Management of Traumatic Brain InjuryTBI in developing countries
Management of Traumatic Brain Injury(TBI) in developing countries without ICP monitoring 쭘리읍쑤어 ជរ បសរ Dong-Keun HYUN M. D. , Department of Neurosurgery, Inha University Hospital Incheon, Korea CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Traumatic Brain Injury –U. S. data • • CDC ; 1. 5 million people in the U. S. each year. 50, 000 people die from TBI each year 85, 000 people suffer long term disabilities. 5. 3 million people live with disabilities caused by TBI. • How about developing and undeveloping country? CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Contents • Classification of TBI as severity, type, image and pathophysiology • Diagnosis especially Neurologic Examinations • Managements focused medical managements without intracranial monitoring CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
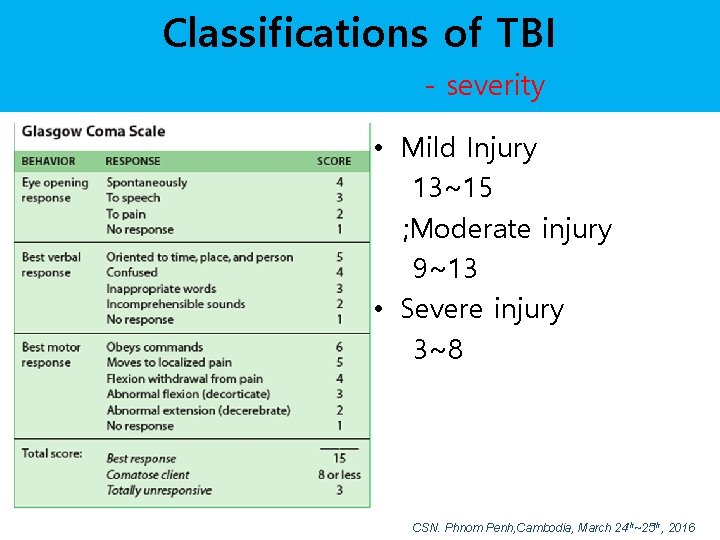
Classifications of TBI - severity • Mild Injury 13~15 ; Moderate injury 9~13 • Severe injury 3~8 CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Classifications of TBI - Type • Focal Brain injury Epidural hematoma Subdural hematoma intracerebral hematoma contusion, laceration SAH IVH • Diffuse Brain injury Concussion Diffuse axonal Injury CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Cerebral Concussion • Reversible injury • Same meaning mild traumatic TBI or mild head injury • GCS at admission 13~15 • Loss of consciousness <20 mins • No focal neurologic deficits • Memory loss after trauma , 24 hours CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
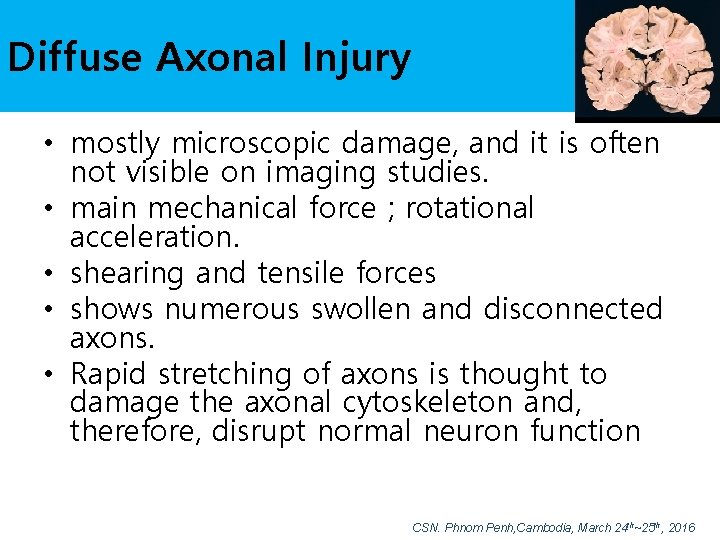
Diffuse Axonal Injury • mostly microscopic damage, and it is often not visible on imaging studies. • main mechanical force ; rotational acceleration. • shearing and tensile forces • shows numerous swollen and disconnected axons. • Rapid stretching of axons is thought to damage the axonal cytoskeleton and, therefore, disrupt normal neuron function CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Secondary injury • It may occur hours or even days after traumatic event. • Injury may result from impairment or local declines in CBF after TBI as a result of local edema, hemorrhage or increased ICP. • As a result of inadequate perfusion, cellular ion pumps may fail, causing a cascade involving intracellular calcium and sodium which may contribute to cellular destruction • Excessive release of excitatory amino acids, such as glutamate and aspartate, exacerbates failure of the ion pumps. • As the cascade continues, cells die, causing free radical formation, proteolysis, and lipid peroxidation. • These factors can ultimately cause neuronal death. CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
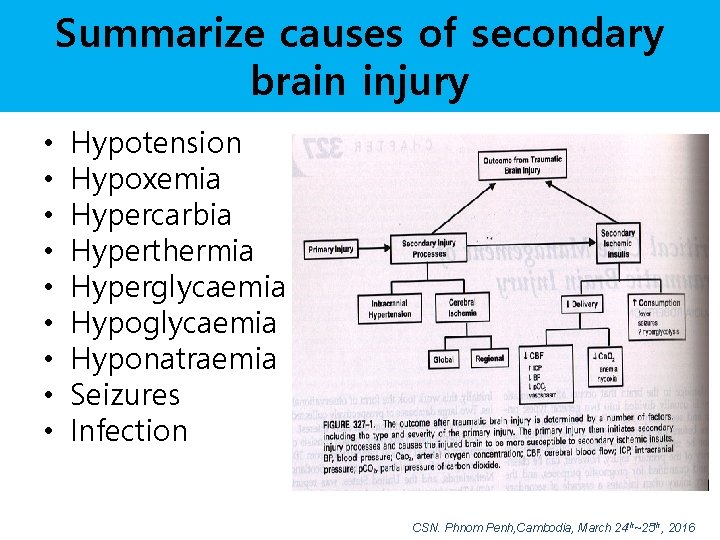
Summarize causes of secondary brain injury • • • Hypotension Hypoxemia Hypercarbia Hyperthermia Hyperglycaemia Hyponatraemia Seizures Infection CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Diagnosis of TBI -1 • Neurological examination and assigning a GCS Score. • Neuroimaging helps in determining the diagnosis and proposed treatment. • The preferred radiologic test in the emergency setting is Brain CT: it is quick, accurate, and widely available. • Follow up CT scans may be performed later to determine whether the injury has progressed. CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Diagnosis of TBI-2 • Magnetic resonance imaging (MRI) can show more details than CT as detecting injury characteristics such as diffuse axonal injury. . • X-rays are still used for head injuries Angiography may be used to detect blood vessel pathology. • Electroencephalography and transcranial doppler may also be used CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Neurologic Examination of TBI • Consciousness level 1. Alert 2. Drowsy 3. Stupor 4. Semicomatous 5. Comatous CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
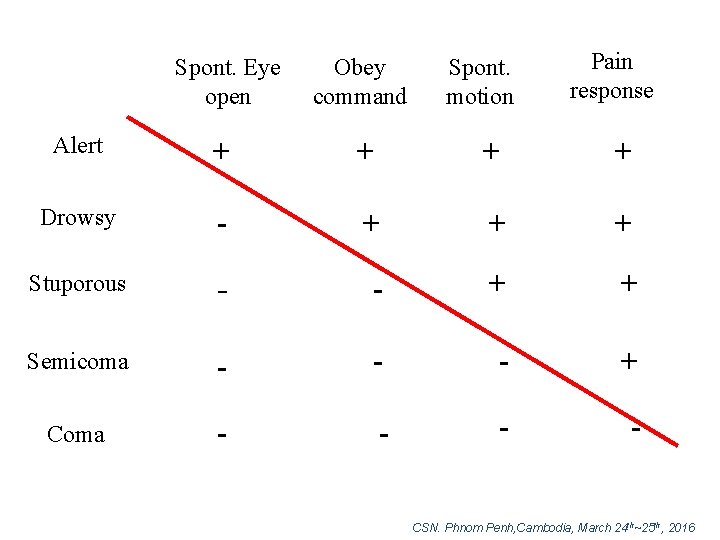
Spont. Eye open Obey command Spont. motion Pain response Alert + + Drowsy - + + + Stuporous - - + + Semicoma - - - + Coma - - CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
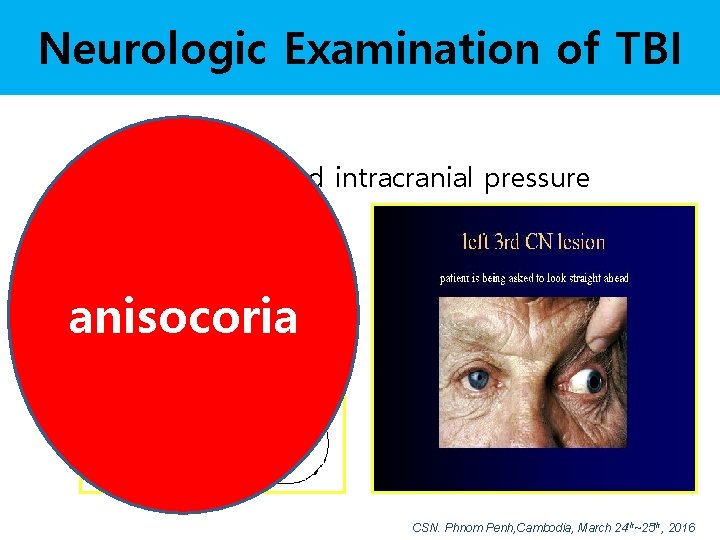
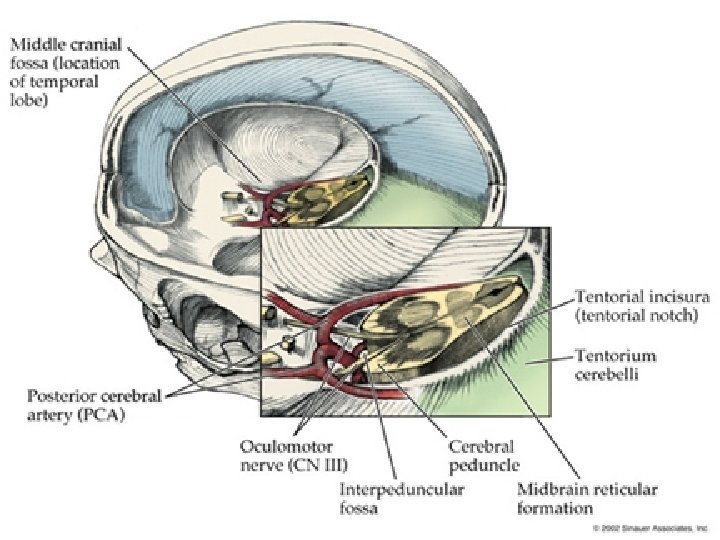
Neurologic Examination of TBI • Signs of increased intracranial pressure – Visual difficulties – Vomiting anisocoria – Dyspnea – Decreased pulse CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
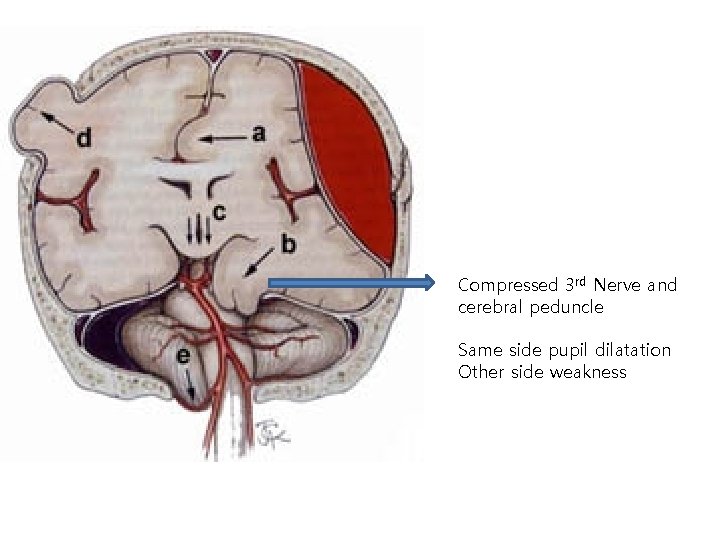
Compressed 3 rd Nerve and cerebral peduncle Same side pupil dilatation Other side weakness

Funduscopic findings of Increased Intracranial hypertension(IICP) papilledema ; chronic elevated ICP IICP -> optic n. sheath compression -> venous circulation compression cf)acute elevated ICP ; retinal hemorrhage, congestion CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
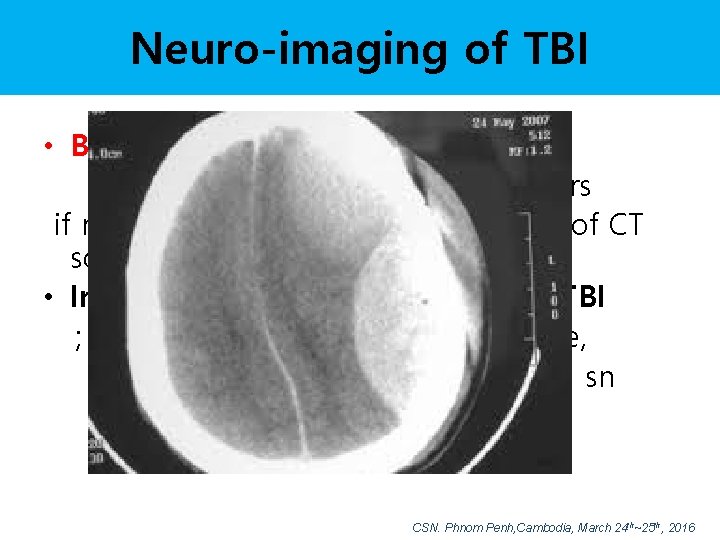
Neuro-imaging of TBI • Brain CT – first choice of TBI must be available 24 hours if not available, 24 hrs – just one slice of CT scan may give helps • Indications of Brain CT after Mild TBI ; altered consciousness, skull fracture, LOC, focal neurological deficit, IICP sn and sx, antiplatelet medication, symptoms aggravation CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Signs of Increased ICP decreasing level of consciousness, paralysis or weakness on one side of the body, Light reflex and anisocoria Cushing's triad, a slow heart rate with high blood pressure and respiratory depression • Abnormal posturing • Small children with moderate to severe TBI may have some of these symptoms. • Other signs seen in young children include persistent crying, inability to be consoled, listlessness, refusal to nurse or eat and irritability • • CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Controle of Increased ICP • • • osmotherapy analgesia sedation optimal ventilation surgical positioning of patient CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016

Managements
The specific goals in the acute management of severe traumatic brain injury are: Focused Increased 1. Protect the airway & oxygenation 2. Ventilate to normocapnia 3. Correct hypovolaemia & hypotension 4. CT Scan when appropriate 5. Neurosurgery if indicated 6. Intensive Care for further monitoring and management 7. Prevent complications intracranial hypertension CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016

ICP IS JUST EPIPHENOM OF TBI Dr. Chesnut

Sins of the Past Most of our current understanding about ICP comes from studies done in the 70’s, 80’s, and 90’s UW/HMC Neurotrauma Research Group
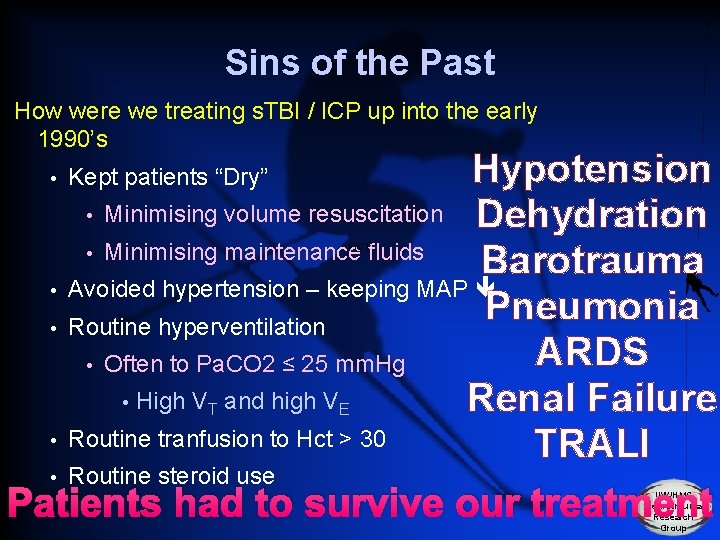
Sins of the Past How were we treating s. TBI / ICP up into the early 1990’s Hypotension • Minimising volume resuscitation Dehydration • Minimising maintenance fluids Barotrauma • Avoided hypertension – keeping MAP Pneumonia • Routine hyperventilation ARDS • Often to Pa. CO 2 ≤ 25 mm. Hg • High V and high V Renal Failure • Routine tranfusion to Hct > 30 TRALI • Routine steroid use Patients had to survive our treatment • Kept patients “Dry” T E UW/HMC Neurotrauma Research Group
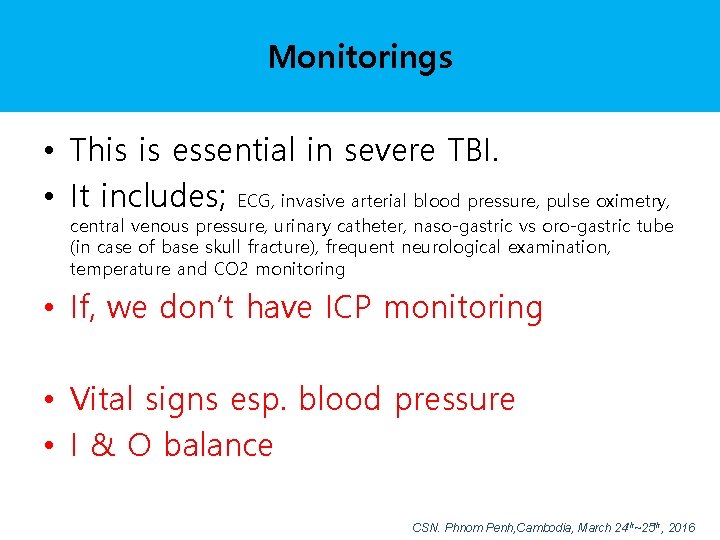
Monitorings • This is essential in severe TBI. • It includes; ECG, invasive arterial blood pressure, pulse oximetry, central venous pressure, urinary catheter, naso-gastric vs oro-gastric tube (in case of base skull fracture), frequent neurological examination, temperature and CO 2 monitoring • If, we don’t have ICP monitoring • Vital signs esp. blood pressure • I & O balance CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
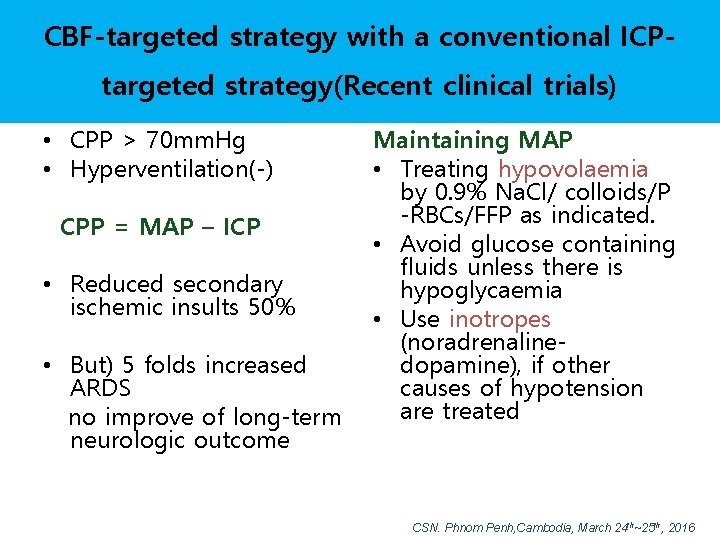
CBF-targeted strategy with a conventional ICPtargeted strategy(Recent clinical trials) • CPP > 70 mm. Hg • Hyperventilation(-) CPP = MAP – ICP • Reduced secondary ischemic insults 50% • But) 5 folds increased ARDS no improve of long-term neurologic outcome Maintaining MAP • Treating hypovolaemia by 0. 9% Na. Cl/ colloids/P -RBCs/FFP as indicated. • Avoid glucose containing fluids unless there is hypoglycaemia • Use inotropes (noradrenalinedopamine), if other causes of hypotension are treated CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
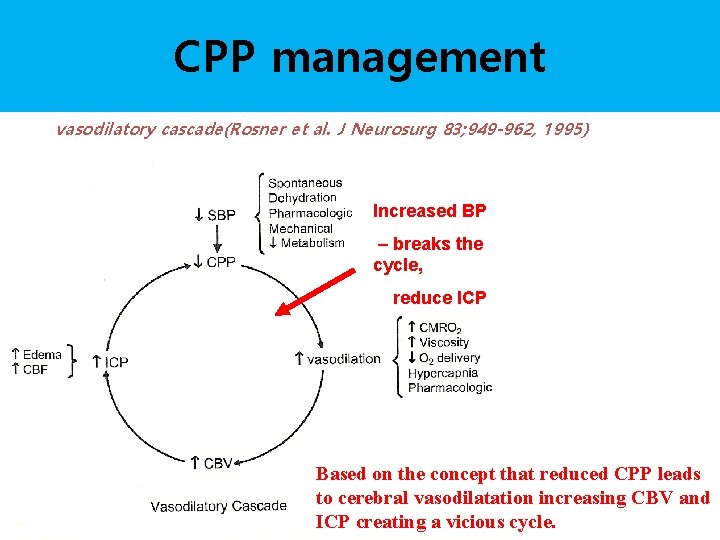
CPP management vasodilatory cascade(Rosner et al. J Neurosurg 83; 949 -962, 1995) Increased BP – breaks the cycle, reduce ICP Based on the concept that reduced CPP leads to cerebral vasodilatation increasing CBV and ICP creating a vicious cycle.
Blood pressure and oxygenation • BP should be monitored and hypotension(systolic < 90 mm. Hg) avoided • Oxygenation shoud be monitored • Hypoxia; Pa. O 2<60 mm. Hg or O 2 saturation<90% avoided (II) CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Airway protection and controlled ventilation • Trauma Coma Data Bank ; Hypoxia : 19% of comatose head-injured patients arrival at ER • hypoxia, hypercarbia dramatically raised ICP • controlled ventilation prevent rapid changes in Pa. CO 2 CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Hyperventilation • Pa. CO 2 < 20 to 25 mm Hg Pa. CO 2 1 mm Hg -> 2% CBF change • Prophylactic hyperventilation (Pa. CO 2 <25 mm. Hg) is not recommended(II) • Hyperventilation is recommended as a temporizing measure for the reduction of elevated ICP • Should be avoided during the first 24 hrs after injury when CBF is often critically reduced (Level III recommended) CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Indications early intubation • Comatous consciousness ; GCS<8 • Can not obey command with tachypnea(30/min), sternal recession or upper airway bleeding • Pa. O 2<70 mm. Hg or Pa. CO 2>45 mm. Hg CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Head elevation 30 ˚ • Moraine JJ et al ; Is cerebral perfusion pressure a major determinant of cerebral blood flow during head elevation in comatose patients with severe intracranial lesions? J Neurosurg 92: 606 -614, 2000 0~45 ˚head elevation ICP gradual decrease to 30˚ elevation to initial pr at 45˚ CBF gradual decrease to 45 ˚ CPP maintain to 30 ˚ decrease to 45 ˚ • Ivan Ng et al : Effects of head posture on cerebral hemodynamics: its influences on intracranial pressure, cerebral perfusion pressure, and cerebral oxygenation. Neurosurg March(54) No 3. 593 -603, 2004 ICP was significant lower than 0 degree, MAP remained relatively unchanged. CPP, global venous cerebral oxygenation, regional cerebral oxygenation were not affected. Benefits reduction of ICP without compromising CPP and cardiac output prevent gastric reflux decreased pulmonary aspiration compared with head flat position Decreased ICP CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Mannitol mannose alcohol(1962, Wise & Chater) Rapid infusion during 15 minutes and continued effect for 4 hours Effect - early; blood viscosity decreased, increased blood flow ->vasoconstriction - late; osmotic dehydration • Mannitol is effective for control of raised ICP at dose of 0. 25 gm/kg to 1 g/Kg body weight • Arterial hypotension(systolic BP<90 mm. Hg) should be avoid(II) Keep Renal function (S-osm < 320 m. Osm/L), electrolytes abnormality CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016

Other Treatments • • Hypothermia or prophylactic hypothermia Infection prophylaxis Deep vein thrombosis prevention Induced coma therapy ; Barbiturate, sedative, analgesics, profopol Nutrition Seizure prevention Fever Steroid CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
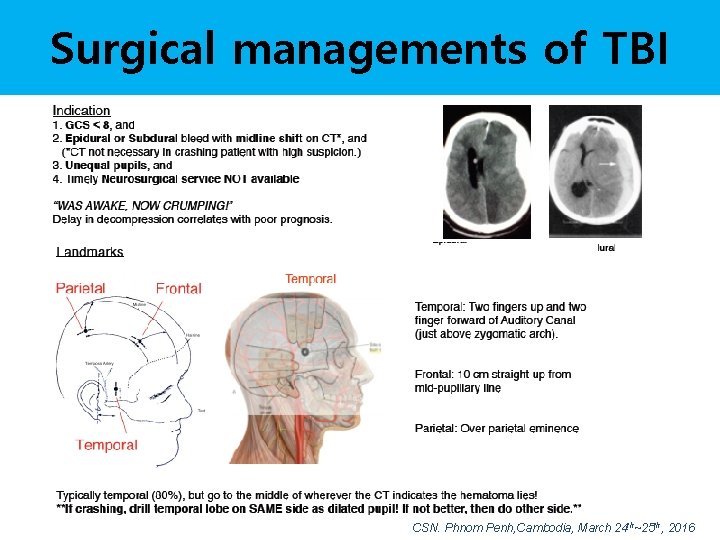
Surgical managements of TBI CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016

Surgical managements of TBI Decompressive craniectomy standard and extended CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
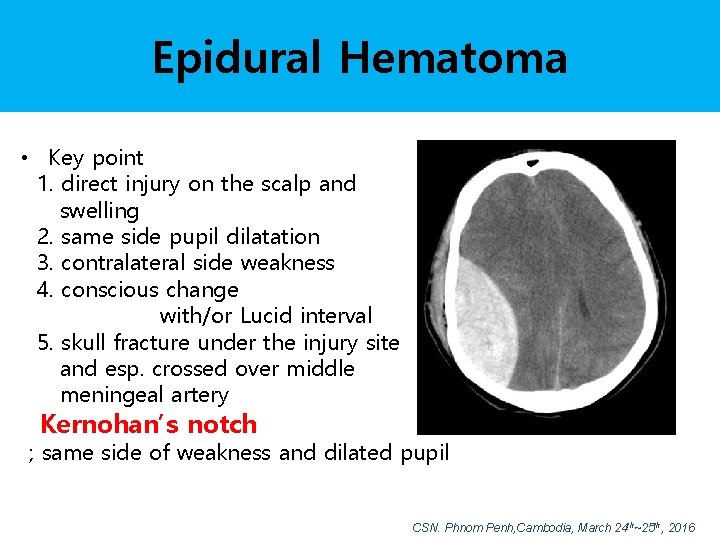
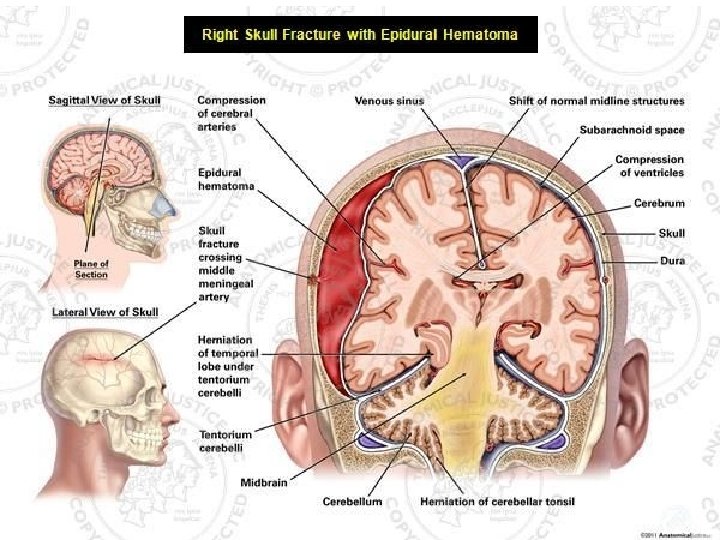
Epidural Hematoma • Key point 1. direct injury on the scalp and swelling 2. same side pupil dilatation 3. contralateral side weakness 4. conscious change with/or Lucid interval 5. skull fracture under the injury site and esp. crossed over middle meningeal artery Kernohan’s notch ; same side of weakness and dilated pupil CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
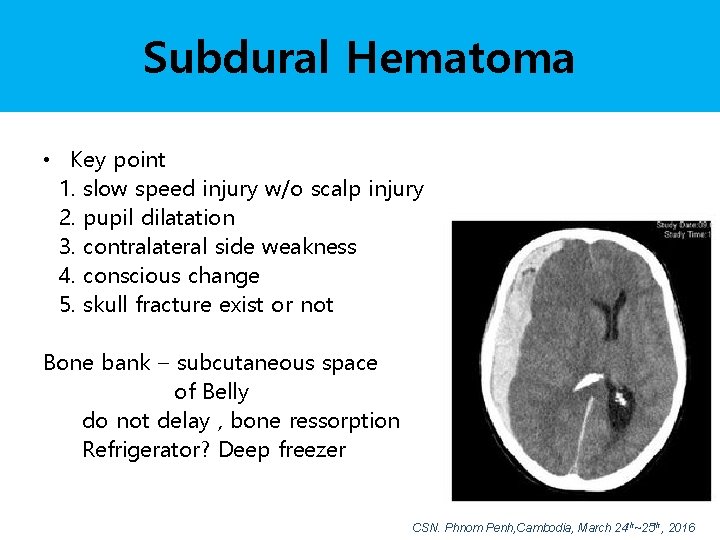
Subdural Hematoma • Key point 1. slow speed injury w/o scalp injury 2. pupil dilatation 3. contralateral side weakness 4. conscious change 5. skull fracture exist or not Bone bank – subcutaneous space of Belly do not delay , bone ressorption Refrigerator? Deep freezer CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016


Sirkaks, Inca neurosugeon, Ancient Peru
How Brain Injuries treated? CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
How Brain Injuries treated? CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Summary Medical managements of TBI • ICP is not the target, just tools • Preventing Secondary injury • Neurological evaluation and CT scan, timely, frequently • Blood pressure, MAP ; keep brain perfusion pressure • Intravascular volume ; no dry brain • Keep Body balance(nutrition, electrolyte etc) • Preventing side effect ; fever, infection, seizure • If available, hypothermia, coma therapy • Most important monitoring ; care giver(Dr. Nurse) CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
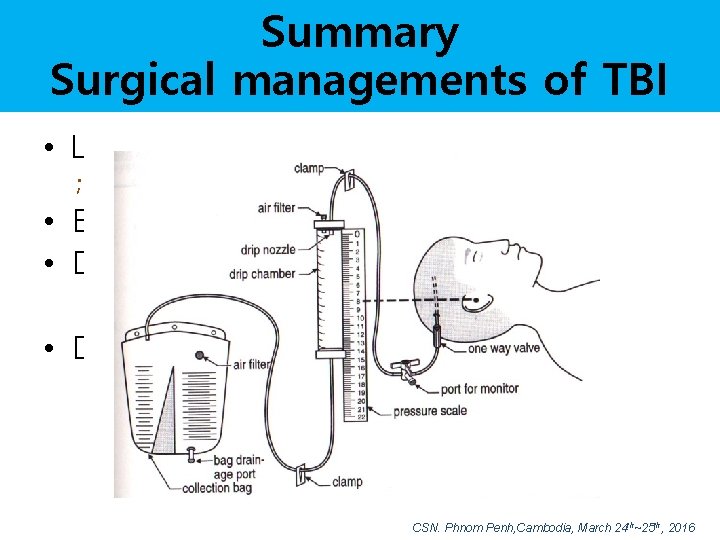
Summary Surgical managements of TBI • Lower intracranial pressure ; surgical removal of primary lesions • Extraventricular drainage, if needed • Decompressive craniectomy ; unilateral or bilateral, bifrontal • Decra, Rescueicp – no benefit to longterm effect ; maybe stretching injury CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
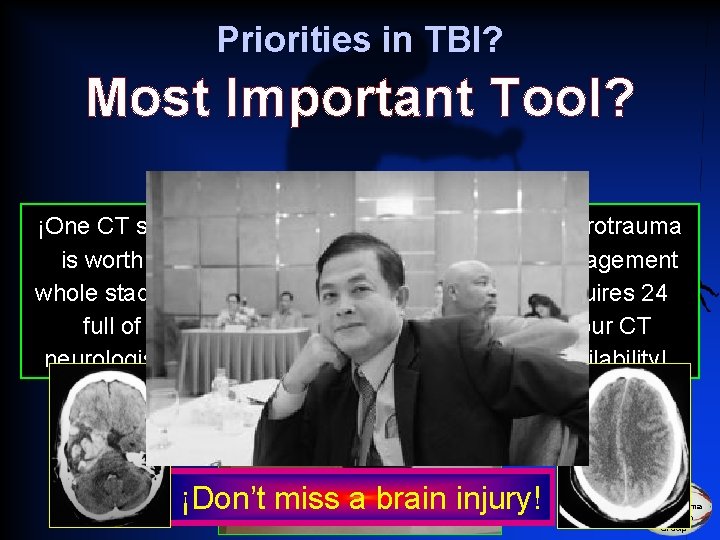
Priorities in TBI? Most Important Tool? ¡One CT scan is worth a whole stadium full of neurologists! ¡Neurotrauma management requires 24 hour CT availability! ¡Know what you are treating! ¡Don’t miss a brain injury! UW/HMC Neurotrauma Research Group
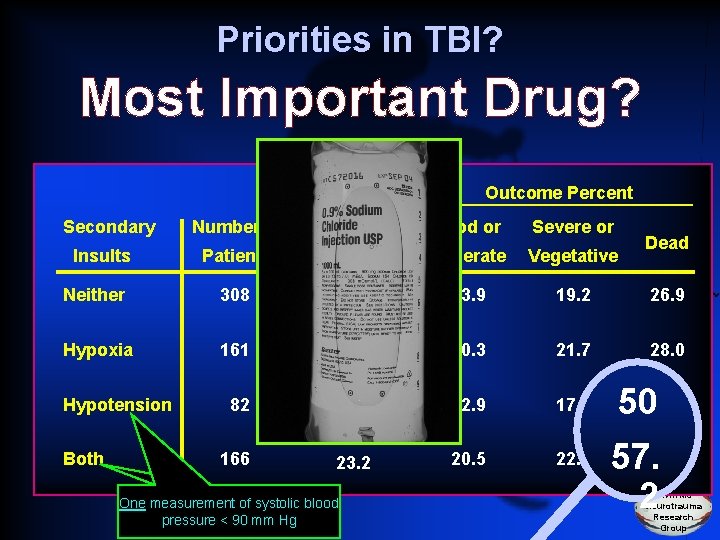
Priorities in TBI? Most Important Drug? Outcome Percent Secondary Number of Good or Severe or Insults Patients Moderate Vegetative Neither 308 43. 0 53. 9 19. 2 26. 9 Hypoxia 161 22. 4 50. 3 21. 7 28. 0 Hypotension 82 11. 4 32. 9 17. 1 5050. 0 Both 166 23. 2 20. 5 22. 3 One measurement of systolic blood pressure < 90 mm Hg Dead 57. 2 2 UW/HMC Neurotrauma Research Group

Priorities in TBI? Most Important Monitor? UW/HMC Neurotrauma Research Group

Thank You Cambodia CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Prophylactic Hypothermia • Not significantly associated with decreased mortality when compared with normothermic controls. • However, preliminary findings suggest that a greater decreased in mortality risk is observed when target temperatures are maintained for more than 48 hrs(III) • Target temperature 32 -33 ℃ or >33 ℃ • Rewarming 1 degress/hr CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Mechanisms of Hypothermia a. Decreased cerebral metabolism (decrease glucose and O 2 consumption) - each 1℃ decrease in temperature, cerebral metabolic decrease 6 -7% b. Inhibition of caspase activation and prevention of mitochondrial dysfunction - prevent cell injury from leading to apoptosis c. Decreased overload of excitatory neurotransmitters and modification of intracellular ion concentrations Suppressed ischemic-induced inflammatory reactions and release of inflammatory cytokines d. e. Decreased free-radical production f. Vascular permeability(BBB stabilization) an decreased edema formation g. Maintenance cell membrane integrity, reduced intracellular acidosis CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Method of Hypothermia a. placing cold blankets or wet gause b. continuous infusion of paralytic drugs to prevent to shivering but, keep cough reflex c. rectal temperature 33℃ & maintain d. rewarming : rate no greater than 1 ℃/hour e. limitation ; cardiovascular diseases, traumatic shock, age(less than 15 or older than 65) CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Side effects of Hypothermia • • • Cardiac suppression(decrease MABP, HR) Renal effect – severe polyuresis Electrolyte imbalance Infection, decreased immunity Coagulation abnormality CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Infection prophylaxis • Periprocedural antibiotics for intubation should be administrated to reduced the incidence of pneumonia. However, it does not change length of stay or mortality • Early tracheostomy should be performed to reduced mechanical ventilation days. However, it does not alter mortality or the rate of nosocomial pneumonia(II) • Routine ventricular catheter exchange of prophylactic antibiotic use for ventricular catheter placement is not recommended to reduce infection(III) CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Deep vein thrombosis prophylaxis(III) • Graudated compression stocking or intermittent pneumatic compression(IPC) stockings are recommended, unless lower extremity injuries prevent their use. Use shoud be continued until patients are ambulatory • Low molecular weight heparin(LMWH) or low dose unfractionated heparin should be used in combination with mechanical prophylaxis. However, there is an increased risk for expansion of intracranial hemorrhage • ; insufficient evidence to support ; preferred agents, dose, or timing of pharmacological prophylaxis for deep vein thrombosis(DVT) CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
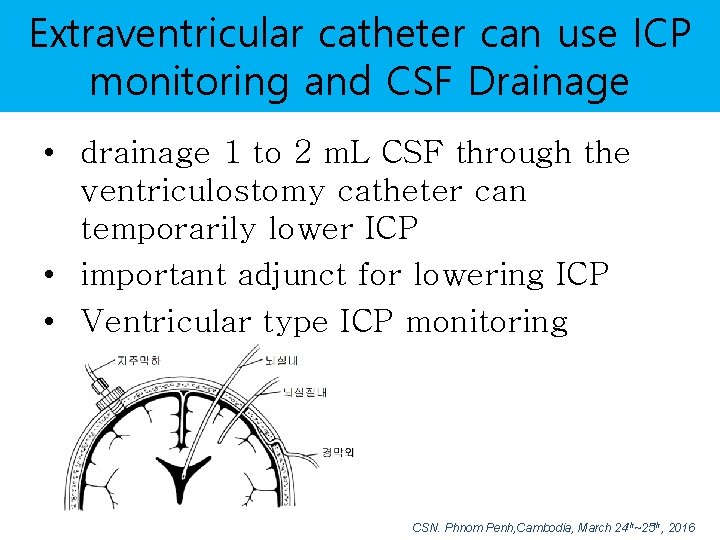
Extraventricular catheter can use ICP monitoring and CSF Drainage • drainage 1 to 2 m. L CSF through the ventriculostomy catheter can temporarily lower ICP • important adjunct for lowering ICP • Ventricular type ICP monitoring CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016

Anesthetics, Analgesics, and Sedatives • Prophylactic administration of barbiturates to induce burst suppression EEG is not recommended • High-dose barbiturate administration is recommended to control elevated ICP refractory to maximum standard medical and surgical treatment. Hemodynamic stability is essential before and during barbiturate therapy. • Propofol is recommended for the control of ICP, but not for improvement in mortality or 6 months outcome. CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
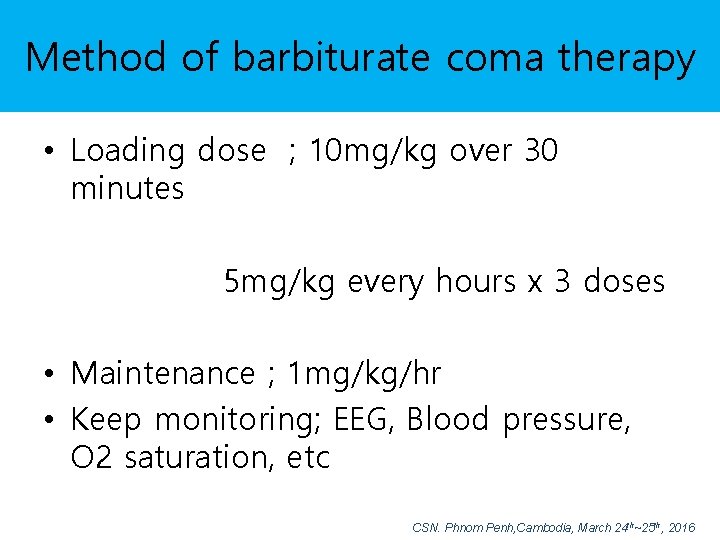
Method of barbiturate coma therapy • Loading dose ; 10 mg/kg over 30 minutes 5 mg/kg every hours x 3 doses • Maintenance ; 1 mg/kg/hr • Keep monitoring; EEG, Blood pressure, O 2 saturation, etc CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
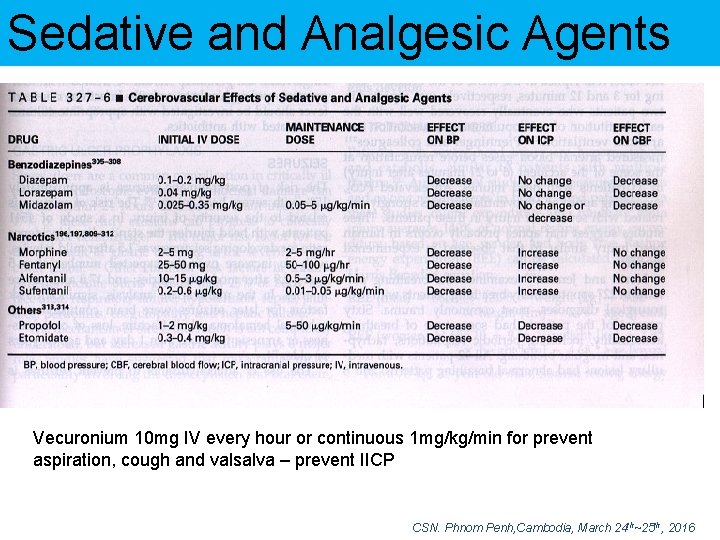
Sedative and Analgesic Agents Vecuronium 10 mg IV every hour or continuous 1 mg/kg/min for prevent aspiration, cough and valsalva – prevent IICP CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
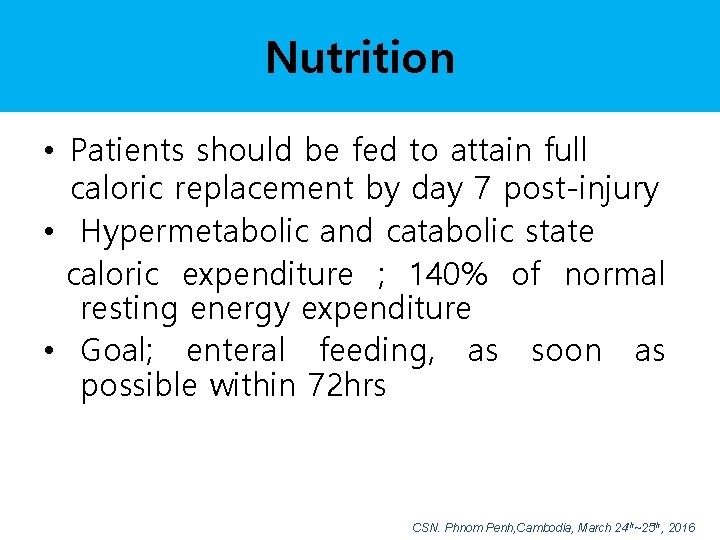
Nutrition • Patients should be fed to attain full caloric replacement by day 7 post-injury • Hypermetabolic and catabolic state caloric expenditure ; 140% of normal resting energy expenditure • Goal; enteral feeding, as soon as possible within 72 hrs CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
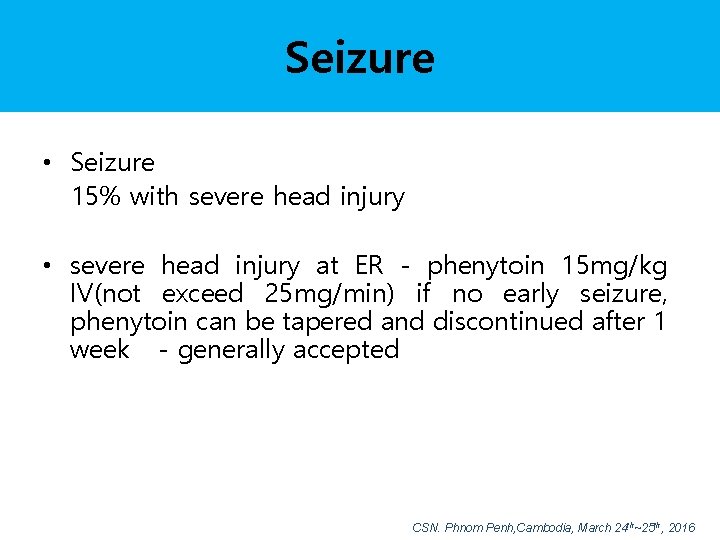
Seizure • Seizure 15% with severe head injury • severe head injury at ER - phenytoin 15 mg/kg IV(not exceed 25 mg/min) if no early seizure, phenytoin can be tapered and discontinued after 1 week - generally accepted CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Antiseizure Prophylaxis • Prophylactic use of phenytoin or valproate is not recommended for preventing late posttraumatic seizure(PTS) • Anticonvulsants are indicated to decrease the incidence of early PTS(within 7 days of injury). However, early PTS is not associated with worse outcomes. CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Fever • Fever common during recovery from a head injury potent cerebral vasodilator and raised ICP increased cerebral metabolic requirement treatments – antipyretics cooling blankets infection controlled CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Steroids • not recommended for improving outcome or reducing ICP. Moderate or severe TBI, high-dose methylprednisolone is associated with increased mortality and is not recommended(I) CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
Hyperventilation • Pa. CO 2 < 20 to 25 mm Hg Pa. CO 2 1 mm Hg -> 2% CBF change • Prophylactic hyperventilation (Pa. CO 2 <25 mm. Hg) is not recommended(II) • Hyperventilation is recommended as a temporizing measure for the reduction of elevated ICP • Should be avoided during the first 24 hrs after injury when CBF is often critically reduced (Level III recommended) CSN. Phnom Penh, Cambodia, March 24 th~25 th, 2016
- Slides: 67