Management of Testicular Tumours Dr Sunil Shroff MS


- Slides: 39

Management of Testicular Tumours Dr. Sunil Shroff, MS, FRCS (UK ), D. Urol (Lond. ) Prof & HOD Sri. Ramachandra Medical College & Research Institution, Chennai
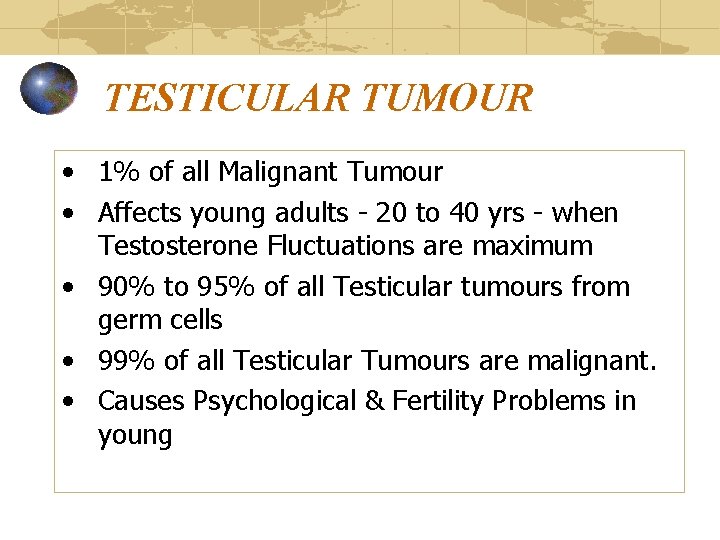
TESTICULAR TUMOUR • 1% of all Malignant Tumour • Affects young adults - 20 to 40 yrs - when Testosterone Fluctuations are maximum • 90% to 95% of all Testicular tumours from germ cells • 99% of all Testicular Tumours are malignant. • Causes Psychological & Fertility Problems in young
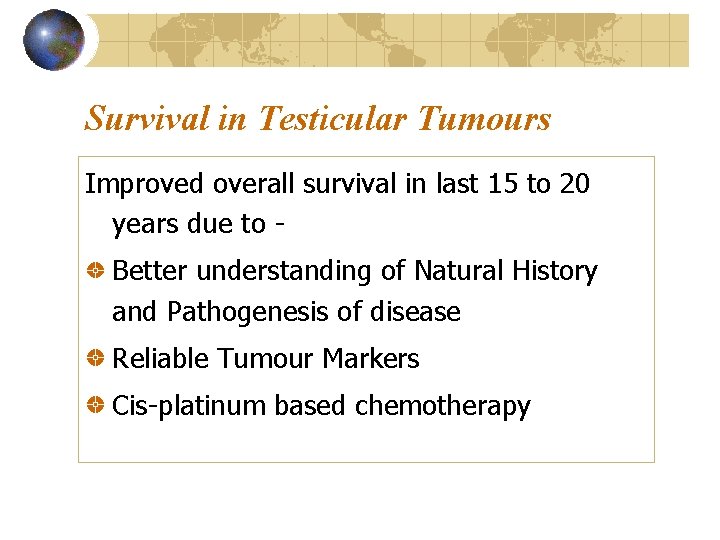
Survival in Testicular Tumours Improved overall survival in last 15 to 20 years due to Better understanding of Natural History and Pathogenesis of disease Reliable Tumour Markers Cis-platinum based chemotherapy
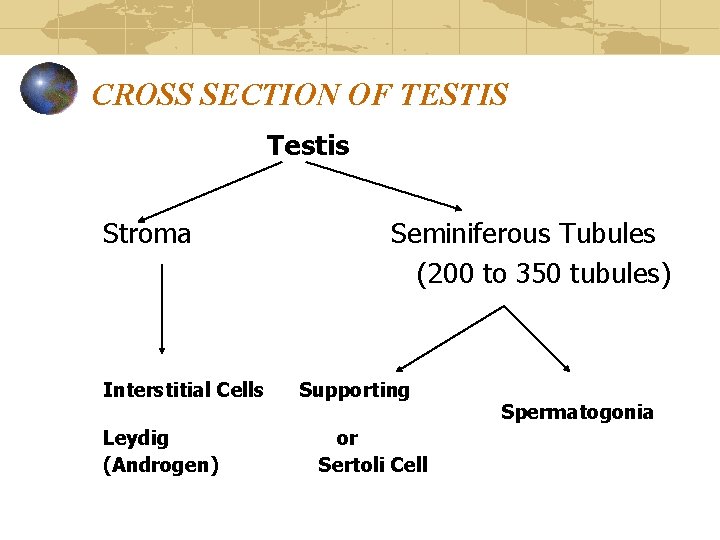
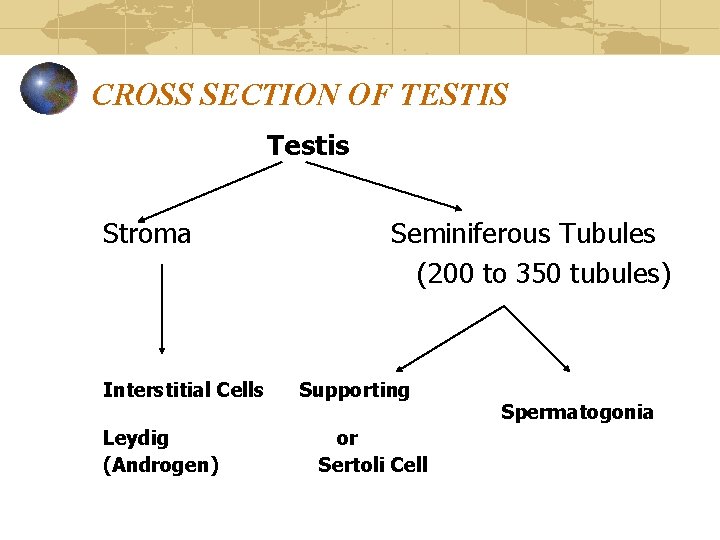
CROSS SECTION OF TESTIS Testis Stroma Interstitial Cells Leydig (Androgen) Seminiferous Tubules (200 to 350 tubules) Supporting or Sertoli Cell Spermatogonia
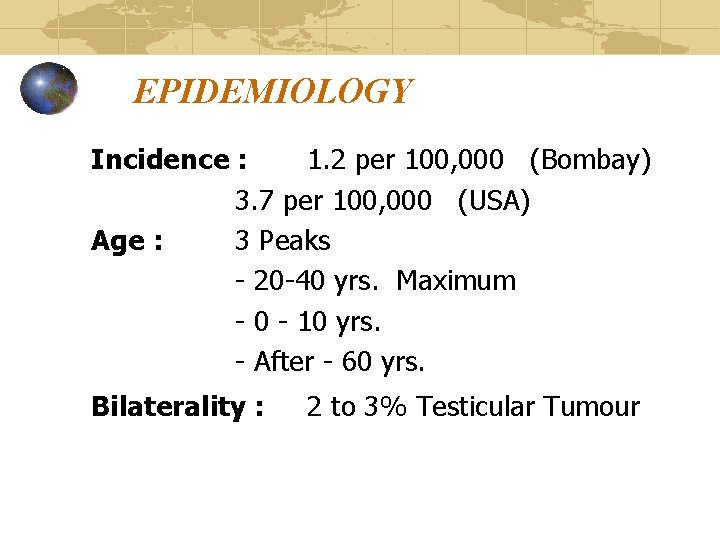
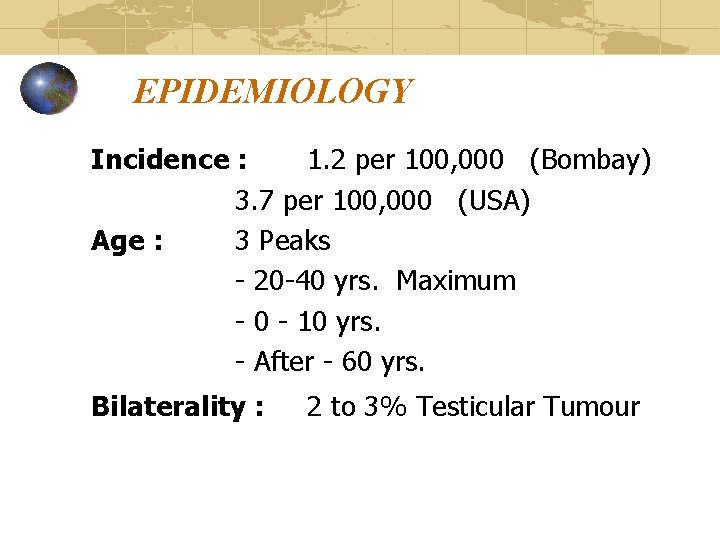
EPIDEMIOLOGY Incidence : 1. 2 per 100, 000 (Bombay) 3. 7 per 100, 000 (USA) Age : 3 Peaks - 20 -40 yrs. Maximum - 0 - 10 yrs. - After - 60 yrs. Bilaterality : 2 to 3% Testicular Tumour
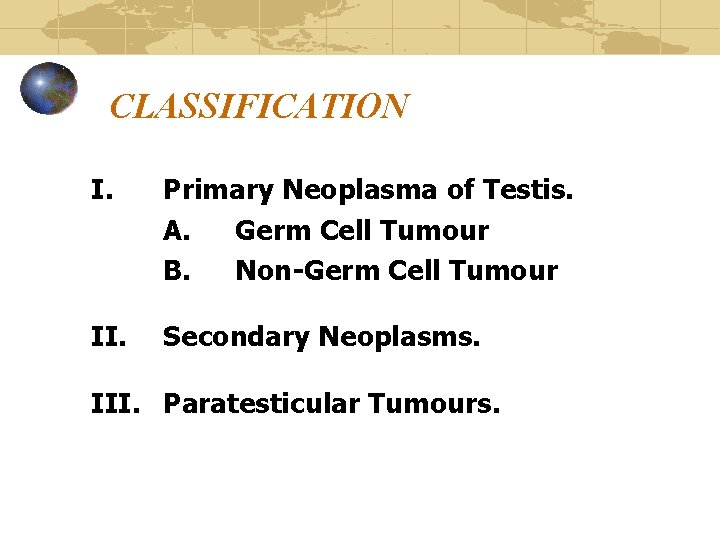
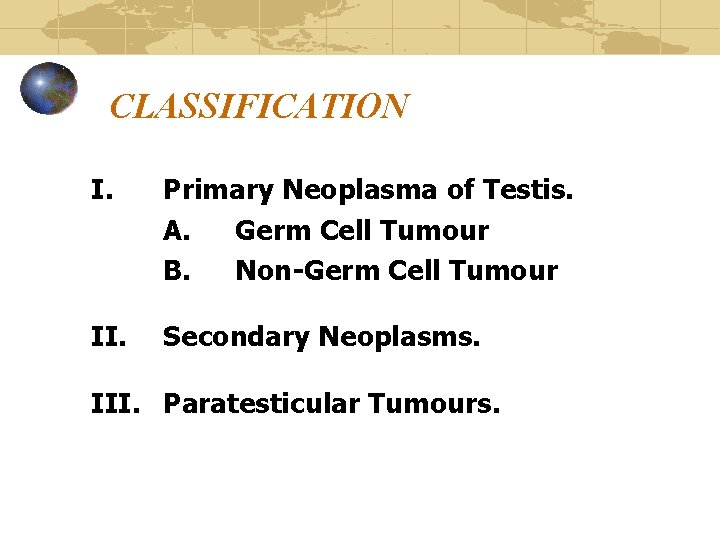
CLASSIFICATION I. Primary Neoplasma of Testis. A. Germ Cell Tumour B. Non-Germ Cell Tumour II. Secondary Neoplasms. III. Paratesticular Tumours.
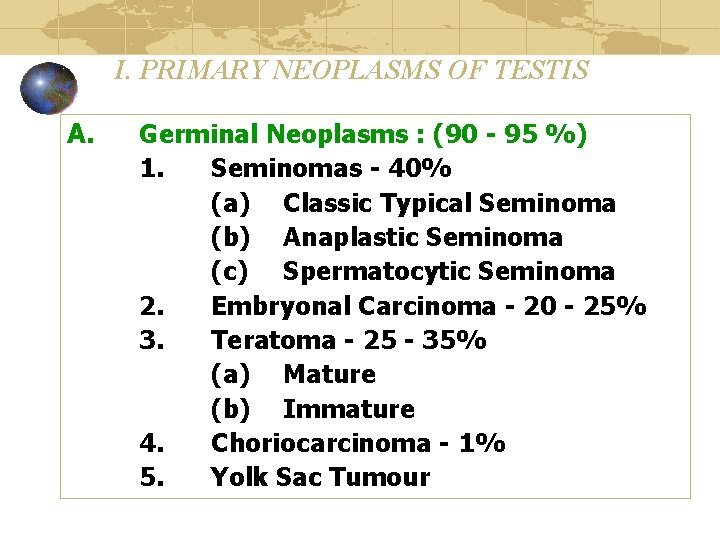
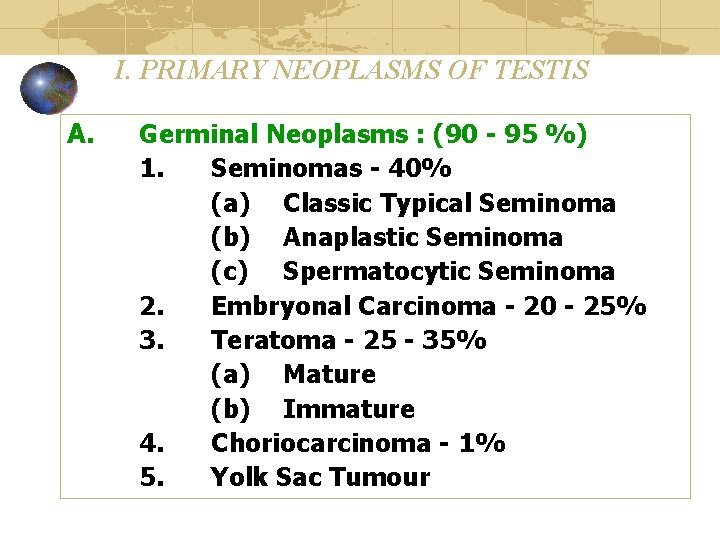
I. PRIMARY NEOPLASMS OF TESTIS A. Germinal Neoplasms : (90 - 95 %) 1. Seminomas - 40% (a) Classic Typical Seminoma (b) Anaplastic Seminoma (c) Spermatocytic Seminoma 2. Embryonal Carcinoma - 20 - 25% 3. Teratoma - 25 - 35% (a) Mature (b) Immature 4. Choriocarcinoma - 1% 5. Yolk Sac Tumour
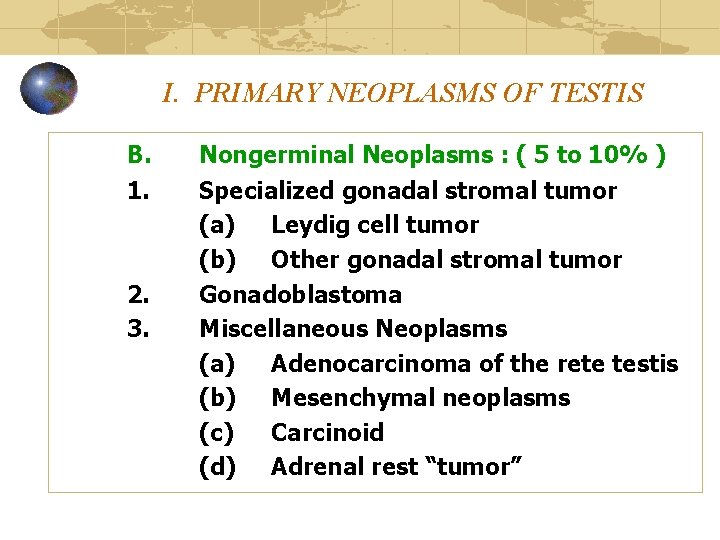
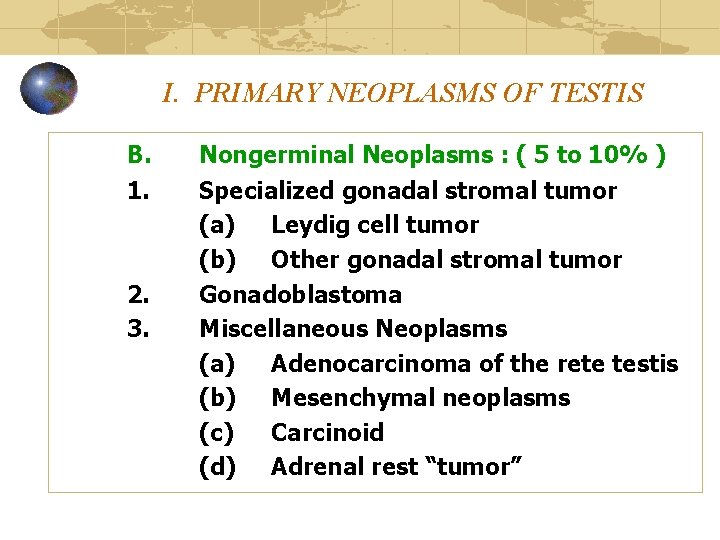
I. PRIMARY NEOPLASMS OF TESTIS B. 1. 2. 3. Nongerminal Neoplasms : ( 5 to 10% ) Specialized gonadal stromal tumor (a) Leydig cell tumor (b) Other gonadal stromal tumor Gonadoblastoma Miscellaneous Neoplasms (a) Adenocarcinoma of the rete testis (b) Mesenchymal neoplasms (c) Carcinoid (d) Adrenal rest “tumor”
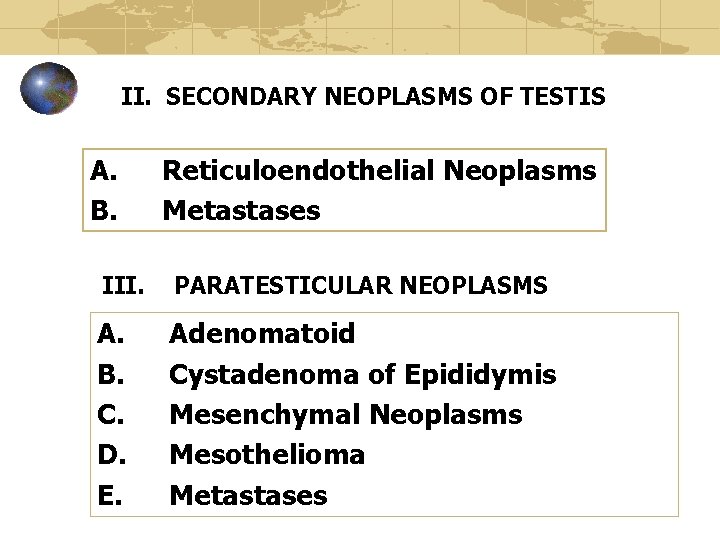
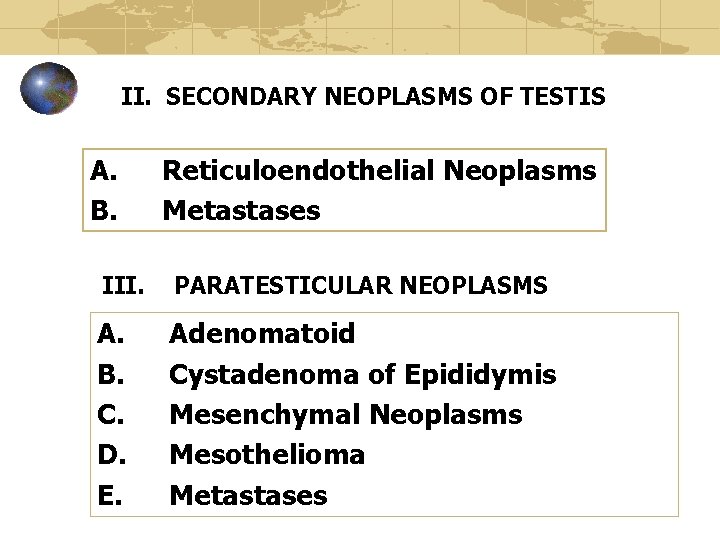
II. SECONDARY NEOPLASMS OF TESTIS A. B. Reticuloendothelial Neoplasms Metastases III. PARATESTICULAR NEOPLASMS A. B. C. D. E. Adenomatoid Cystadenoma of Epididymis Mesenchymal Neoplasms Mesothelioma Metastases
AETIOLOGY OF TESTICULAR TUMOUR 1. Cryptorchidism 2. Carcinoma in situ 3. Trauma 4. Atrophy
CRYPTORCHIDISM & TESTICULAR TUMOUR Risk of Carcinoma developing in undescended testis is 14 to 48 times the normal expected incidence
CRYPTORCHIDISM & TESTICULAR TUMOUR The cause for malignancy are as follows: Abnormal Germ Cell Morphology Elevated temperature in abdomen & Inguinal region as opposed to scrotum Endocrinal disturbances Gonadal dysgenesis
Testicular Tumour & Molecular Biology (Recent Advances) Molecular & Genetic Research may help Future patient with Testicular Tumours: • Earlier diagnosis • Identify Susceptible Individuals
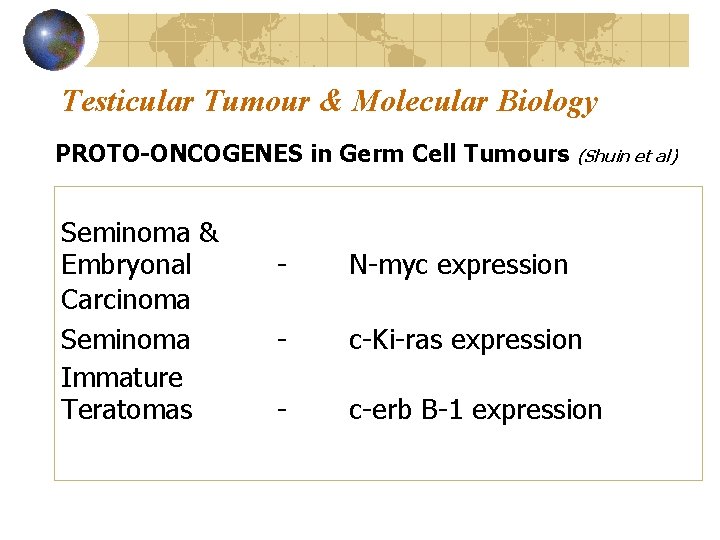
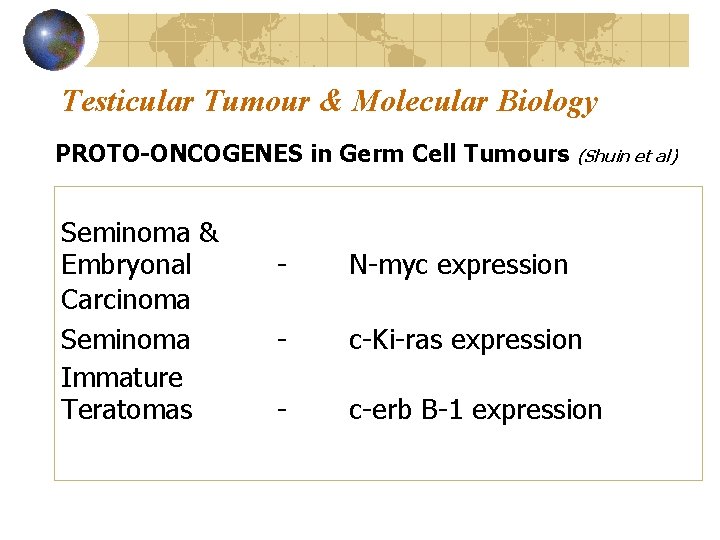
Testicular Tumour & Molecular Biology PROTO-ONCOGENES in Germ Cell Tumours (Shuin et al) Seminoma & Embryonal Carcinoma Seminoma Immature Teratomas - N-myc expression - c-Ki-ras expression - c-erb B-1 expression
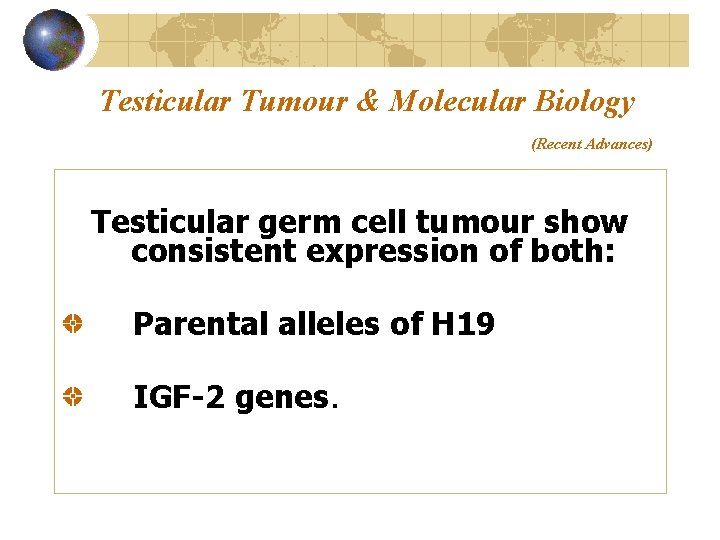
Testicular Tumour & Molecular Biology (Recent Advances) Testicular germ cell tumour show consistent expression of both: Parental alleles of H 19 IGF-2 genes.
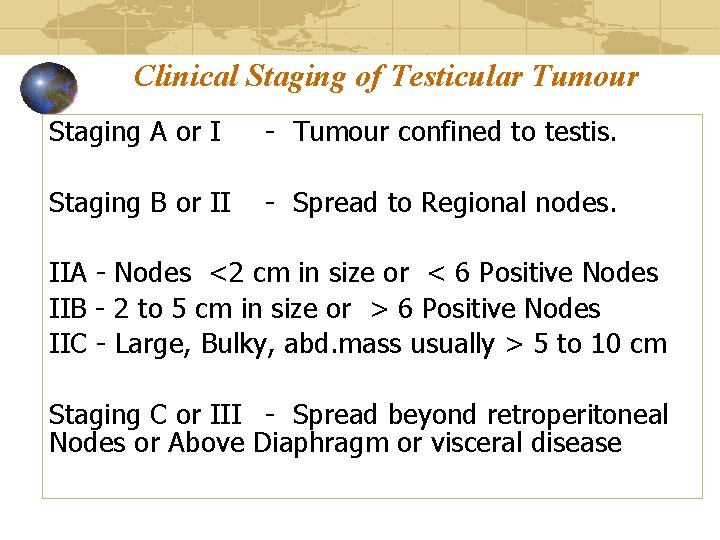
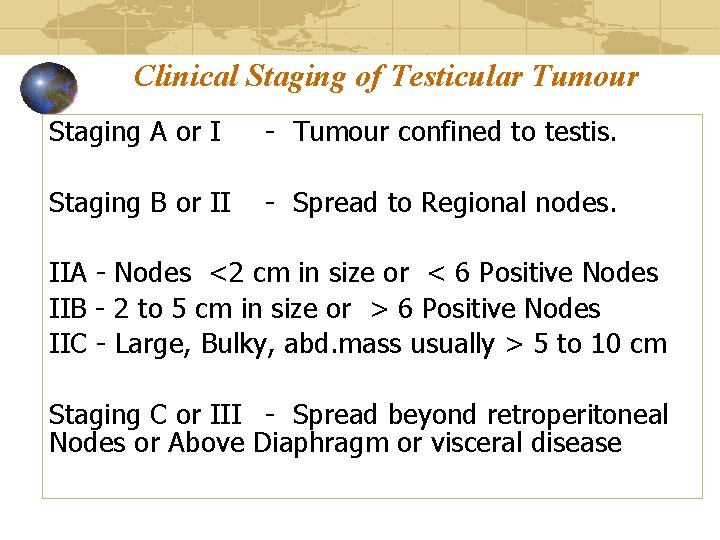
Clinical Staging of Testicular Tumour Staging A or I - Tumour confined to testis. Staging B or II - Spread to Regional nodes. IIA - Nodes <2 cm in size or < 6 Positive Nodes IIB - 2 to 5 cm in size or > 6 Positive Nodes IIC - Large, Bulky, abd. mass usually > 5 to 10 cm Staging C or III - Spread beyond retroperitoneal Nodes or Above Diaphragm or visceral disease
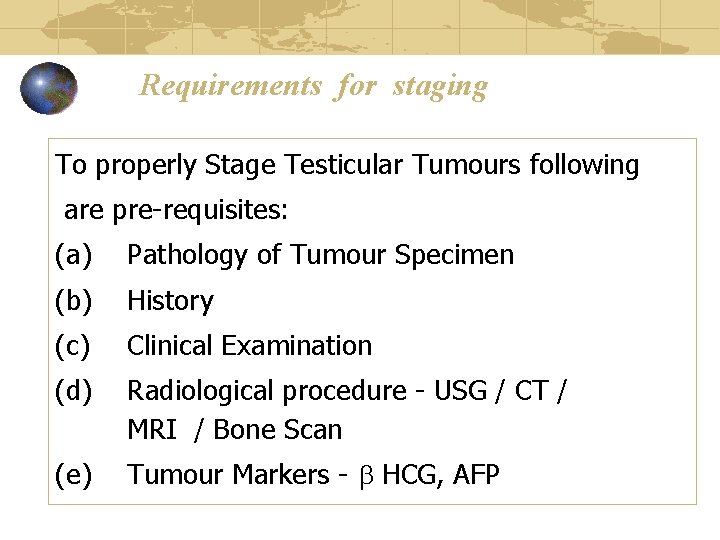
Requirements for staging To properly Stage Testicular Tumours following are pre-requisites: (a) Pathology of Tumour Specimen (b) History (c) Clinical Examination (d) Radiological procedure - USG / CT / MRI / Bone Scan (e) Tumour Markers - HCG, AFP
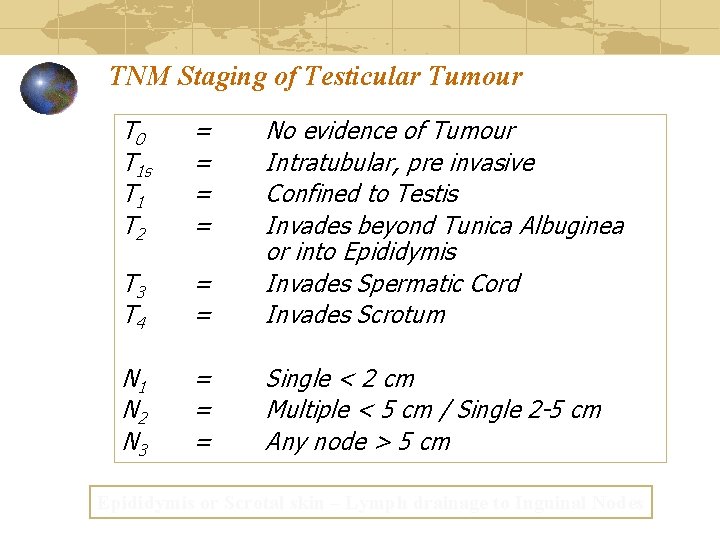
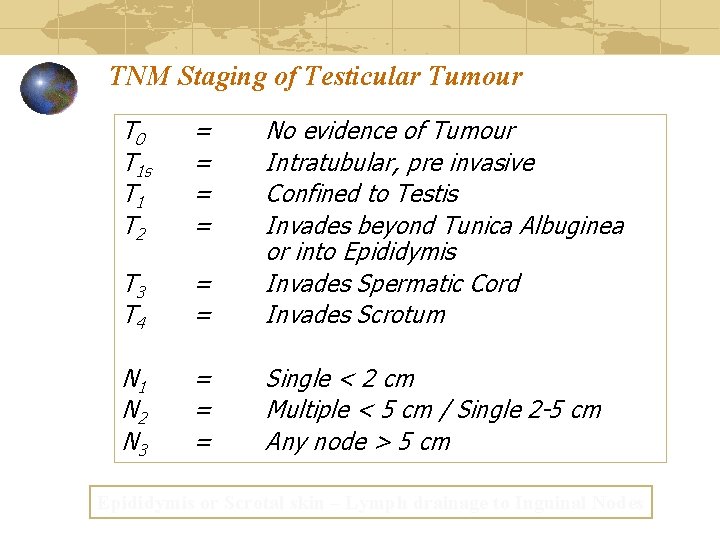
TNM Staging of Testicular Tumour T 0 T 1 s T 1 T 2 = = T 3 T 4 = = No evidence of Tumour Intratubular, pre invasive Confined to Testis Invades beyond Tunica Albuginea or into Epididymis Invades Spermatic Cord Invades Scrotum N 1 N 2 N 3 = = = Single < 2 cm Multiple < 5 cm / Single 2 -5 cm Any node > 5 cm Epididymis or Scrotal skin – Lymph drainage to Inguinal Nodes
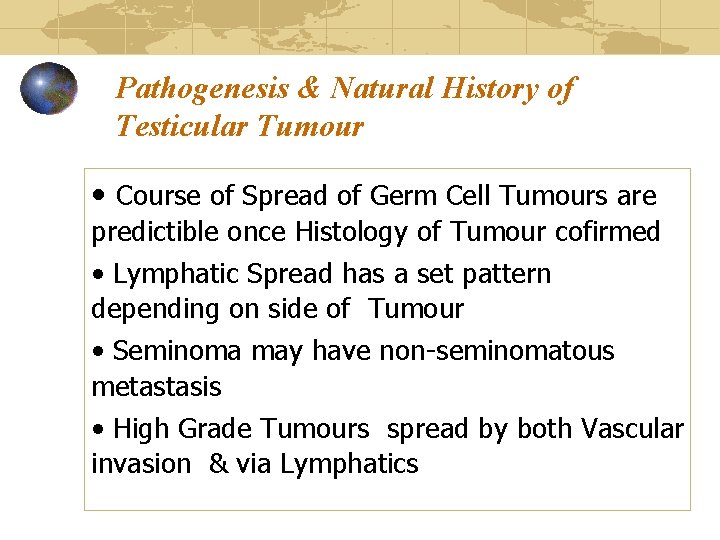
Pathogenesis & Natural History of Testicular Tumour • Course of Spread of Germ Cell Tumours are predictible once Histology of Tumour cofirmed • Lymphatic Spread has a set pattern depending on side of Tumour • Seminoma may have non-seminomatous metastasis • High Grade Tumours spread by both Vascular invasion & via Lymphatics
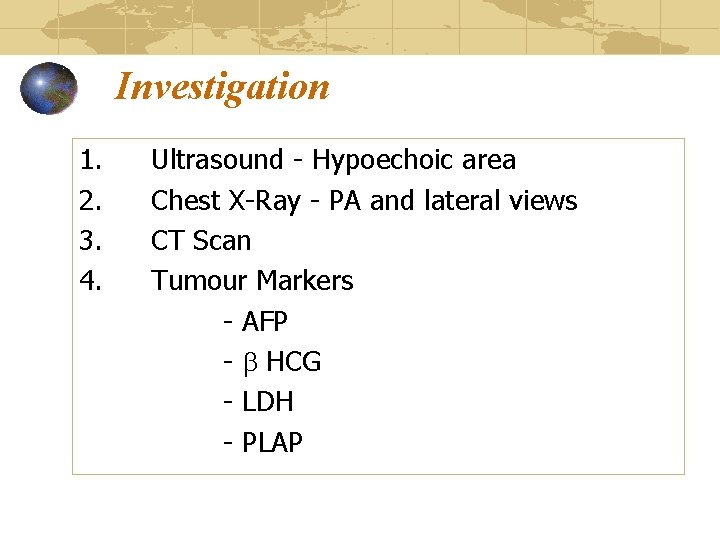
Investigation 1. 2. 3. 4. Ultrasound - Hypoechoic area Chest X-Ray - PA and lateral views CT Scan Tumour Markers - AFP - HCG - LDH - PLAP
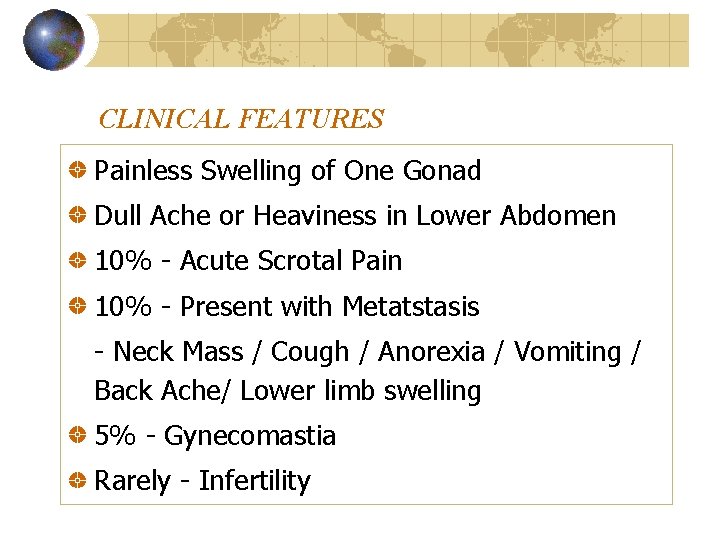
CLINICAL FEATURES Painless Swelling of One Gonad Dull Ache or Heaviness in Lower Abdomen 10% - Acute Scrotal Pain 10% - Present with Metatstasis - Neck Mass / Cough / Anorexia / Vomiting / Back Ache/ Lower limb swelling 5% - Gynecomastia Rarely - Infertility
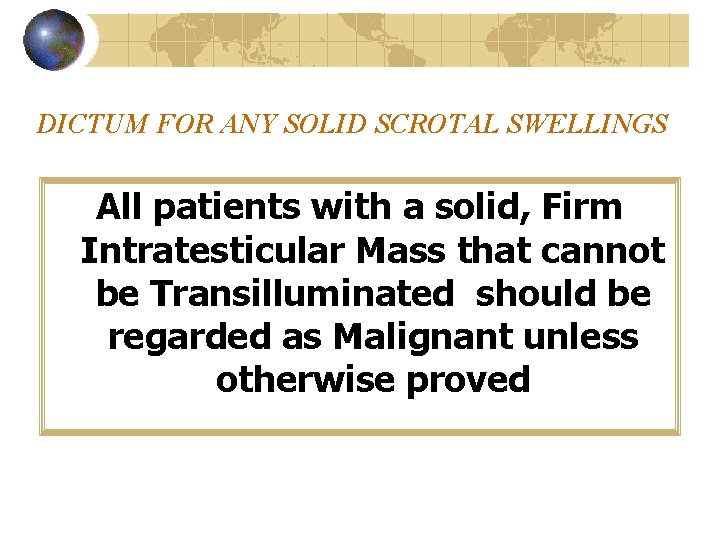
DICTUM FOR ANY SOLID SCROTAL SWELLINGS All patients with a solid, Firm Intratesticular Mass that cannot be Transilluminated should be regarded as Malignant unless otherwise proved
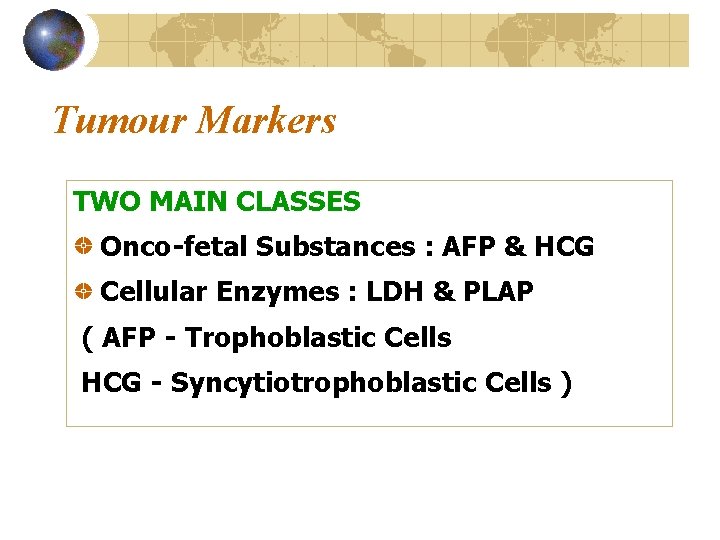
Tumour Markers TWO MAIN CLASSES Onco-fetal Substances : AFP & HCG Cellular Enzymes : LDH & PLAP ( AFP - Trophoblastic Cells HCG - Syncytiotrophoblastic Cells )
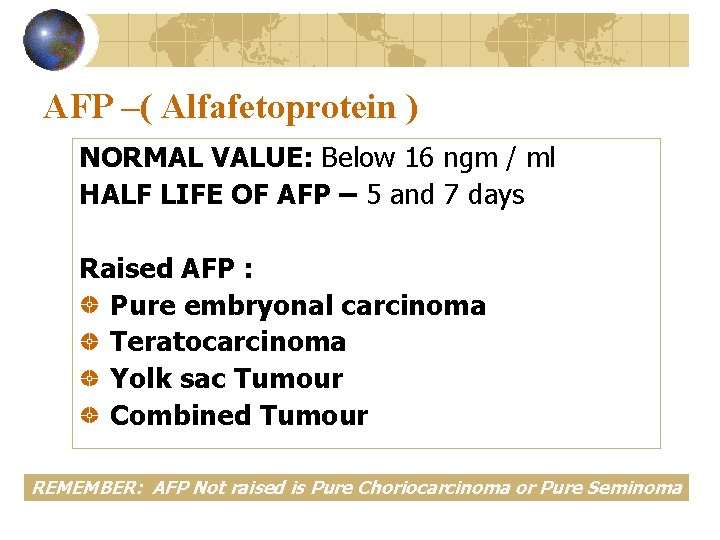
AFP –( Alfafetoprotein ) NORMAL VALUE: Below 16 ngm / ml HALF LIFE OF AFP – 5 and 7 days Raised AFP : Pure embryonal carcinoma Teratocarcinoma Yolk sac Tumour Combined Tumour REMEMBER: AFP Not raised is Pure Choriocarcinoma or Pure Seminoma
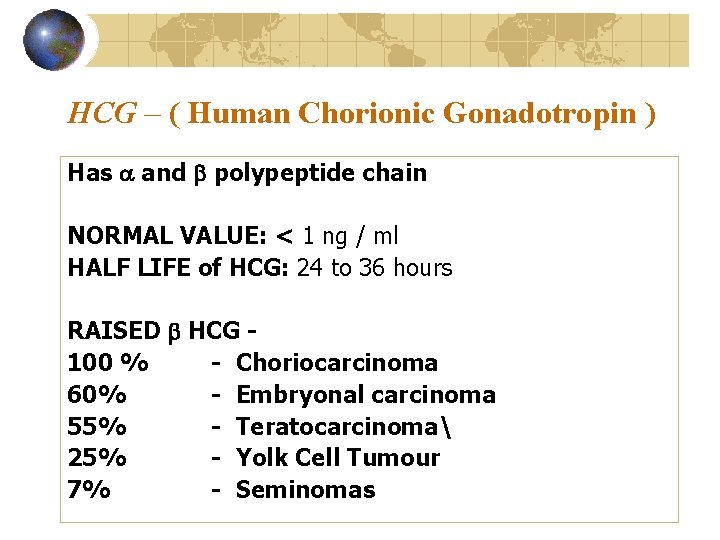
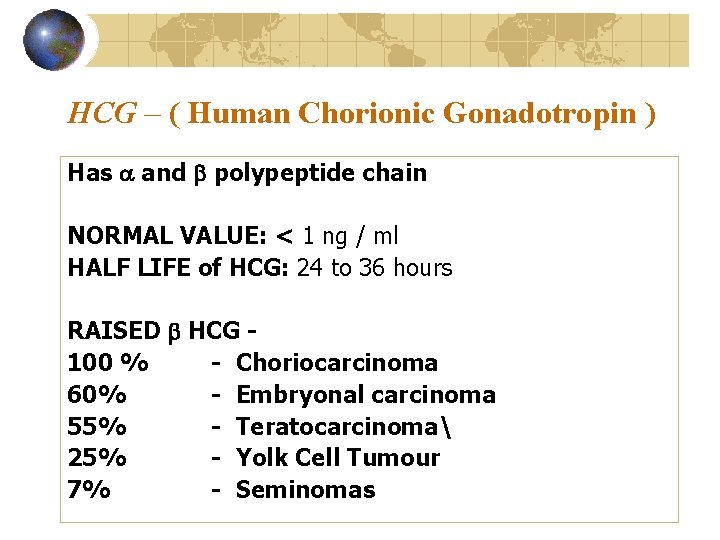
HCG – ( Human Chorionic Gonadotropin ) Has and polypeptide chain NORMAL VALUE: < 1 ng / ml HALF LIFE of HCG: 24 to 36 hours RAISED HCG 100 % - Choriocarcinoma 60% - Embryonal carcinoma 55% - Teratocarcinoma 25% - Yolk Cell Tumour 7% - Seminomas
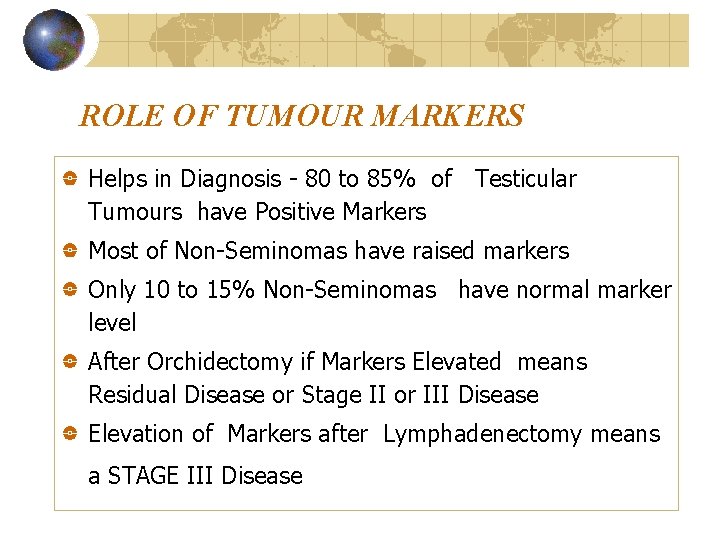
ROLE OF TUMOUR MARKERS Helps in Diagnosis - 80 to 85% of Testicular Tumours have Positive Markers Most of Non-Seminomas have raised markers Only 10 to 15% Non-Seminomas have normal marker level After Orchidectomy if Markers Elevated means Residual Disease or Stage II or III Disease Elevation of Markers after Lymphadenectomy means a STAGE III Disease
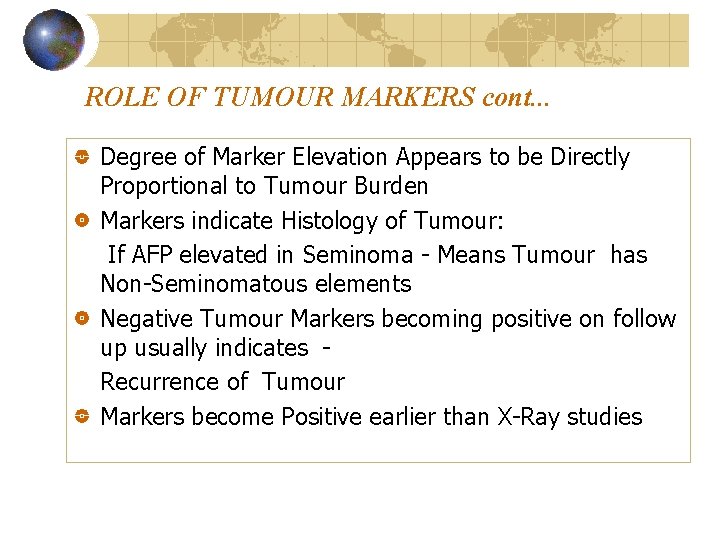
ROLE OF TUMOUR MARKERS cont. . . Degree of Marker Elevation Appears to be Directly Proportional to Tumour Burden Markers indicate Histology of Tumour: If AFP elevated in Seminoma - Means Tumour has Non-Seminomatous elements Negative Tumour Markers becoming positive on follow up usually indicates Recurrence of Tumour Markers become Positive earlier than X-Ray studies

PRINCIPLES OF TREATMENT Treatment should be aimed at one stage above the clinical stage Seminomas Radiotherapy. Radio-Sensitive. Treat with Non-Seminomas are Radio-Resistant and best treated by Surgery Advanced Disease or Metastasis - Responds well to Chemotherapy
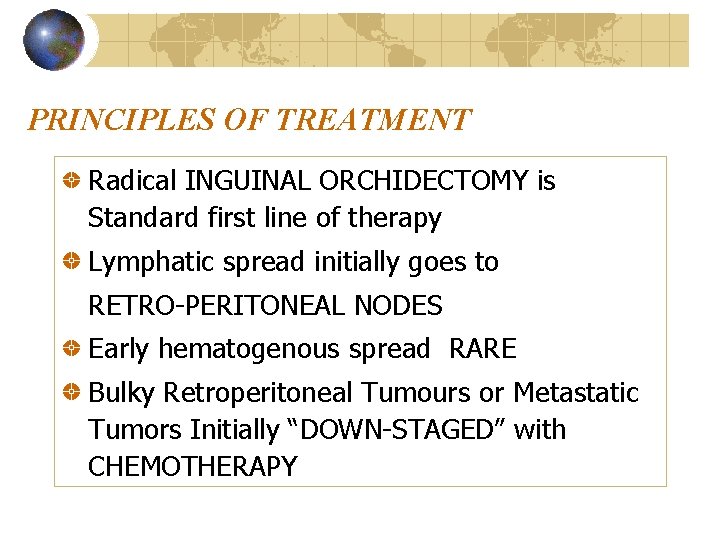
PRINCIPLES OF TREATMENT Radical INGUINAL ORCHIDECTOMY is Standard first line of therapy Lymphatic spread initially goes to RETRO-PERITONEAL NODES Early hematogenous spread RARE Bulky Retroperitoneal Tumours or Metastatic Tumors Initially “DOWN-STAGED” with CHEMOTHERAPY
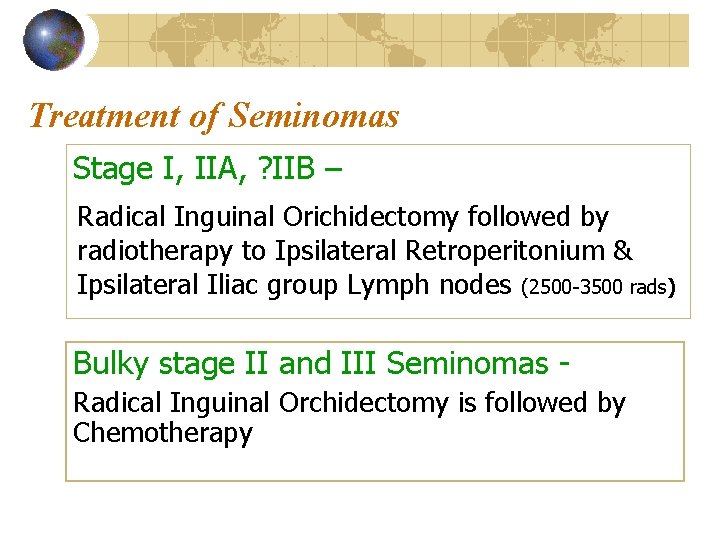
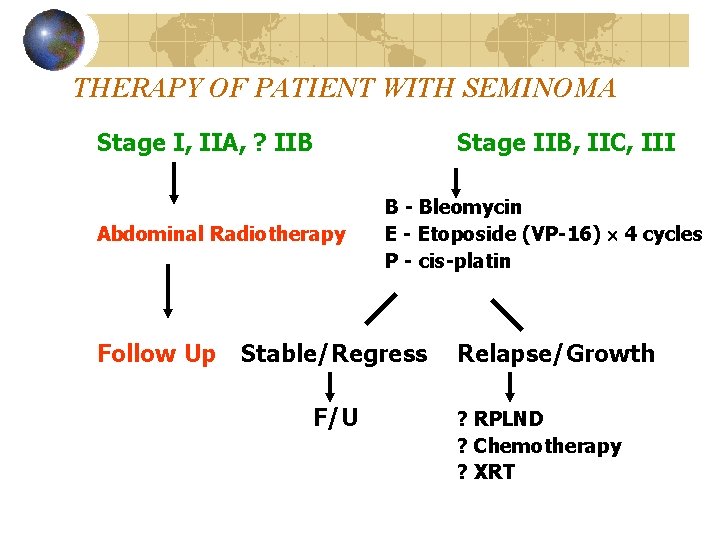
Treatment of Seminomas Stage I, IIA, ? IIB – Radical Inguinal Orichidectomy followed by radiotherapy to Ipsilateral Retroperitonium & Ipsilateral Iliac group Lymph nodes (2500 -3500 rads) Bulky stage II and III Seminomas Radical Inguinal Orchidectomy is followed by Chemotherapy
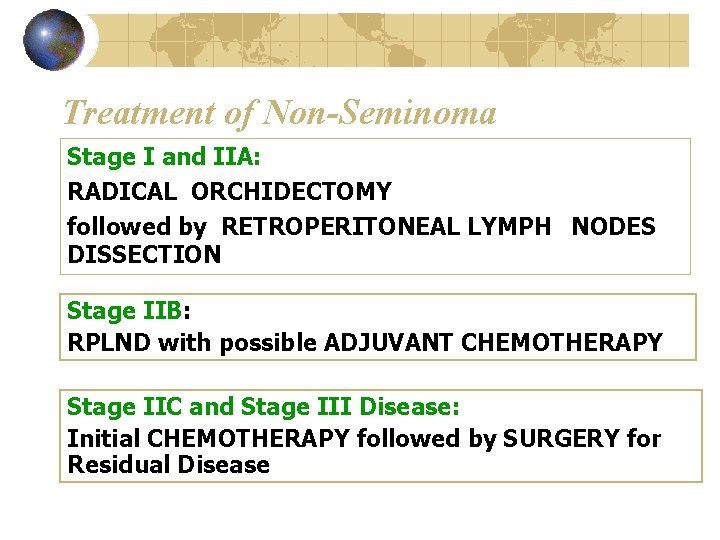
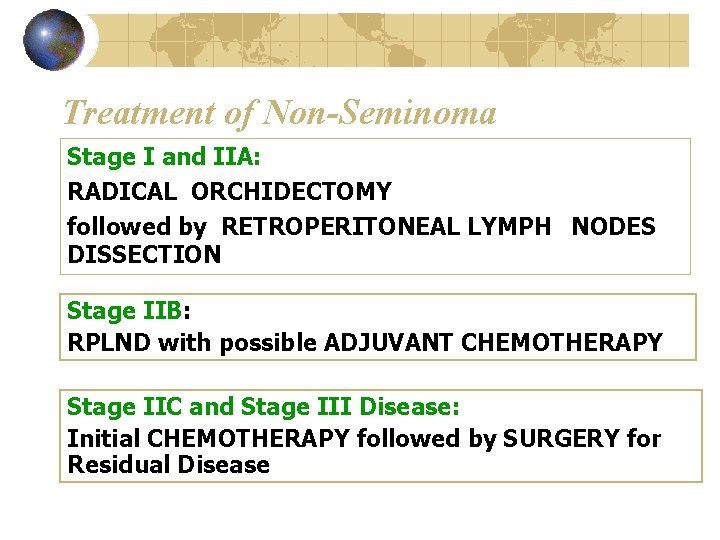
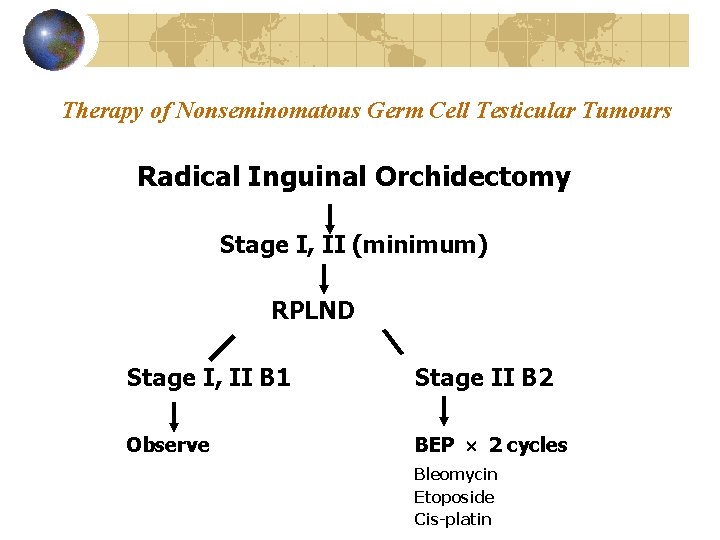
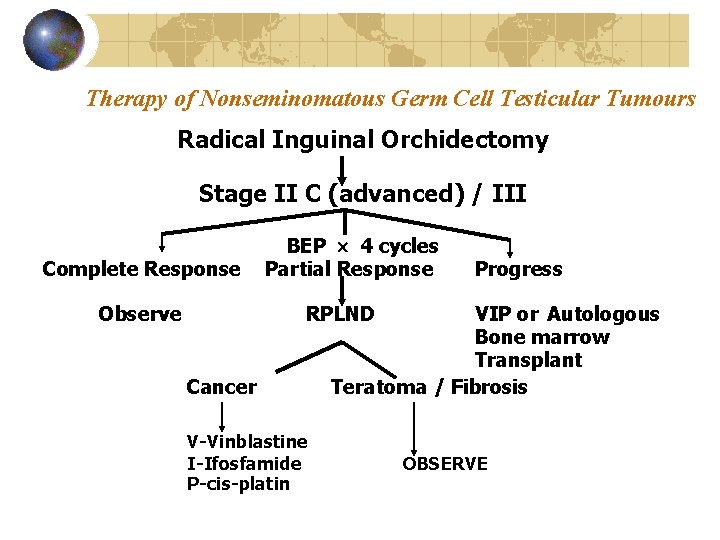
Treatment of Non-Seminoma Stage I and IIA: RADICAL ORCHIDECTOMY followed by RETROPERITONEAL LYMPH NODES DISSECTION Stage IIB: RPLND with possible ADJUVANT CHEMOTHERAPY Stage IIC and Stage III Disease: Initial CHEMOTHERAPY followed by SURGERY for Residual Disease
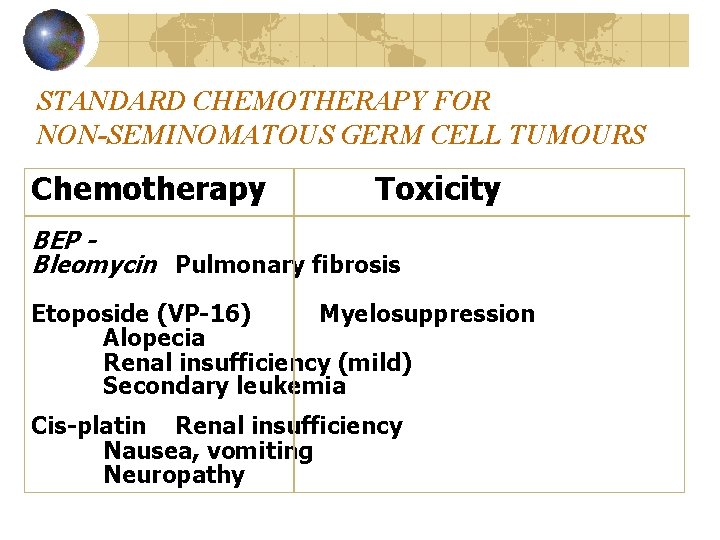
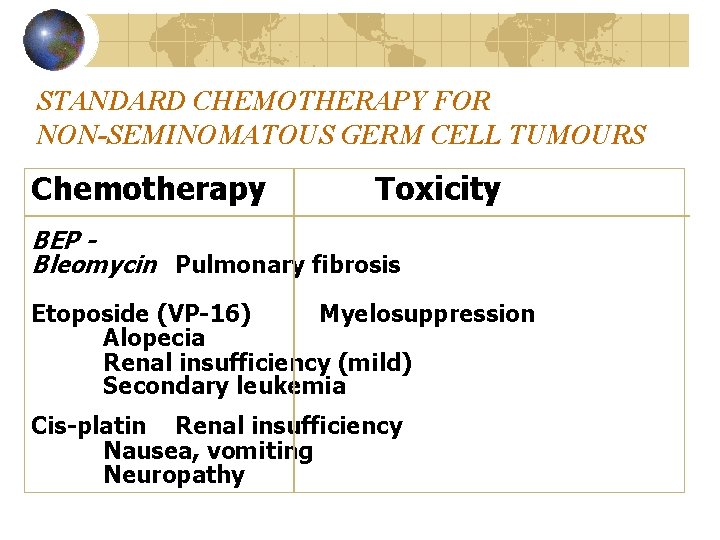
STANDARD CHEMOTHERAPY FOR NON-SEMINOMATOUS GERM CELL TUMOURS Chemotherapy Toxicity BEP Bleomycin Pulmonary fibrosis Etoposide (VP-16) Myelosuppression Alopecia Renal insufficiency (mild) Secondary leukemia Cis-platin Renal insufficiency Nausea, vomiting Neuropathy
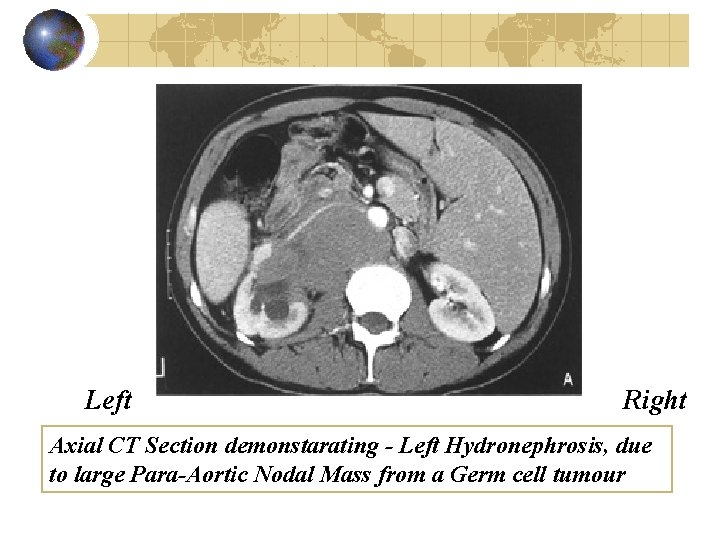
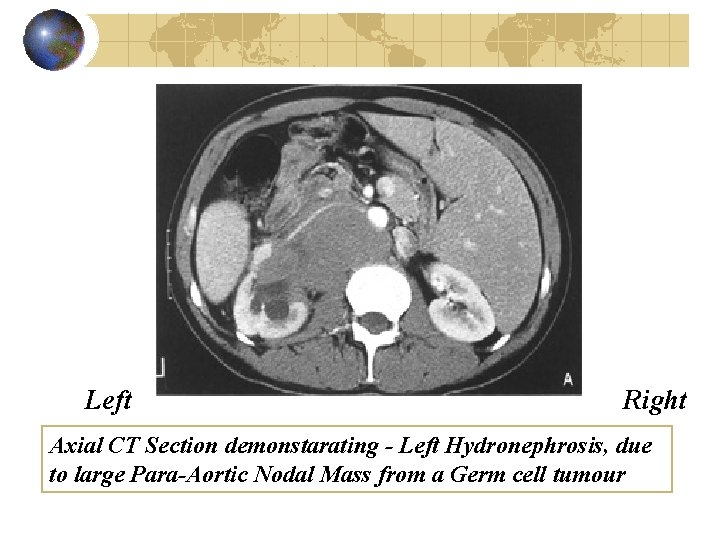
Left Right Axial CT Section demonstarating - Left Hydronephrosis, due to large Para-Aortic Nodal Mass from a Germ cell tumour
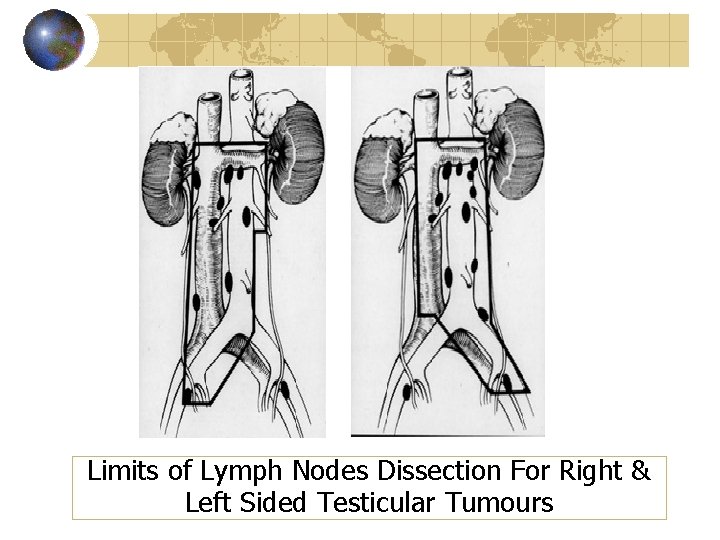
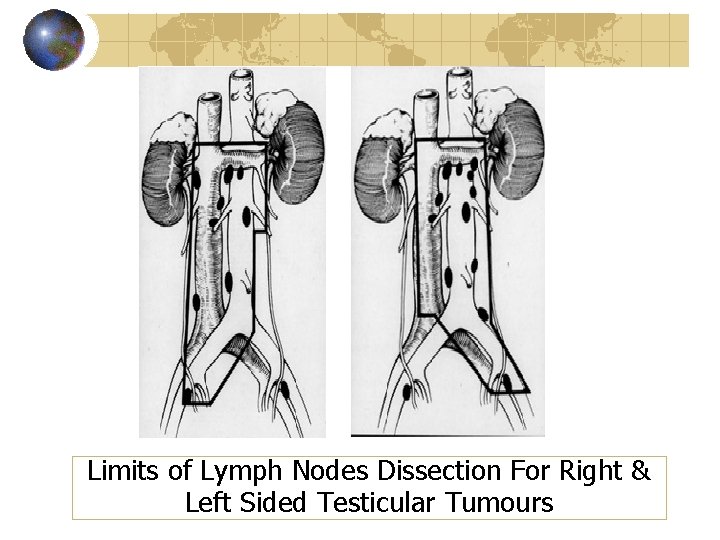
Limits of Lymph Nodes Dissection For Right & Left Sided Testicular Tumours
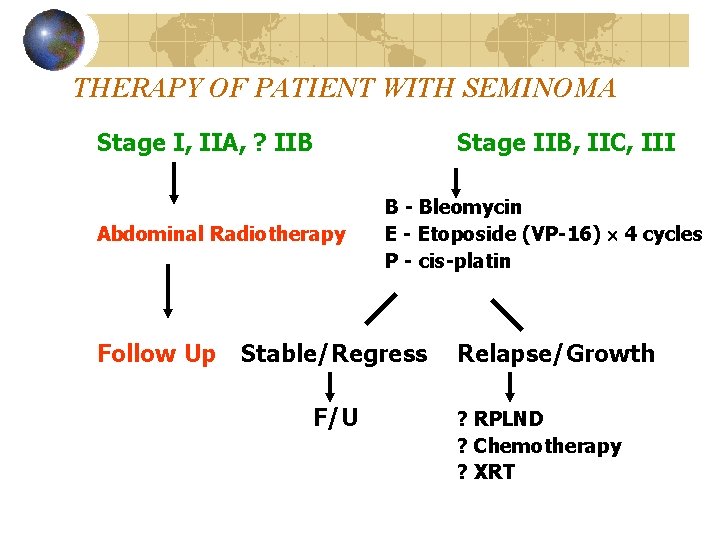
THERAPY OF PATIENT WITH SEMINOMA Stage I, IIA, ? IIB Abdominal Radiotherapy Follow Up Stage IIB, IIC, III B - Bleomycin E - Etoposide (VP-16) 4 cycles P - cis-platin Stable/Regress F/U Relapse/Growth ? RPLND ? Chemotherapy ? XRT
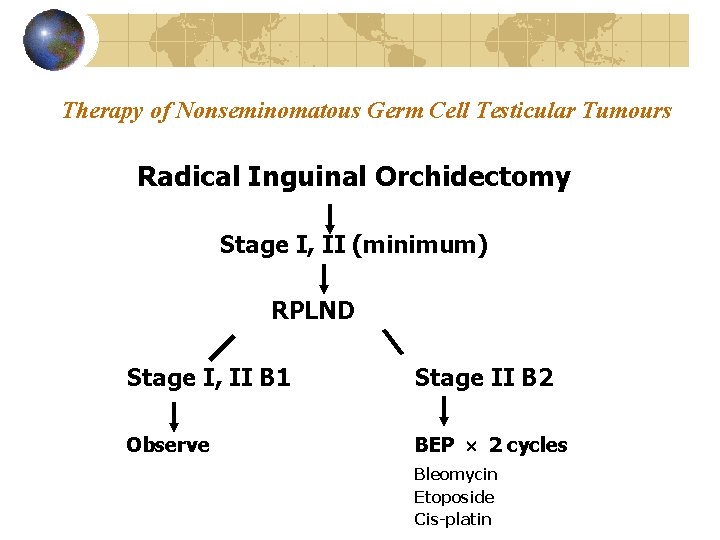
Therapy of Nonseminomatous Germ Cell Testicular Tumours Radical Inguinal Orchidectomy Stage I, II (minimum) RPLND Stage I, II B 1 Stage II B 2 Observe BEP 2 cycles Bleomycin Etoposide Cis-platin
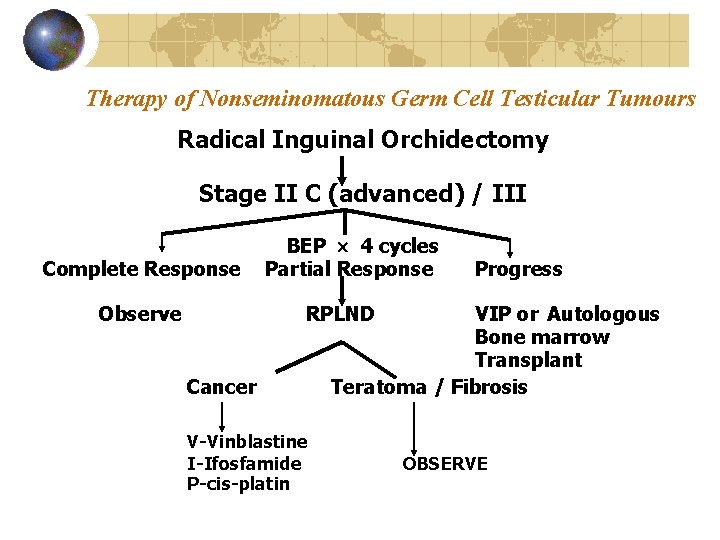
Therapy of Nonseminomatous Germ Cell Testicular Tumours Radical Inguinal Orchidectomy Stage II C (advanced) / III Complete Response Observe BEP 4 cycles Partial Response Progress RPLND Cancer V-Vinblastine I-Ifosfamide P-cis-platin VIP or Autologous Bone marrow Transplant Teratoma / Fibrosis OBSERVE
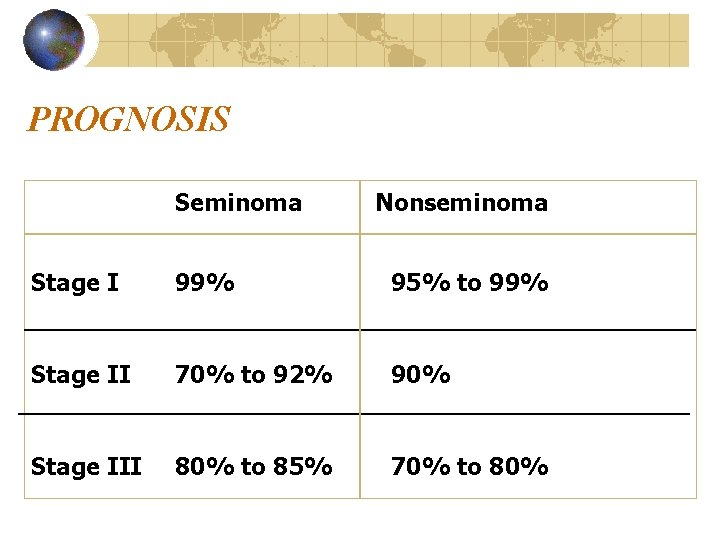
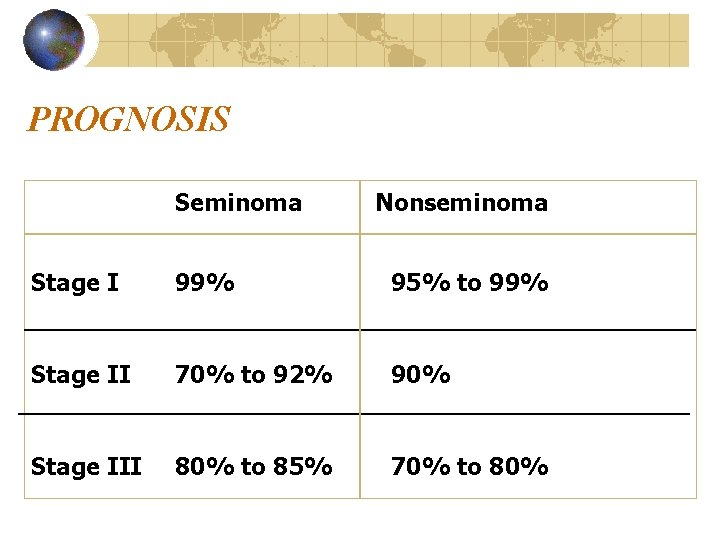
PROGNOSIS Seminoma Nonseminoma Stage I 99% 95% to 99% Stage II 70% to 92% 90% Stage III 80% to 85% 70% to 80%
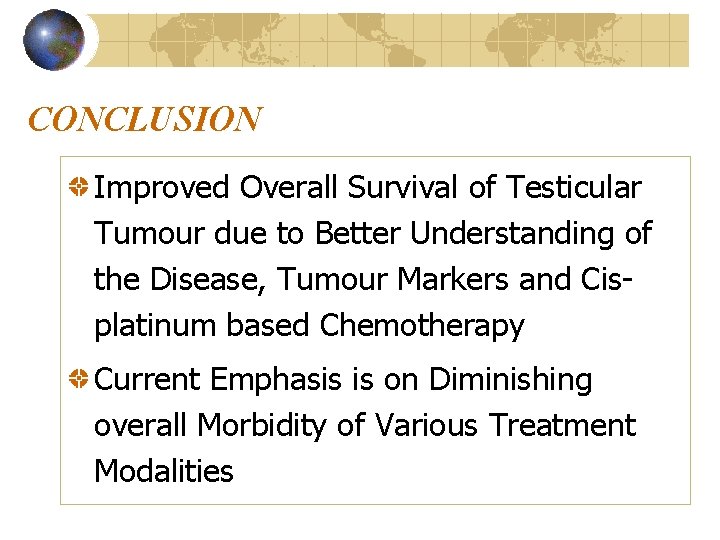
CONCLUSION Improved Overall Survival of Testicular Tumour due to Better Understanding of the Disease, Tumour Markers and Cisplatinum based Chemotherapy Current Emphasis is on Diminishing overall Morbidity of Various Treatment Modalities