MANAGEMENT OF THE CLIENT EXPERIENCING SHOCK Shock Definition





- Slides: 27
MANAGEMENT OF THE CLIENT EXPERIENCING SHOCK
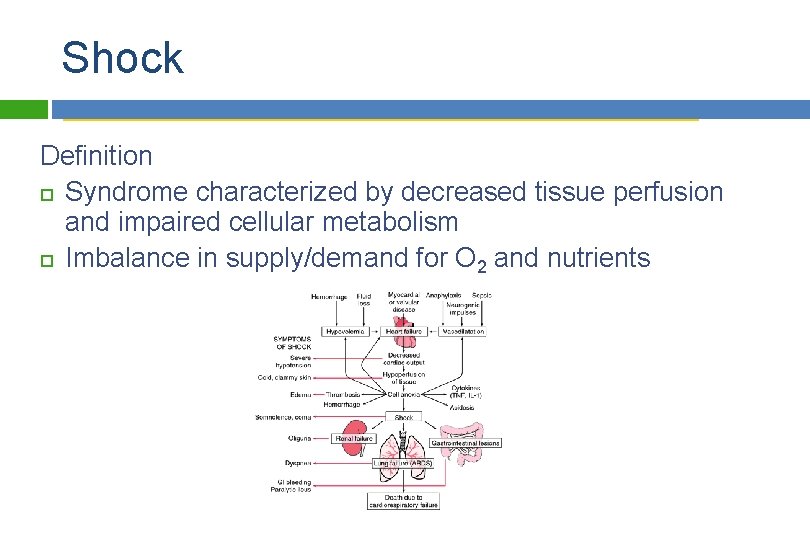
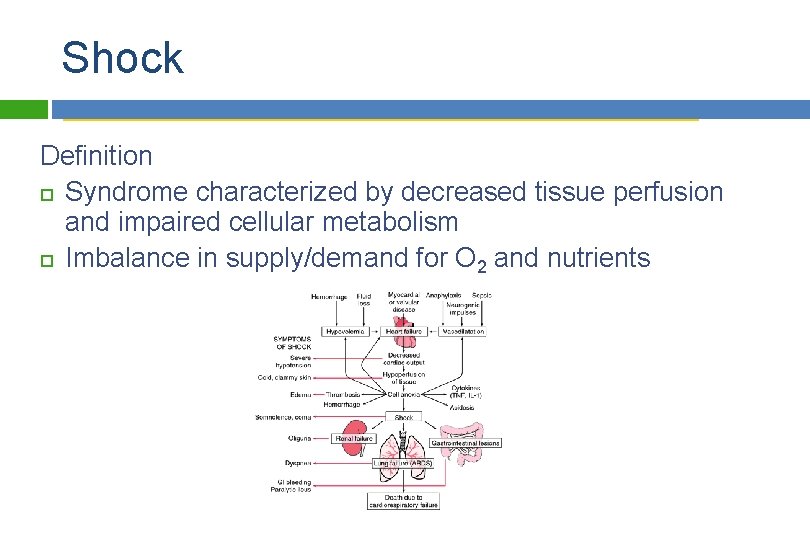
Shock Definition Syndrome characterized by decreased tissue perfusion and impaired cellular metabolism Imbalance in supply/demand for O 2 and nutrients Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
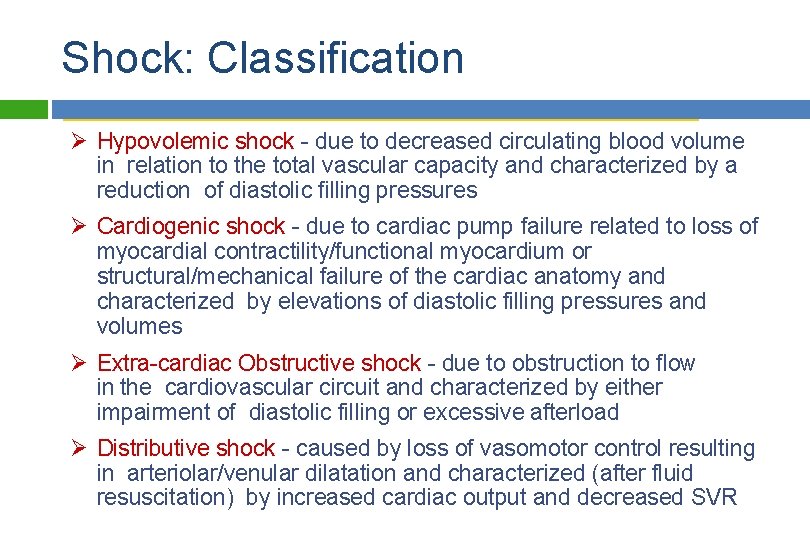
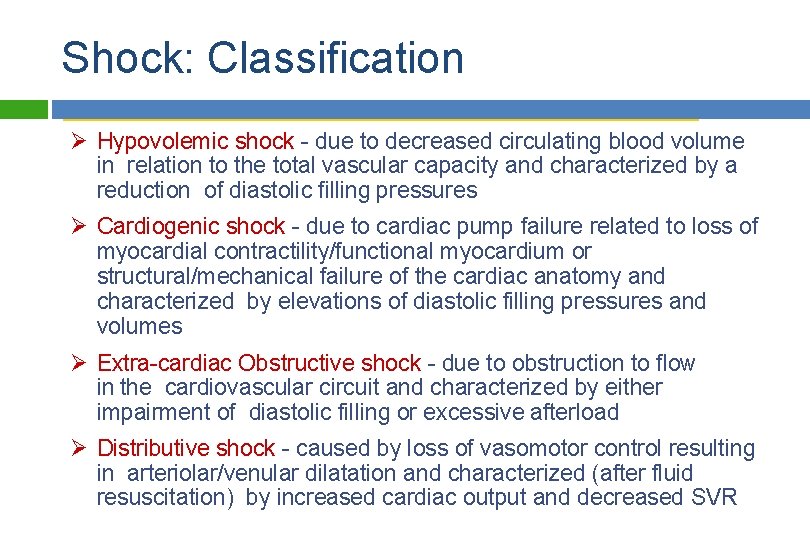
Shock: Classification Ø Hypovolemic shock - due to decreased circulating blood volume in relation to the total vascular capacity and characterized by a reduction of diastolic filling pressures Ø Cardiogenic shock - due to cardiac pump failure related to loss of myocardial contractility/functional myocardium or structural/mechanical failure of the cardiac anatomy and characterized by elevations of diastolic filling pressures and volumes Ø Extra-cardiac Obstructive shock - due to obstruction to flow in the cardiovascular circuit and characterized by either impairment of diastolic filling or excessive afterload Ø Distributive shock - caused by loss of vasomotor control resulting in arteriolar/venular dilatation and characterized (after fluid resuscitation) by increased cardiac output and decreased SVR Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Shock facts Cardiogenic shock - a major component of the mortality associated with cardiovascular disease (the #1 cause of U. S. deaths) Hypovolemic shock - the major contributor to early mortality from trauma (the #1 cause of death in those < 45 years of age) Septic shock - the most common cause of death in American ICUs (the 13 th leading cause of death overall in US) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
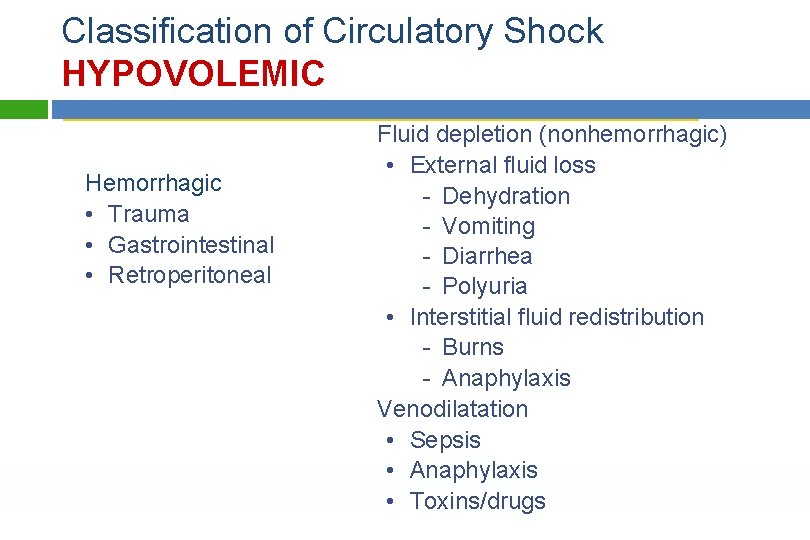
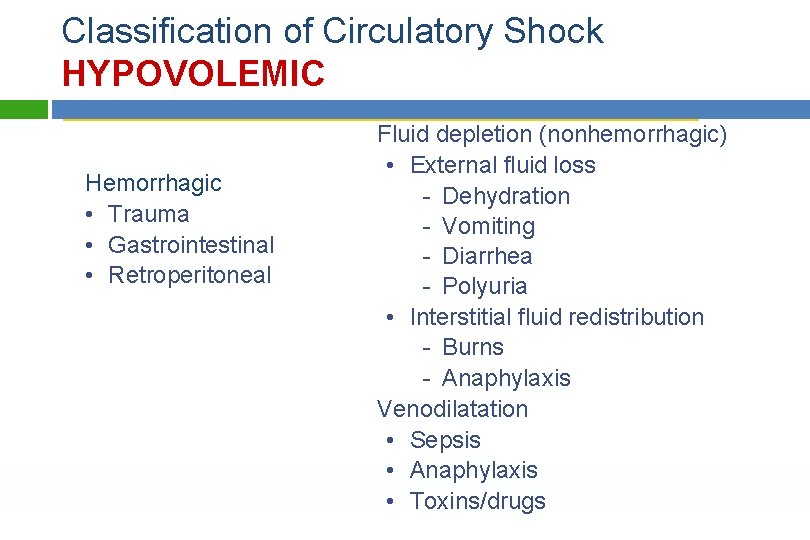
Classification of Circulatory Shock HYPOVOLEMIC Fluid depletion (nonhemorrhagic) • External fluid loss Hemorrhagic - Dehydration • Trauma - Vomiting • Gastrointestinal - Diarrhea • Retroperitoneal - Polyuria • Interstitial fluid redistribution - Burns - Anaphylaxis Venodilatation • Sepsis • Anaphylaxis Copyright © 2014 by Mosby, an imprint of Elsevier Inc. • Toxins/drugs
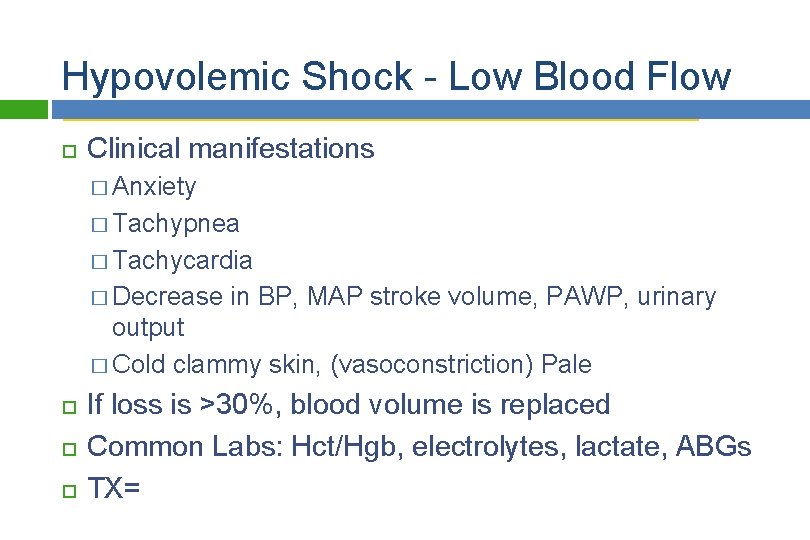
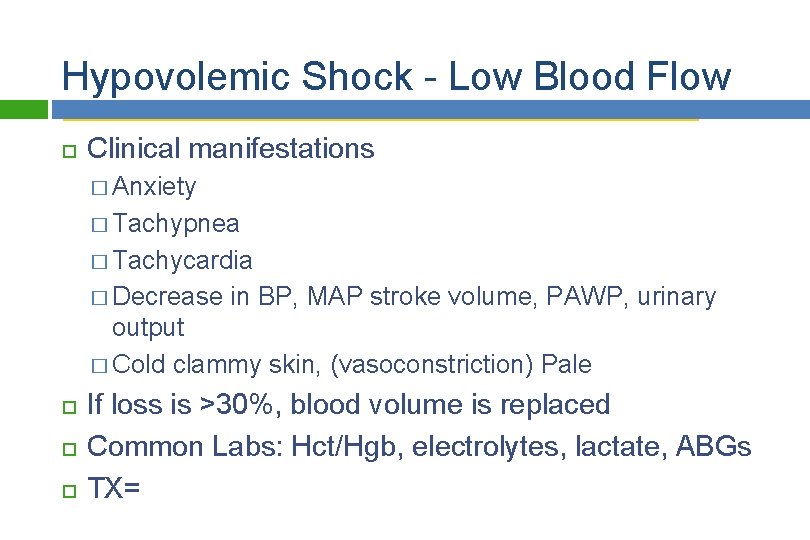
Hypovolemic Shock - Low Blood Flow Clinical manifestations � Anxiety � Tachypnea � Tachycardia � Decrease in BP, MAP stroke volume, PAWP, urinary output � Cold clammy skin, (vasoconstriction) Pale If loss is >30%, blood volume is replaced Common Labs: Hct/Hgb, electrolytes, lactate, ABGs TX= Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
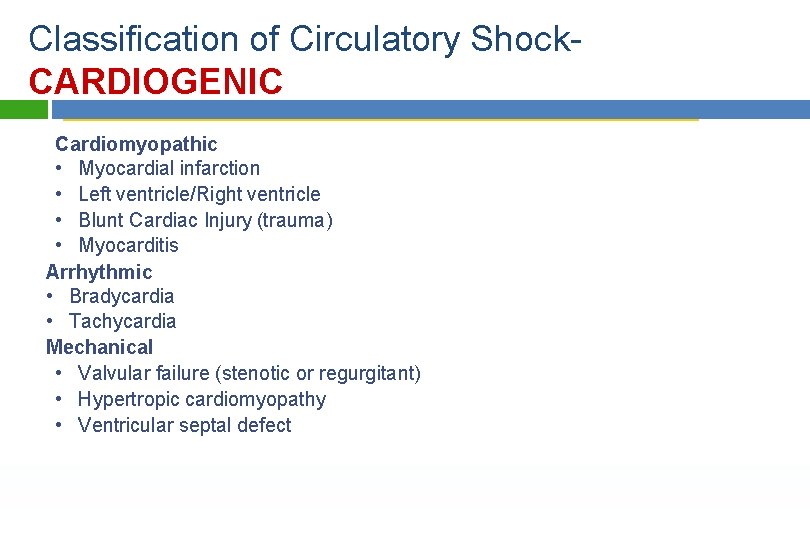
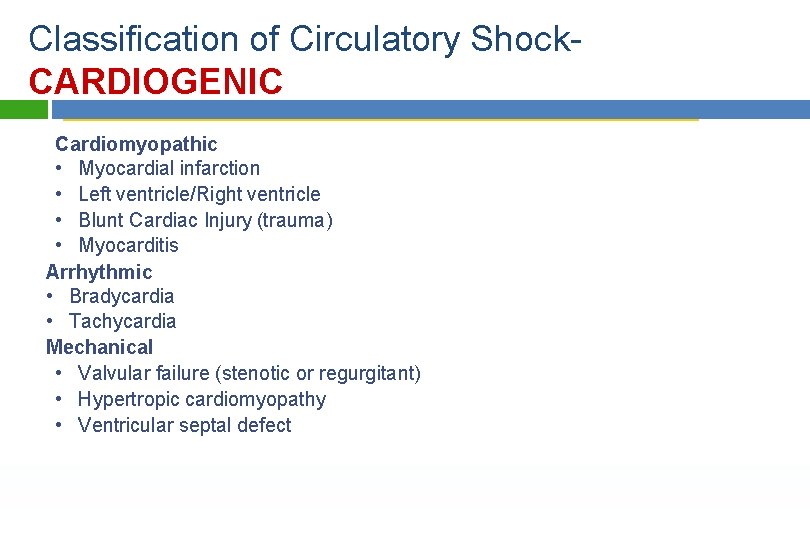
Classification of Circulatory Shock. CARDIOGENIC Cardiomyopathic • Myocardial infarction • Left ventricle/Right ventricle • Blunt Cardiac Injury (trauma) • Myocarditis Arrhythmic • Bradycardia • Tachycardia Mechanical • Valvular failure (stenotic or regurgitant) • Hypertropic cardiomyopathy • Ventricular septal defect Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
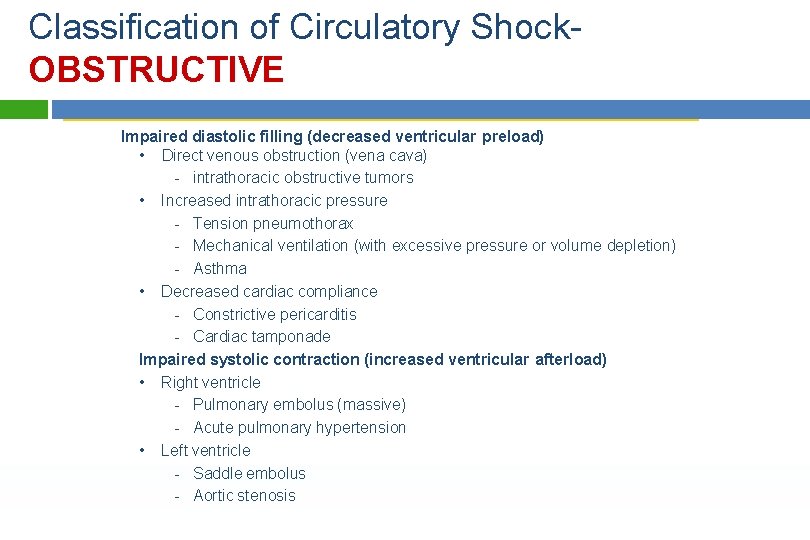
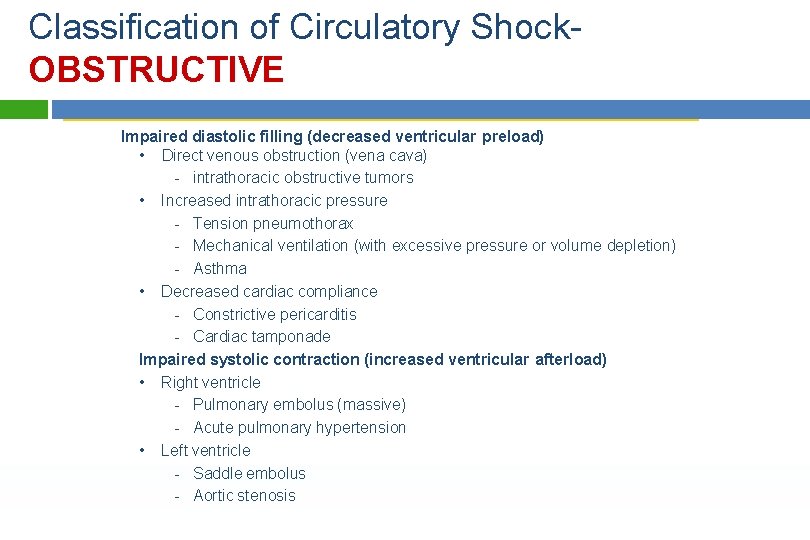
Classification of Circulatory Shock. OBSTRUCTIVE Impaired diastolic filling (decreased ventricular preload) • Direct venous obstruction (vena cava) - intrathoracic obstructive tumors • Increased intrathoracic pressure - Tension pneumothorax - Mechanical ventilation (with excessive pressure or volume depletion) - Asthma • Decreased cardiac compliance - Constrictive pericarditis - Cardiac tamponade Impaired systolic contraction (increased ventricular afterload) • Right ventricle - Pulmonary embolus (massive) - Acute pulmonary hypertension • Left ventricle - Saddle embolus - Aortic stenosis Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
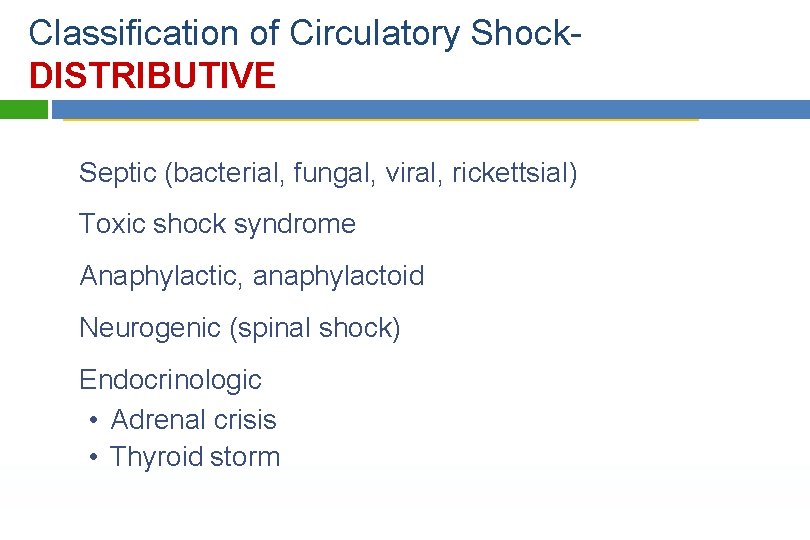
Classification of Circulatory Shock. DISTRIBUTIVE Septic (bacterial, fungal, viral, rickettsial) Toxic shock syndrome Anaphylactic, anaphylactoid Neurogenic (spinal shock) Endocrinologic • Adrenal crisis • Thyroid storm Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
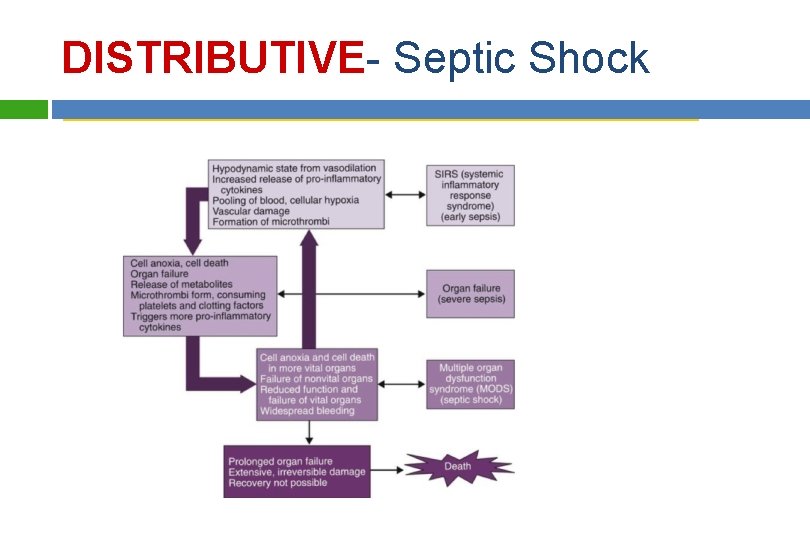
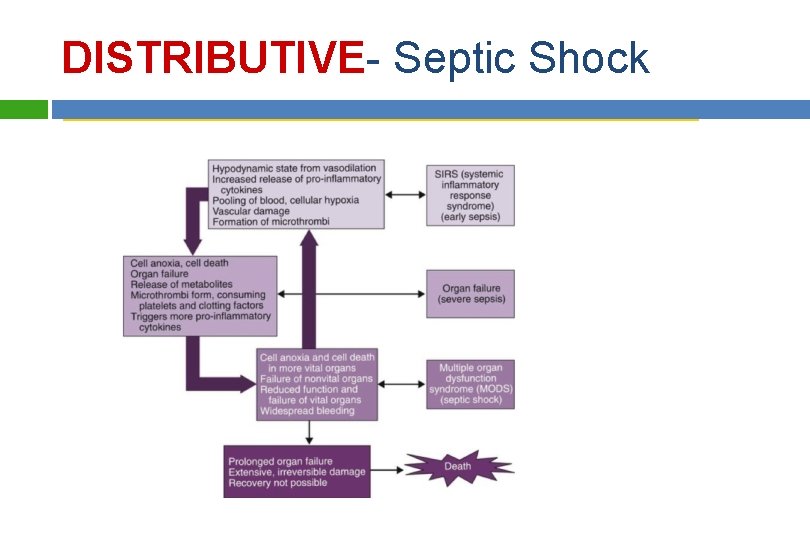
DISTRIBUTIVE- Septic Shock Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
DISTRIBUTIVE- Septic Shock Clinical manifestations �Tachypnea/hyperventilation �Temperature dysregulation �↓ Urine output �Altered neurologic status �GI dysfunction �Respiratory failure Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
DISTRIBUTIVE- Anaphylactic Shock Acute, life-threatening hypersensitivity (allergic) reaction � Massive vasodilation � Release of vasoactive mediators � ↑ Capillary permeability Swelling of the lips and tongue, angioedema � Anxiety, confusion, dizziness Wheezing, stridor Sense of impending doom Flushing, pruritus, urticaria � Chest pain Respiratory distress and � Incontinence circulatory failure Clinical manifestations Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
DISTRIBUTIVE- Neurogenic Shock Hemodynamic phenomenon Can occur within 30 minutes of a spinal cord injury at the fifth thoracic (T 5) vertebra or above Can last up to 6 weeks Can occur in response to spinal anesthesia Results in massive vasodilation, leading to pooling of blood in vessels Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
DISTRIBUTIVE- Neurogenic Shock Clinical manifestations � Hypotension � Bradycardia � Temperature dysregulation (resulting in heat loss) � Dry skin � Poikilothermia (taking on the temperature of the environment) Treatment aimed at symptoms Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Stages of Shock 1. Initial stage � MAP is decreased by less than 10 m g. 2. Nonprogressive stage � MAP decreases by 10 to 15 m g from baseline � Tissue hypoxia occurs in nonvital organs 3. Progressive stage � decrease in MAP of more than 20 m g � Vital organs are hypoxic 4. Refractory stage � Development of multiple organ dysfunction syndrome (MODS). Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Diagnosis and Evaluation Assessment, Lab and Diagnostic Tests Physical Assessment Hgb, WBC, platelets PT/PTT Electrolytes Arterial blood gases BUN, Cr Ca, Mg, Blood Sugar Serum lactate, Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Diagnosis and Evaluation. Monitoring 12 -lead ECG Chest x-ray Hemodynamic monitoring Arterial pressure catheter (monitors 2 systemic BP) 2 2 CVP monitoring (2 -6 mm Hg) Pulmonary artery catheter SVO 2 Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Collaborative Care Successful management includes: � Identification of patients at risk for shock � Integration of the patient’s history, physical examination, and clinical findings to establish a diagnosis General management strategies � Ensure patent airway � Maximize oxygen delivery � Increase supply Oxygen and ventilation 1. 2. 3. Optimize CO with fluid replacement or drugs Increase hemoglobin by transfusion Increase arterial oxygen with supplemental oxygen and mechanical ventilation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Collaborative Care Fluid Resuscitation � Cornerstone of therapy for septic, hypovolemic, and anaphylactic shock = volume expansion � Isotonic crystalloids (e. g. , normal saline) for initial resuscitation of shock Volume expansion � If the patient does not respond to 2– 3 L of crystalloids, blood administration and central venous monitoring may be instituted Complications of fluid resuscitation Hypothermia Coagulopath Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Collaborative Care Primary goal of drug therapy = correction of decreased tissue perfusion � Vasopressor drugs (e. g. , norepinephrine) Achieve/maintain MAP >60 to 65 mm Hg Reserved for patients unresponsive to fluid resuscitation Continuously monitor end-organ perfusion � Vasodilator therapy (e. g. , nitroglycerin, nitroprusside) Achieve/maintain MAP >65 mm Hg Nutrition is vital to decreasing morbidity from shock � Initiate parenteral nutrition if enteral nutrition contraindicated or fails to meet at least 80% of caloric requirements Copyright © 2014 by Mosby, an imprint of Elsevier Inc. � Monitor protein, nitrogen balance, BUN, glucose,
Collaborative Care - Cardiogenic Shock Restore blood flow to the myocardium by restoring the balance between O 2 supply and demand Thrombolytic therapy Angioplasty with stenting Emergency revascularization Valve replacement Hemodynamic monitoring Drug therapy (e. g. , diuretics to reduce preload) Circulatory assist devices (e. g. , intraaortic balloon pump, ventricular assist device) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Collaborative Care - Hypovolemic Shock Management focuses on stopping the loss of fluid and restoring the circulating volume Fluid replacement is calculated using a 3: 1 rule (3 m. L of isotonic crystalloid for every 1 m. L of estimated blood loss) Both crystalloids (such as normal saline solution) and colloids (like albumin) have a role in fluid resuscitation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Collaborative Care - Septic Shock Fluid replacement to restore perfusion � Hemodynamic monitoring Vasopressor drug therapy IV corticosteroids for patients who require vasopressor therapy Antibiotics (after cultures are obtained) Broad-spectrum antibiotics given first Specific antibiotics given based on the organism identified Glucose levels <180 mg/d. L Copyright © 2014 by Mosby, an imprint of Elsevier Inc. Stress ulcer prophylaxis with histamine (H 2)-receptor
Collaborative Care - Neurogenic Shock In spinal cord injury: spinal stability � Treatment of the hypotension and bradycardia with vasopressors and atropine � Fluids used cautiously as hypotension generally is not related to fluid loss � Monitor for hypothermia Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Collaborative Care - Anaphylactic Shock Epinephrine, diphenhydramine Maintain a patent airway � Nebulized bronchodilators � Aerosolized epinephrine � Endotracheal intubation or cricothyroidotomy may be necessary Aggressive fluid replacement IV corticosteroids if significant hypotension persists after 1– 2 hours of aggressive therapy Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Collaborative Care - Obstructive Shock Early recognition and treatment is primary strategy Mechanical decompression Radiation or removal of mass Decompressive laparotomy Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Evaluation Normal or baseline, ECG, BP, CVP, and PAWP Normal temperature Warm, dry skin Urinary output >0. 5 m. L/kg/hr (>30 m. L/hr) Normal RR and Sa. O 2 ≥ 90% Verbalization of fears, anxiety Copyright © 2014 by Mosby, an imprint of Elsevier Inc.