Management of Vitamin D Deficiency in Adults Guidance

- Slides: 12
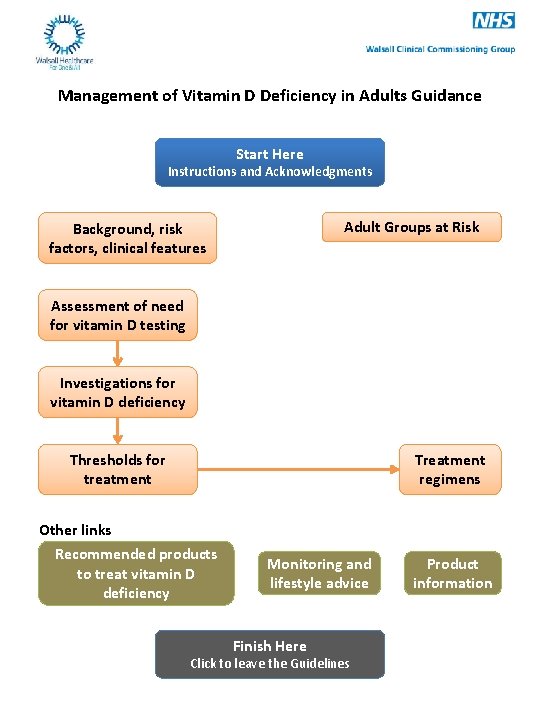
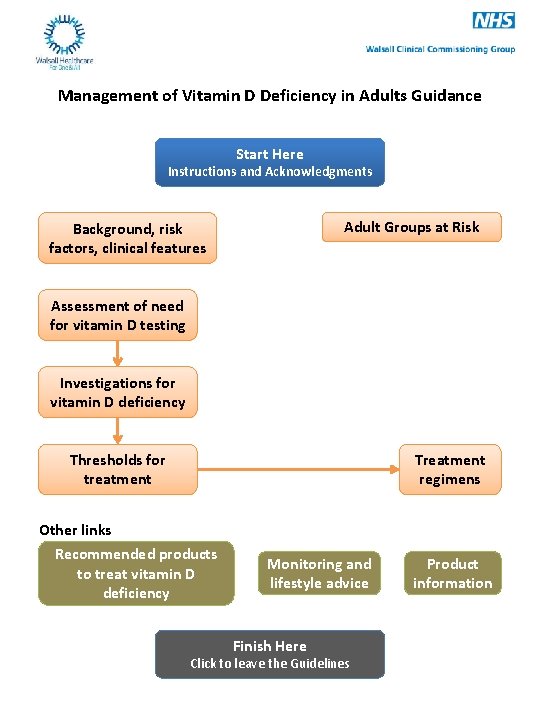
Management of Vitamin D Deficiency in Adults Guidance Start Here Instructions and Acknowledgments Adult Groups at Risk Background, risk factors, clinical features Assessment of need for vitamin D testing Investigations for vitamin D deficiency Treatment regimens Thresholds for treatment Other links Recommended products to treat vitamin D deficiency Monitoring and lifestyle advice Finish Here Click to leave the Guidelines Product information
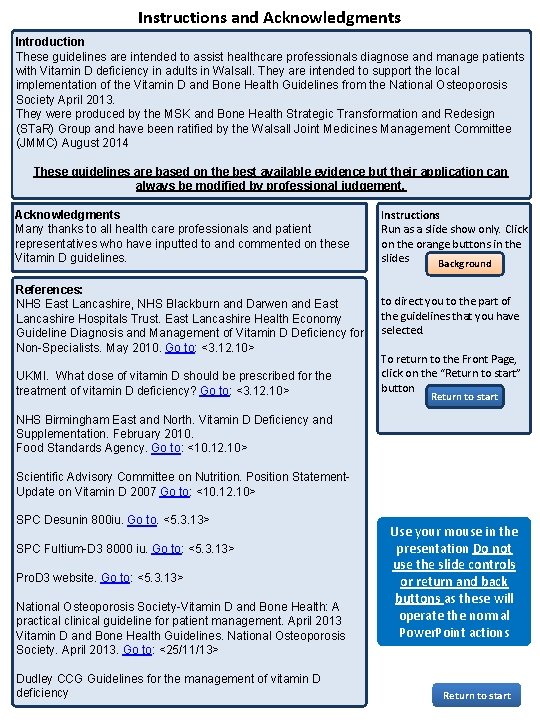
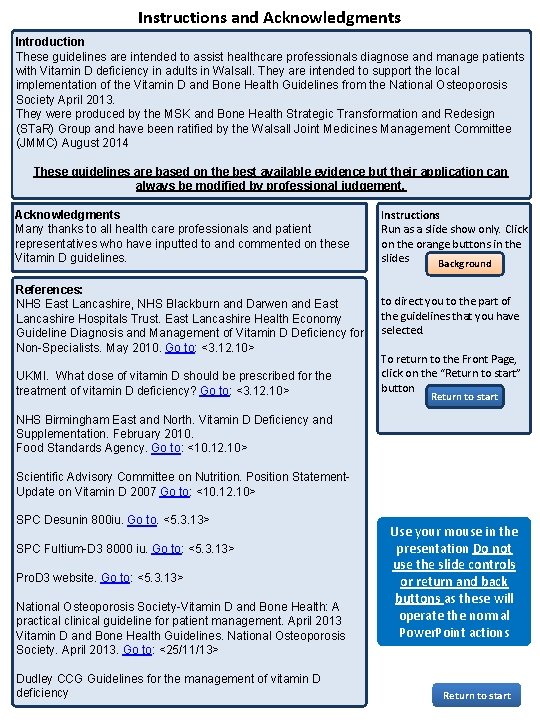
Instructions and Acknowledgments Introduction These guidelines are intended to assist healthcare professionals diagnose and manage patients with Vitamin D deficiency in adults in Walsall. They are intended to support the local implementation of the Vitamin D and Bone Health Guidelines from the National Osteoporosis Society April 2013. They were produced by the MSK and Bone Health Strategic Transformation and Redesign (STa. R) Group and have been ratified by the Walsall Joint Medicines Management Committee (JMMC) August 2014 These guidelines are based on the best available evidence but their application can always be modified by professional judgement. Acknowledgments Many thanks to all health care professionals and patient representatives who have inputted to and commented on these Vitamin D guidelines. Instructions Run as a slide show only. Click on the orange buttons in the slides Background References: NHS East Lancashire, NHS Blackburn and Darwen and East Lancashire Hospitals Trust. East Lancashire Health Economy Guideline Diagnosis and Management of Vitamin D Deficiency for Non-Specialists. May 2010. Go to: <3. 12. 10> to direct you to the part of the guidelines that you have selected. UKMI. What dose of vitamin D should be prescribed for the treatment of vitamin D deficiency? Go to: <3. 12. 10> To return to the Front Page, click on the “Return to start” button Return to start NHS Birmingham East and North. Vitamin D Deficiency and Supplementation. February 2010. Food Standards Agency. Go to: <10. 12. 10> Scientific Advisory Committee on Nutrition. Position Statement. Update on Vitamin D 2007 Go to: <10. 12. 10> SPC Desunin 800 iu. Go to. <5. 3. 13> SPC Fultium-D 3 8000 iu. Go to: <5. 3. 13> Pro. D 3 website. Go to: <5. 3. 13> National Osteoporosis Society-Vitamin D and Bone Health: A practical clinical guideline for patient management. April 2013 Vitamin D and Bone Health Guidelines. National Osteoporosis Society. April 2013. Go to: <25/11/13> Dudley CCG Guidelines for the management of vitamin D deficiency Use your mouse in the presentation Do not use the slide controls or return and back buttons as these will operate the normal Power. Point actions Return to start
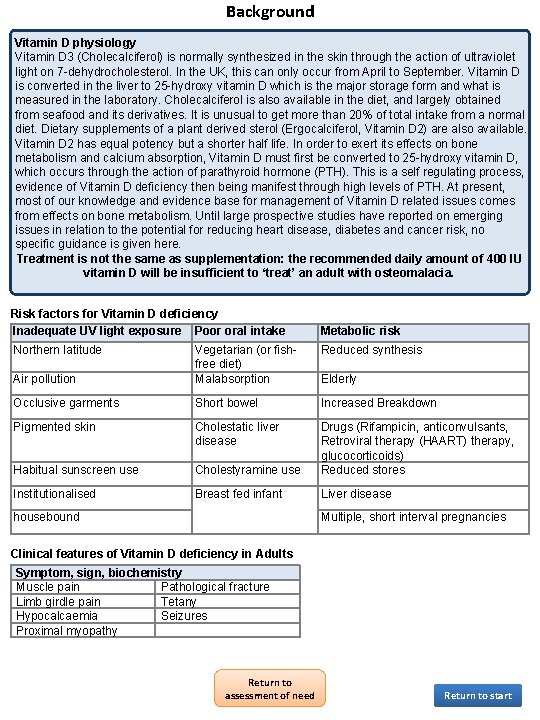
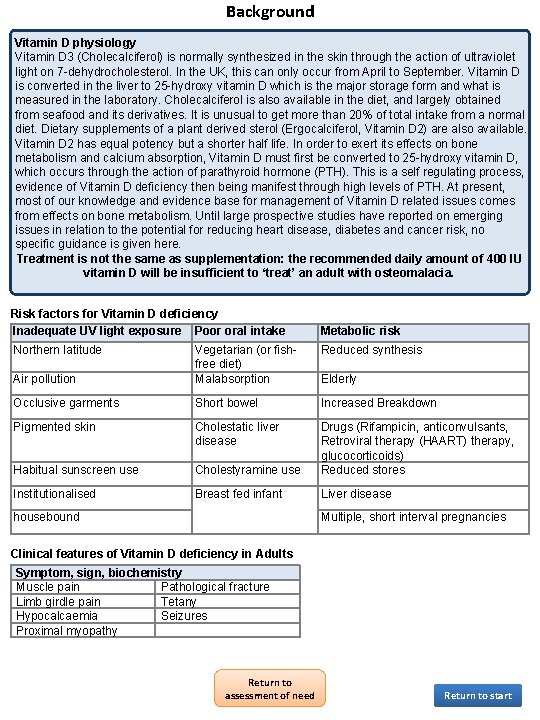
Background Vitamin D physiology Vitamin D 3 (Cholecalciferol) is normally synthesized in the skin through the action of ultraviolet light on 7 -dehydrocholesterol. In the UK, this can only occur from April to September. Vitamin D is converted in the liver to 25 -hydroxy vitamin D which is the major storage form and what is measured in the laboratory. Cholecalciferol is also available in the diet, and largely obtained from seafood and its derivatives. It is unusual to get more than 20% of total intake from a normal diet. Dietary supplements of a plant derived sterol (Ergocalciferol, Vitamin D 2) are also available. Vitamin D 2 has equal potency but a shorter half life. In order to exert its effects on bone metabolism and calcium absorption, Vitamin D must first be converted to 25 -hydroxy vitamin D, which occurs through the action of parathyroid hormone (PTH). This is a self regulating process, evidence of Vitamin D deficiency then being manifest through high levels of PTH. At present, most of our knowledge and evidence base for management of Vitamin D related issues comes from effects on bone metabolism. Until large prospective studies have reported on emerging issues in relation to the potential for reducing heart disease, diabetes and cancer risk, no specific guidance is given here. Treatment is not the same as supplementation: the recommended daily amount of 400 IU vitamin D will be insufficient to ‘treat’ an adult with osteomalacia. Risk factors for Vitamin D deficiency Inadequate UV light exposure Poor oral intake Metabolic risk Northern latitude Reduced synthesis Air pollution Vegetarian (or fishfree diet) Malabsorption Occlusive garments Short bowel Increased Breakdown Pigmented skin Cholestatic liver disease Habitual sunscreen use Cholestyramine use Drugs (Rifampicin, anticonvulsants, Retroviral therapy (HAART) therapy, glucocorticoids) Reduced stores Institutionalised Breast fed infant Liver disease housebound Elderly Multiple, short interval pregnancies Clinical features of Vitamin D deficiency in Adults Symptom, sign, biochemistry Muscle pain Pathological fracture Limb girdle pain Tetany Hypocalcaemia Seizures Proximal myopathy Return to assessment of need Return to start
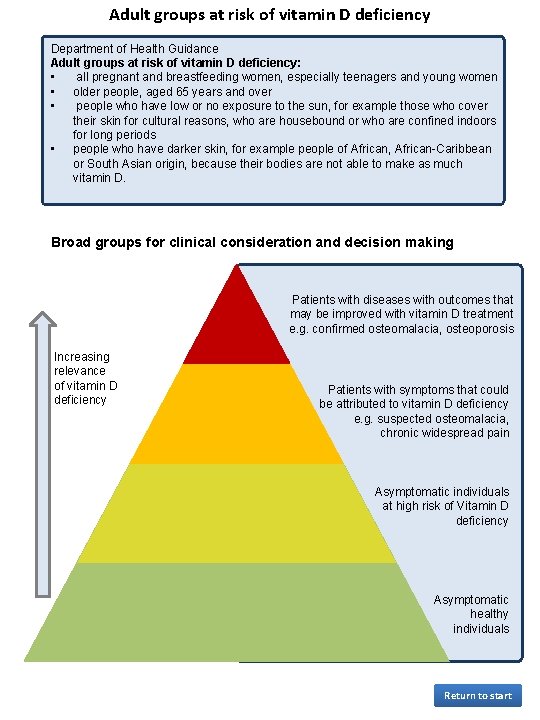
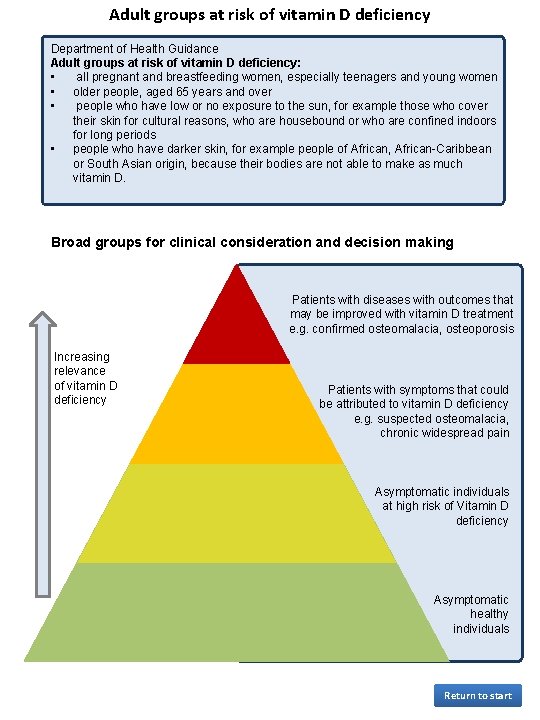
Adult groups at risk of vitamin D deficiency Department of Health Guidance Adult groups at risk of vitamin D deficiency: • all pregnant and breastfeeding women, especially teenagers and young women • older people, aged 65 years and over • people who have low or no exposure to the sun, for example those who cover their skin for cultural reasons, who are housebound or who are confined indoors for long periods • people who have darker skin, for example people of African, African-Caribbean or South Asian origin, because their bodies are not able to make as much vitamin D. Broad groups for clinical consideration and decision making Patients with diseases with outcomes that may be improved with vitamin D treatment e. g. confirmed osteomalacia, osteoporosis Increasing relevance of vitamin D deficiency Patients with symptoms that could be attributed to vitamin D deficiency e. g. suspected osteomalacia, chronic widespread pain Asymptomatic individuals at high risk of Vitamin D deficiency Asymptomatic healthy individuals Return to start
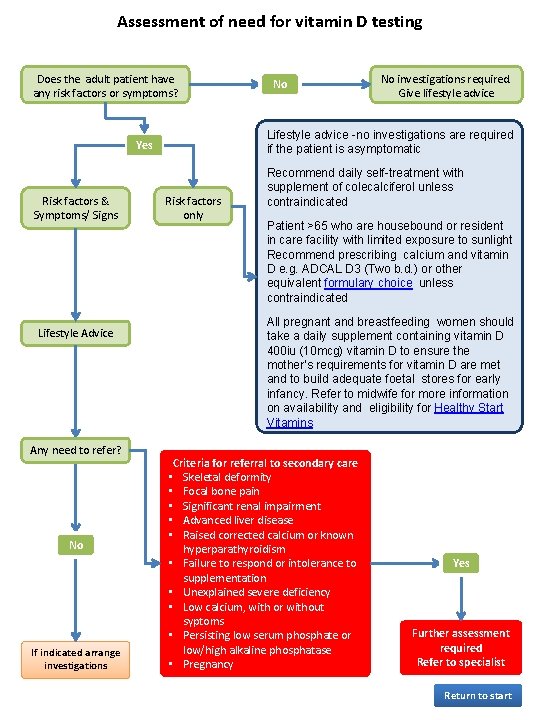
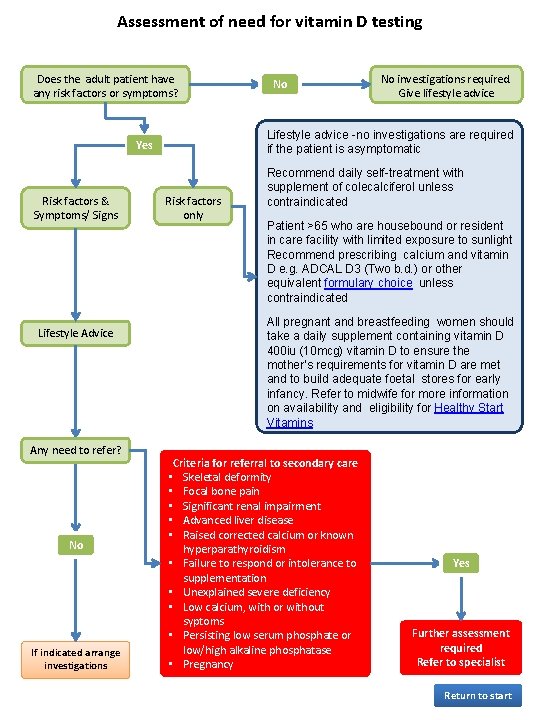
Assessment of need for vitamin D testing Does the adult patient have any risk factors or symptoms? Lifestyle Advice Any need to refer? No If indicated arrange investigations No investigations required. Give lifestyle advice Lifestyle advice -no investigations are required if the patient is asymptomatic Yes Risk factors & Symptoms/ Signs No Risk factors only Recommend daily self-treatment with supplement of colecalciferol unless contraindicated Patient >65 who are housebound or resident in care facility with limited exposure to sunlight Recommend prescribing calcium and vitamin D e. g. ADCAL D 3 (Two b. d. ) or other equivalent formulary choice unless contraindicated All pregnant and breastfeeding women should take a daily supplement containing vitamin D 400 iu (10 mcg) vitamin D to ensure the mother’s requirements for vitamin D are met and to build adequate foetal stores for early infancy. Refer to midwife for more information on availability and eligibility for Healthy Start Vitamins Criteria for referral to secondary care • Skeletal deformity • Focal bone pain • Significant renal impairment • Advanced liver disease • Raised corrected calcium or known hyperparathyroidism • Failure to respond or intolerance to supplementation • Unexplained severe deficiency • Low calcium, with or without syptoms • Persisting low serum phosphate or low/high alkaline phosphatase • Pregnancy Yes Further assessment required Refer to specialist Return to start
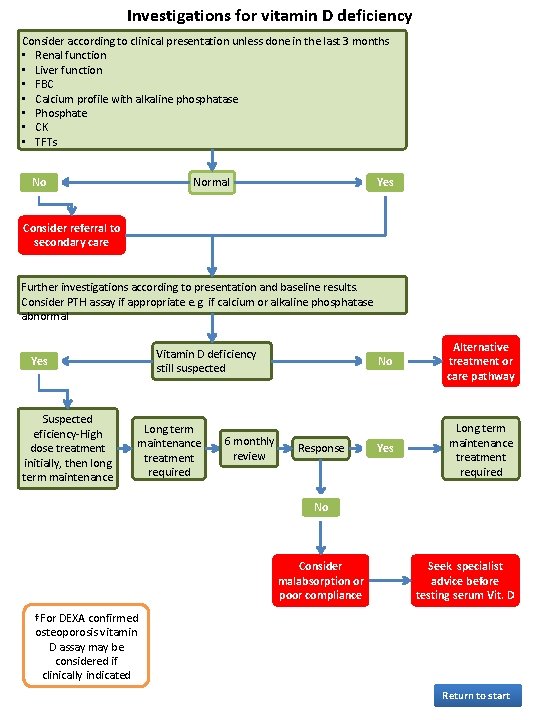
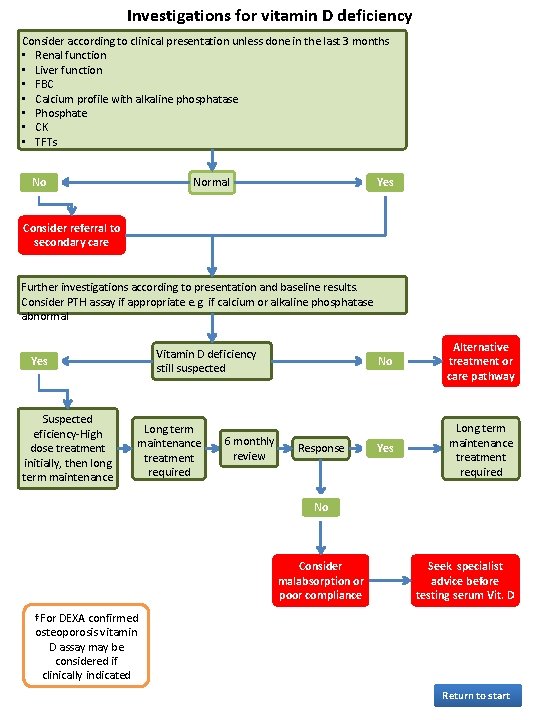
Investigations for vitamin D deficiency Consider according to clinical presentation unless done in the last 3 months • Renal function • Liver function • FBC • Calcium profile with alkaline phosphatase • Phosphate • CK • TFTs No Normal Yes Consider referral to secondary care Further investigations according to presentation and baseline results. Consider PTH assay if appropriate e. g. if calcium or alkaline phosphatase abnormal Vitamin D deficiency still suspected Yes Suspected eficiency-High dose treatment initially, then long term maintenance Long term maintenance treatment required 6 monthly review Response No Alternative treatment or care pathway Yes Long term maintenance treatment required No Consider malabsorption or poor compliance Seek specialist advice before testing serum Vit. D †For DEXA confirmed osteoporosis vitamin D assay may be considered if clinically indicated Return to start
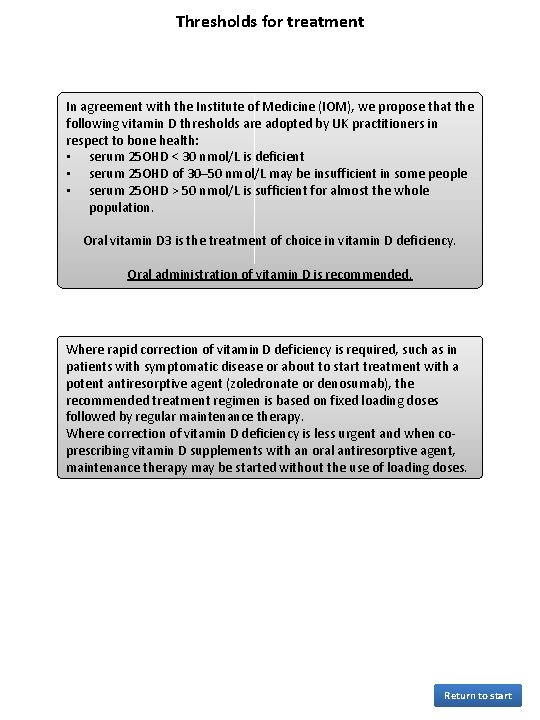
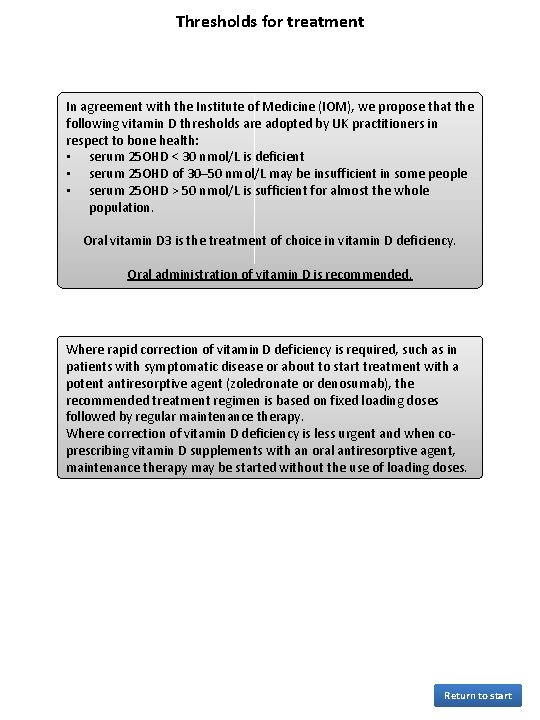
Thresholds for treatment In agreement with the Institute of Medicine (IOM), we propose that the following vitamin D thresholds are adopted by UK practitioners in respect to bone health: • serum 25 OHD < 30 nmol/L is deficient • serum 25 OHD of 30– 50 nmol/L may be insufficient in some people • serum 25 OHD > 50 nmol/L is sufficient for almost the whole population. Oral vitamin D 3 is the treatment of choice in vitamin D deficiency. Oral administration of vitamin D is recommended. Where rapid correction of vitamin D deficiency is required, such as in patients with symptomatic disease or about to start treatment with a potent antiresorptive agent (zoledronate or denosumab), the recommended treatment regimen is based on fixed loading doses followed by regular maintenance therapy. Where correction of vitamin D deficiency is less urgent and when coprescribing vitamin D supplements with an oral antiresorptive agent, maintenance therapy may be started without the use of loading doses. Return to start
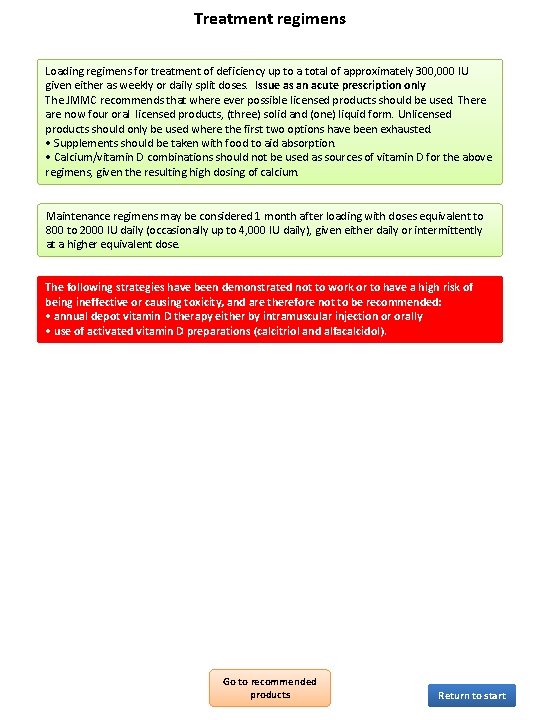
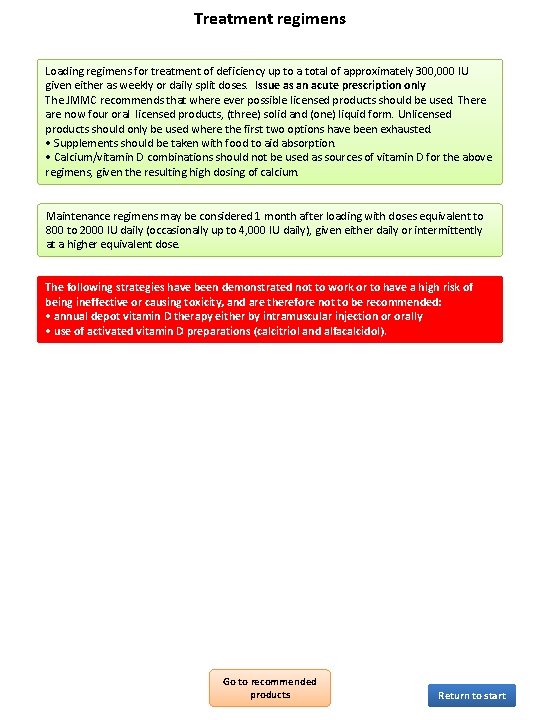
Treatment regimens Loading regimens for treatment of deficiency up to a total of approximately 300, 000 IU given either as weekly or daily split doses. Issue as an acute prescription only The JMMC recommends that where ever possible licensed products should be used. There are now four oral licensed products, (three) solid and (one) liquid form. Unlicensed products should only be used where the first two options have been exhausted. • Supplements should be taken with food to aid absorption. • Calcium/vitamin D combinations should not be used as sources of vitamin D for the above regimens, given the resulting high dosing of calcium. Maintenance regimens may be considered 1 month after loading with doses equivalent to 800 to 2000 IU daily (occasionally up to 4, 000 IU daily), given either daily or intermittently at a higher equivalent dose. The following strategies have been demonstrated not to work or to have a high risk of being ineffective or causing toxicity, and are therefore not to be recommended: • annual depot vitamin D therapy either by intramuscular injection or orally • use of activated vitamin D preparations (calcitriol and alfacalcidol). Go to recommended products Return to start
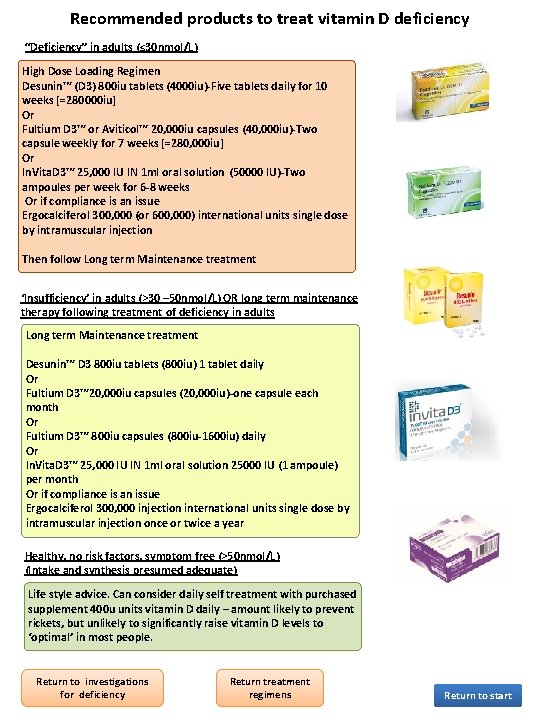
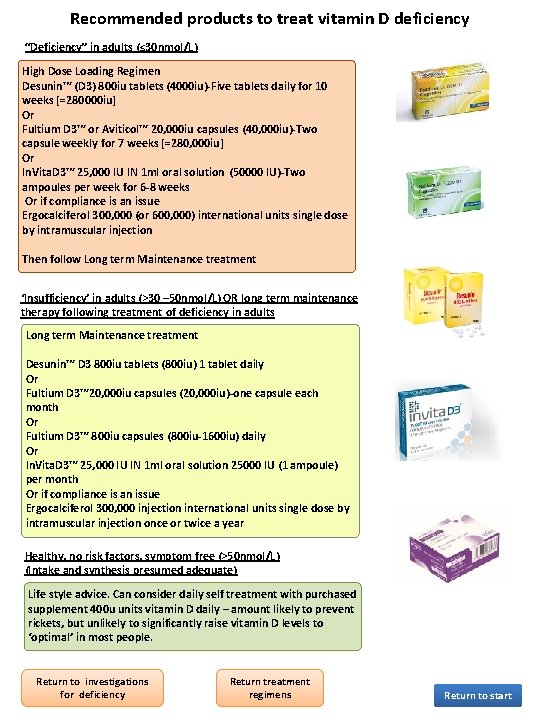
Recommended products to treat vitamin D deficiency “Deficiency” in adults (≤ 30 nmol/L) High Dose Loading Regimen Desunin™ (D 3) 800 iu tablets (4000 iu)-Five tablets daily for 10 weeks [=280000 iu] Or Fultium D 3™ or Aviticol™ 20, 000 iu capsules (40, 000 iu)-Two capsule weekly for 7 weeks [=280, 000 iu] Or In. Vita. D 3™ 25, 000 IU IN 1 ml oral solution (50000 IU)-Two ampoules per week for 6 -8 weeks Or if compliance is an issue Ergocalciferol 300, 000 (or 600, 000) international units single dose by intramuscular injection Then follow Long term Maintenance treatment ‘Insufficiency’ in adults (>30 – 50 nmol/L) OR long term maintenance therapy following treatment of deficiency in adults Long term Maintenance treatment Desunin™ D 3 800 iu tablets (800 iu) 1 tablet daily Or Fultium D 3™ 20, 000 iu capsules (20, 000 iu)-one capsule each month Or Fultium D 3™ 800 iu capsules (800 iu-1600 iu) daily Or In. Vita. D 3™ 25, 000 IU IN 1 ml oral solution 25000 IU (1 ampoule) per month Or if compliance is an issue Ergocalciferol 300, 000 injection international units single dose by intramuscular injection once or twice a year Healthy, no risk factors, symptom free (>50 nmol/L) (Intake and synthesis presumed adequate) Life style advice. Can consider daily self treatment with purchased supplement 400 u units vitamin D daily – amount likely to prevent rickets, but unlikely to significantly raise vitamin D levels to ‘optimal’ in most people. Return to investigations for deficiency Return treatment regimens Return to start
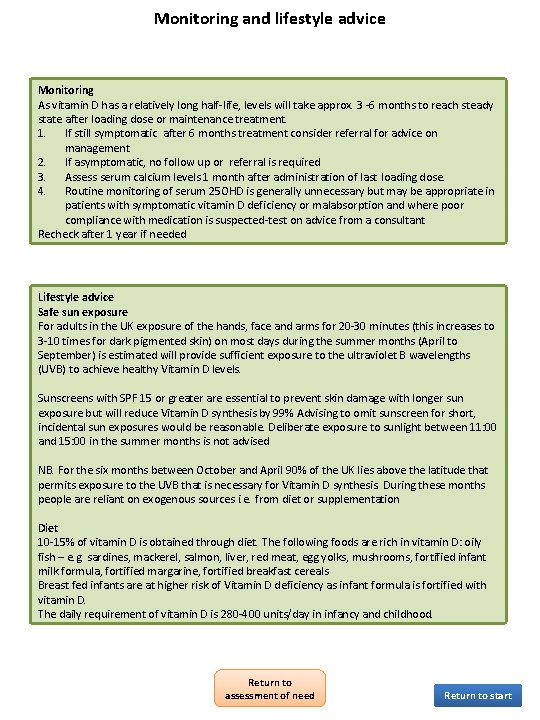
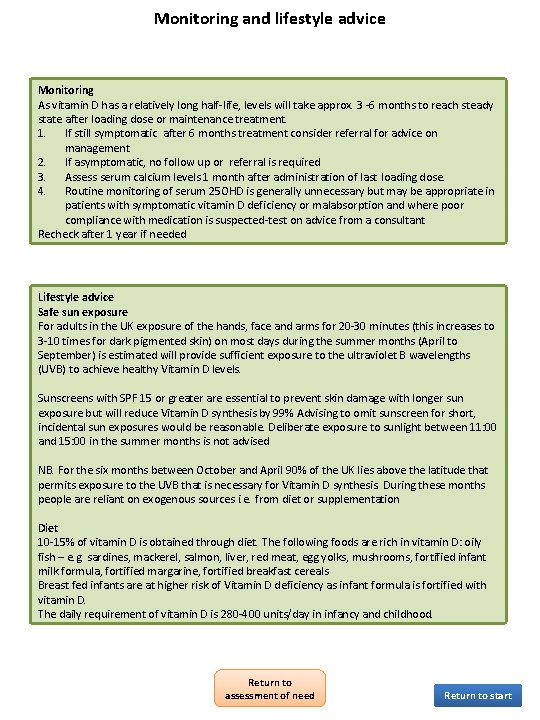
Monitoring and lifestyle advice Monitoring As vitamin D has a relatively long half-life, levels will take approx. 3 -6 months to reach steady state after loading dose or maintenance treatment. 1. If still symptomatic after 6 months treatment consider referral for advice on management 2. If asymptomatic, no follow up or referral is required 3. Assess serum calcium levels 1 month after administration of last loading dose. 4. Routine monitoring of serum 25 OHD is generally unnecessary but may be appropriate in patients with symptomatic vitamin D deficiency or malabsorption and where poor compliance with medication is suspected-test on advice from a consultant Recheck after 1 year if needed Lifestyle advice Safe sun exposure For adults in the UK exposure of the hands, face and arms for 20 -30 minutes (this increases to 3 -10 times for dark pigmented skin) on most days during the summer months (April to September) is estimated will provide sufficient exposure to the ultraviolet B wavelengths (UVB) to achieve healthy Vitamin D levels. Sunscreens with SPF 15 or greater are essential to prevent skin damage with longer sun exposure but will reduce Vitamin D synthesis by 99% Advising to omit sunscreen for short, incidental sun exposures would be reasonable. Deliberate exposure to sunlight between 11: 00 and 15: 00 in the summer months is not advised NB. For the six months between October and April 90% of the UK lies above the latitude that permits exposure to the UVB that is necessary for Vitamin D synthesis. During these months people are reliant on exogenous sources i. e. from diet or supplementation Diet 10 -15% of vitamin D is obtained through diet. The following foods are rich in vitamin D: oily fish – e. g. sardines, mackerel, salmon, liver, red meat, egg yolks, mushrooms, fortified infant milk formula, fortified margarine, fortified breakfast cereals Breast fed infants are at higher risk of Vitamin D deficiency as infant formula is fortified with vitamin D. The daily requirement of vitamin D is 280 -400 units/day in infancy and childhood. Return to assessment of need Return to start
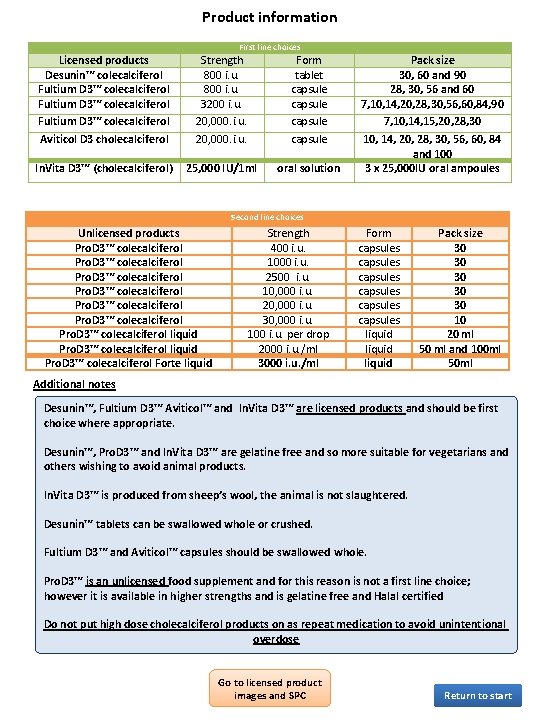
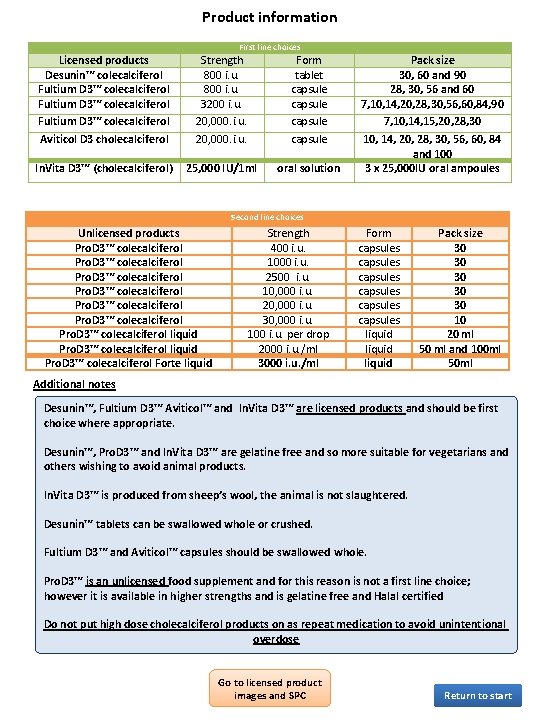
Product information First line choices Licensed products Desunin™ colecalciferol Fultium D 3™ colecalciferol Aviticol D 3 cholecalciferol Strength 800 i. u. 3200 i. u. 20, 000. i. u. Form tablet capsule In. Vita D 3™ (cholecalciferol) 25, 000 IU/1 ml oral solution Pack size 30, 60 and 90 28, 30, 56 and 60 7, 10, 14, 20, 28, 30, 56, 60, 84, 90 7, 10, 14, 15, 20, 28, 30 10, 14, 20, 28, 30, 56, 60, 84 and 100 3 x 25, 000 IU oral ampoules Second line choices Unlicensed products Pro. D 3™ colecalciferol Pro. D 3™ colecalciferol liquid Pro. D 3™ colecalciferol Forte liquid Strength 400 i. u. 1000 i. u. 2500 i. u. 10, 000 i. u. 20, 000 i. u. 30, 000 i. u. 100 i. u. per drop 2000 i. u. /ml 3000 i. u. /ml Form capsules capsules liquid Pack size 30 30 30 10 20 ml 50 ml and 100 ml 50 ml Additional notes Desunin™, Fultium D 3™ Aviticol™ and In. Vita D 3™ are licensed products and should be first choice where appropriate. Desunin™, Pro. D 3™ and In. Vita D 3™ are gelatine free and so more suitable for vegetarians and others wishing to avoid animal products. In. Vita D 3™ is produced from sheep’s wool, the animal is not slaughtered. Desunin™ tablets can be swallowed whole or crushed. Fultium D 3™ and Aviticol™ capsules should be swallowed whole. Pro. D 3™ is an unlicensed food supplement and for this reason is not a first line choice; however it is available in higher strengths and is gelatine free and Halal certified Do not put high dose cholecalciferol products on as repeat medication to avoid unintentional overdose Go to licensed product images and SPC Return to start

Licensed product images-click on links for SPC Fultium-D 3 800 iu Fultium-D 3 3200 iu Desunin 800 iu In. Vita. D 3 Aviticol 20, 000 iu Return to product information Return to start