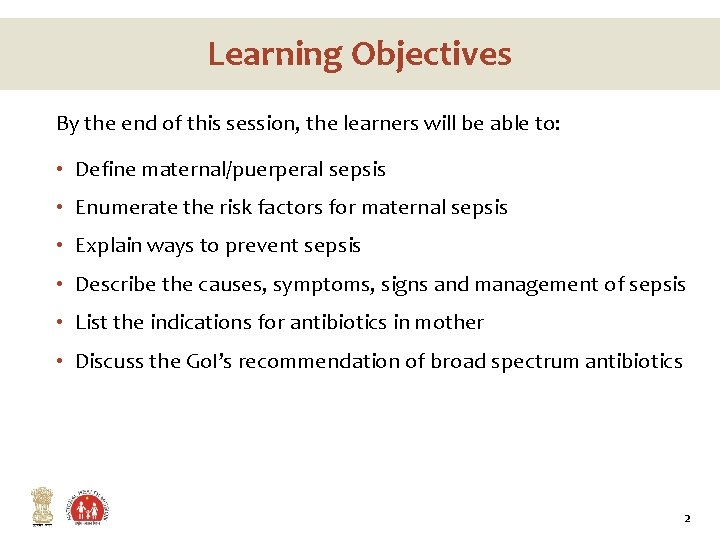
Puerperal Sepsis is a Leading Cause of Maternal Death in Postpartum Period Puerperal sepsis can be prevented and managed by: • Maintaining hygiene and hand washing and following strict infection prevention practices before handling mother • Reducing frequent PV examination during labour • Early identification and judicious use of antibiotics in mothers showing signs of infection 3
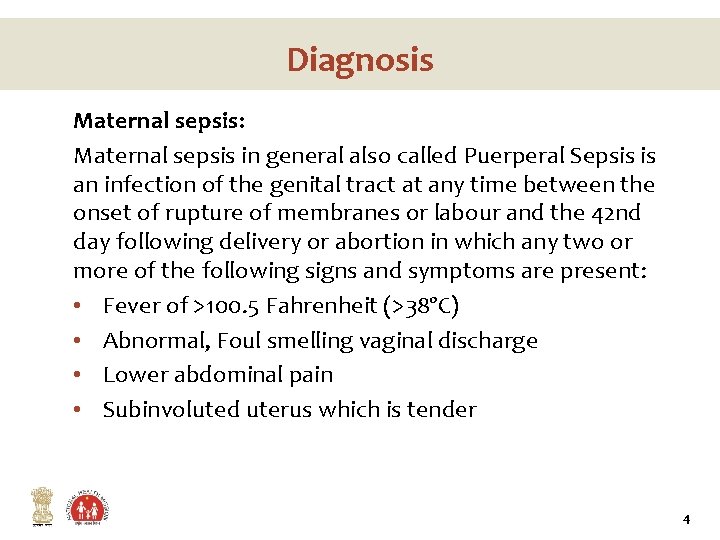
Diagnosis Maternal sepsis: Maternal sepsis in general also called Puerperal Sepsis is an infection of the genital tract at any time between the onset of rupture of membranes or labour and the 42 nd day following delivery or abortion in which any two or more of the following signs and symptoms are present: • Fever of >100. 5 Fahrenheit (>38ºC) • Abnormal, Foul smelling vaginal discharge • Lower abdominal pain • Subinvoluted uterus which is tender 4
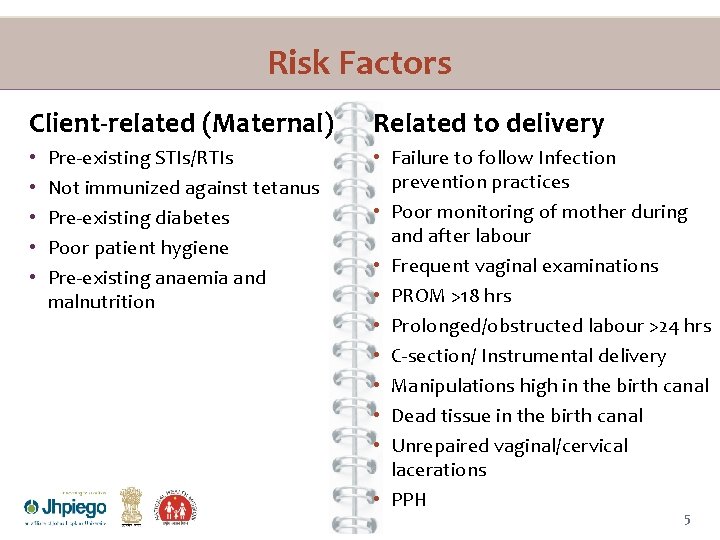
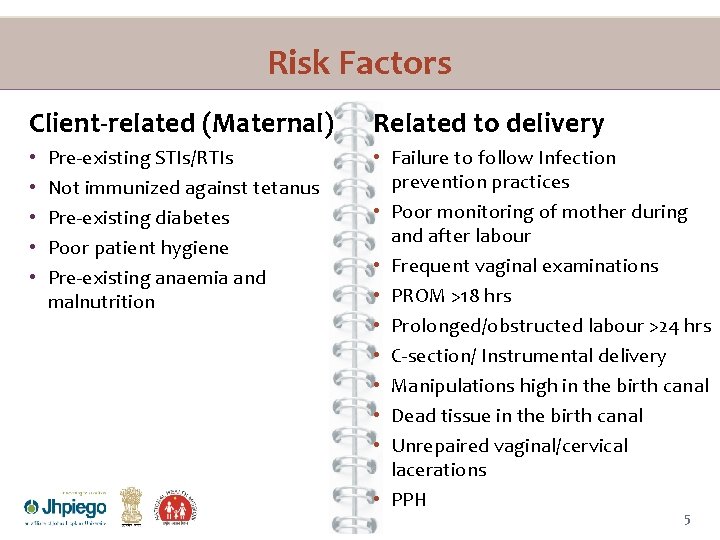
Risk Factors Client-related (Maternal) • • • Pre-existing STIs/RTIs Not immunized against tetanus Pre-existing diabetes Poor patient hygiene Pre-existing anaemia and malnutrition Related to delivery • Failure to follow Infection prevention practices • Poor monitoring of mother during and after labour • Frequent vaginal examinations • PROM >18 hrs • Prolonged/obstructed labour >24 hrs • C-section/ Instrumental delivery • Manipulations high in the birth canal • Dead tissue in the birth canal • Unrepaired vaginal/cervical lacerations • PPH 5
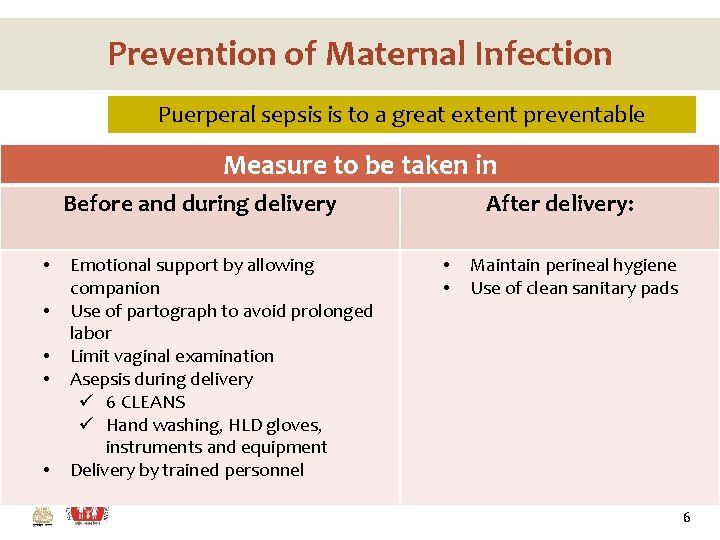
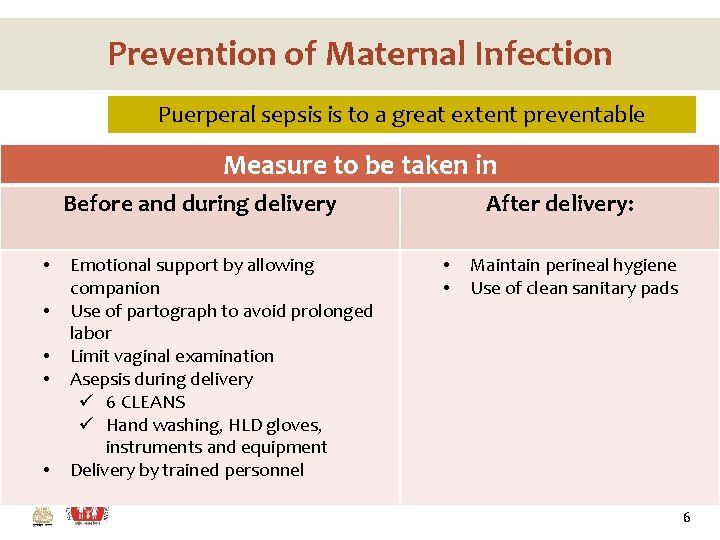
Prevention of Maternal Infection Puerperal sepsis is to a great extent preventable Measure to be taken in Before and during delivery • • • Emotional support by allowing companion Use of partograph to avoid prolonged labor Limit vaginal examination Asepsis during delivery ü 6 CLEANS ü Hand washing, HLD gloves, instruments and equipment Delivery by trained personnel After delivery: • • Maintain perineal hygiene Use of clean sanitary pads 6
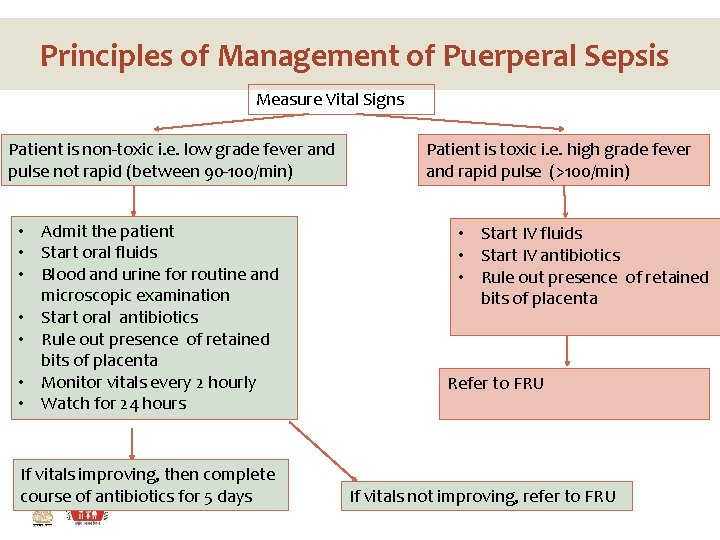
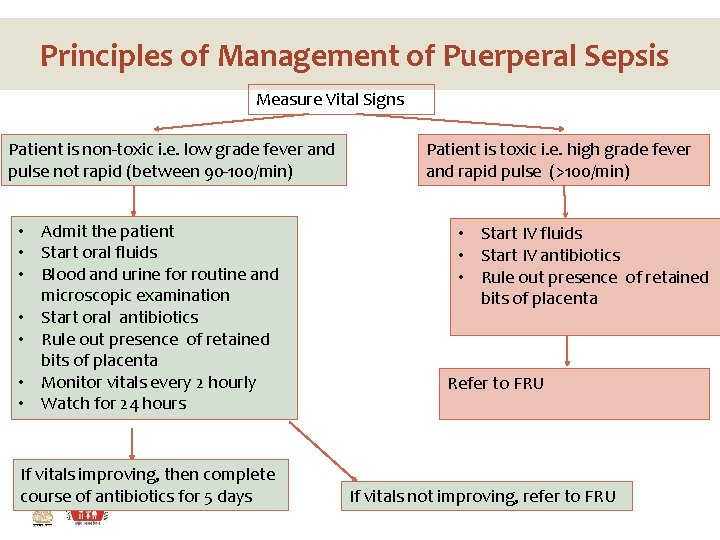
Principles of Management of Puerperal Sepsis Measure Vital Signs Patient is non-toxic i. e. low grade fever and pulse not rapid (between 90 -100/min) • Admit the patient • Start oral fluids • Blood and urine for routine and microscopic examination • Start oral antibiotics • Rule out presence of retained bits of placenta • Monitor vitals every 2 hourly • Watch for 24 hours If vitals improving, then complete course of antibiotics for 5 days Patient is toxic i. e. high grade fever and rapid pulse (>100/min) • Start IV fluids • Start IV antibiotics • Rule out presence of retained bits of placenta Refer to FRU If vitals not improving, refer to FRU
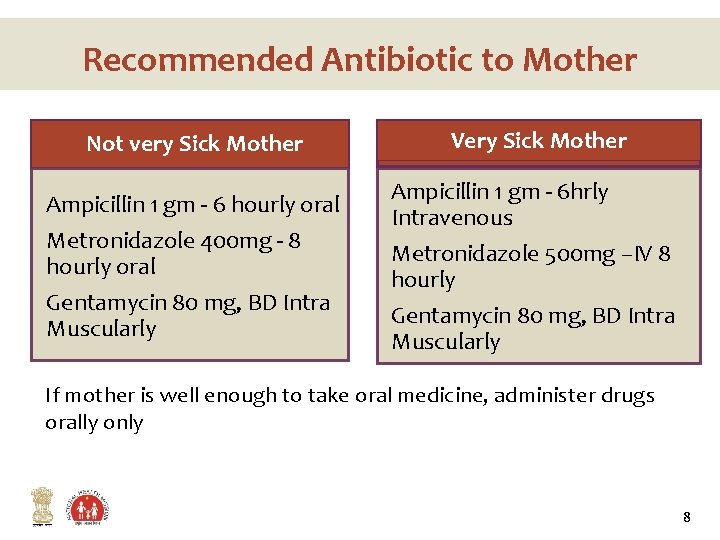
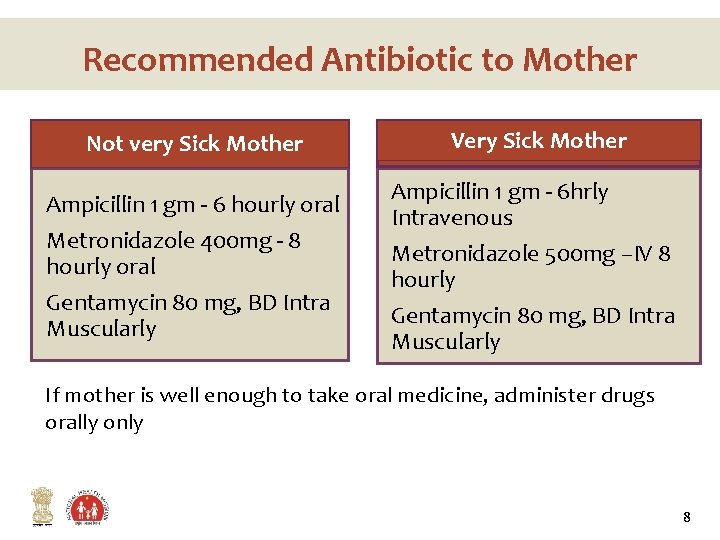
Recommended Antibiotic to Mother Not very Sick Mother Ampicillin 1 gm - 6 hourly oral Metronidazole 400 mg - 8 hourly oral Gentamycin 80 mg, BD Intra Muscularly Very Sick Mother Ampicillin 1 gm - 6 hrly Intravenous Metronidazole 500 mg –IV 8 hourly Gentamycin 80 mg, BD Intra Muscularly If mother is well enough to take oral medicine, administer drugs orally only 8
Key messages • Puerperal sepsis is one of the leading causes of maternal deaths • Puerperal sepsis is to a great extent preventable • Antibiotics should be given to the woman only if they are indicated • At periphery, ANM should identify the indications for antibiotics and give first dose before referral 9