MANAGEMENT OF UNCONSCIOUS PATIENT DR MANSOOR AHMAD KHAN
- Slides: 50
MANAGEMENT OF UNCONSCIOUS PATIENT DR MANSOOR AHMAD KHAN MB, MD, FASN (USA) ASSOCIATE PROFESSOR DEPT OF INTERNAL MEDICINE
INTRODUCTION • Unconscious patient makes everybody anxious • Requires structured way of approach • Should act Urgently / Appropriately / Accurately • Conscious> Drowsy> Unconscious> ? Death / Permanent Brain Damage
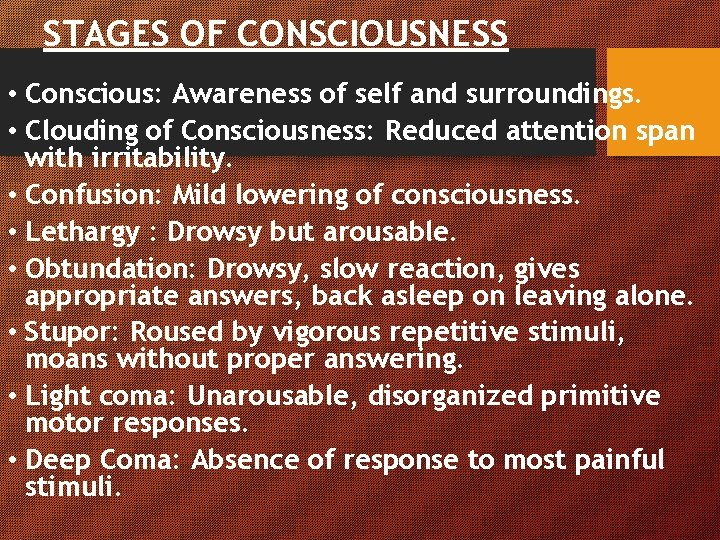
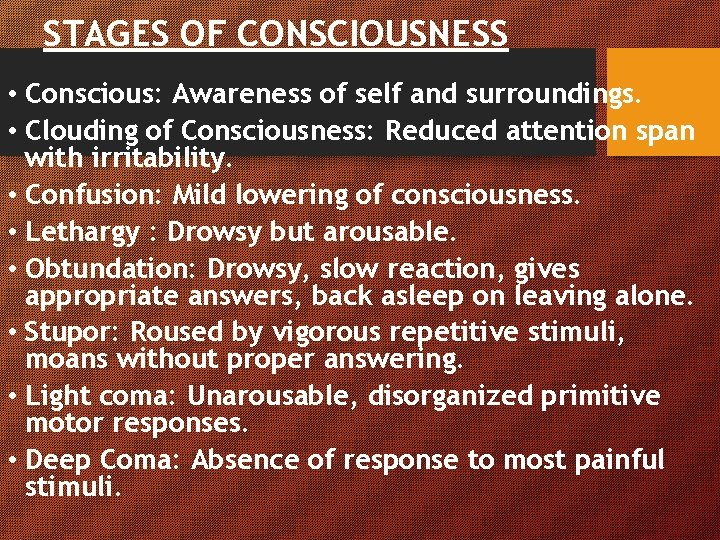
STAGES OF CONSCIOUSNESS • Conscious: Awareness of self and surroundings. • Clouding of Consciousness: Reduced attention span with irritability. • Confusion: Mild lowering of consciousness. • Lethargy : Drowsy but arousable. • Obtundation: Drowsy, slow reaction, gives appropriate answers, back asleep on leaving alone. • Stupor: Roused by vigorous repetitive stimuli, moans without proper answering. • Light coma: Unarousable, disorganized primitive motor responses. • Deep Coma: Absence of response to most painful stimuli.
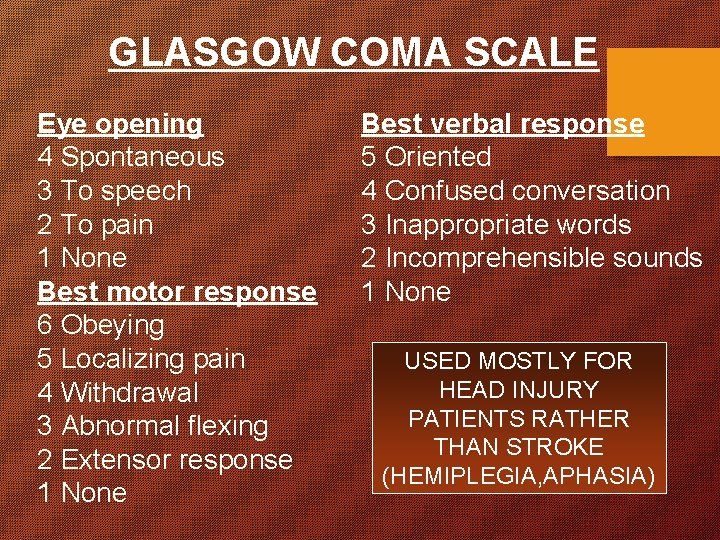
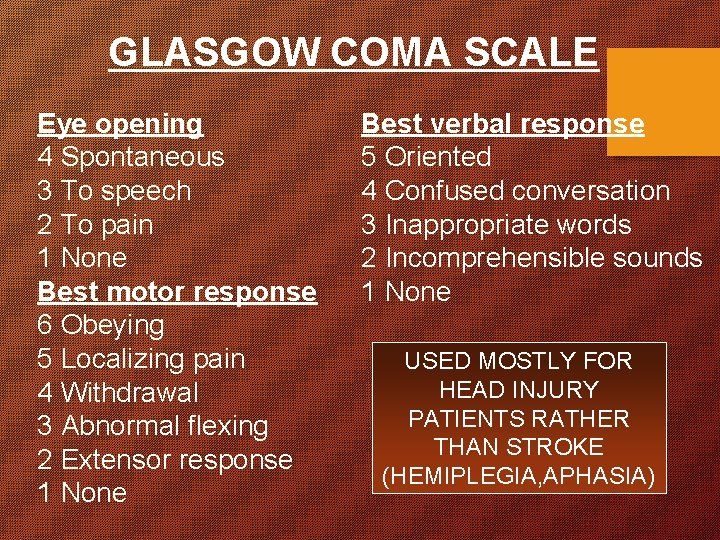
GLASGOW COMA SCALE Eye opening 4 Spontaneous 3 To speech 2 To pain 1 None Best motor response 6 Obeying 5 Localizing pain 4 Withdrawal 3 Abnormal flexing 2 Extensor response 1 None Best verbal response 5 Oriented 4 Confused conversation 3 Inappropriate words 2 Incomprehensible sounds 1 None USED MOSTLY FOR HEAD INJURY PATIENTS RATHER THAN STROKE (HEMIPLEGIA, APHASIA)
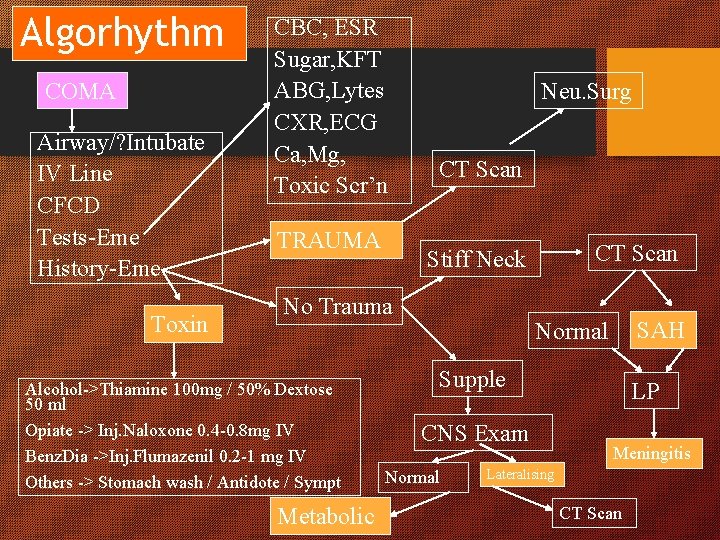
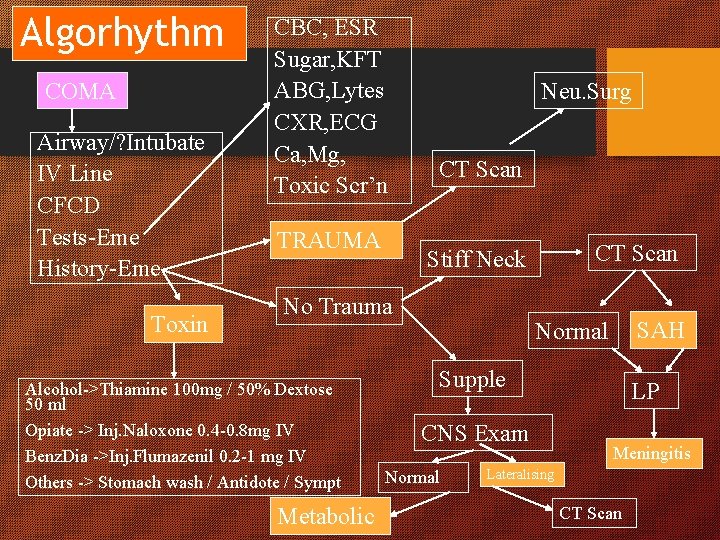
Algorhythm COMA Airway/? Intubate IV Line CFCD Tests-Eme History-Eme Toxin CBC, ESR Sugar, KFT ABG, Lytes CXR, ECG Ca, Mg, Toxic Scr’n TRAUMA Neu. Surg CT Scan No Trauma Alcohol->Thiamine 100 mg / 50% Dextose 50 ml Opiate -> Inj. Naloxone 0. 4 -0. 8 mg IV Benz. Dia ->Inj. Flumazenil 0. 2 -1 mg IV Others -> Stomach wash / Antidote / Sympt Metabolic CT Scan Stiff Neck SAH Normal Supple CNS Exam Normal LP Meningitis Lateralising CT Scan
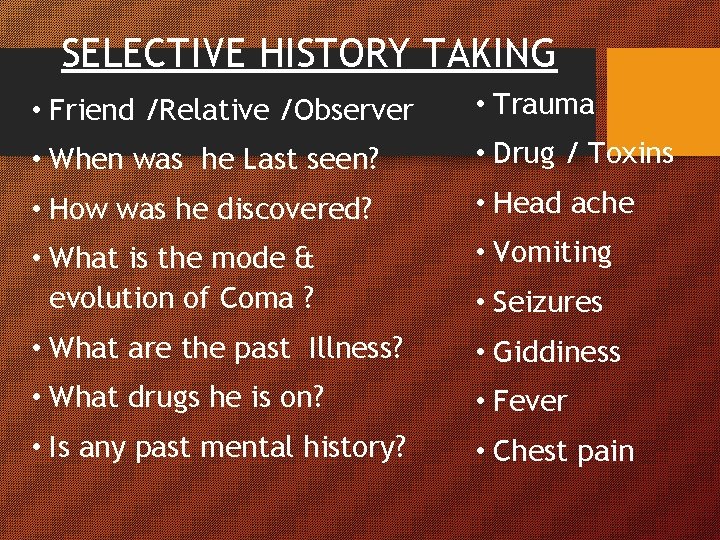
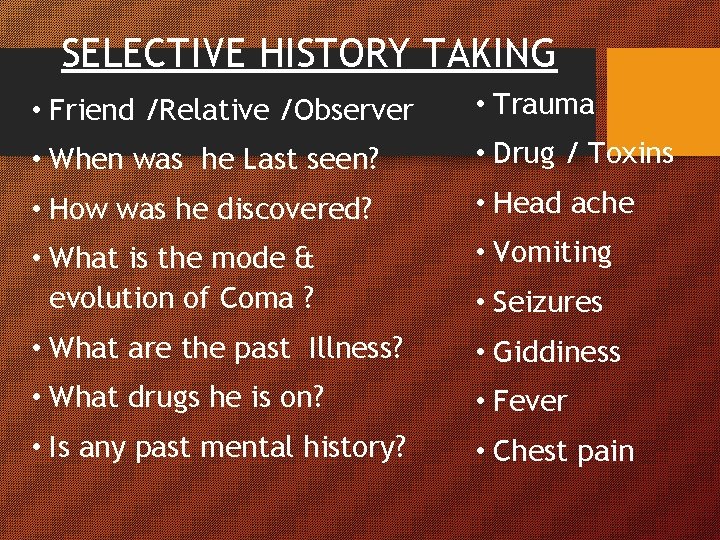
SELECTIVE HISTORY TAKING • Friend /Relative /Observer • Trauma • When was he Last seen? • Drug / Toxins • How was he discovered? • Head ache • What is the mode & evolution of Coma ? • Vomiting • What are the past Illness? • Giddiness • What drugs he is on? • Fever • Is any past mental history? • Chest pain • Seizures
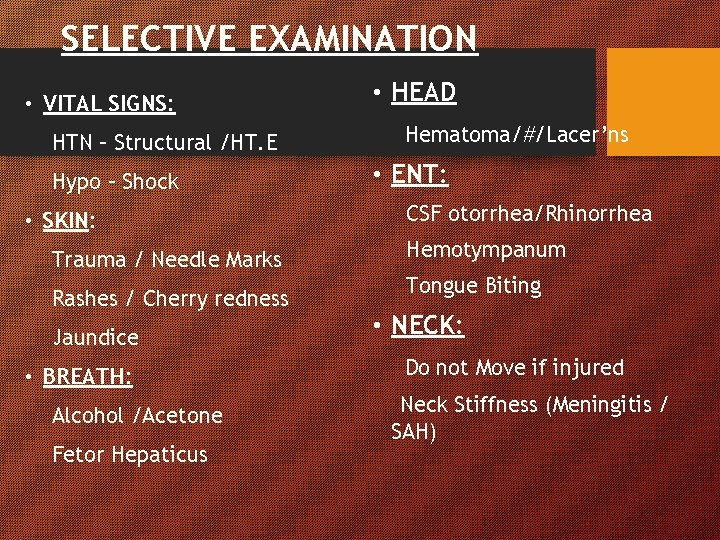
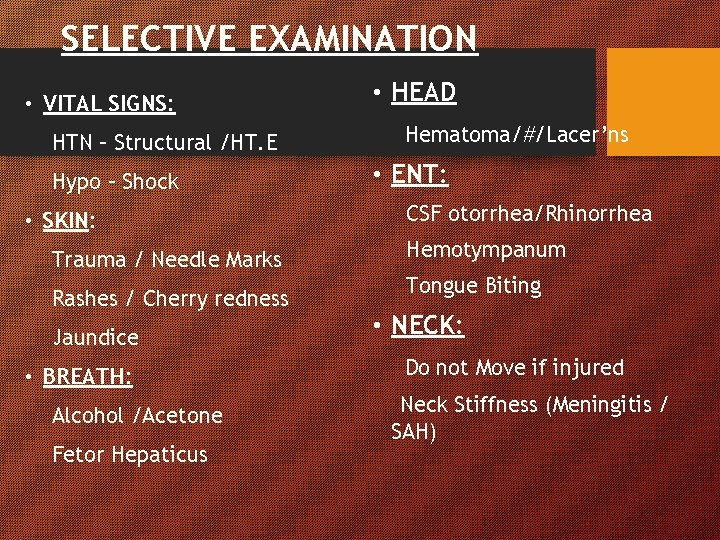
SELECTIVE EXAMINATION • VITAL SIGNS: HTN – Structural /HT. E Hypo – Shock • SKIN: Trauma / Needle Marks Rashes / Cherry redness Jaundice • BREATH: Alcohol /Acetone Fetor Hepaticus • HEAD Hematoma/#/Lacer’ns • ENT: CSF otorrhea/Rhinorrhea Hemotympanum Tongue Biting • NECK: Do not Move if injured Neck Stiffness (Meningitis / SAH)
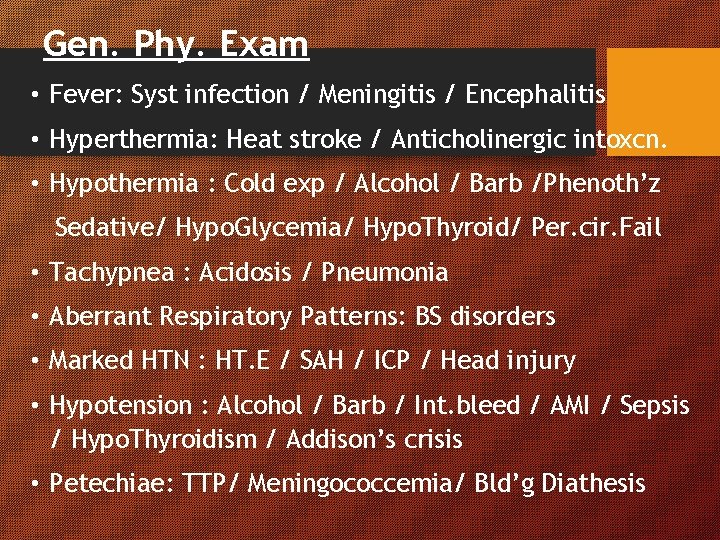
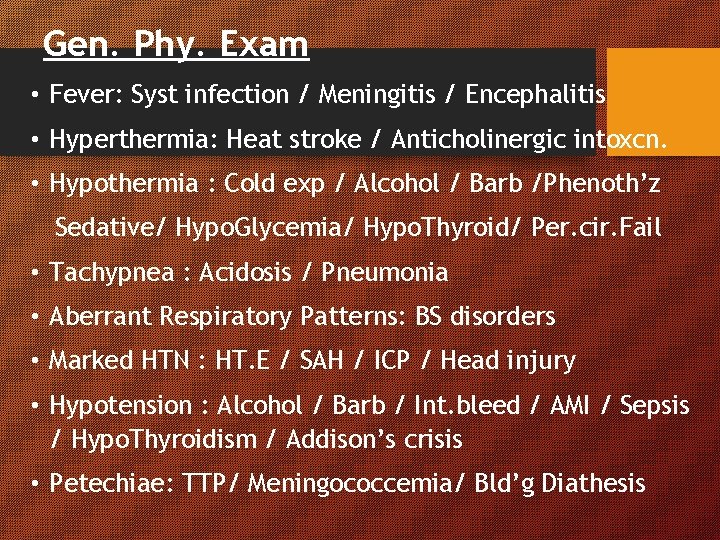
Gen. Phy. Exam • Fever: Syst infection / Meningitis / Encephalitis • Hyperthermia: Heat stroke / Anticholinergic intoxcn. • Hypothermia : Cold exp / Alcohol / Barb /Phenoth’z Sedative/ Hypo. Glycemia/ Hypo. Thyroid/ Per. cir. Fail • Tachypnea : Acidosis / Pneumonia • Aberrant Respiratory Patterns: BS disorders • Marked HTN : HT. E / SAH / ICP / Head injury • Hypotension : Alcohol / Barb / Int. bleed / AMI / Sepsis / Hypo. Thyroidism / Addison’s crisis • Petechiae: TTP/ Meningococcemia/ Bld’g Diathesis
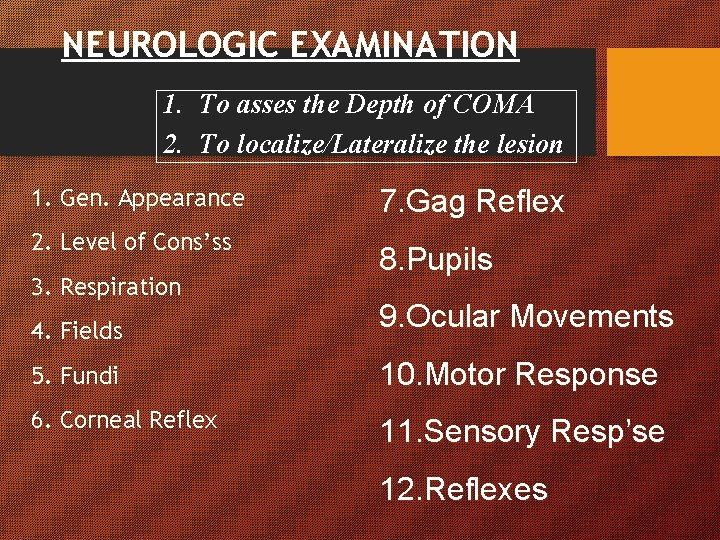
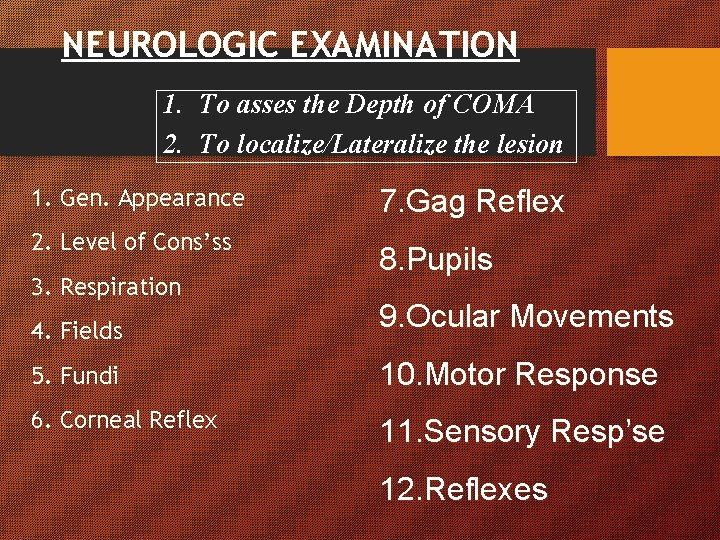
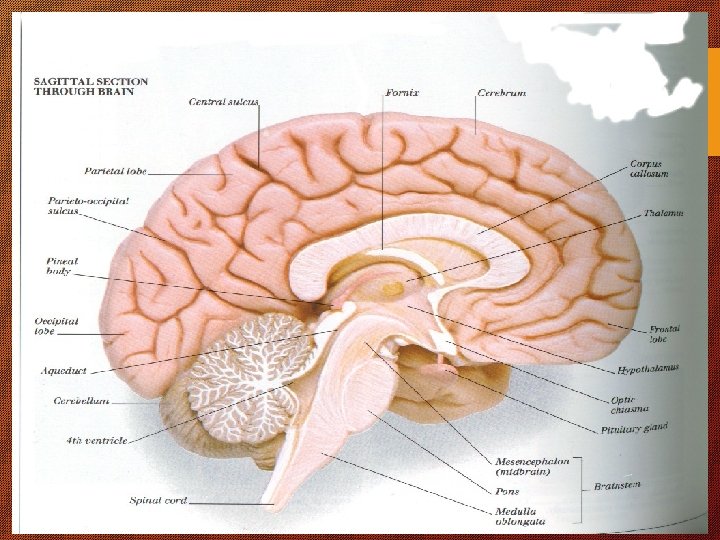
NEUROLOGIC EXAMINATION 1. To asses the Depth of COMA 2. To localize/Lateralize the lesion 1. Gen. Appearance 2. Level of Cons’ss 3. Respiration 7. Gag Reflex 8. Pupils 4. Fields 9. Ocular Movements 5. Fundi 10. Motor Response 6. Corneal Reflex 11. Sensory Resp’se 12. Reflexes
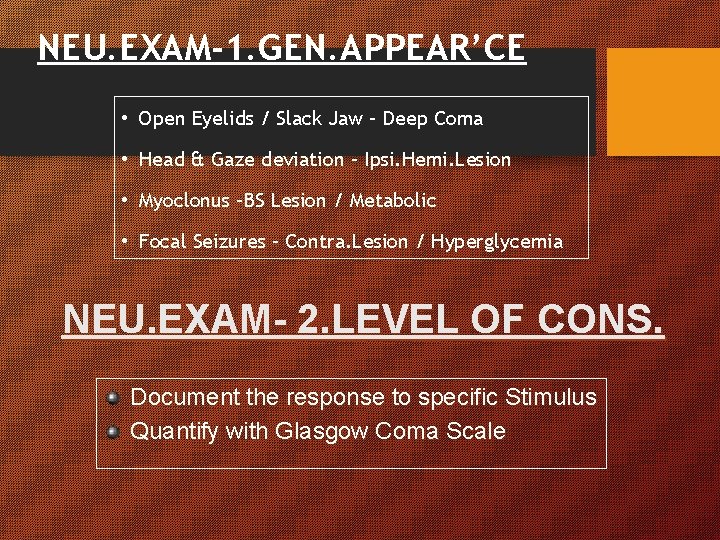
NEU. EXAM-1. GEN. APPEAR’CE • Open Eyelids / Slack Jaw – Deep Coma • Head & Gaze deviation – Ipsi. Hemi. Lesion • Myoclonus –BS Lesion / Metabolic • Focal Seizures – Contra. Lesion / Hyperglycemia NEU. EXAM- 2. LEVEL OF CONS. Document the response to specific Stimulus Quantify with Glasgow Coma Scale
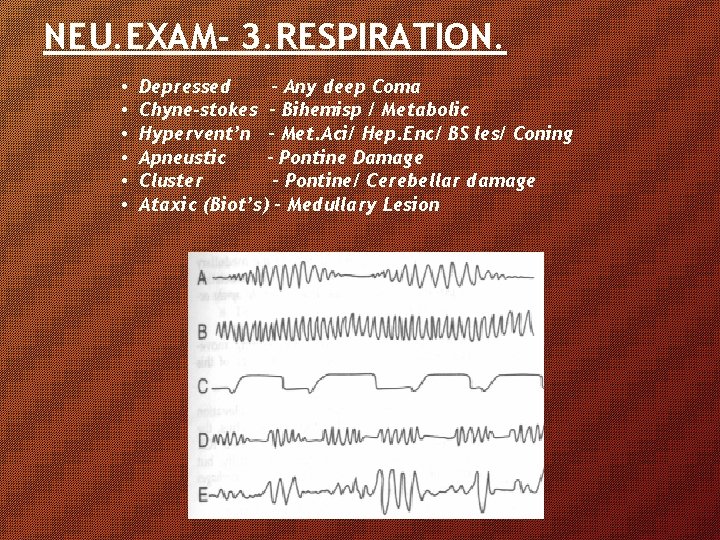
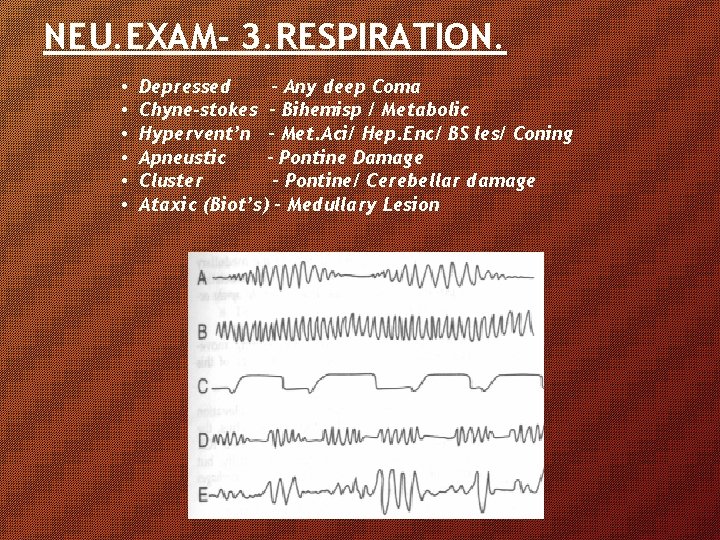
NEU. EXAM- 3. RESPIRATION. • • • Depressed – Any deep Coma Chyne-stokes – Bihemisp / Metabolic Hypervent’n – Met. Aci/ Hep. Enc/ BS les/ Coning Apneustic – Pontine Damage Cluster – Pontine/ Cerebellar damage Ataxic (Biot’s) – Medullary Lesion
NEUROLOGIC EXAMINATION 4. Fields – By Menace Reflex 5. Fundii –Papilledema - >12 hrs of ↑ ICT Subhyloid H’ge – Asst’d č SAH 6. Corneal Reflex – Aff: Cr. V / Eff: Cr. VII 7. Gag Reflex – Absent in BS Les / Deep coma 11. Sensory Response – Lateralizing Sensory Loss 12. Deep T. Reflex – Helps in Lateralizing 13. Plantar Reflex -- Helps in Lateralizing -- ↑ ↑ Structural / Metabolic
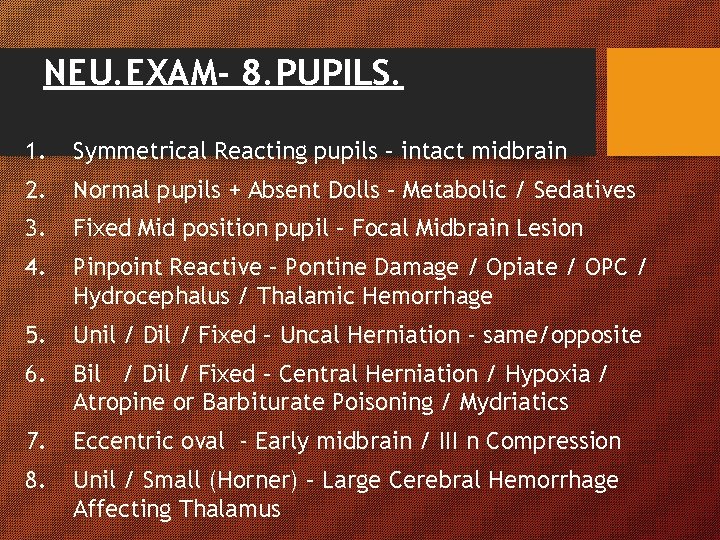
NEU. EXAM- 8. PUPILS. 1. Symmetrical Reacting pupils – intact midbrain 2. Normal pupils + Absent Dolls – Metabolic / Sedatives 3. Fixed Mid position pupil – Focal Midbrain Lesion 4. Pinpoint Reactive – Pontine Damage / Opiate / OPC / Hydrocephalus / Thalamic Hemorrhage 5. Unil / Dil / Fixed – Uncal Herniation - same/opposite 6. Bil / Dil / Fixed – Central Herniation / Hypoxia / Atropine or Barbiturate Poisoning / Mydriatics 7. Eccentric oval - Early midbrain / III n Compression 8. Unil / Small (Horner) – Large Cerebral Hemorrhage Affecting Thalamus
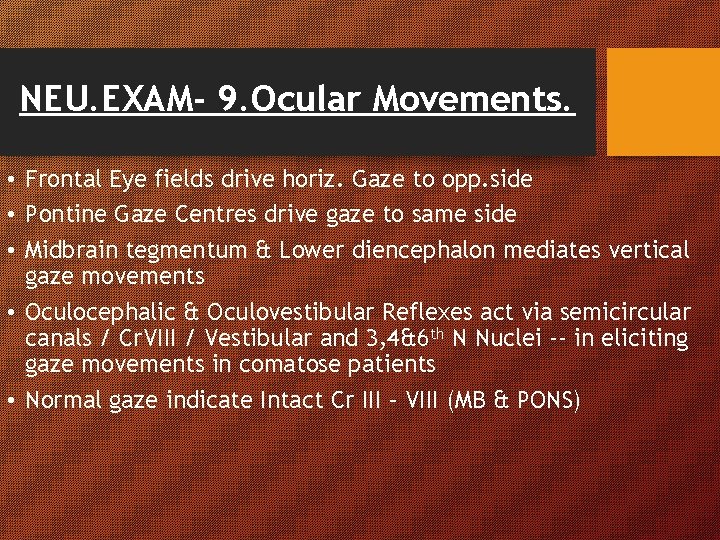
NEU. EXAM- 9. Ocular Movements. • Frontal Eye fields drive horiz. Gaze to opp. side • Pontine Gaze Centres drive gaze to same side • Midbrain tegmentum & Lower diencephalon mediates vertical gaze movements • Oculocephalic & Oculovestibular Reflexes act via semicircular canals / Cr. VIII / Vestibular and 3, 4&6 th N Nuclei -- in eliciting gaze movements in comatose patients • Normal gaze indicate Intact Cr III – VIII (MB & PONS)
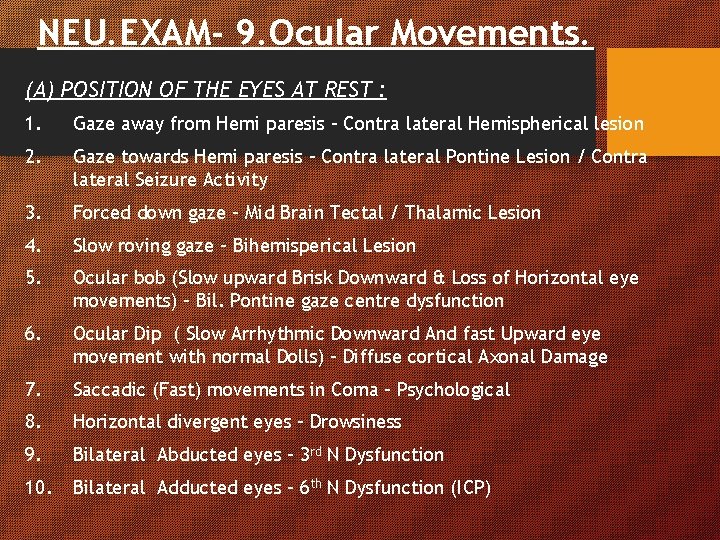
NEU. EXAM- 9. Ocular Movements. (A) POSITION OF THE EYES AT REST : 1. Gaze away from Hemi paresis – Contra lateral Hemispherical lesion 2. Gaze towards Hemi paresis – Contra lateral Pontine Lesion / Contra lateral Seizure Activity 3. Forced down gaze – Mid Brain Tectal / Thalamic Lesion 4. Slow roving gaze – Bihemisperical Lesion 5. Ocular bob (Slow upward Brisk Downward & Loss of Horizontal eye movements) – Bil. Pontine gaze centre dysfunction 6. Ocular Dip ( Slow Arrhythmic Downward And fast Upward eye movement with normal Dolls) – Diffuse cortical Axonal Damage 7. Saccadic (Fast) movements in Coma – Psychological 8. Horizontal divergent eyes – Drowsiness 9. Bilateral Abducted eyes – 3 rd N Dysfunction 10. Bilateral Adducted eyes – 6 th N Dysfunction (ICP)
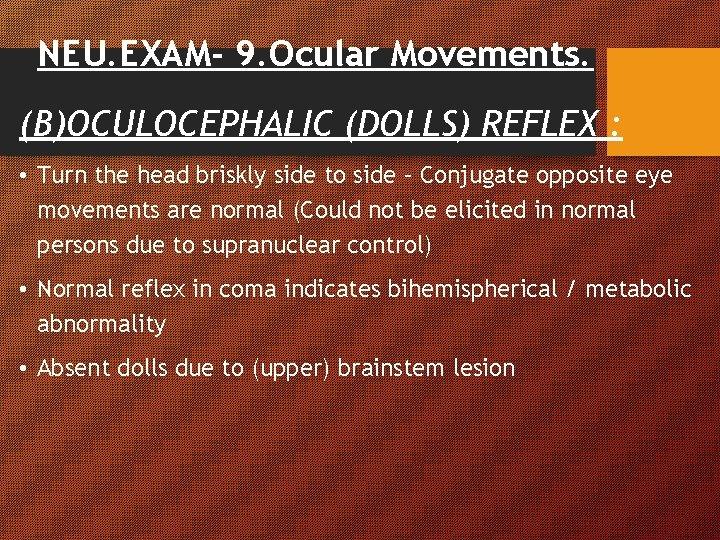
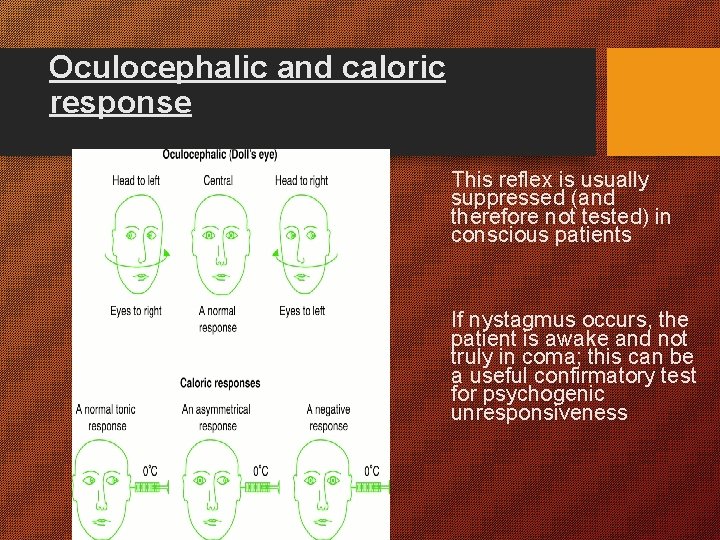
NEU. EXAM- 9. Ocular Movements. (B)OCULOCEPHALIC (DOLLS) REFLEX : • Turn the head briskly side to side – Conjugate opposite eye movements are normal (Could not be elicited in normal persons due to supranuclear control) • Normal reflex in coma indicates bihemispherical / metabolic abnormality • Absent dolls due to (upper) brainstem lesion
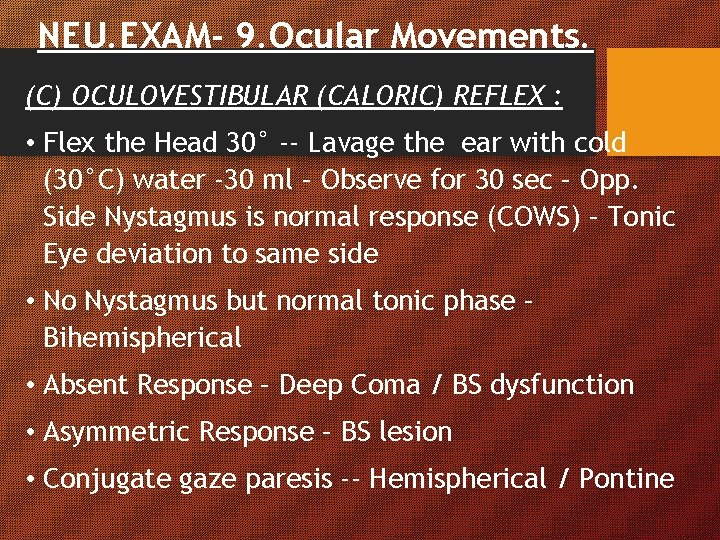
NEU. EXAM- 9. Ocular Movements. (C) OCULOVESTIBULAR (CALORIC) REFLEX : • Flex the Head 30° -- Lavage the ear with cold (30°C) water -30 ml – Observe for 30 sec – Opp. Side Nystagmus is normal response (COWS) – Tonic Eye deviation to same side • No Nystagmus but normal tonic phase – Bihemispherical • Absent Response – Deep Coma / BS dysfunction • Asymmetric Response – BS lesion • Conjugate gaze paresis -- Hemispherical / Pontine
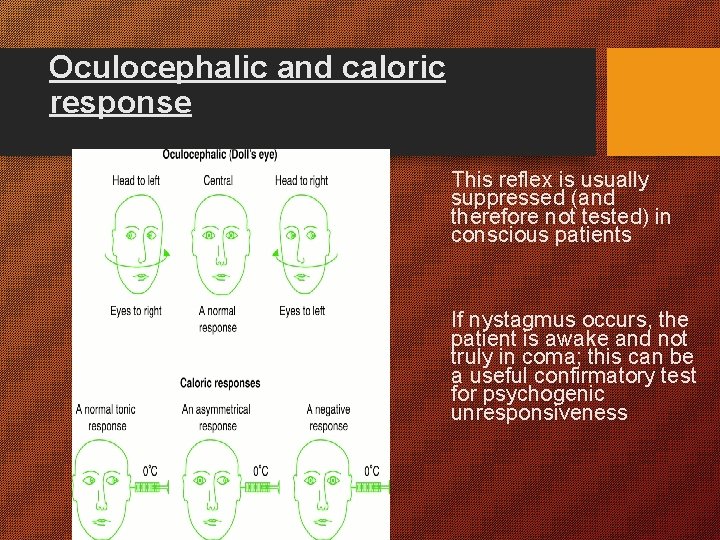
Oculocephalic and caloric response This reflex is usually suppressed (and therefore not tested) in conscious patients If nystagmus occurs, the patient is awake and not truly in coma; this can be a useful confirmatory test for psychogenic unresponsiveness
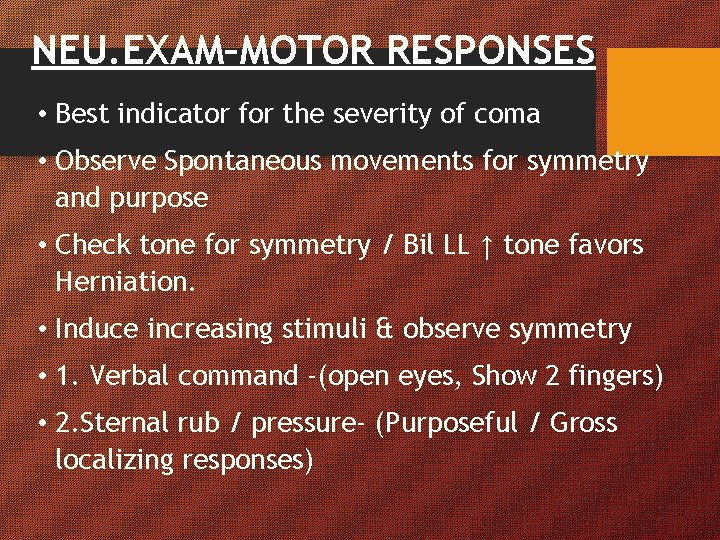
NEU. EXAM–MOTOR RESPONSES • Best indicator for the severity of coma • Observe Spontaneous movements for symmetry and purpose • Check tone for symmetry / Bil LL ↑ tone favors Herniation. • Induce increasing stimuli & observe symmetry • 1. Verbal command -(open eyes, Show 2 fingers) • 2. Sternal rub / pressure- (Purposeful / Gross localizing responses)
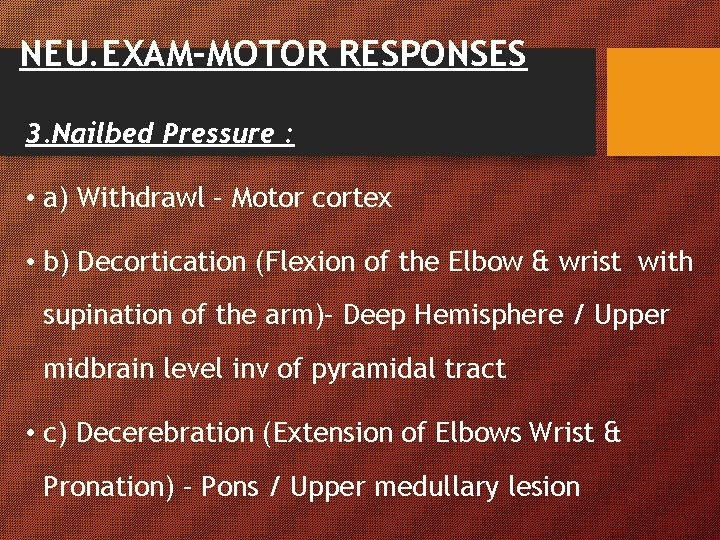
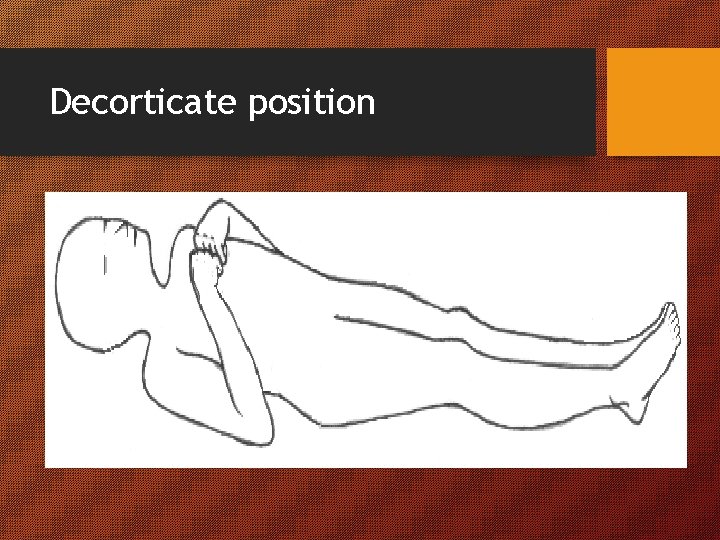
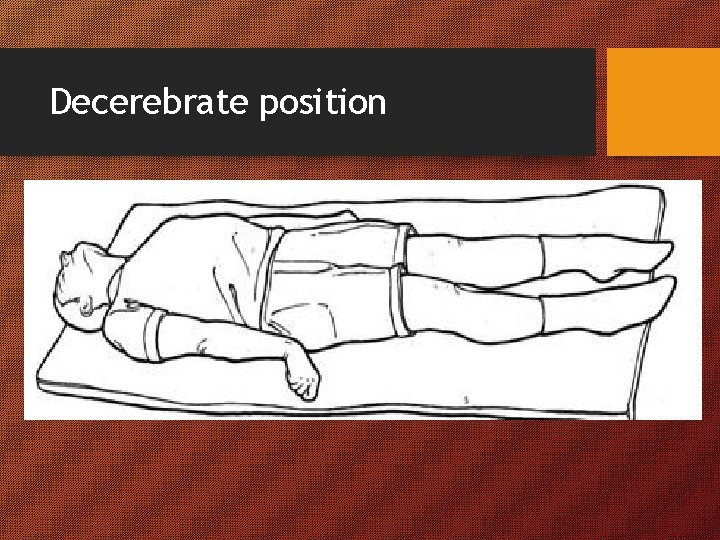
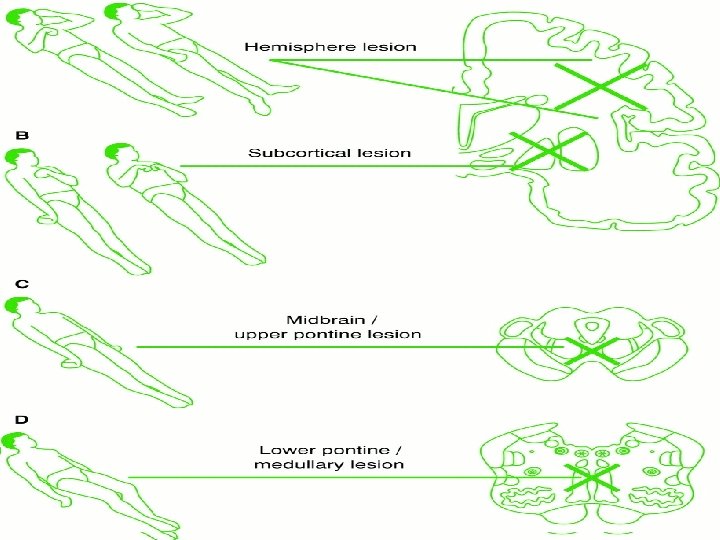
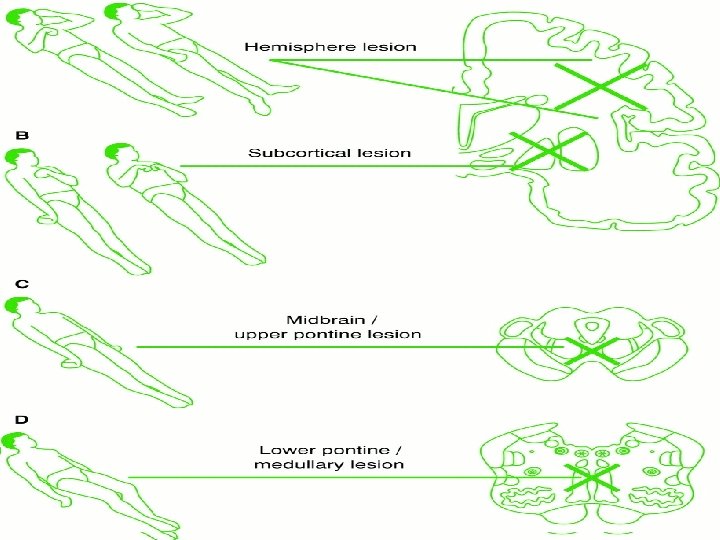
NEU. EXAM–MOTOR RESPONSES 3. Nailbed Pressure : • a) Withdrawl – Motor cortex • b) Decortication (Flexion of the Elbow & wrist with supination of the arm)– Deep Hemisphere / Upper midbrain level inv of pyramidal tract • c) Decerebration (Extension of Elbows Wrist & Pronation) – Pons / Upper medullary lesion
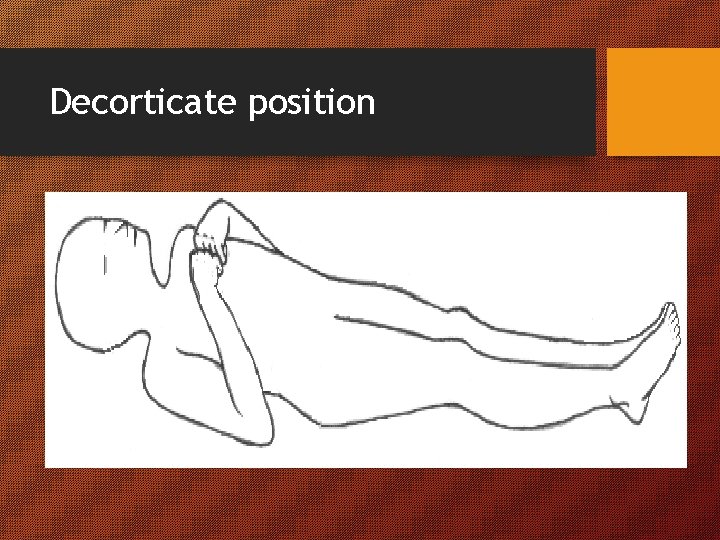
Decorticate position
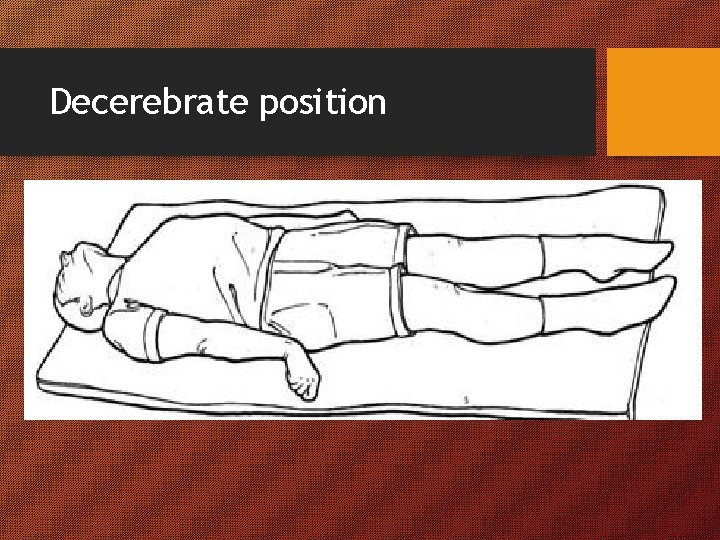
Decerebrate position
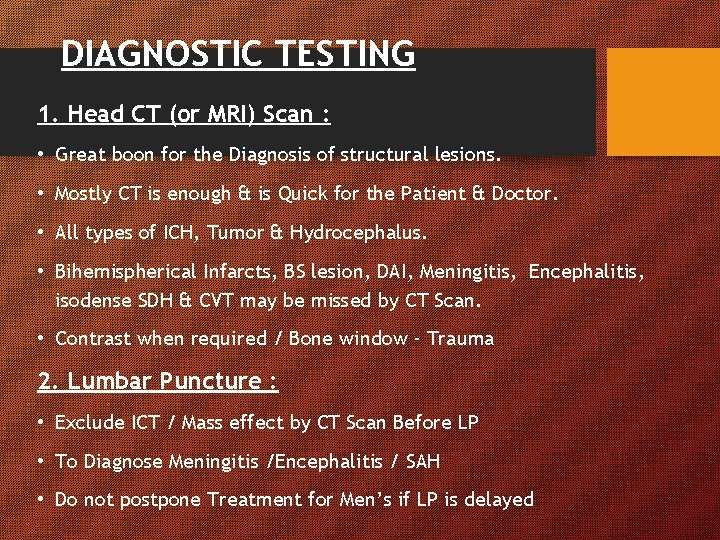
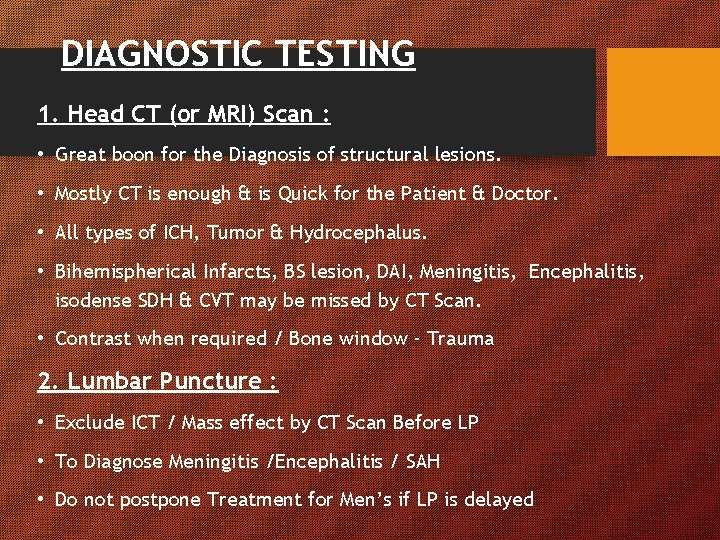
DIAGNOSTIC TESTING 1. Head CT (or MRI) Scan : • Great boon for the Diagnosis of structural lesions. • Mostly CT is enough & is Quick for the Patient & Doctor. • All types of ICH, Tumor & Hydrocephalus. • Bihemispherical Infarcts, BS lesion, DAI, Meningitis, Encephalitis, isodense SDH & CVT may be missed by CT Scan. • Contrast when required / Bone window - Trauma 2. Lumbar Puncture : • Exclude ICT / Mass effect by CT Scan Before LP • To Diagnose Meningitis /Encephalitis / SAH • Do not postpone Treatment for Men’s if LP is delayed
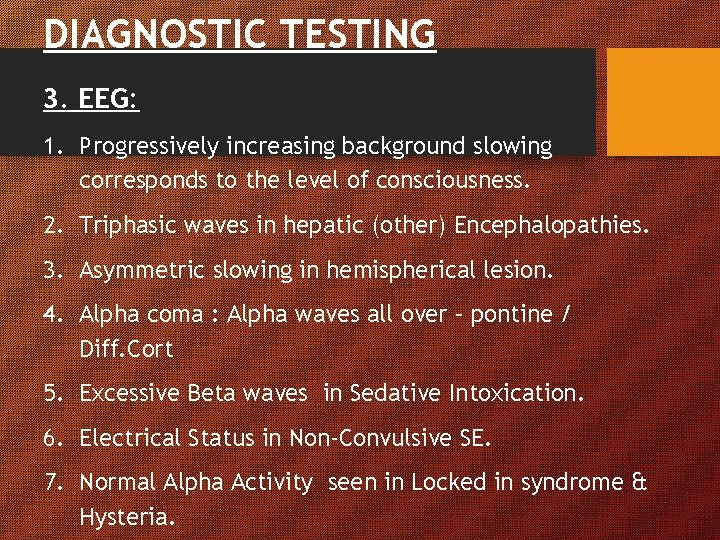
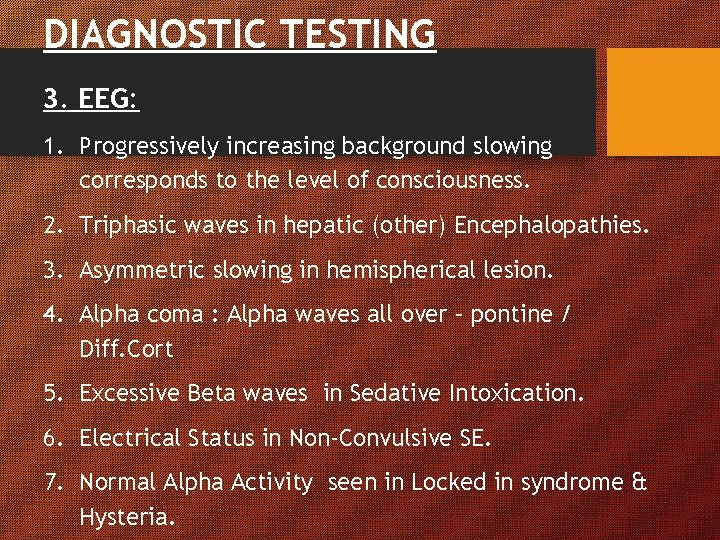
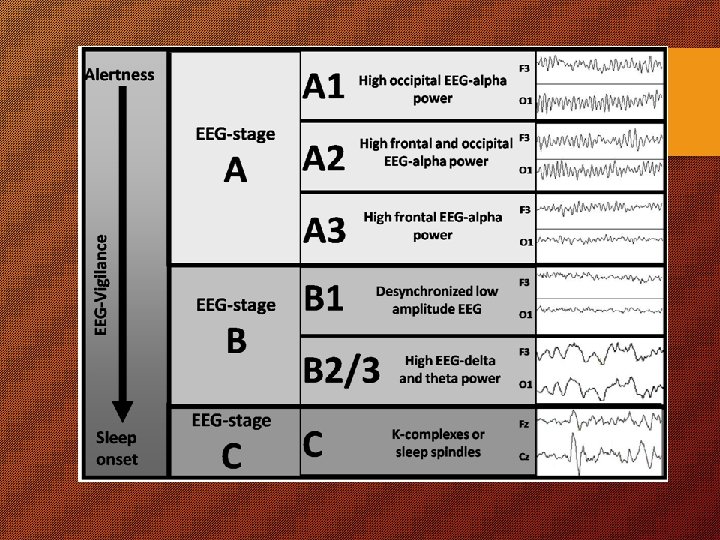
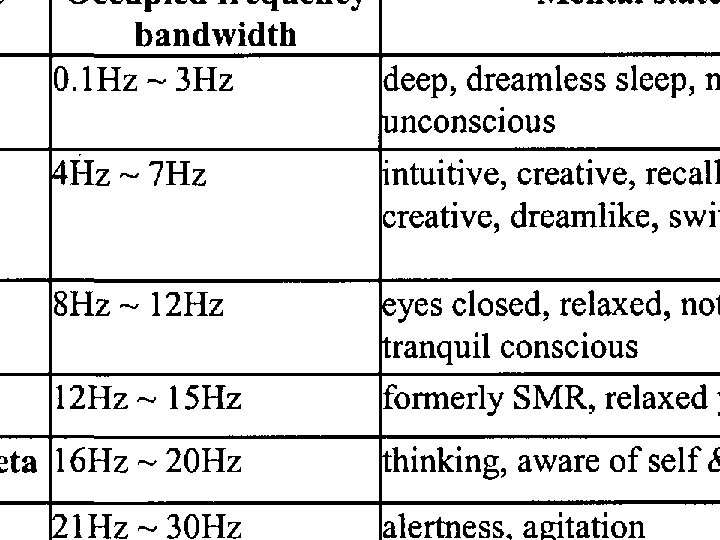
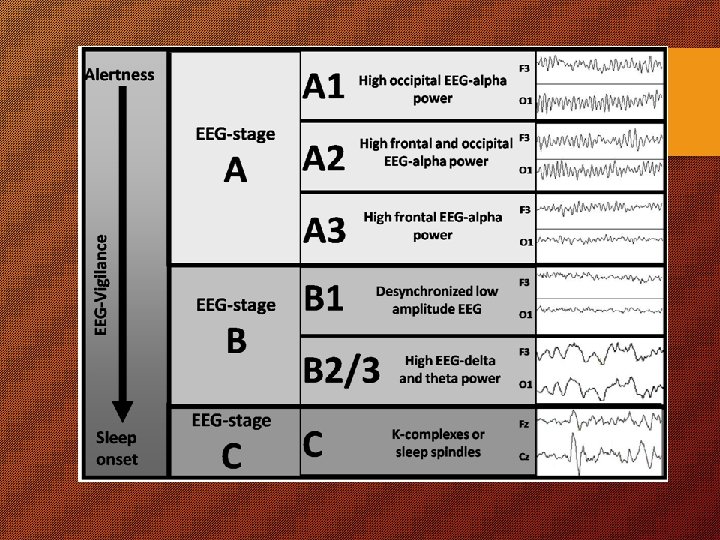
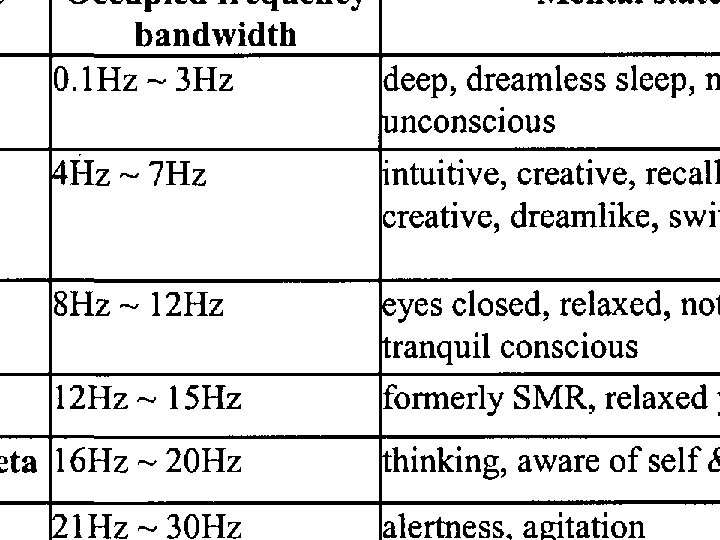
DIAGNOSTIC TESTING 3. EEG: 1. Progressively increasing background slowing corresponds to the level of consciousness. 2. Triphasic waves in hepatic (other) Encephalopathies. 3. Asymmetric slowing in hemispherical lesion. 4. Alpha coma : Alpha waves all over – pontine / Diff. Cort 5. Excessive Beta waves in Sedative Intoxication. 6. Electrical Status in Non-Convulsive SE. 7. Normal Alpha Activity seen in Locked in syndrome & Hysteria.
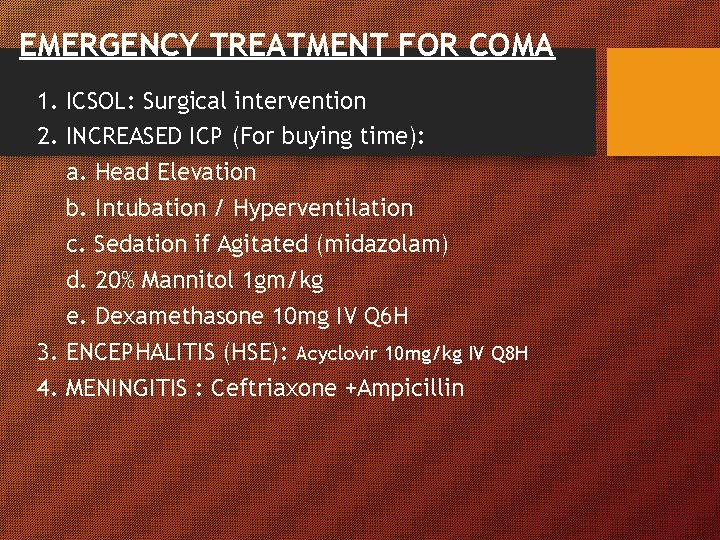
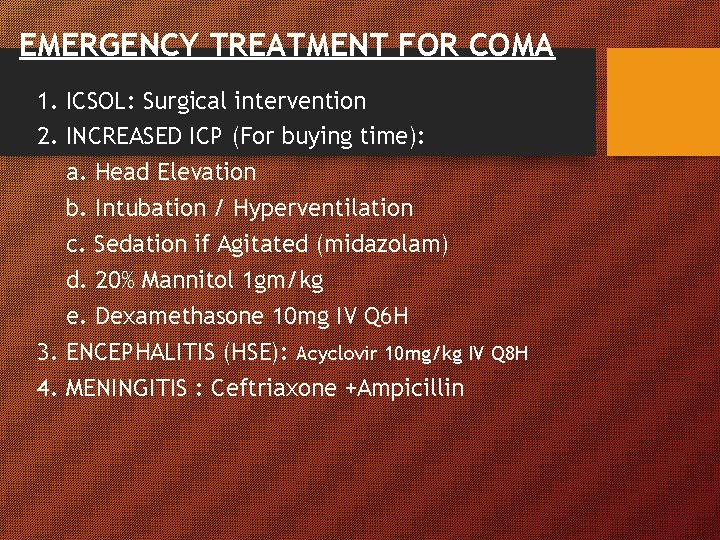
EMERGENCY TREATMENT FOR COMA 1. ICSOL: Surgical intervention 2. INCREASED ICP (For buying time): a. Head Elevation b. Intubation / Hyperventilation c. Sedation if Agitated (midazolam) d. 20% Mannitol 1 gm/kg e. Dexamethasone 10 mg IV Q 6 H 3. ENCEPHALITIS (HSE): Acyclovir 10 mg/kg IV Q 8 H 4. MENINGITIS : Ceftriaxone +Ampicillin
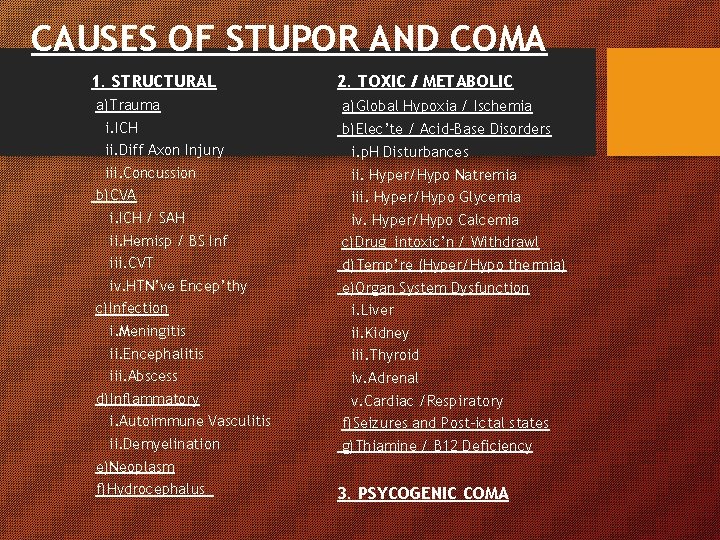
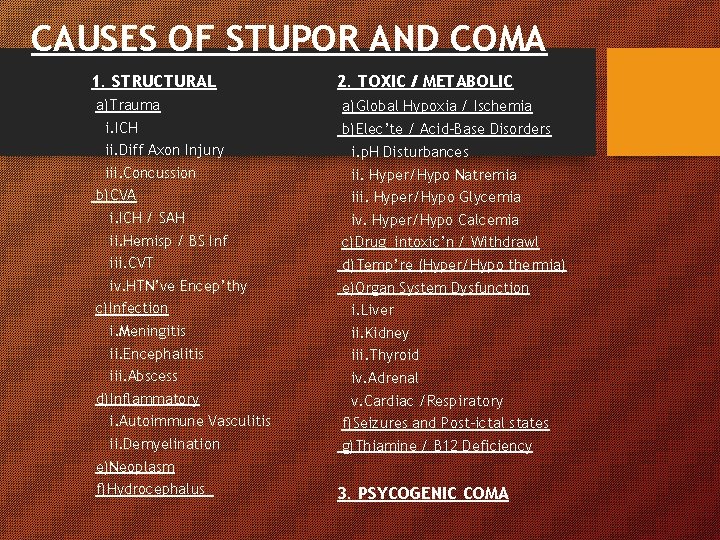
CAUSES OF STUPOR AND COMA 1. STRUCTURAL a)Trauma i. ICH 2. TOXIC / METABOLIC a)Global Hypoxia / Ischemia b)Elec’te / Acid-Base Disorders ii. Diff Axon Injury i. p. H Disturbances iii. Concussion ii. Hyper/Hypo Natremia b)CVA i. ICH / SAH iii. Hyper/Hypo Glycemia iv. Hyper/Hypo Calcemia ii. Hemisp / BS Inf c)Drug intoxic’n / Withdrawl iii. CVT d)Temp’re (Hyper/Hypo thermia) iv. HTN’ve Encep’thy e)Organ System Dysfunction c)Infection i. Liver i. Meningitis ii. Kidney ii. Encephalitis iii. Thyroid iii. Abscess iv. Adrenal d)Inflammatory v. Cardiac /Respiratory i. Autoimmune Vasculitis f)Seizures and Post-ictal states ii. Demyelination g)Thiamine / B 12 Deficiency e)Neoplasm f)Hydrocephalus 3. PSYCOGENIC COMA
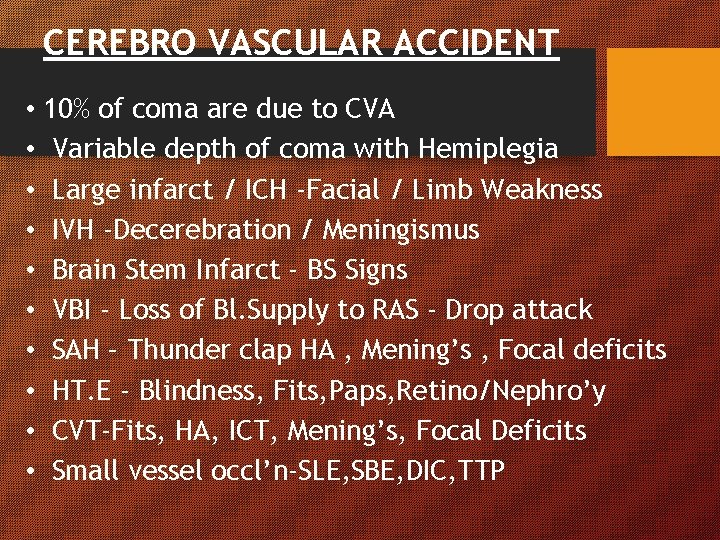
CEREBRO VASCULAR ACCIDENT • 10% of coma are due to CVA • Variable depth of coma with Hemiplegia • Large infarct / ICH -Facial / Limb Weakness • IVH -Decerebration / Meningismus • Brain Stem Infarct - BS Signs • VBI - Loss of Bl. Supply to RAS - Drop attack • SAH – Thunder clap HA , Mening’s , Focal deficits • HT. E - Blindness, Fits, Paps, Retino/Nephro’y • CVT-Fits, HA, ICT, Mening’s, Focal Deficits • Small vessel occl’n-SLE, SBE, DIC, TTP
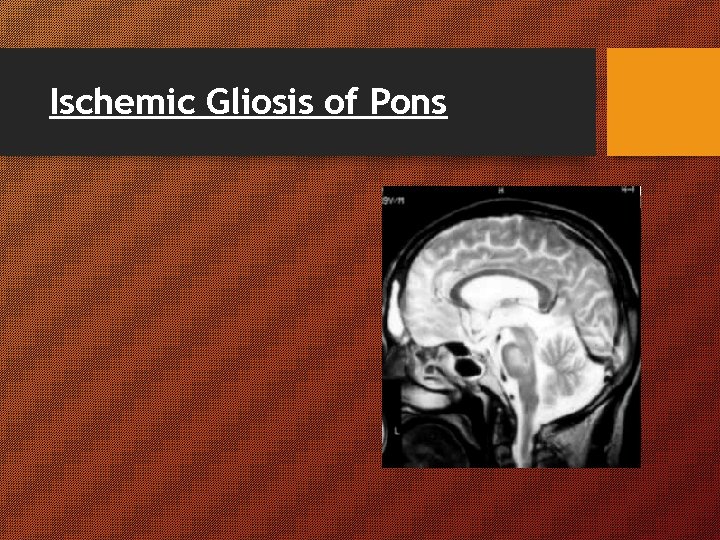
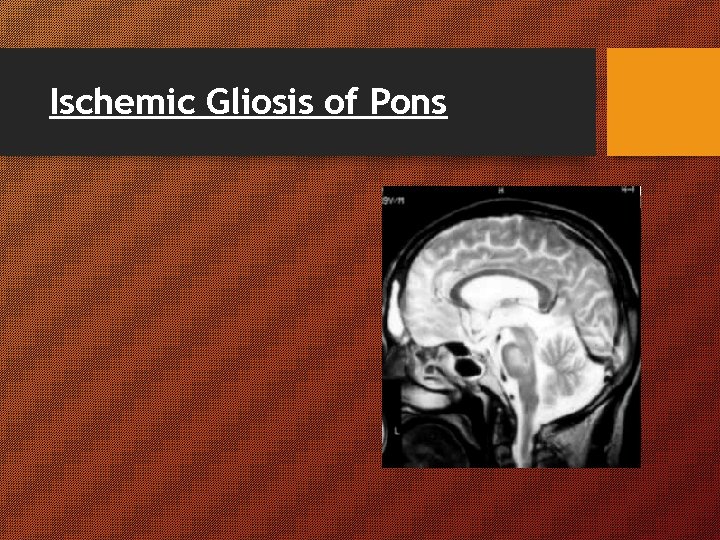
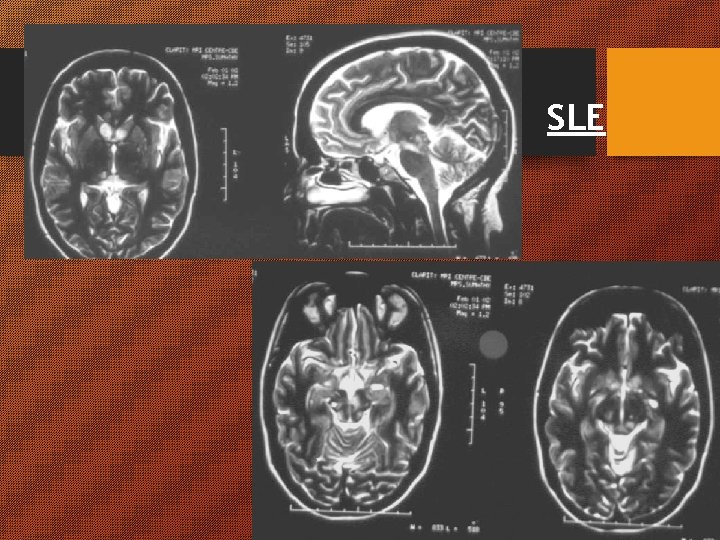
Ischemic Gliosis of Pons
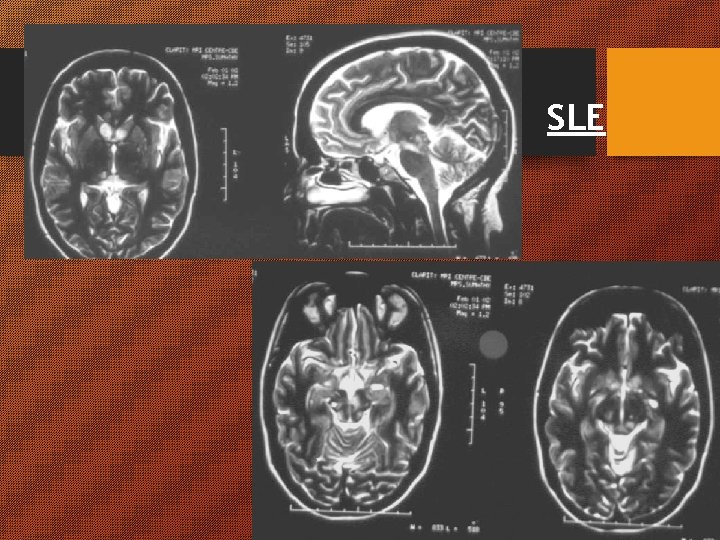
SLE
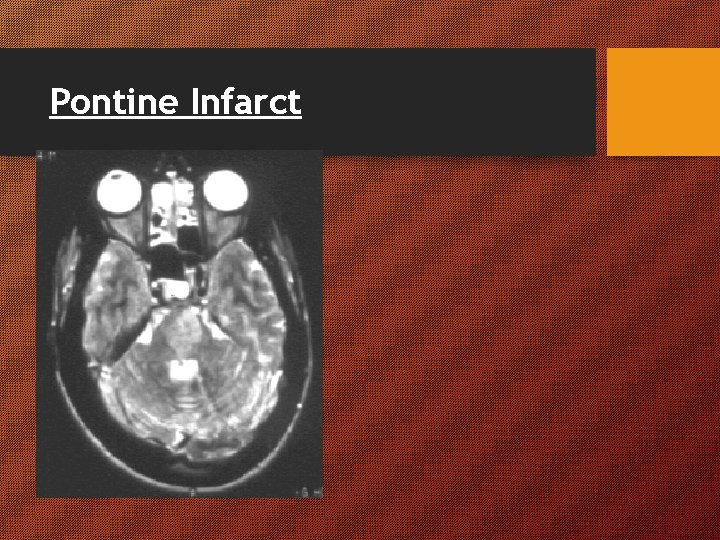
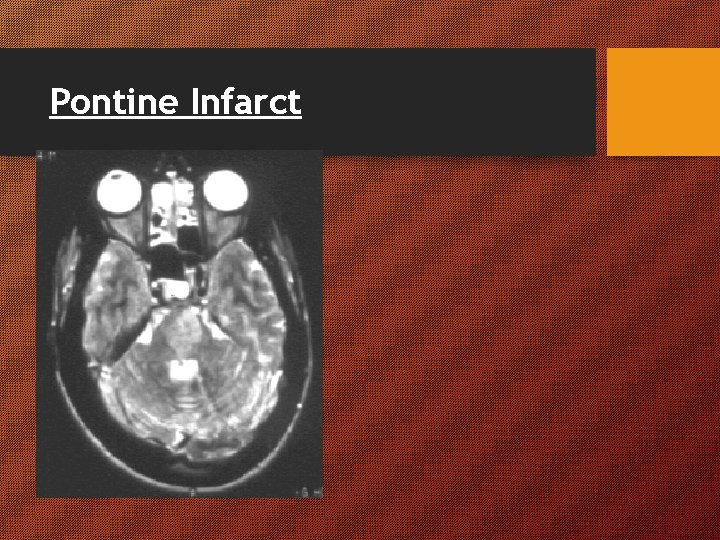
Pontine Infarct
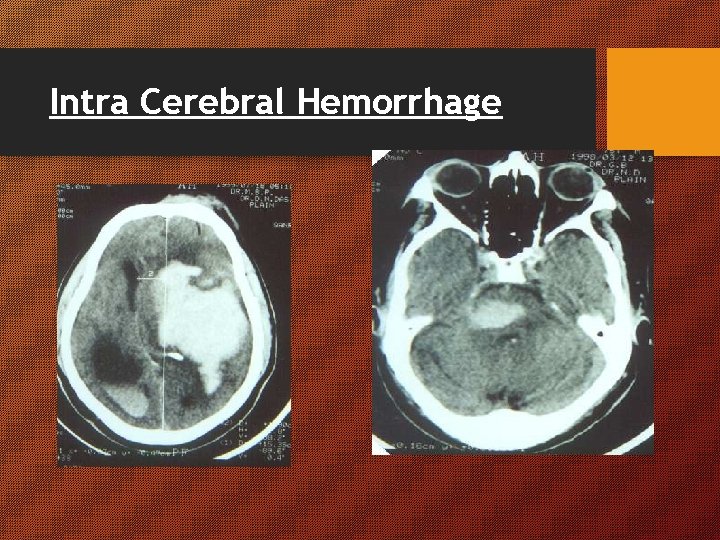
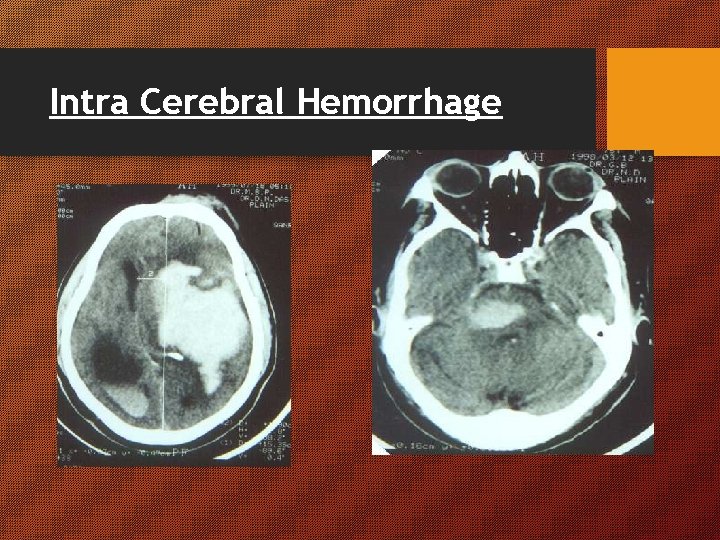
Intra Cerebral Hemorrhage
ANEURYSM & SAH • 10 / 1, 000 PER YEAR • Frequently in females • Age, HTN, Smoking, Alcohol –risk • 70% gets Warning leaks • 45% Manifest as COMA at the onset • Suspicion, CT & LP are Diagnostic methods • MRA, CT Angio & DSA for confirmation • Close monitor’g, rest, sedate, Vol. expaners, AED, Avoid Vasospasm, Anti HTN, & Dulcolax • Plan Surgery at the earliest
Aneurysms
TRAUMA • • 13% of coma are due to trauma History & Evidences of external Injury Concussion – Immediate / Late Coma Contusion / Laceration – Foc. def / Seiz’s EDH extra dural (MMA H’ge) - Lucid Interval SDH – Delayed Symptoms Monitor T, P, BP, ICP, CT, MRI, C. Spine for all Trauma.
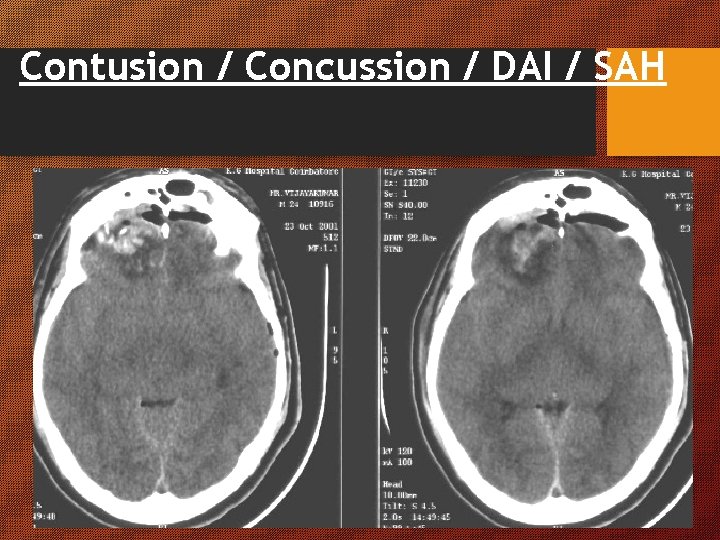
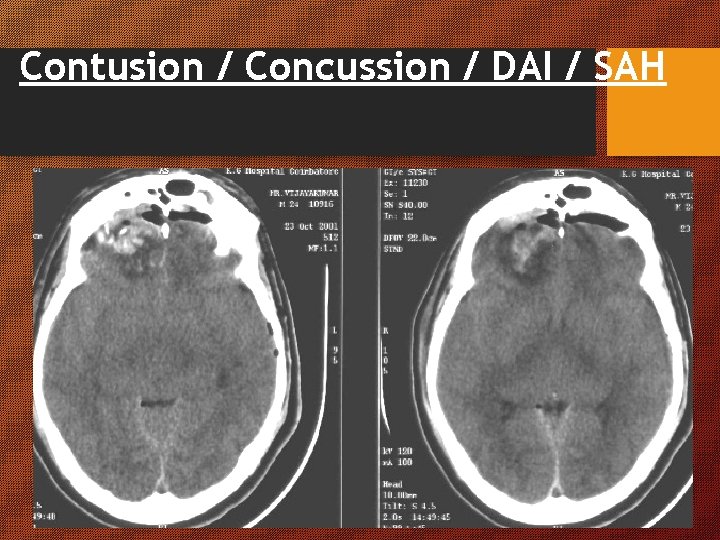
Contusion / Concussion / DAI / SAH
ALCOHOL INTOXICATION • Common Cause of Coma • Flushed face, Conj. inj. , Bounding pulse, Dil’d pp, • Alcohol from Breath, Stomach & Blood • ICH, Trauma, SDH, Wernicke’s Encp’thy • Urgent CT, LFT, Coag’ln profile • Inj. B 1 & 50% Dextrose if hypoglycemic • AED (anti epileptic drugs) if H/O seizures
Post ictal state • Tongue bite, Froath, Bloody sputum, Injury • Etiology of convulsion may be different • Confusion & Irritability • Brief stupor and profound sleep • To rule out Non-Convulsive Status DIABETES Hypo is worse so give IV dextrose Decrease DTR, T, BP, Hyd’n, / Inc P, R Smell of Acetone
Poisoning • • • Suicidal/ Homicidal/ Accidental Drugs and Toxins History / Physical findings Lavage/ Symptomatic/ Antidote/ Tt Compl No Lateralizing signs Depth of coma Acc to Strength & Amount Meningitis HA, Fever, LOC, Meningismus (not in age extremes & Imm. supp), ICP ENT infection, SBE, Rash in mening. meng’s Do CT before LP
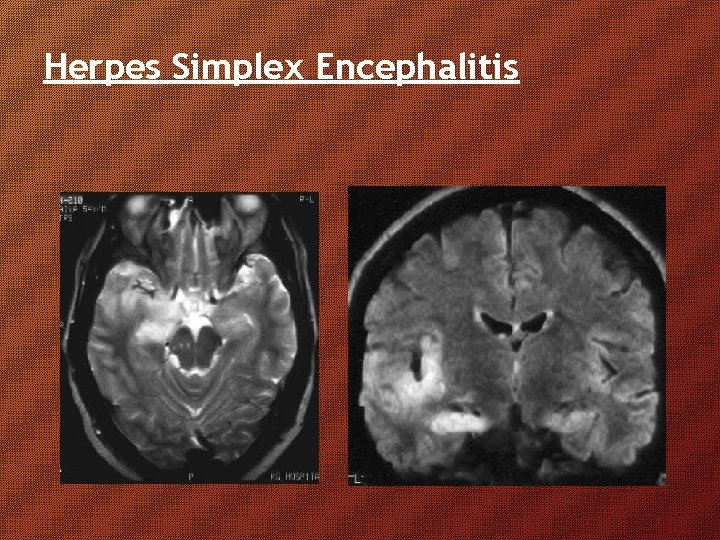
ENCEPHALITIS • Present with Fever, Meningismus, Altered sensorium, seizures and focal Deficits. • Usually the Seizures are difficult to control • EEG& CSF are better diagnostic tools than Imaging • HSE affects FT regions asymmetrically present with focal seizures • EEG may show PLEDs(periodic lateralized epileptiform discharge) Focal epileptic activity or slowing • MRI shows signal alterations in inferior FT regions asymmetrically • IV Acyclovir is the Treatment of choice with full dose AED
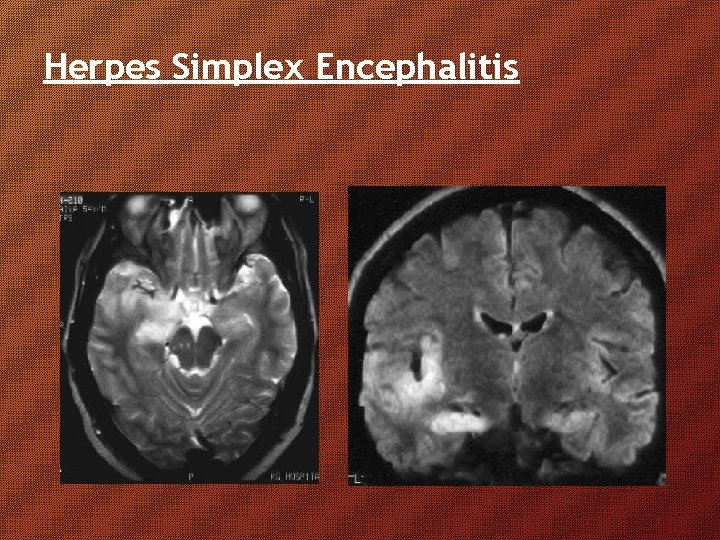
Herpes Simplex Encephalitis
PSEUDOCOMA 1. PSYCHOGENIC COMA • Negativistic Behavior (Resists opening eye) • Avoidance Behavior (Hand avoids face on dropping) • Intact Saccades / Normal Caloric response • Recovery on very painful stimuli 2. LOCKED IN SYNDROME • Complete paralysis except for vertical eye movements • Pt usually alert and can communicate thru’ EOM • Due to bilateral Pontine Damage (Infarct) 3. AKINETIC MUTISM (Motionless, Mindless Wakefulness) • Extreme psychomotor retardation- Appears awake • Show Delayed Limited responses • Due to Extensive Thalamic / Frontal Damage
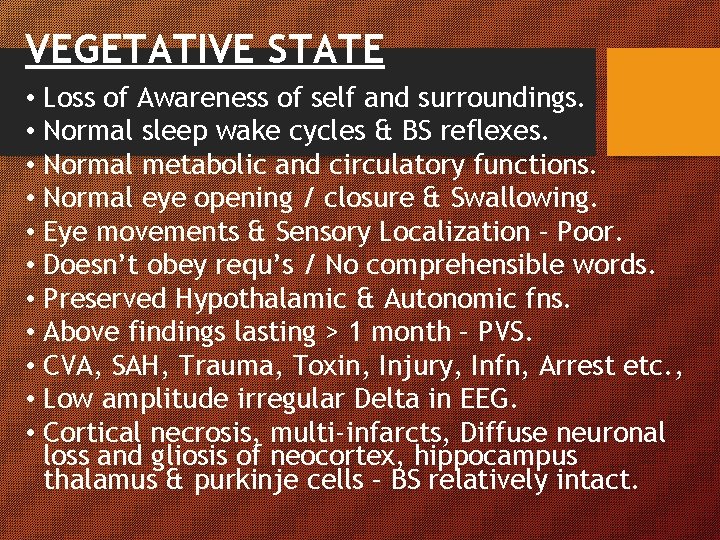
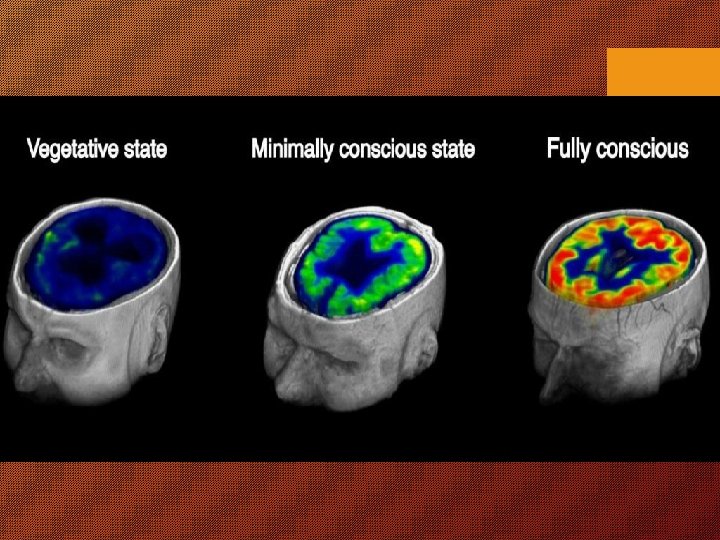
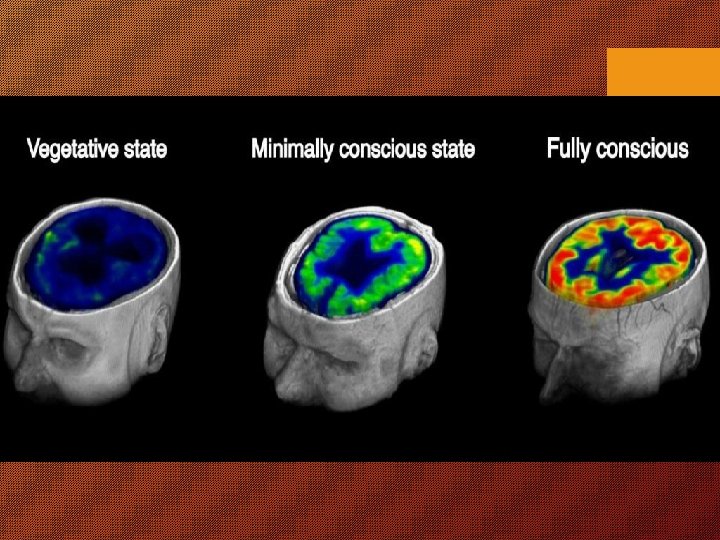
VEGETATIVE STATE • Loss of Awareness of self and surroundings. • Normal sleep wake cycles & BS reflexes. • Normal metabolic and circulatory functions. • Normal eye opening / closure & Swallowing. • Eye movements & Sensory Localization – Poor. • Doesn’t obey requ’s / No comprehensible words. • Preserved Hypothalamic & Autonomic fns. • Above findings lasting > 1 month – PVS. • CVA, SAH, Trauma, Toxin, Injury, Infn, Arrest etc. , • Low amplitude irregular Delta in EEG. • Cortical necrosis, multi-infarcts, Diffuse neuronal loss and gliosis of neocortex, hippocampus thalamus & purkinje cells – BS relatively intact.
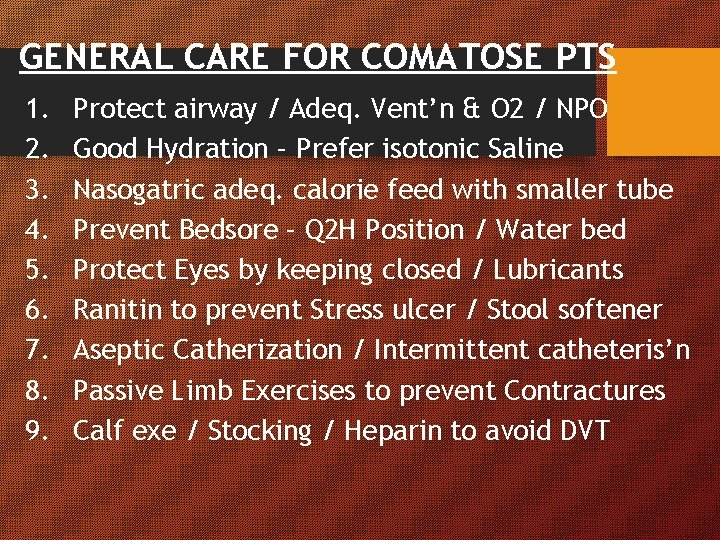
GENERAL CARE FOR COMATOSE PTS 1. 2. 3. 4. 5. 6. 7. 8. 9. Protect airway / Adeq. Vent’n & O 2 / NPO Good Hydration – Prefer isotonic Saline Nasogatric adeq. calorie feed with smaller tube Prevent Bedsore – Q 2 H Position / Water bed Protect Eyes by keeping closed / Lubricants Ranitin to prevent Stress ulcer / Stool softener Aseptic Catherization / Intermittent catheteris’n Passive Limb Exercises to prevent Contractures Calf exe / Stocking / Heparin to avoid DVT
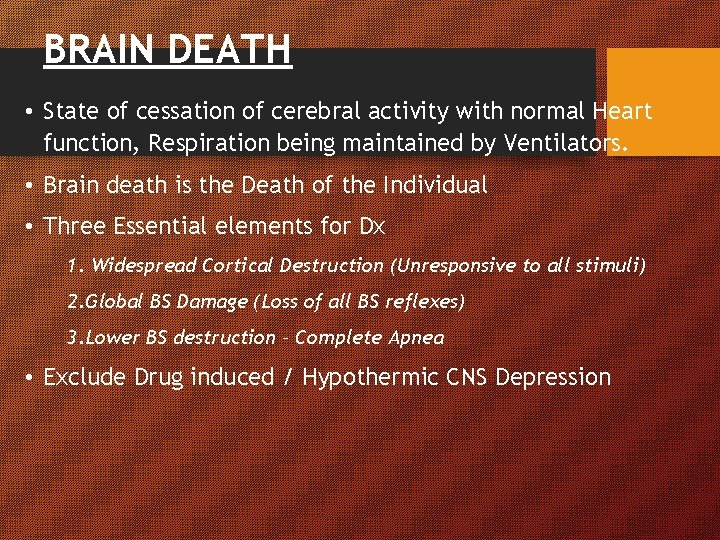
BRAIN DEATH • State of cessation of cerebral activity with normal Heart function, Respiration being maintained by Ventilators. • Brain death is the Death of the Individual • Three Essential elements for Dx 1. Widespread Cortical Destruction (Unresponsive to all stimuli) 2. Global BS Damage (Loss of all BS reflexes) 3. Lower BS destruction – Complete Apnea • Exclude Drug induced / Hypothermic CNS Depression
THANK YOU