Management of sexually transmitted infections Dr Anupong Chitwarakorn

- Slides: 39
Management of sexually transmitted infections Dr. Anupong Chitwarakorn Department of Disease Control Module 3 Sub module
Content Review of evidence of STD as co-factors in HIV transmission Intervention studies : STD control reduce HIV incidence Principles and strategies of STD control program in developing countries
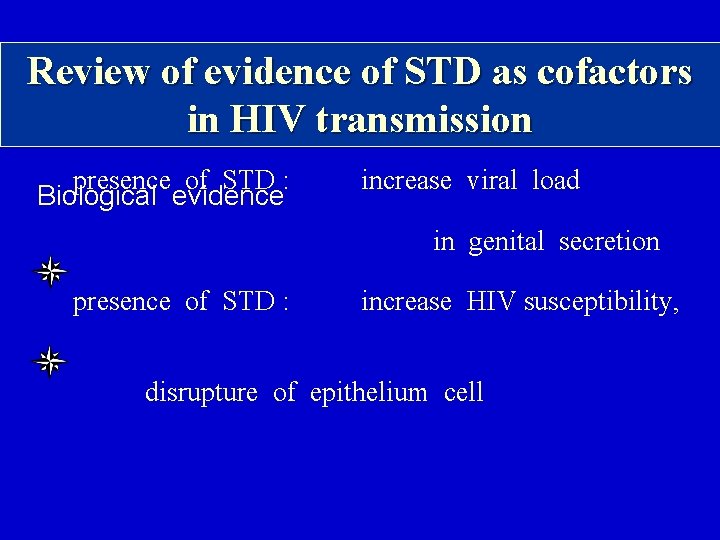
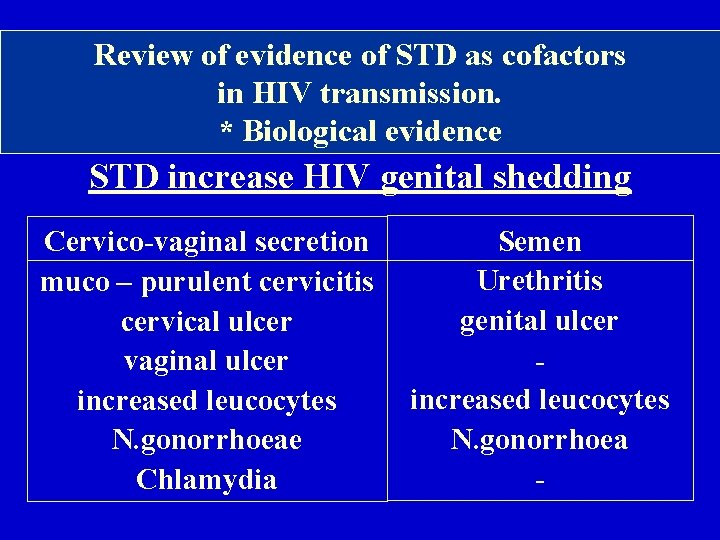
Review of evidence of STD as cofactors in HIV transmission presence of STD : Biological evidence increase viral load in genital secretion presence of STD : increase HIV susceptibility, disrupture of epithelium cell
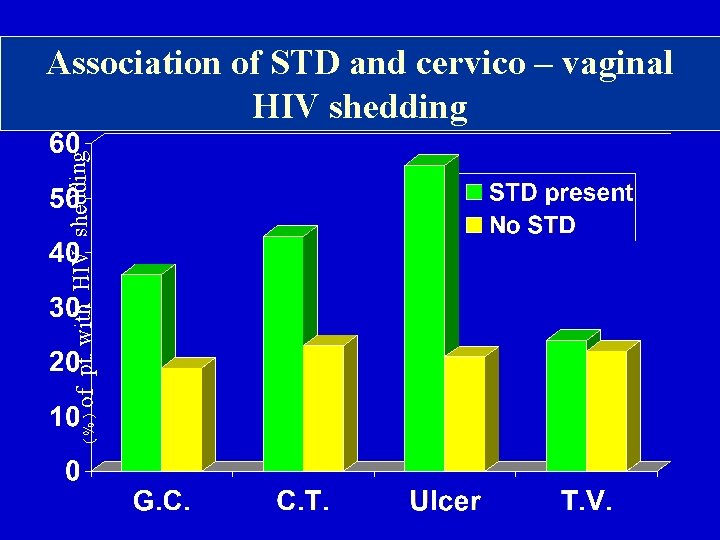
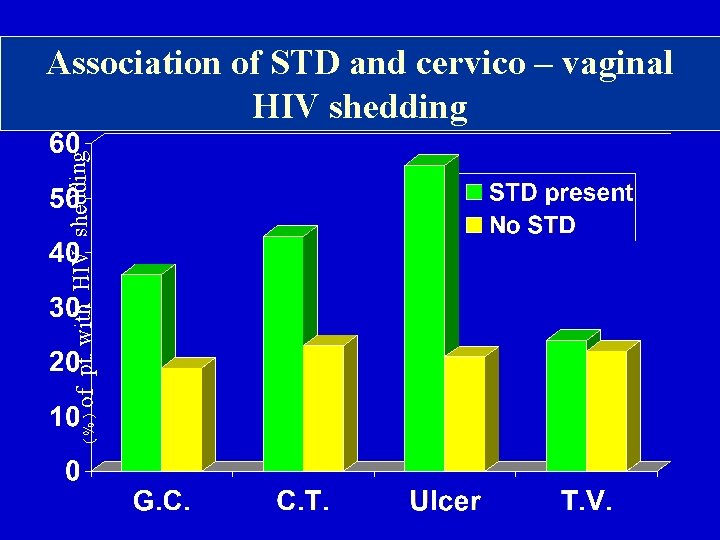
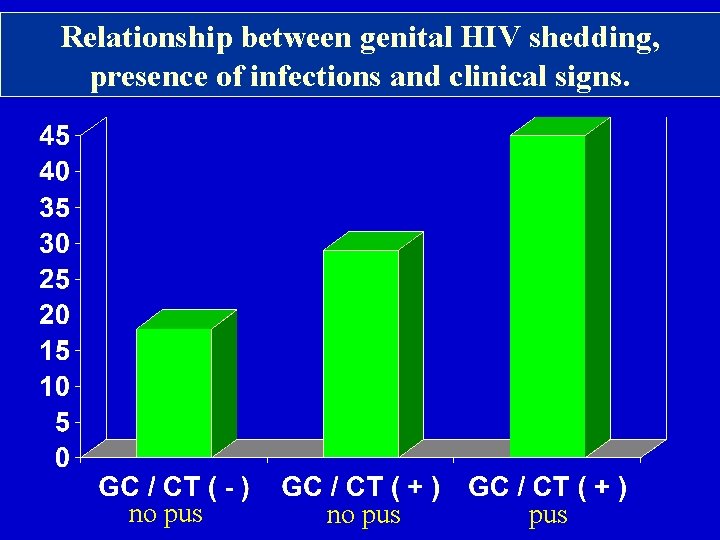
( % ) of pt. with HIV shedding Association of STD and cervico – vaginal HIV shedding
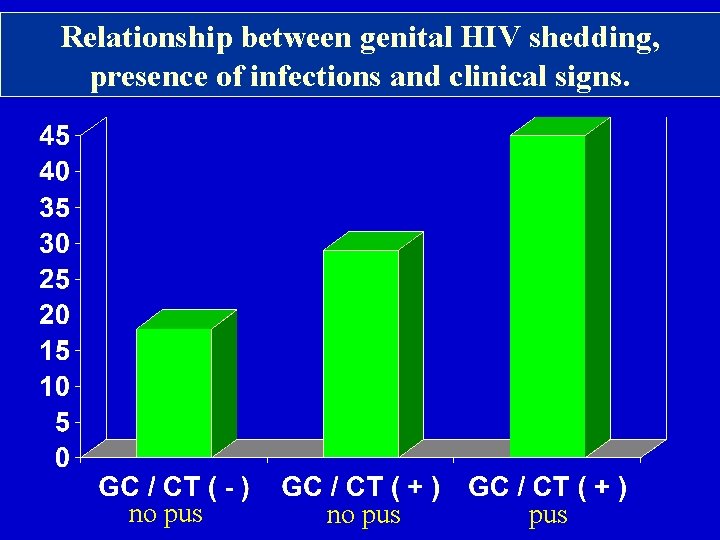
Relationship between genital HIV shedding, presence of infections and clinical signs. no pus pus
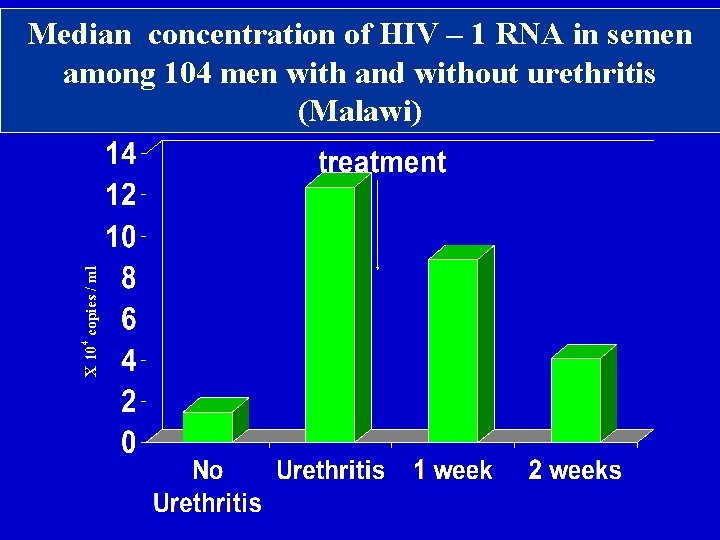
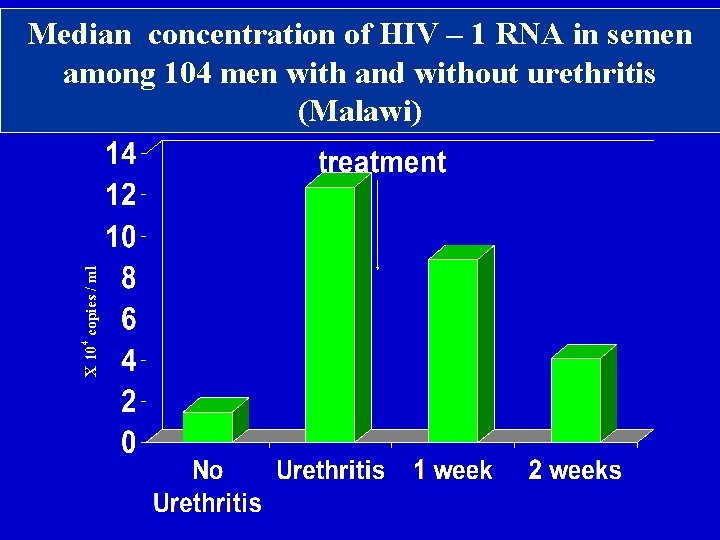
X 104 copies / ml Median concentration of HIV – 1 RNA in semen among 104 men with and without urethritis (Malawi)
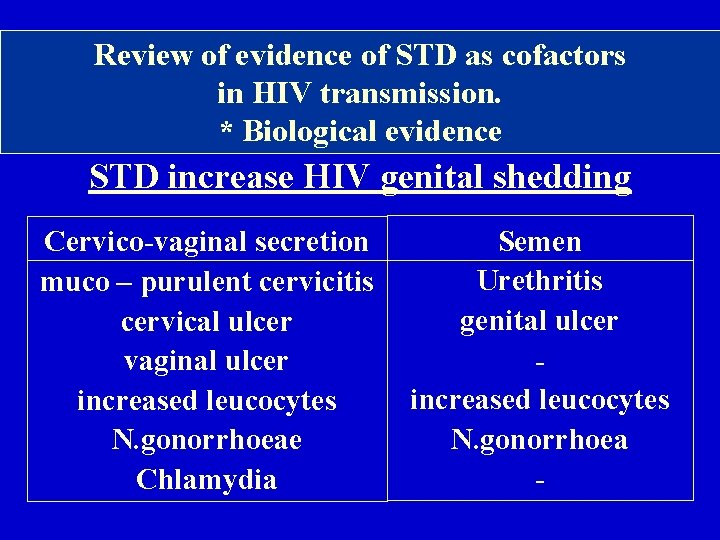
Review of evidence of STD as cofactors in HIV transmission. * Biological evidence STD increase HIV genital shedding Semen Cervico-vaginal secretion Urethritis muco – purulent cervicitis genital ulcer cervical ulcer vaginal ulcer increased leucocytes N. gonorrhoeae Chlamydia
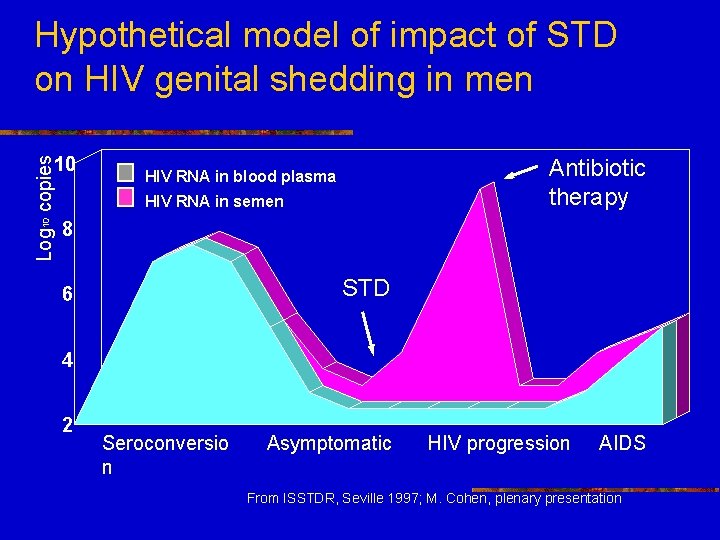
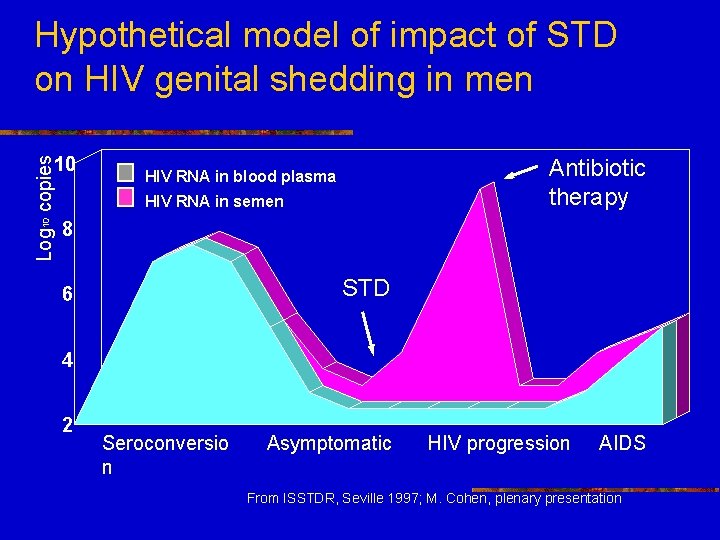
Hypothetical model of impact of STD on HIV genital shedding in men Log 10 copies 10 Antibiotic therapy HIV RNA in blood plasma HIV RNA in semen 8 STD 6 4 2 Seroconversio n Asymptomatic HIV progression AIDS From ISSTDR, Seville 1997; M. Cohen, plenary presentation
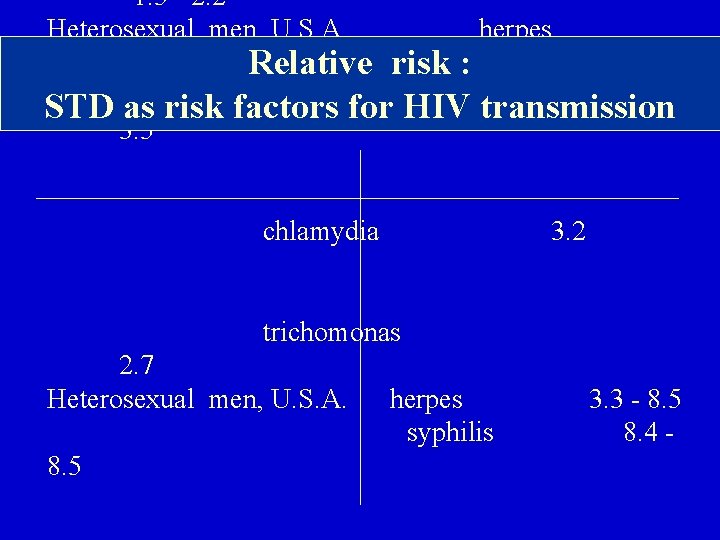
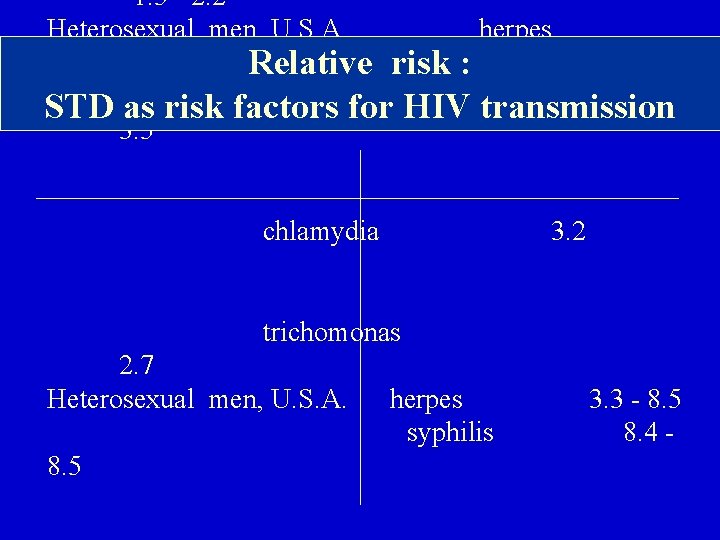
1. 5 - 2. 2 Heterosexual men, U. S. A. herpes 4. 4 Relative risk : Heterosexual women, Zaire gonorrhoea STD as risk factors for HIV transmission 3. 5 chlamydia 3. 2 trichomonas 2. 7 Heterosexual men, U. S. A. herpes 3. 3 - 8. 5 syphilis 8. 4 - 8. 5
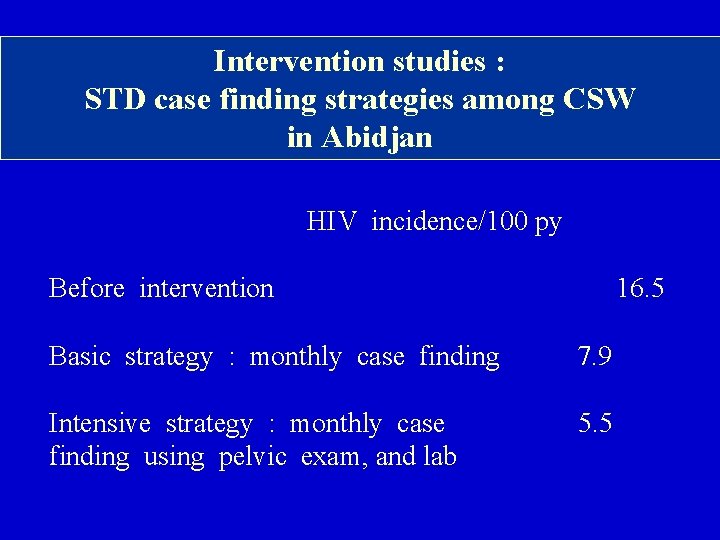
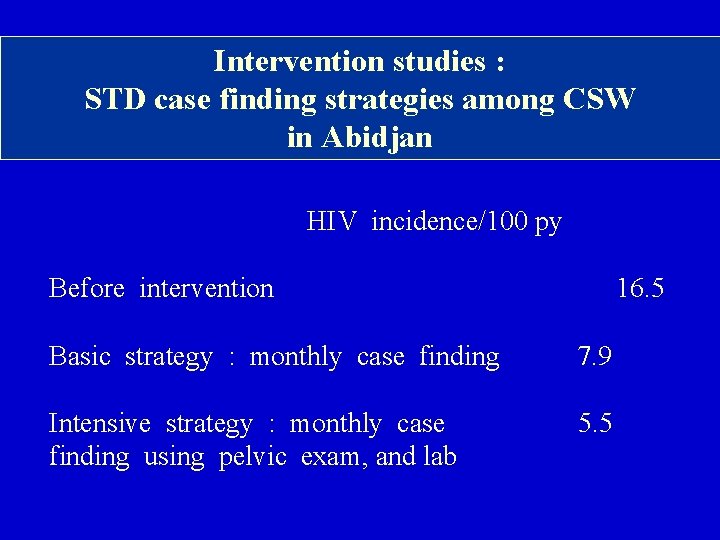
Intervention studies : STD case finding strategies among CSW in Abidjan HIV incidence/100 py Before intervention 16. 5 Basic strategy : monthly case finding 7. 9 Intensive strategy : monthly case 5. 5 finding using pelvic exam, and lab
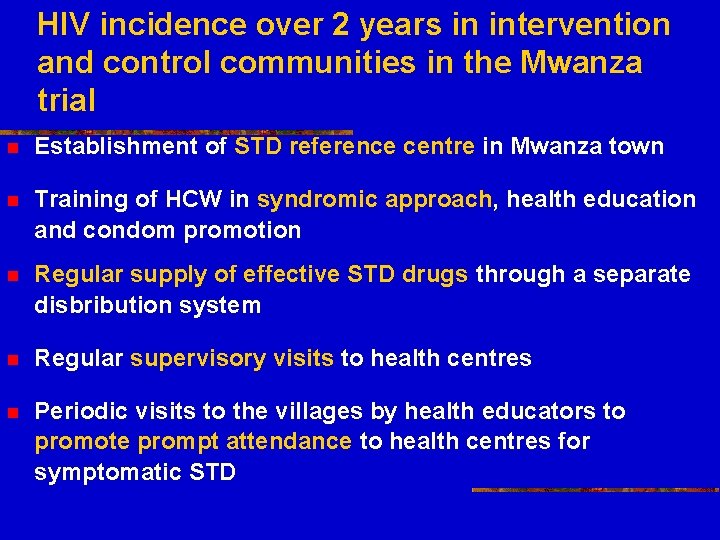
HIV incidence over 2 years in intervention and control communities in the Mwanza trial n Establishment of STD reference centre in Mwanza town n Training of HCW in syndromic approach, health education and condom promotion n Regular supply of effective STD drugs through a separate disbribution system n Regular supervisory visits to health centres n Periodic visits to the villages by health educators to promote prompt attendance to health centres for symptomatic STD
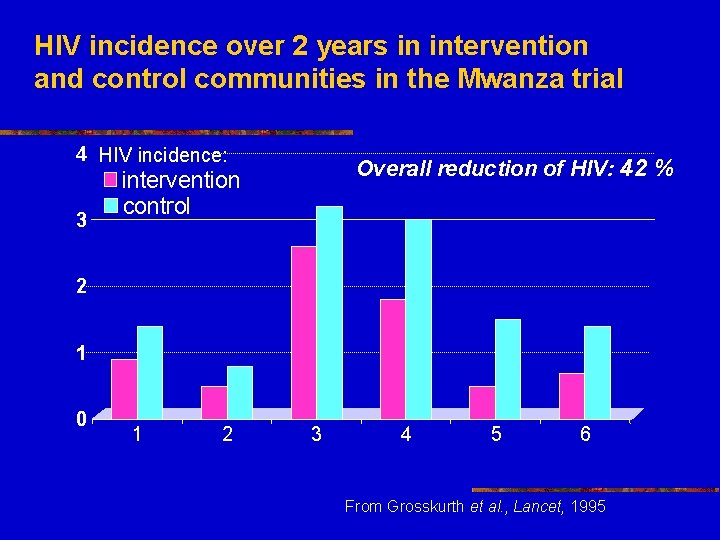
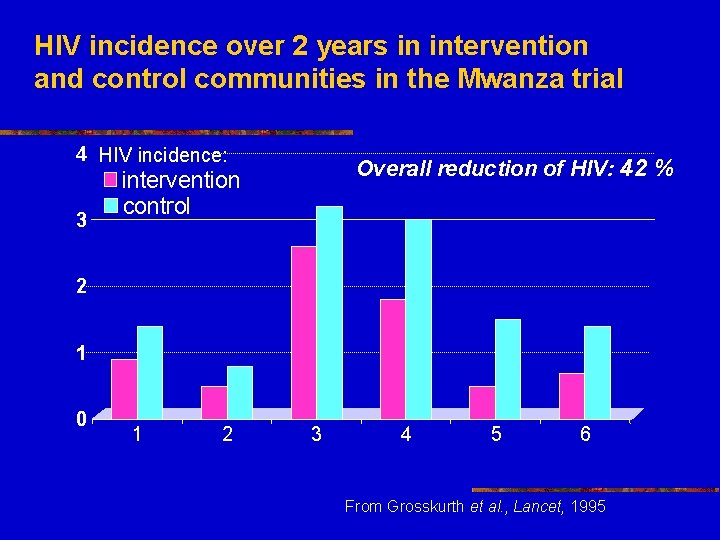
HIV incidence over 2 years in intervention and control communities in the Mwanza trial 4 HIV incidence: 3 Overall reduction of HIV: 42 % intervention control 2 1 0 1 2 3 4 5 6 From Grosskurth et al. , Lancet, 1995
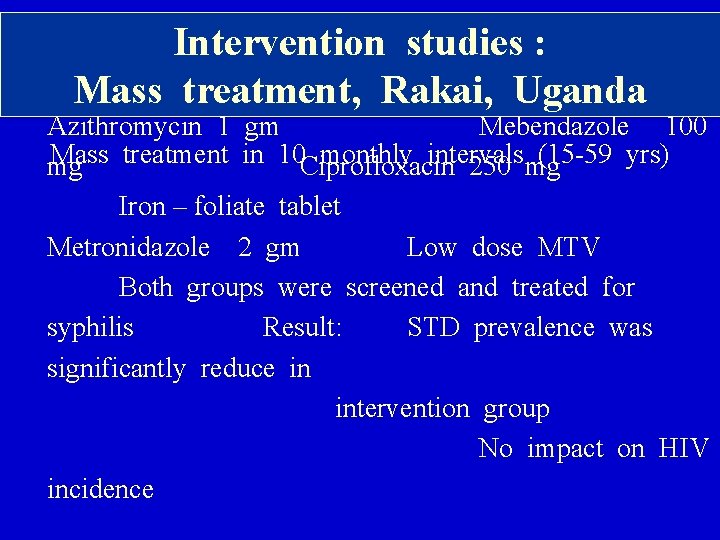
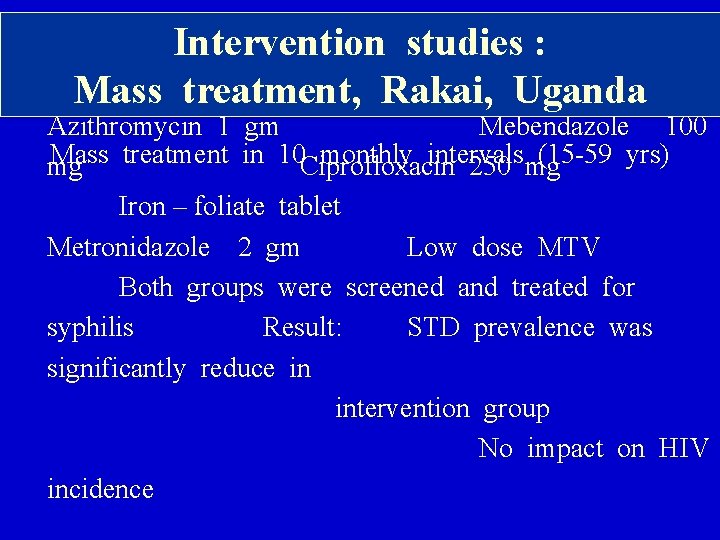
STD group (7, 871) Control clusters Intervention studies : (7, 256) Mass treatment, Rakai, Uganda Azithromycin 1 gm Mebendazole 100 Mass treatment in 10 monthly intervals (15 -59 yrs) mg Ciprofloxacin 250 mg Iron – foliate tablet Metronidazole 2 gm Low dose MTV Both groups were screened and treated for syphilis Result: STD prevalence was significantly reduce in intervention group No impact on HIV incidence
STD Control : Objectives n To interrupt the transmission of STD (acquired infection) n To prevent complication and sequelae n To reduce HIV infection risk
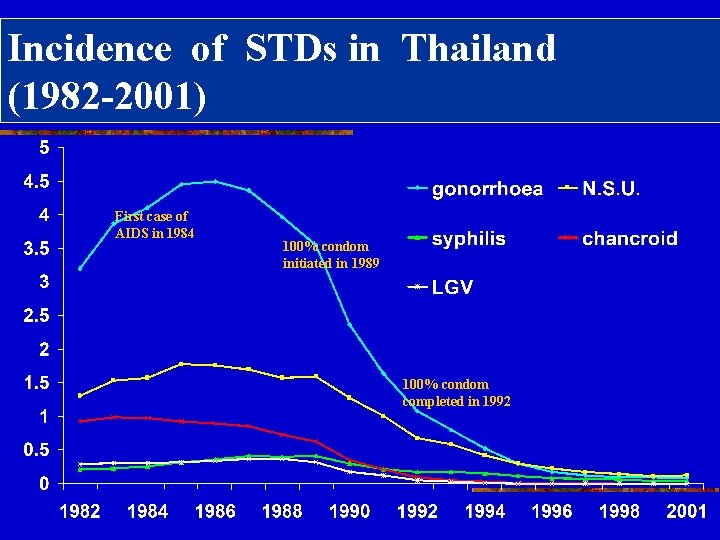
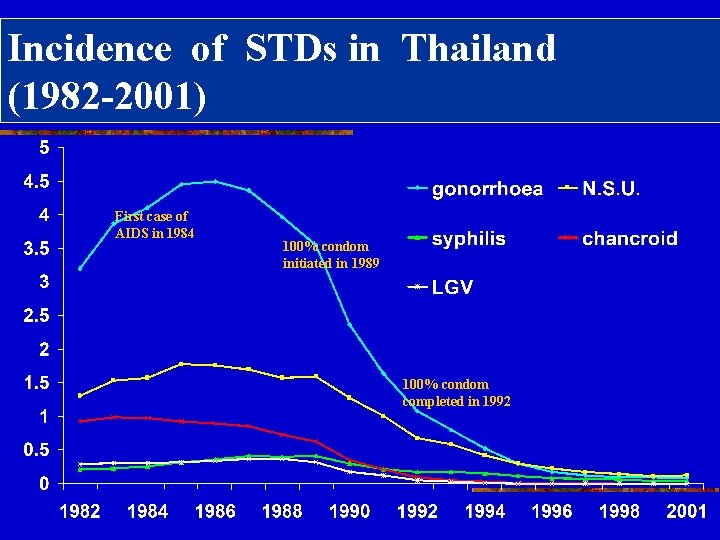
Incidence of STDs in Thailand (1982 -2001) First case of AIDS in 1984 100% condom initiated in 1989 100% condom completed in 1992
STD prevention and control: before 1989 n Case finding n Contact tracing n Case treatment n Health education n Case follow up n Control of CSW
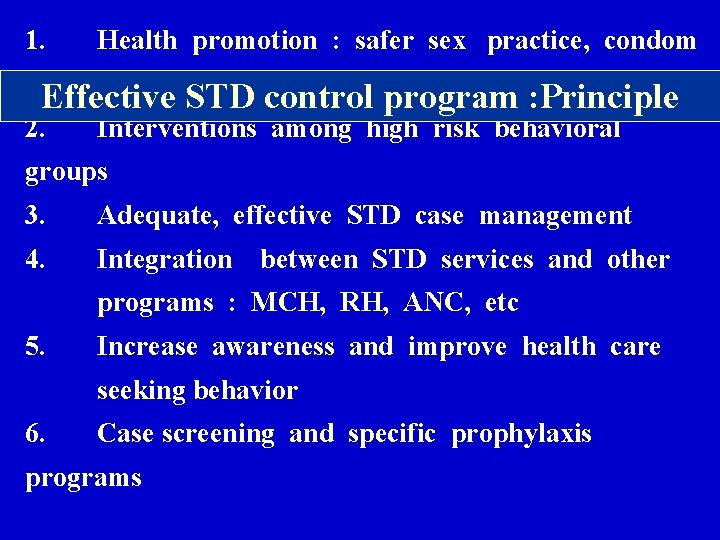
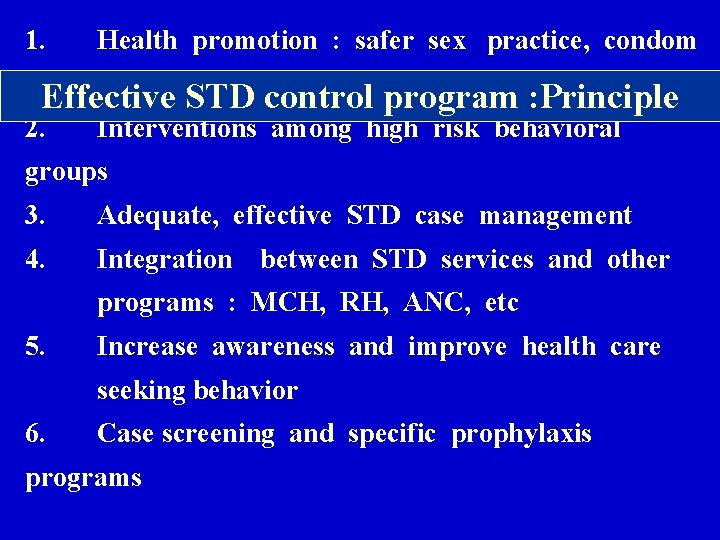
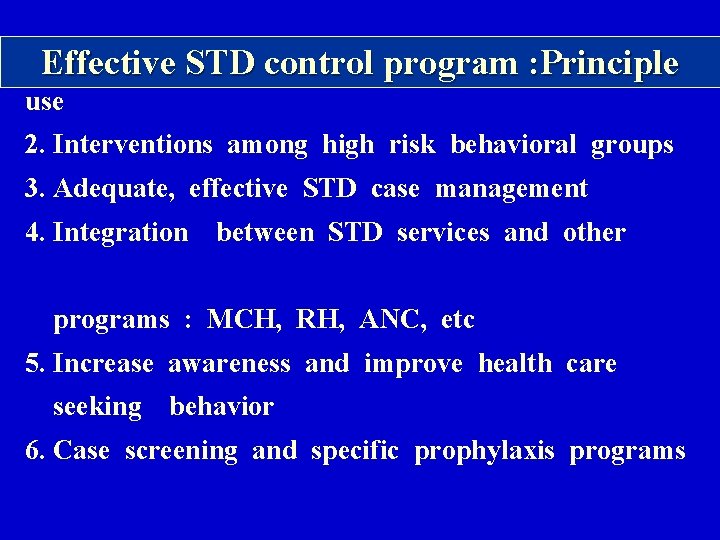
1. Health promotion : safer sex practice, condom use Effective STD control program : Principle 2. Interventions among high risk behavioral groups 3. Adequate, effective STD case management 4. Integration between STD services and other programs : MCH, RH, ANC, etc 5. Increase awareness and improve health care seeking behavior 6. Case screening and specific prophylaxis programs
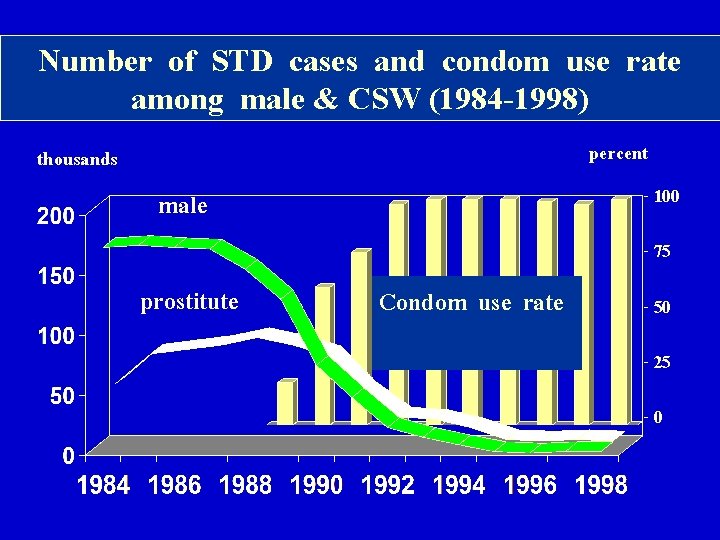
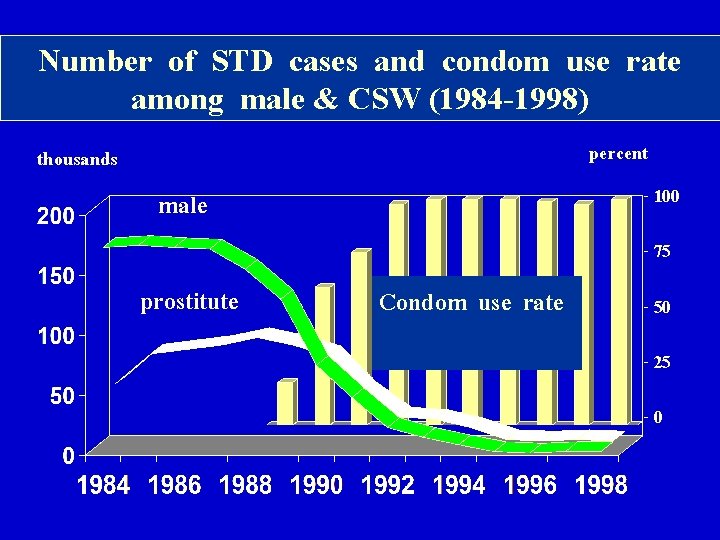
Number of STD cases and condom use rate among male & CSW (1984 -1998) percent thousands - 100 male - 75 prostitute Condom use rate - 50 - 25 -0
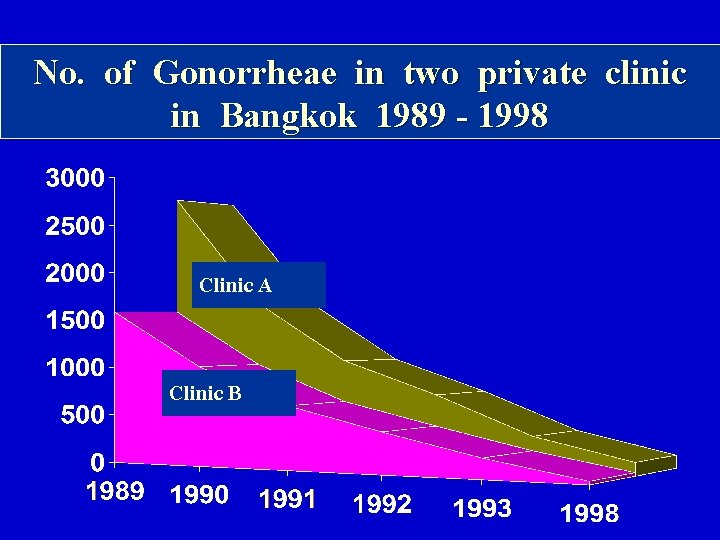
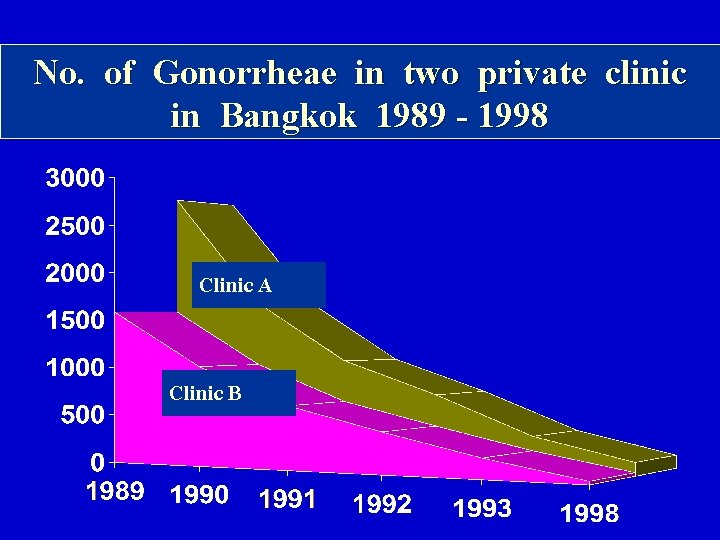
No. of Gonorrheae in two private clinic in Bangkok 1989 - 1998 Clinic A Clinic B
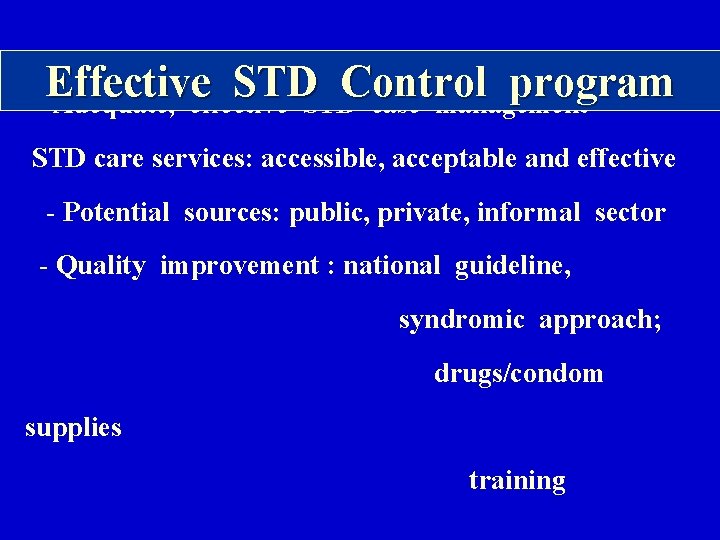
Effective STD Control program Adequate, effective STD case management STD care services: accessible, acceptable and effective - Potential sources: public, private, informal sector - Quality improvement : national guideline, syndromic approach; drugs/condom supplies training
Effective STD Control program Integration/collaboration between STD control program and other programs : ANC, MCH, FP, RH, dermatology and other existing programs To enable early detection of STD and to provide more coverage STD service
Effective STD Control program Increase awareness and improve health care seeking behavior National / local media campaigns Education for youth in / out of school Community initiatives (e. g. peer education/ clubs) Education in health facility waiting area Education as part of STD service Work place education programs
Effective STD Control program Case screening and specific prophylaxis programs • syphilis screening in pregnancy • prophylaxis of opthalmia neonatorum
Effective STD Control program Supporting components STD surveillance system Training of health staffs Monitoring, evaluation and supervision
1. Effective STD control program : Principle Health promotion : safer sex practice, condom use 2. Interventions among high risk behavioral groups 3. Adequate, effective STD case management 4. Integration between STD services and other programs : MCH, RH, ANC, etc 5. Increase awareness and improve health care seeking behavior 6. Case screening and specific prophylaxis programs
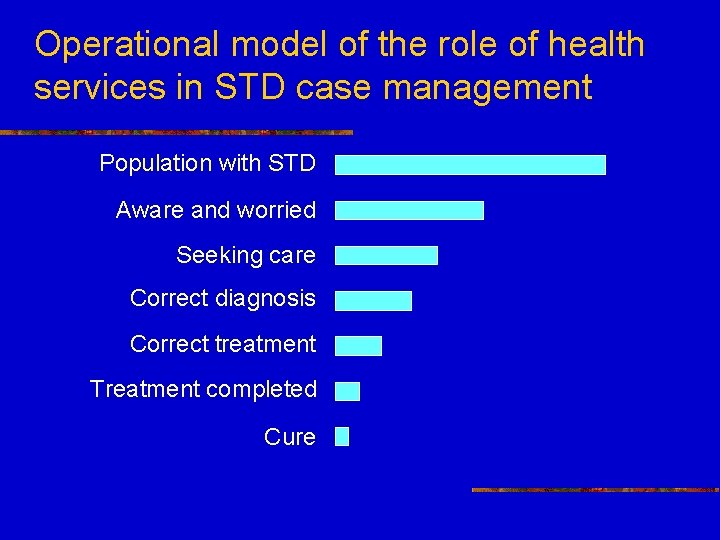
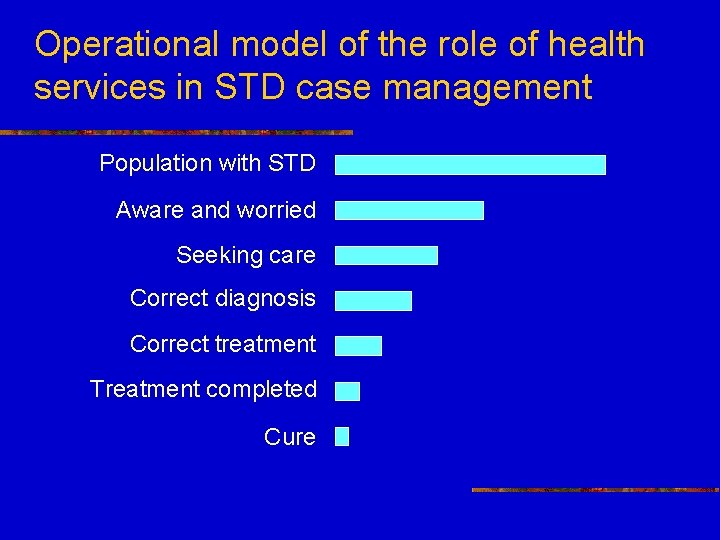
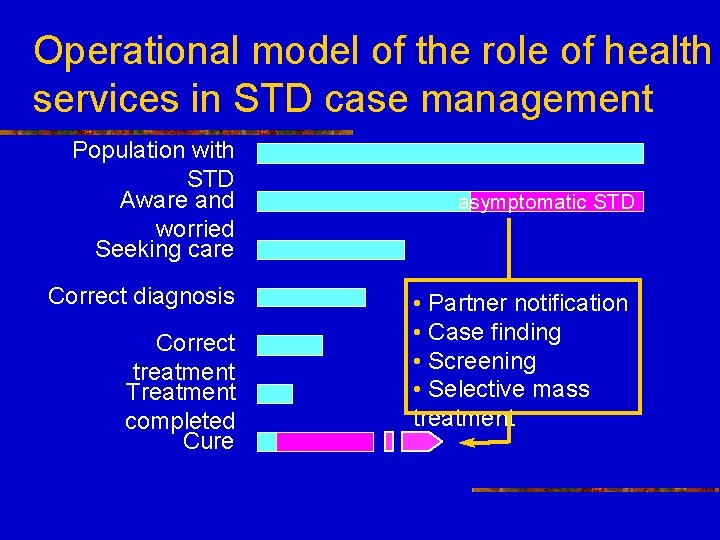
Operational model of the role of health services in STD case management Population with STD Aware and worried Seeking care Correct diagnosis Correct treatment Treatment completed Cure
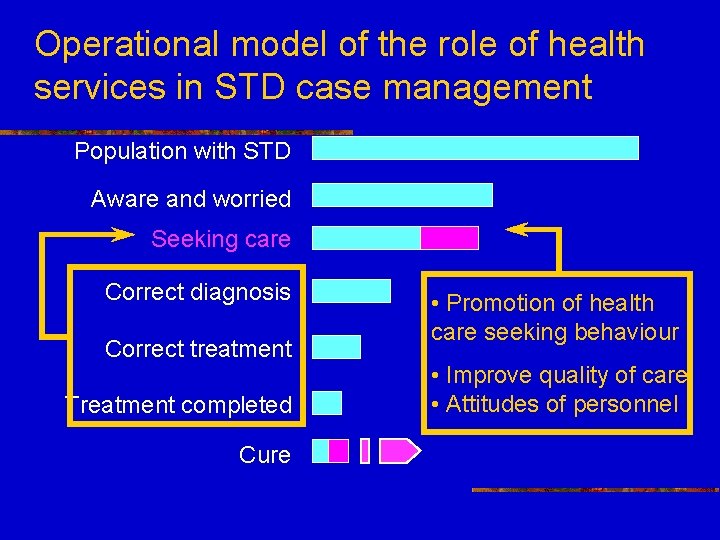
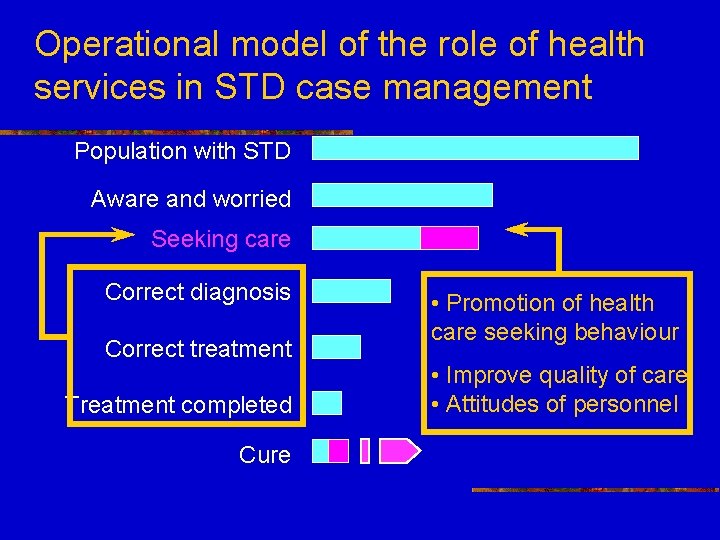
Operational model of the role of health services in STD case management Population with STD Aware and worried Seeking care Correct diagnosis Correct treatment Treatment completed Cure • Promotion of health care seeking behaviour • Improve quality of care • Attitudes of personnel
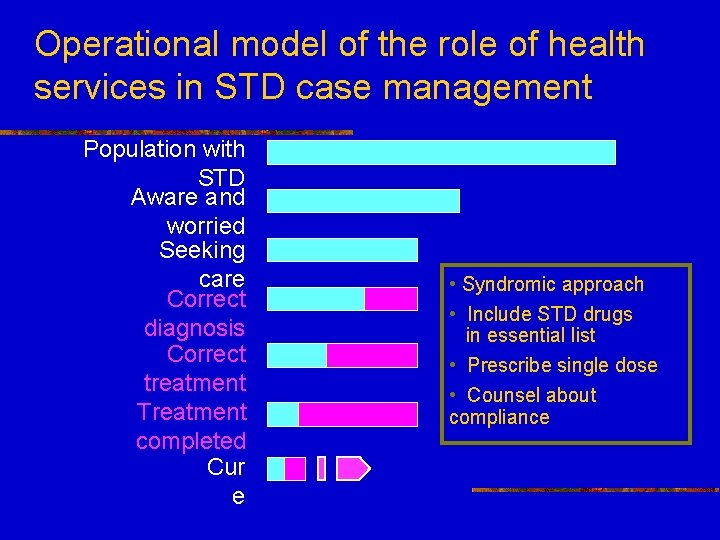
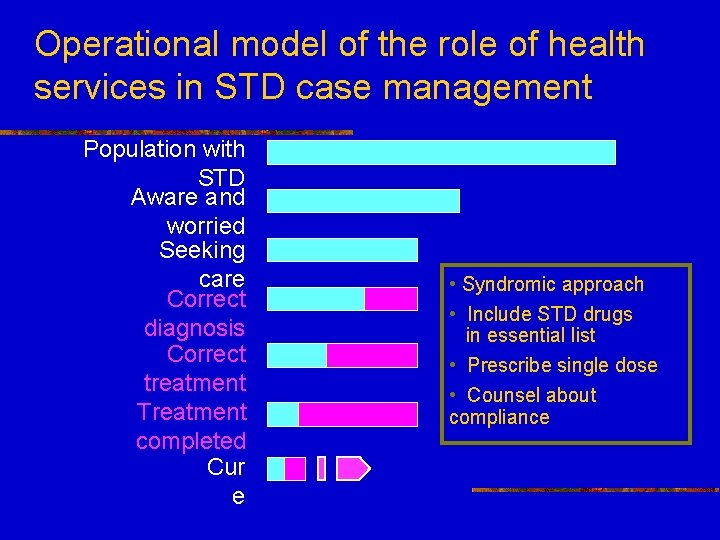
Operational model of the role of health services in STD case management Population with STD Aware and worried Seeking care Correct diagnosis Correct treatment Treatment completed Cur e • Syndromic approach • Include STD drugs in essential list • Prescribe single dose • Counsel about compliance
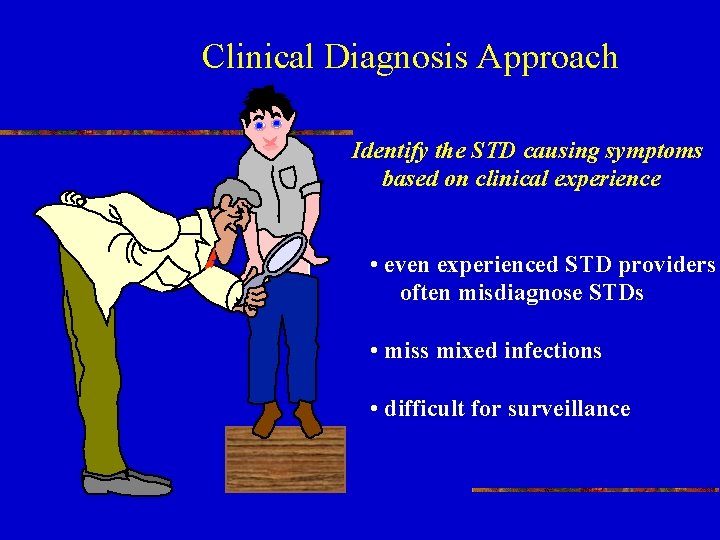
Clinical Diagnosis Approach Identify the STD causing symptoms based on clinical experience • even experienced STD providers often misdiagnose STDs • miss mixed infections • difficult for surveillance
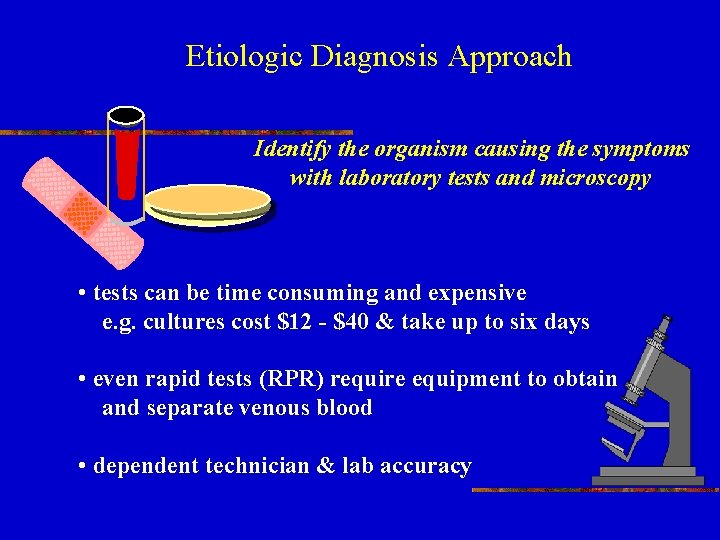
Etiologic Diagnosis Approach Identify the organism causing the symptoms with laboratory tests and microscopy • tests can be time consuming and expensive e. g. cultures cost $12 - $40 & take up to six days • even rapid tests (RPR) require equipment to obtain and separate venous blood • dependent technician & lab accuracy
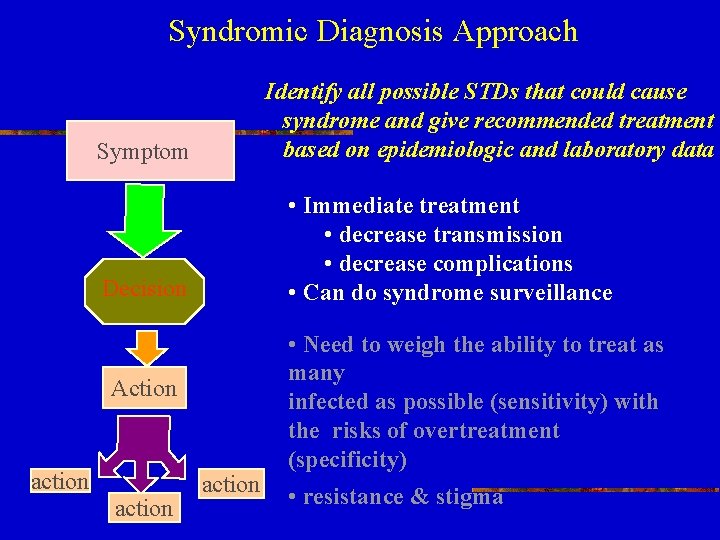
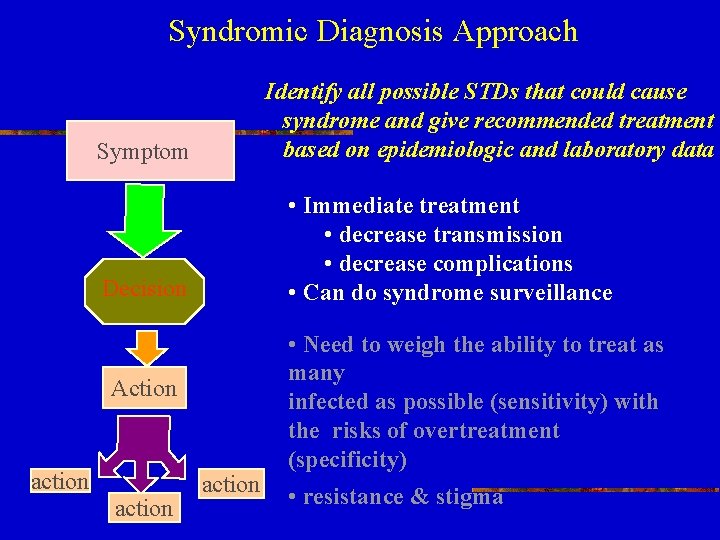
Syndromic Diagnosis Approach Symptom Identify all possible STDs that could cause syndrome and give recommended treatment based on epidemiologic and laboratory data Decision Action action • Immediate treatment • decrease transmission • decrease complications • Can do syndrome surveillance • Need to weigh the ability to treat as many infected as possible (sensitivity) with the risks of overtreatment (specificity) • resistance & stigma

THE SUPPOSED TO … APPROACH Oops! I was supposed to. . . RPR
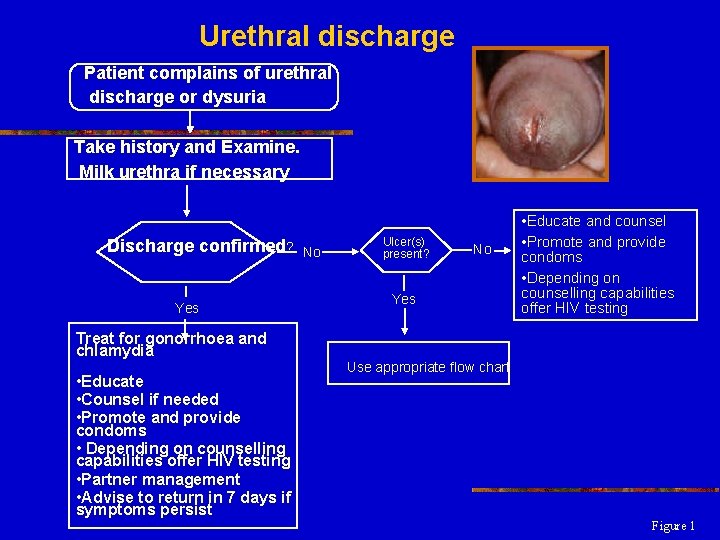
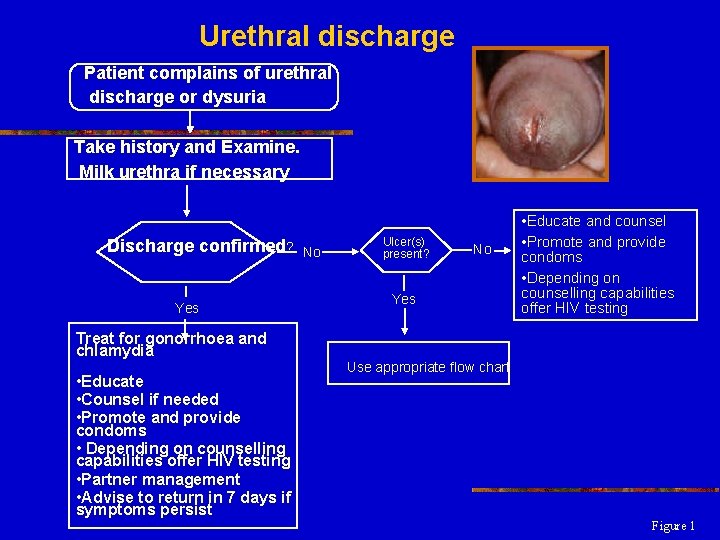
Urethral discharge Patient complains of urethral discharge or dysuria Take history and Examine. Milk urethra if necessary Discharge confirmed? Yes Treat for gonorrhoea and chlamydia • Educate • Counsel if needed • Promote and provide condoms • Depending on counselling capabilities offer HIV testing • Partner management • Advise to return in 7 days if symptoms persist No Ulcer(s) present? No Yes • Educate and counsel • Promote and provide condoms • Depending on counselling capabilities offer HIV testing Use appropriate flow chart Figure 1
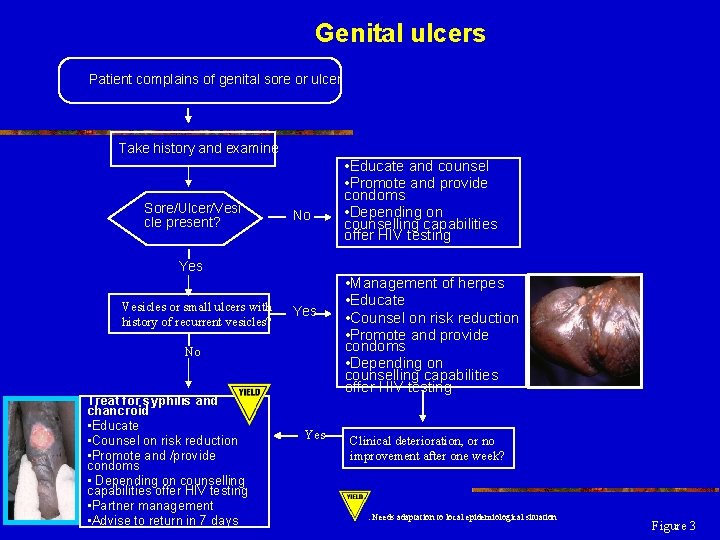
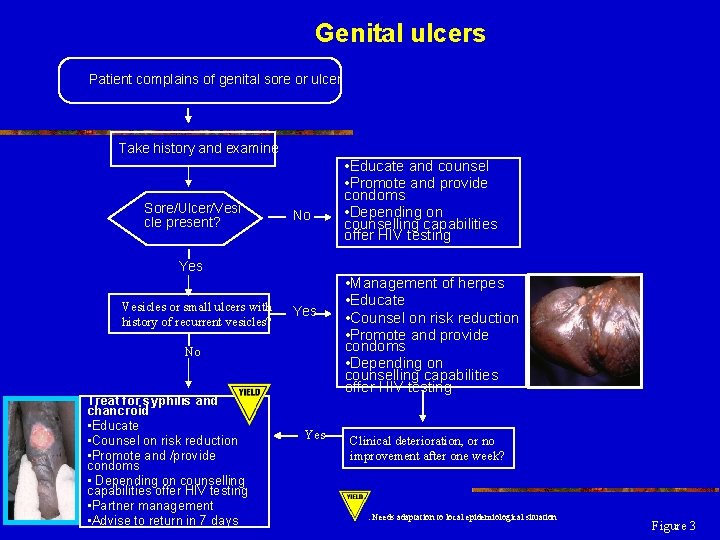
Genital ulcers Patient complains of genital sore or ulcer Take history and examine Sore/Ulcer/Vesi cle present? No • Educate and counsel • Promote and provide condoms • Depending on counselling capabilities offer HIV testing Yes Vesicles or small ulcers with history of recurrent vesicles? Yes No Treat for syphilis and chancroid • Educate • Counsel on risk reduction • Promote and /provide condoms • Depending on counselling capabilities offer HIV testing • Partner management • Advise to return in 7 days Yes • Management of herpes • Educate • Counsel on risk reduction • Promote and provide condoms • Depending on counselling capabilities offer HIV testing Clinical deterioration, or no improvement after one week? : Needs adaptation to local epidemiological situation Figure 3
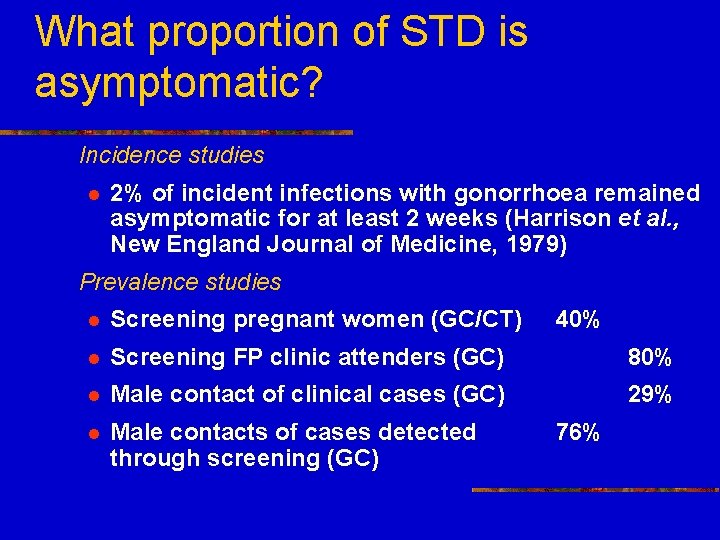
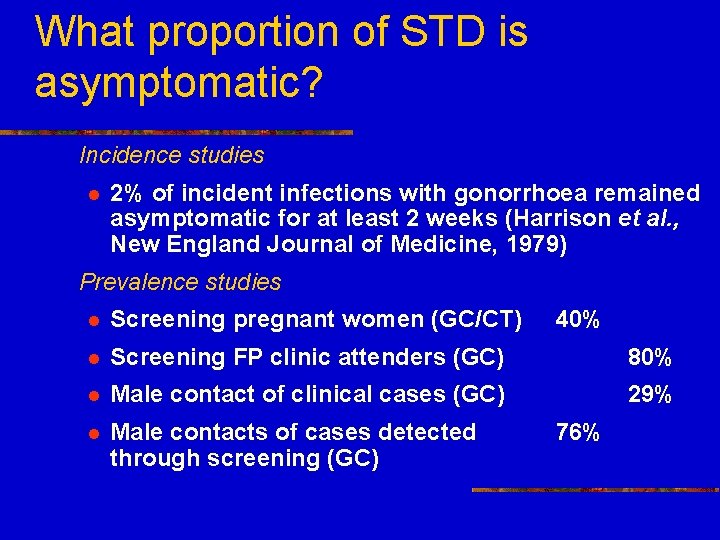
What proportion of STD is asymptomatic? Incidence studies l 2% of incident infections with gonorrhoea remained asymptomatic for at least 2 weeks (Harrison et al. , New England Journal of Medicine, 1979) Prevalence studies l Screening pregnant women (GC/CT) 40% l Screening FP clinic attenders (GC) 80% l Male contact of clinical cases (GC) 29% l Male contacts of cases detected through screening (GC) 76%
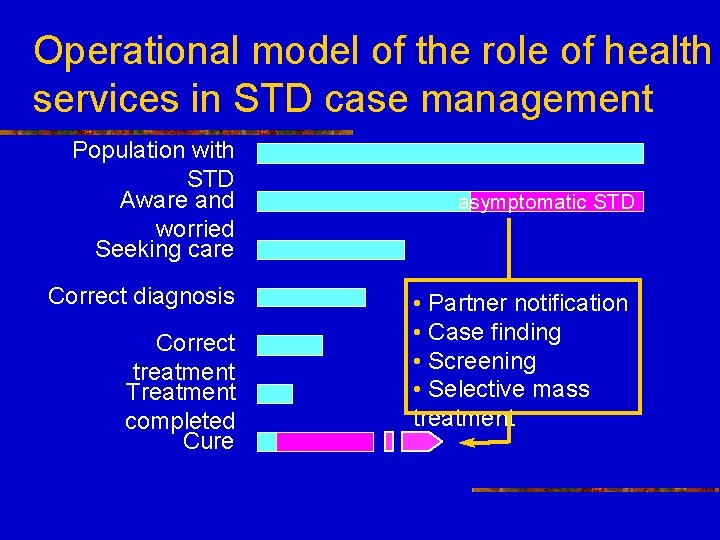
Operational model of the role of health services in STD case management Population with STD Aware and worried Seeking care Correct diagnosis Correct treatment Treatment completed Cure asymptomatic STD • Partner notification • Case finding • Screening • Selective mass treatment
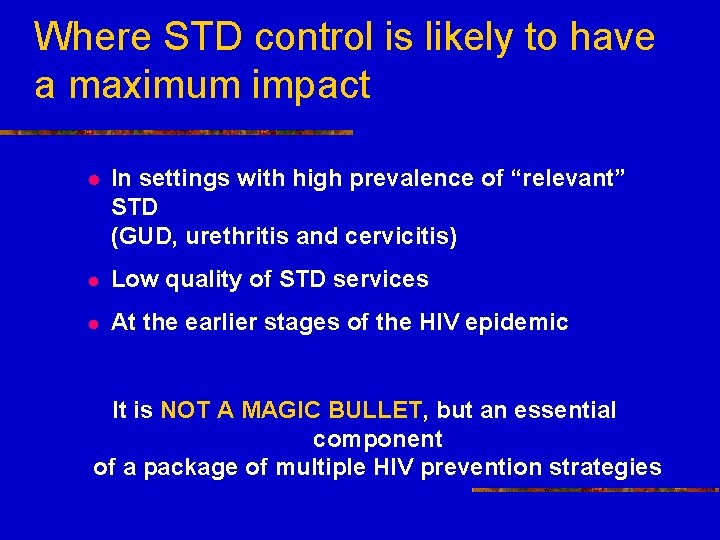
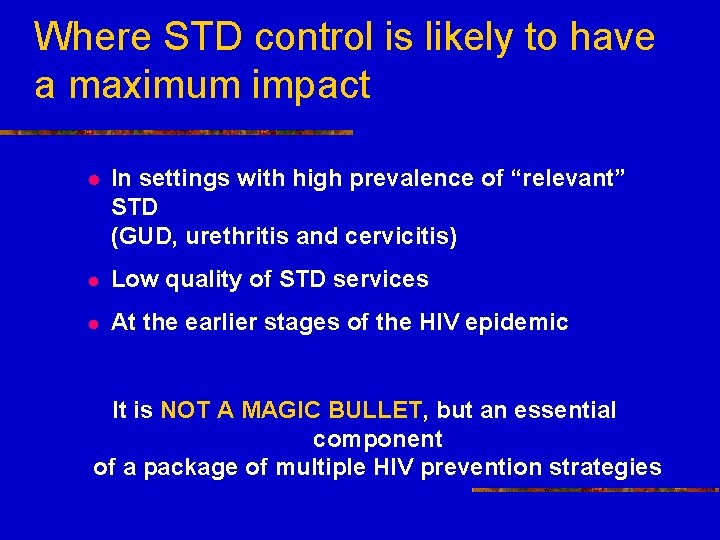
Where STD control is likely to have a maximum impact l In settings with high prevalence of “relevant” STD (GUD, urethritis and cervicitis) l Low quality of STD services l At the earlier stages of the HIV epidemic It is NOT A MAGIC BULLET, but an essential component of a package of multiple HIV prevention strategies
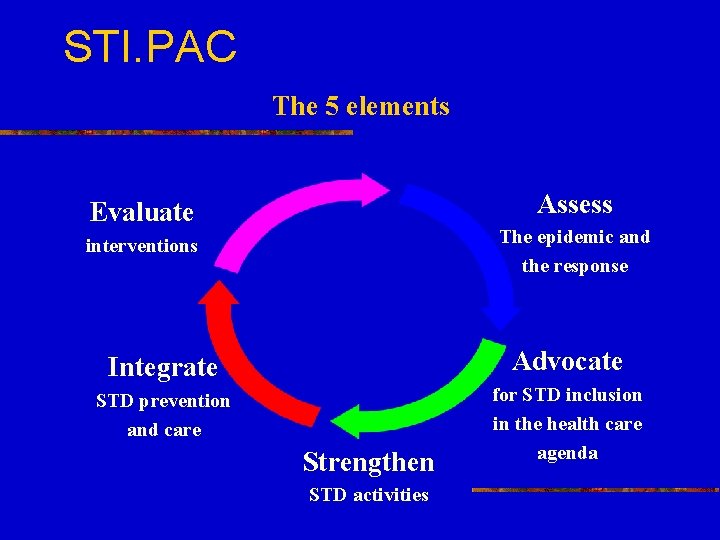
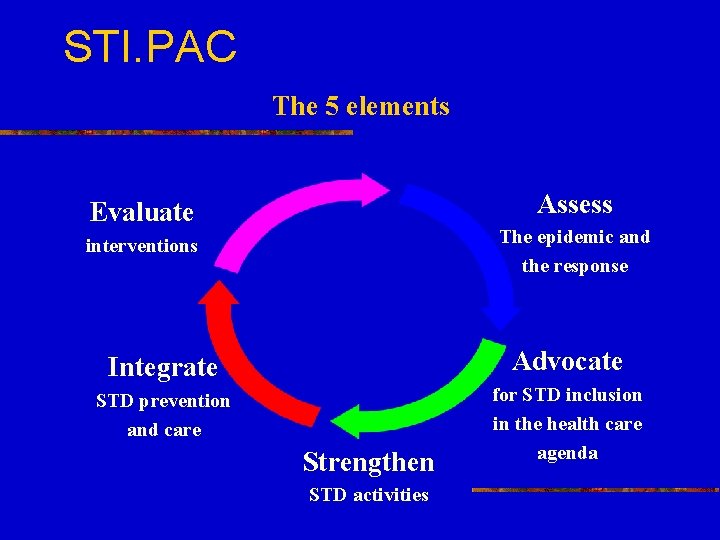
STI. PAC The 5 elements Assess Evaluate The epidemic and the response interventions Integrate Advocate STD prevention and care for STD inclusion in the health care agenda Strengthen STD activities
Thank you See you in Bangkok Word AIDS Conference 11 -16 July, 2004