Management of Surgical Emergencies Part 1 Critical Care



- Slides: 24
Management of Surgical Emergencies Part 1 : Critical Care Chest Trauma causes of Breathlessness and Emergency Management Copyright UKCS #284661815
Learning Outcomes 1. Primary Survey 2. “B” - Breathing with ventilatory support 3. Life threatening breathing problems & Specific injuries 4. Features, signs and treatment
Primary Assessment (Survey) Rapidly identify immediate life threatening and reversible injuries • Airway, Breathing, Circulation, Disability • Treat problems as they are identified • Systematic • Repeatable
Primary Assessment: • Expose (remember the back) • Look, feel, percussion, auscultation (remember the back if possible) • Treat life threatening problems • Reassess following intervention • Vital Signs, oximetry and CXR (if available)
Primary Assessment: Life-threatening injuries: Penetrating chest injury -v. Blunt chest injury Airway Obstruction Tension Pneumothorax Open Pneumothorax Massive Haemothorax Flail Chest Cardiac Tamponade ATOMi. C
Primary Assessment: Potentially life-threatening injuries to look out for: (a) Penetrating chest injury: • Tension pneumothorax • Massive haemothorax • Cardiac tamponade • Open pneumothorax SIGNS MANAGEMENT
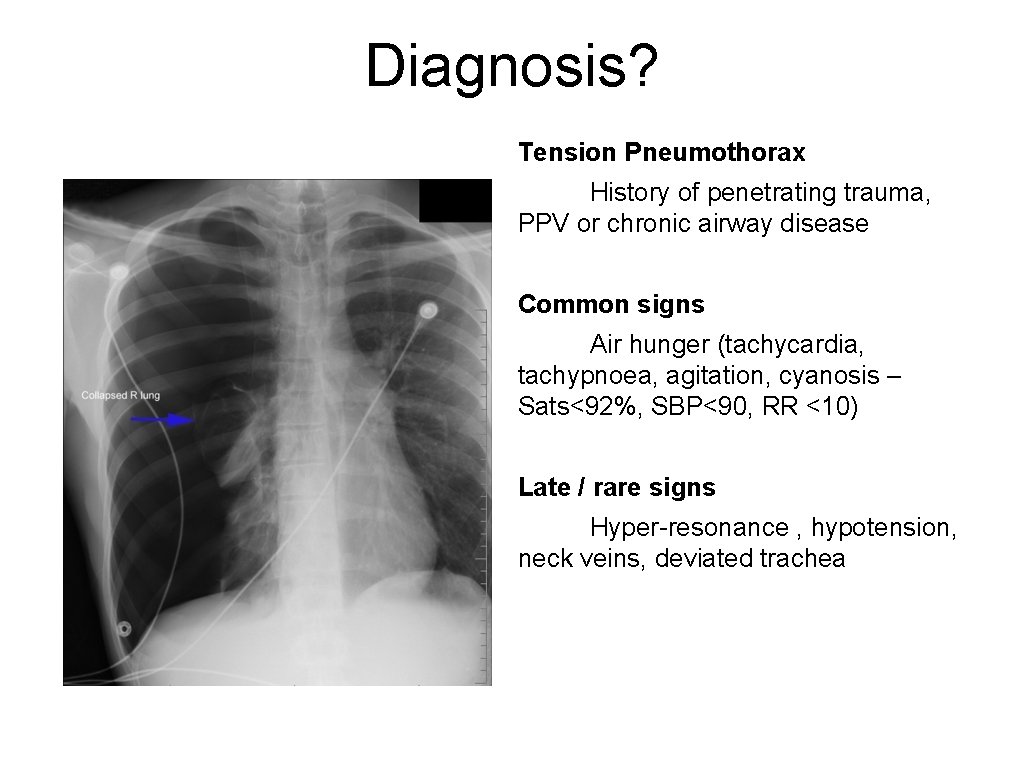
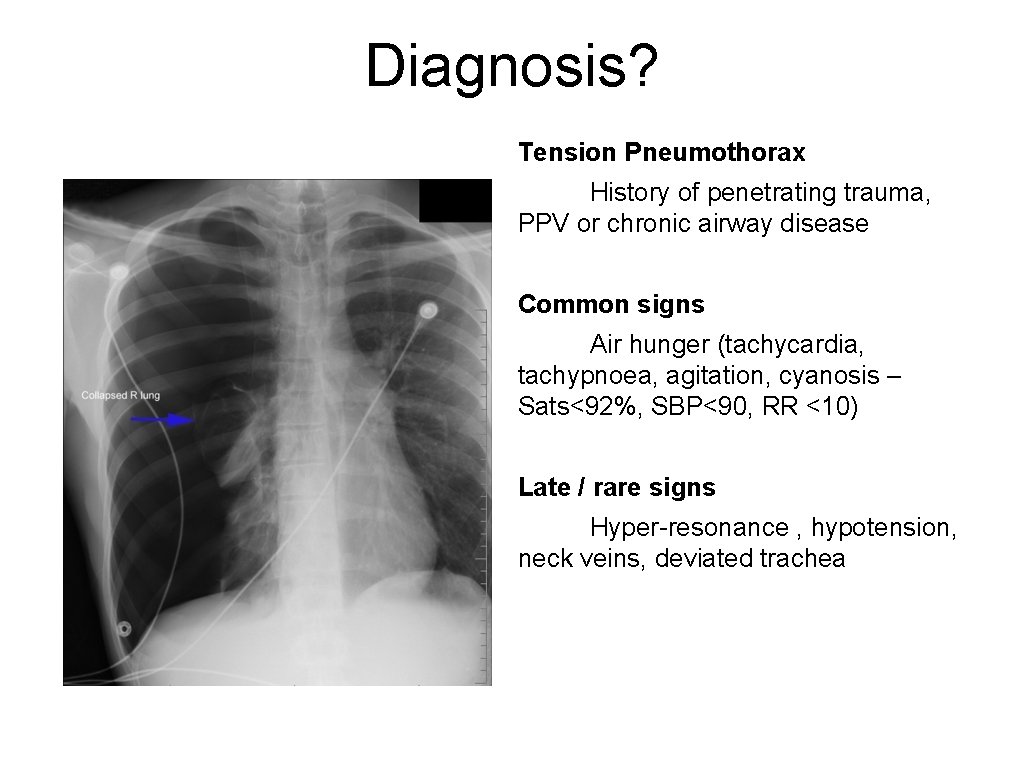
Diagnosis? Tension Pneumothorax History of penetrating trauma, PPV or chronic airway disease Common signs Air hunger (tachycardia, tachypnoea, agitation, cyanosis – Sats<92%, SBP<90, RR <10) Late / rare signs Hyper-resonance , hypotension, neck veins, deviated trachea
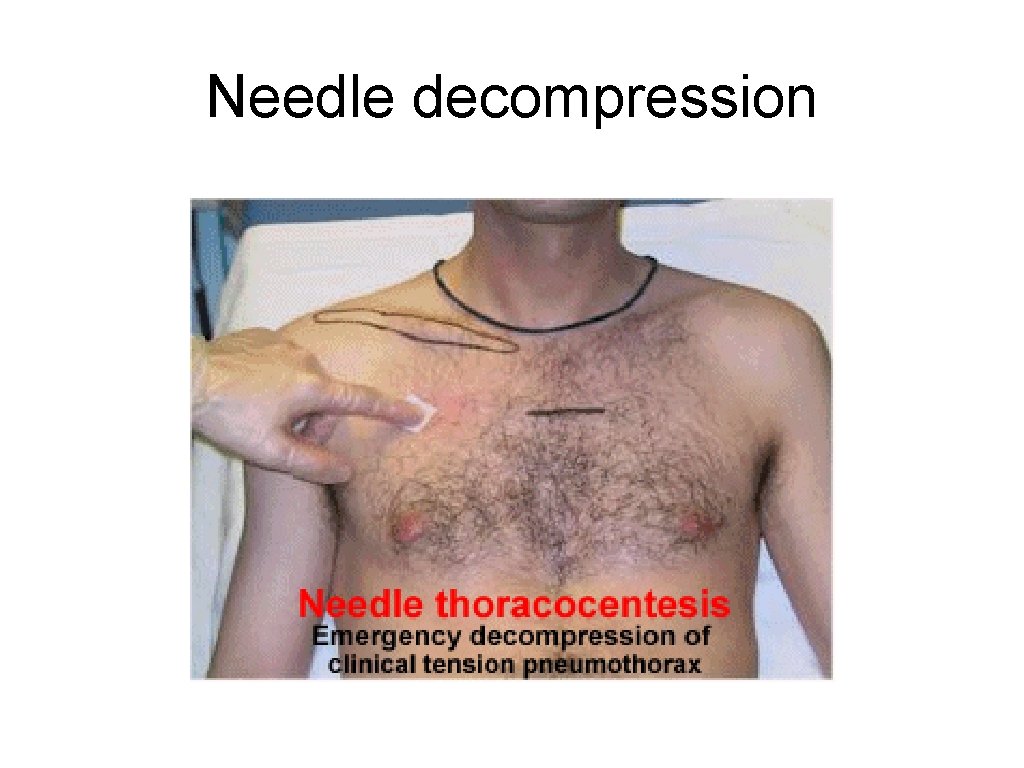
Tension pneumothorax • Clinical diagnosis • X-ray not necessary • Management – Immediate Needle Decompression • How, where • Intercostal drain
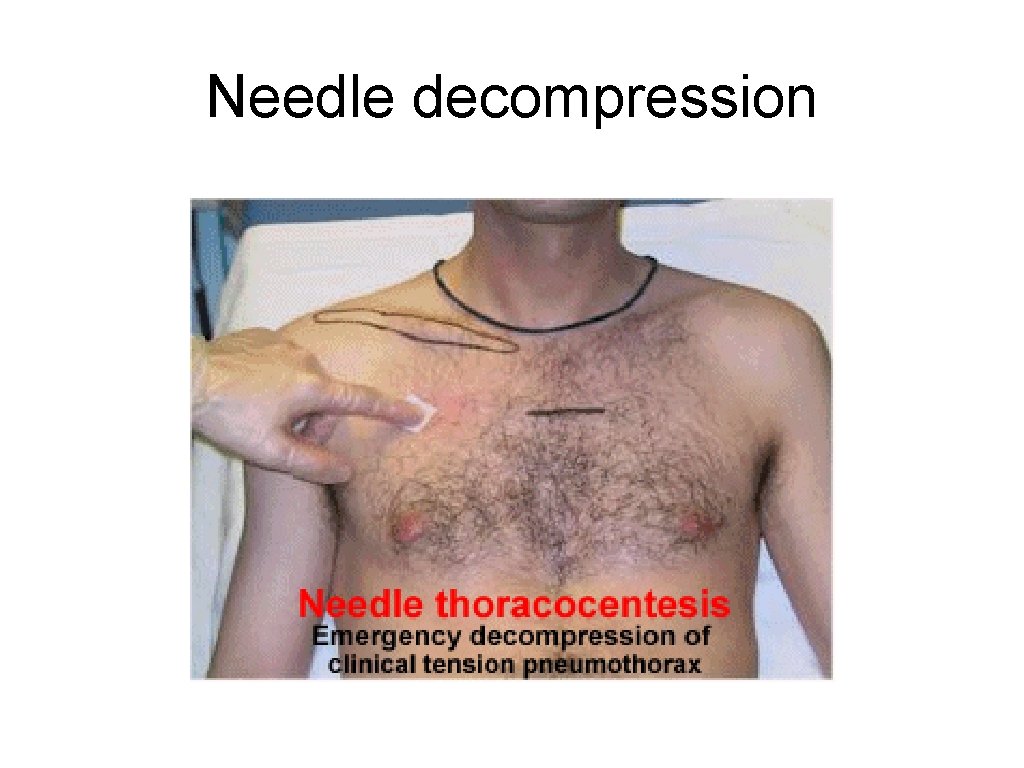
Needle decompression
Needle decompression
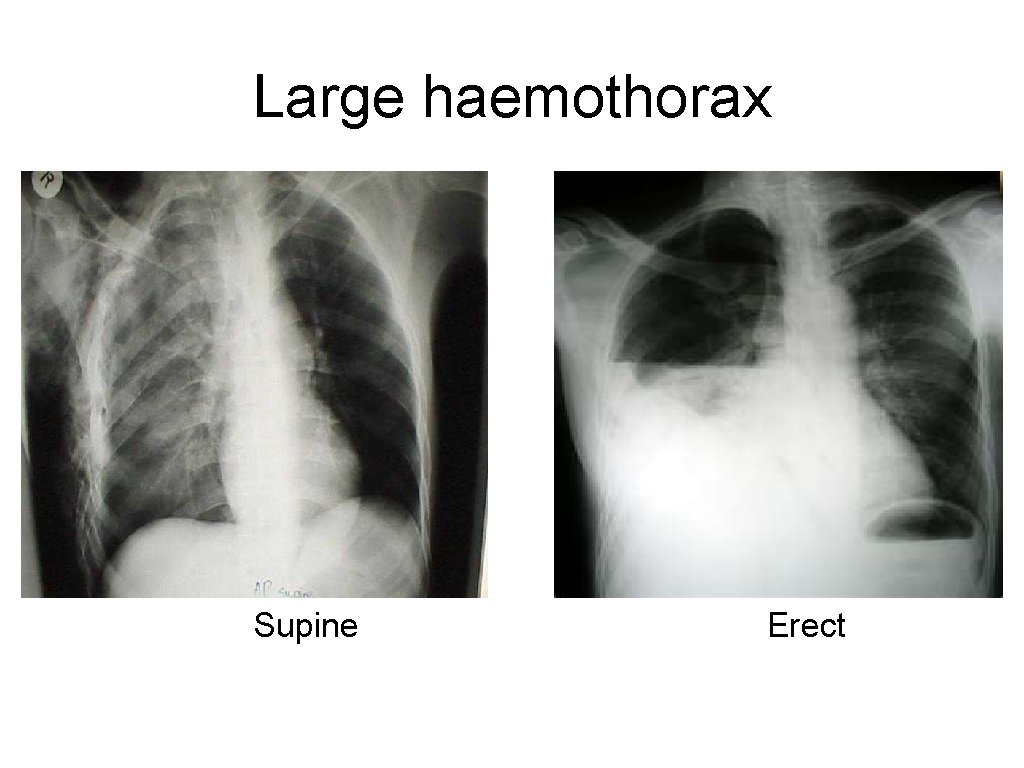
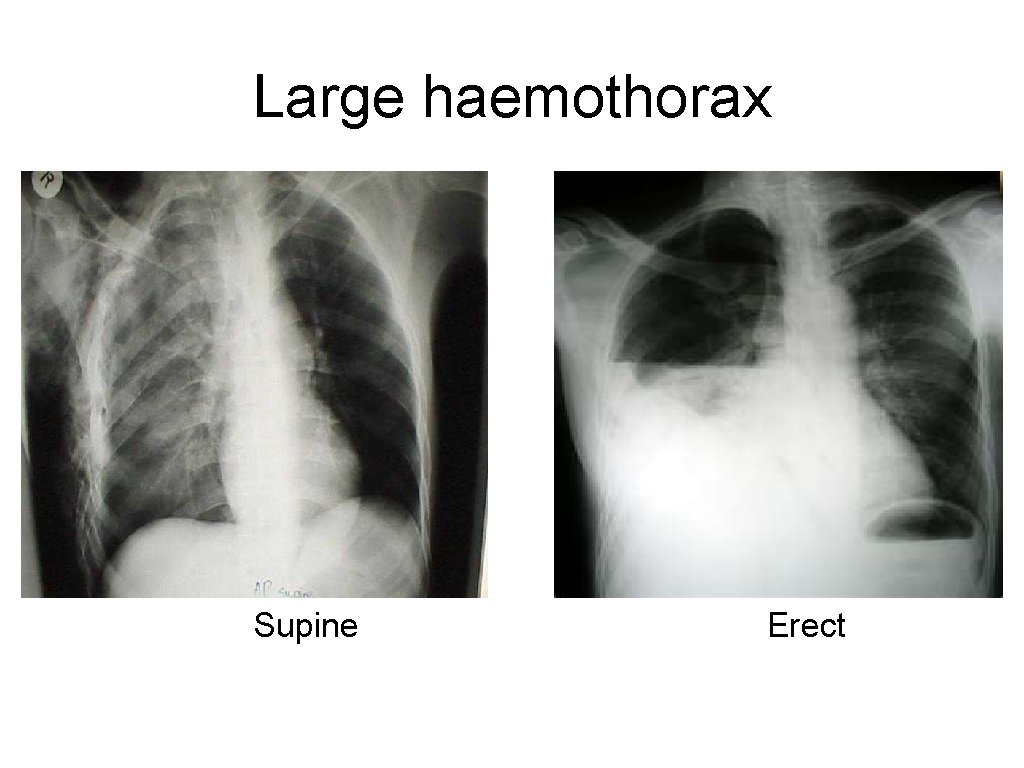
Large haemothorax Supine Erect
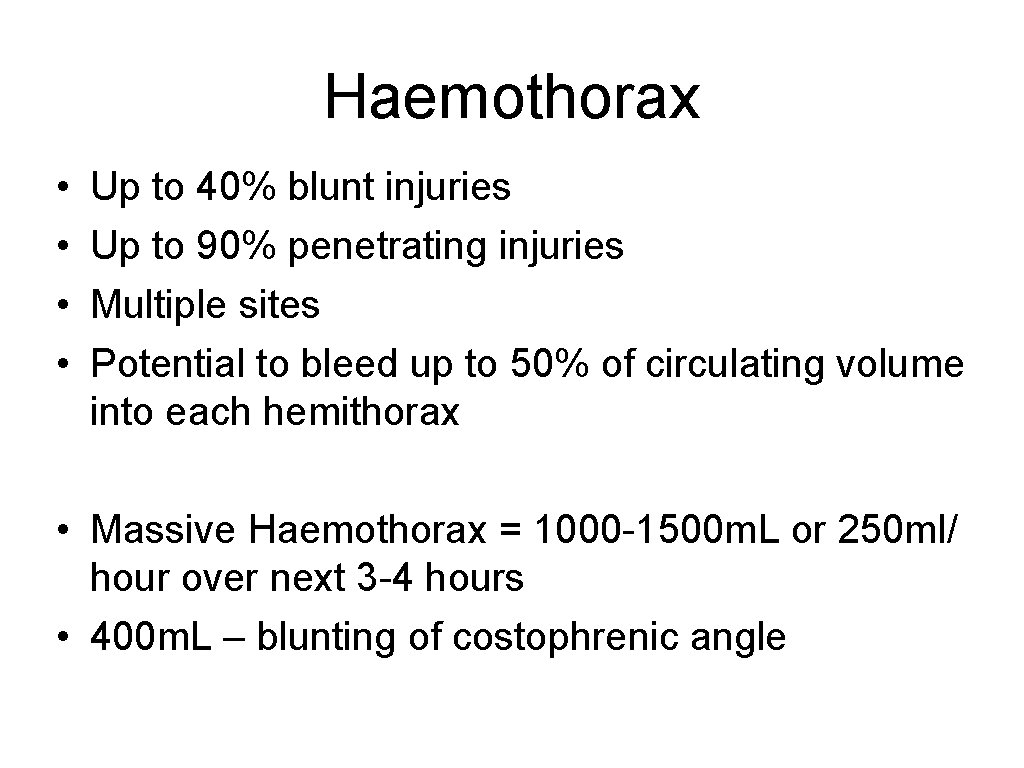
Haemothorax • • Up to 40% blunt injuries Up to 90% penetrating injuries Multiple sites Potential to bleed up to 50% of circulating volume into each hemithorax • Massive Haemothorax = 1000 -1500 m. L or 250 ml/ hour over next 3 -4 hours • 400 m. L – blunting of costophrenic angle

More than one pathology!
Chest Drain insertion
Open Pneumothorax • Definition • Pathophysiology? • Wound diameter? • Treatment?
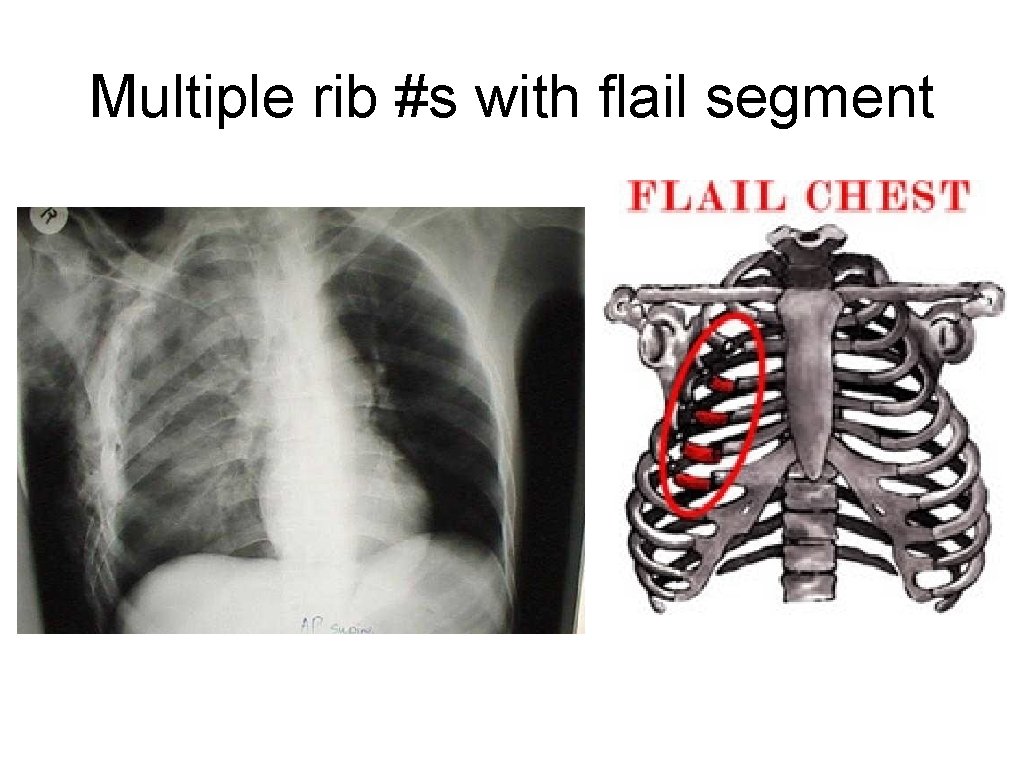
Primary Assessment: Specific, potentially life-threatening injuries to look out for: (b) Blunt chest injury - Flail chest (90% associated with pulmonary contusions) - Ruptured aorta - Ruptured diaphragm
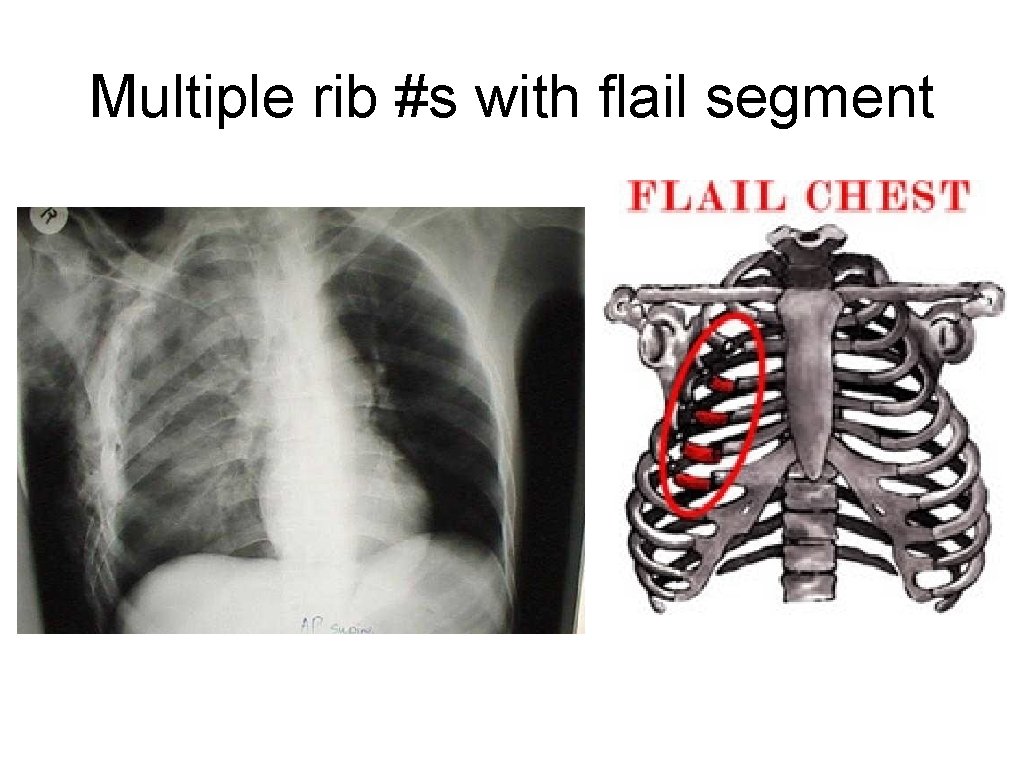
Multiple rib #s with flail segment

Flail chest
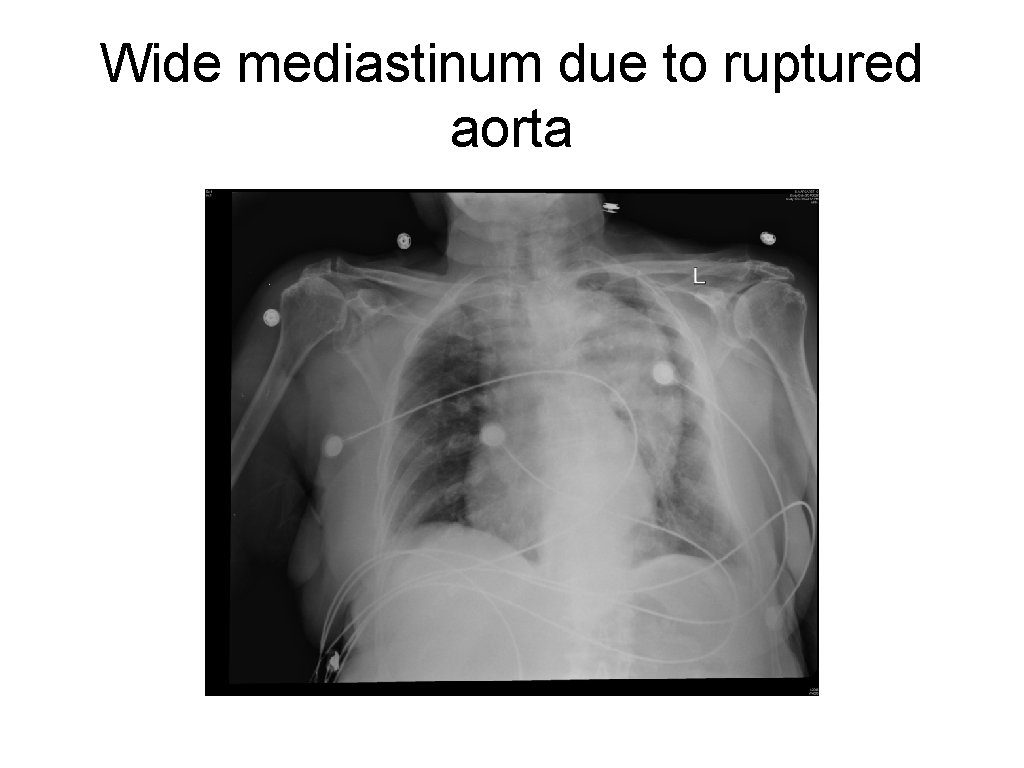
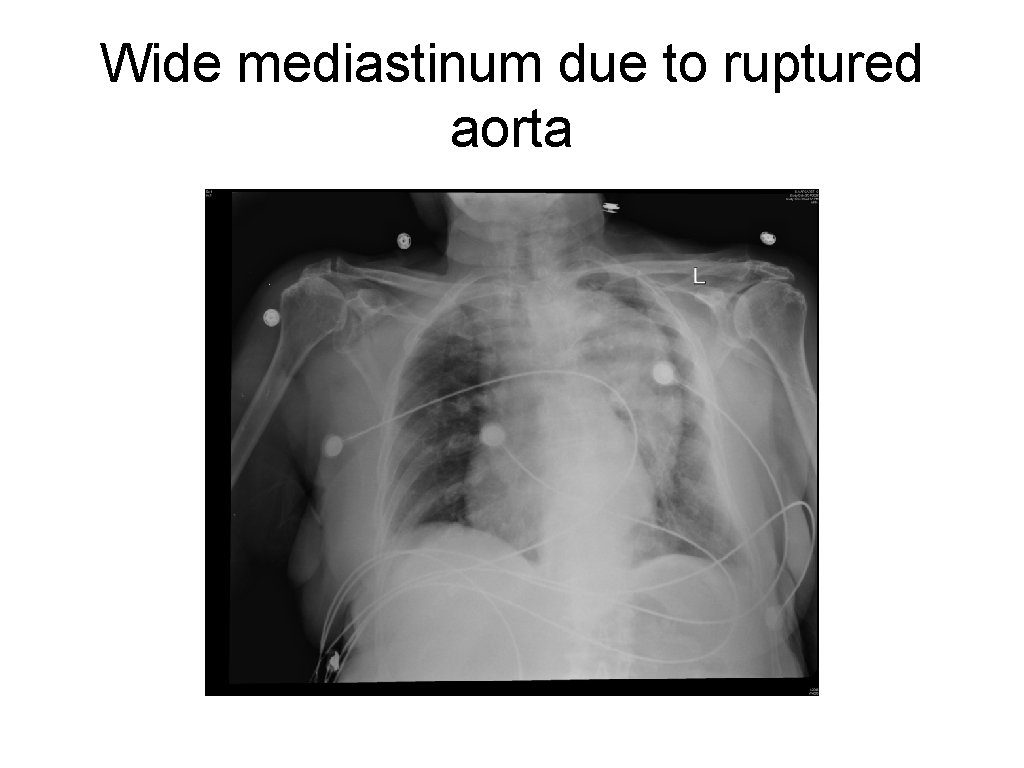
Wide mediastinum due to ruptured aorta
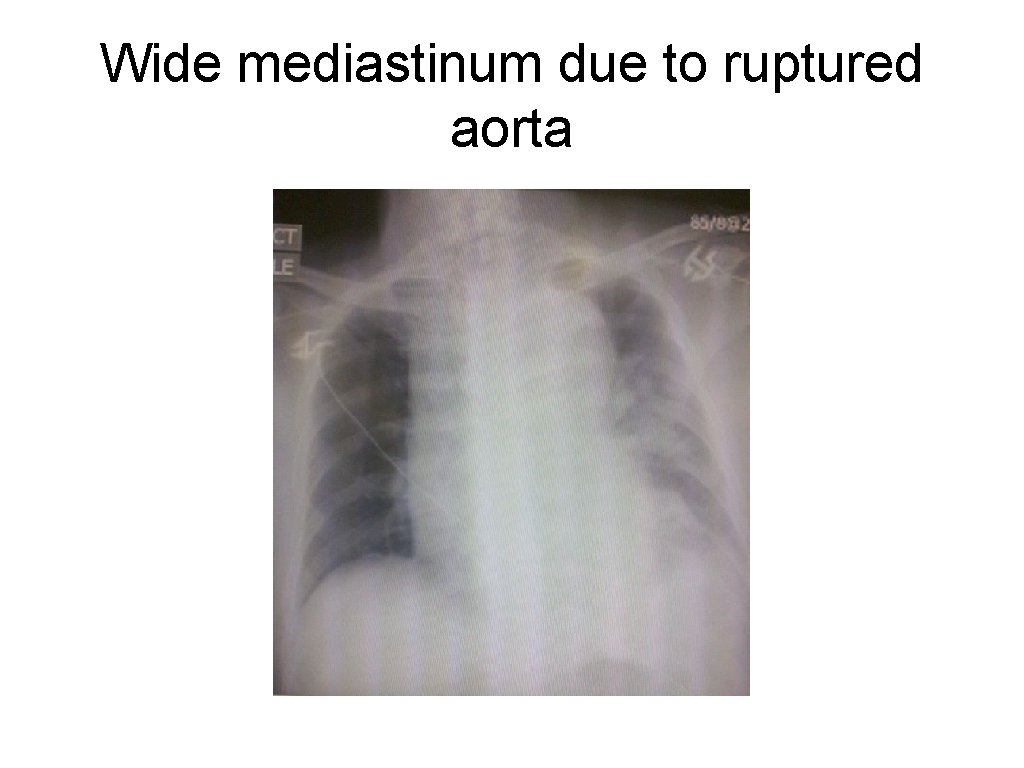
Wide mediastinum due to ruptured aorta

Ruptured left diaphragm
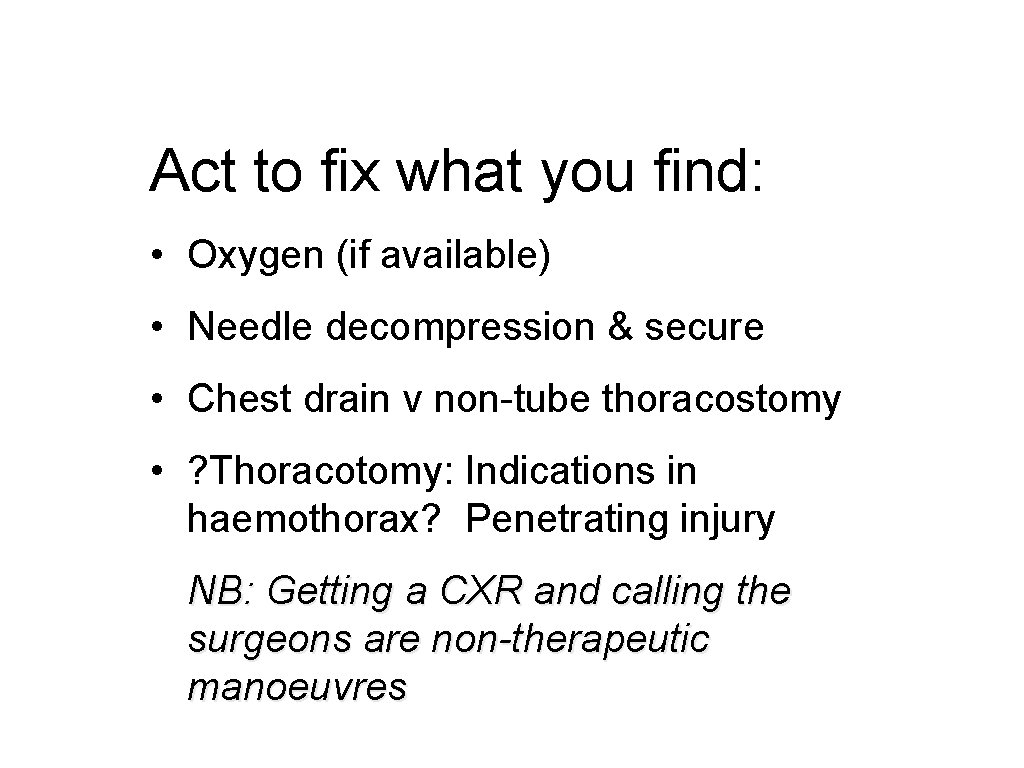
Act to fix what you find: • Oxygen (if available) • Needle decompression & secure • Chest drain v non-tube thoracostomy • ? Thoracotomy: Indications in haemothorax? Penetrating injury NB: Getting a CXR and calling the surgeons are non-therapeutic manoeuvres
Questions?
Summary: • How to assess ‘B’ in primary survey • Specific injuries to look for and how to recognise them • Indications for chest drain • Timing of the CXR • Potential dangers of # ribs… • Remember to look at patients back Copyright UKCS #284661815